The most common etiologic organism associated clinically with actinomycosis is Actinomyces israelii. Actinomyces species exist in the normal flora of the gastrointestinal system and female genitourinary tracts. Abdominal actinomycosis accounts for 20% of all cases, and its diagnosis is difficult.1
We report a case of abdominal actinomycosis that mimicked acute appendicitis.
Case report
A 51-year-old woman with right lower quadrant abdominal pain, fever and vomiting that persisted for 3 days was admitted to our emergency service. On physical examination, her pulse rate was 96 beats/min, her body temperature was 37.4°C, and she had tenderness and rebound pain in the right lower quadrant of the abdomen. The patient had had an intrauterine contraceptive device in place for 10 years. The laboratory findings were within normal limits, except for a C-reactive protein level of 71 mg/L. A computed tomography (CT) scan of the abdomen showed a lesion 3 cm × 2 cm in size that retained minimal intravenous contrast material near the cecum (Fig. 1). Inflammation surrounding this lesion was noted, and a diagnosis of panniculitis was considered. The diameter of the appendix was 7 mm (Fig. 1D).
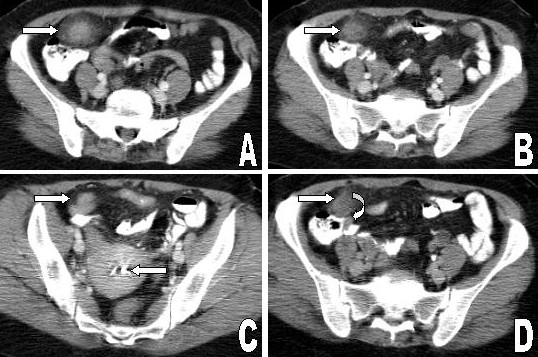
FIG. 1. Abdominal computed tomography images after the administration of oral and intravenous contrast show a 3 × 2-cm contrast-enhancing mass lesion near the cecum (A, B, C [right arrow], D). The intrauterine device is indicated by the arrow on the left. The thickened appendix is shown in panel D (curved arrow).
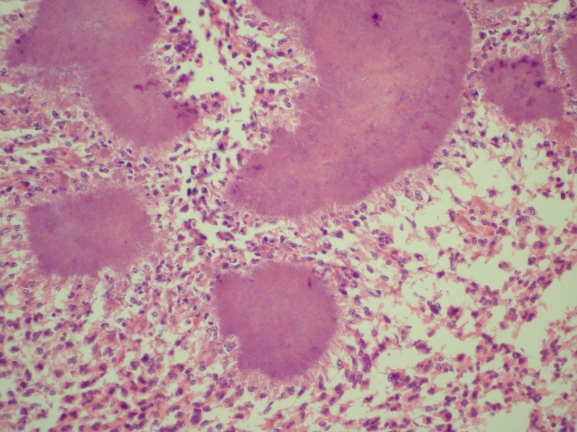
Because the patient's clinical signs suggested acute appendicitis, surgery was performed. Abscesses 4 cm × 3 cm and 2 cm × 1 cm in size were found on the greater omentum and in the periappendicular region respectively. The abscesses and the appendix were excised. Pathological and light microscopic examination showed Actinomyces colonies between inflammatory cells (Fig. 2) and a normal appendix. Postoperatively, the patient received 50 mg/kg of ampicillin intravenously each day for 14 days, followed by 500 mg of amoxicillin orally 3 times a day for 3 months. In addition, the intrauterine contraceptive device was removed. Findings on air-contrast barium enema performed after discharge were within normal limits. Currently, the patient is well, has no signs or symptoms of omental actinomycosis and the CT scan is normal.
FIG. 2. On histologic examination, the abscesses show Actinomyces colonies between inflammatory cells (hematoxylin–eosin stain, original magnification × 400).
Discussion
Abdominal actinomycosis is a rare and insidious clinical entity.1,2 It should be considered in the diagnosis of a patient who presents with nonspecific symptoms and signs including fever, a palpable mass and leukocytosis.2 Recognized causal associations include a history of appendicitis, diverticulitis, inflammatory bowel disease, use of an intrauterine contraceptive device and open or laparoscopic surgery.3 Abdominal actinomycosis should be differentiated from Crohn disease, ulcerative colitis, diverticulitis, neoplasms, intestinal tuberculosis and appendicitis.2,4 We thought that the source of actinomycosis in our patient was the long-term use of an intrauterine contraceptive device.
Radiologic techniques are inadequate in the diagnosis of abdominal actinomycosis, except for CT, which shows the site and content of the lesions and their relation to adjacent tissues.2,3 When actinomycosis is suspected, CT-guided aspiration, with or without core biopsy of suspicious lesions, is a useful investigation.3 Surgery is also valuable as a therapeutic adjunct because it enables the débridement of necrotic tissue, the removal of persistent sinuses and a definitive diagnosis.2 The definitive diagnosis of actinomycosis requires microscopic proof of either the pathogen itself or the presence of specific “sulfur granules.”2,3 A combination of long-term antibiotic therapy and adequate surgery is necessary to ensure the complete eradication of actinomycosis because of the large amount of reactive fibrosis formed by the infection.5 However, recent studies have shown that a combination of complete surgical resection followed by short-term antibiotic treatment is effective therapy.4 Penicillin has been shown to be effective in treating abdominal actinomycosis. Other antibiotics used include tetracycline, erythromycin, doxycycline, clindamycin, imipenem, ceftriaxone and ciprofloxacin.1
As a result, abdominal actinomycosis should be considered in the differential diagnosis of patients who have predisposing factors for actinomycosis and symptoms such as fever, a palpable mass and leukocytosis. In addition, surgery can be performed to supply a definitive diagnosis.
Competing interests: None declared.
Accepted for publication Mar. 25, 2008
Correspondence to: Dr. H. Turan, Baskent University Konya Medical and Research Center, Hocacihan mahallesi, Saray caddesi No: 1, Selçuklu 42080 Konya, Turkey; fax 90 332 2570637; turanhale@yahoo.com
References
- 1.Russo TA. Agents of actinomycosis. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. New York: Churchill Livingstone; 2005. p. 2924-34.
- 2.Huang CJ, Huang TJ, Hsieh JS. Pseudo-colonic carcinoma caused by abdominal actinomycosis: report of two cases. Int J Colorectal Dis 2004;19:283-6. [DOI] [PubMed]
- 3.Abela J, Sciberras J, Meilak M, et al. Omental actinomycosis presenting with right lower quadrant abdominal pain. J Clin Pathol 2004;57:671. [PMC free article] [PubMed]
- 4.Koren R, Dekel Y, Ramadan E, et al. Periappendiceal actinomycosis mimicking malignancy report of a case. Pathol Res Pract 2002;198:441-3. [DOI] [PubMed]
- 5.Atad J, Hallak M, Sharon A, et al. Pelvic actinomycosis. Is long-term antibiotic therapy necessary? J Reprod Med 1999;44:939-44. [PubMed]