The currently accepted definition of an intrathoracic goitre is a thyroid gland with more than 50% of its mass located below the thoracic inlet.1,2 This term can be further classified as an “incomplete” or a “complete” intrathoracic goitre. When the goitre is “incomplete,” a major portion of the goitre on the neck is visible, with its lower pole being substernal, subclavicular or intrathoracic. Conversely, a “complete” or “true” intrathoracic goitre is one that is completely within the mediastinum and separate from a coexisting cervical thyroid gland.1 Thus, the uppermost part is barely palpable in the sternal notch.
Most intrathoracic goitres can be removed safely through a cervical incision.1–5 More invasive sternotomy can be performed for complicated cases in which the goitre cannot be removed by any other procedure.
Case report
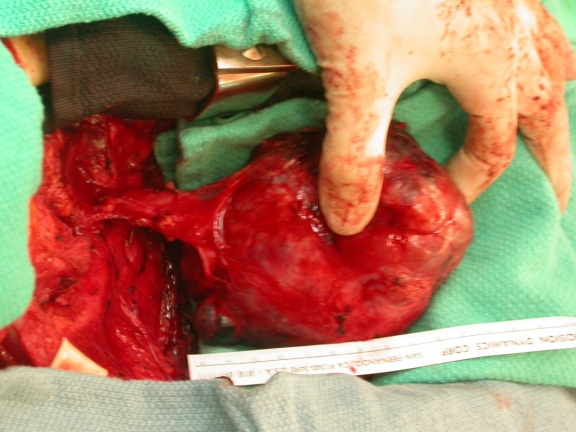
A 33-year-old woman was referred to the otolaryngology clinic with deep vein thrombosis (DVT) in her left subclavian vein shown on ultrasonography and a large retrosternal mass shown on computed tomography, with extension into the anterior superior mediastinum (Fig. 1). There was associated compression of the left subclavian vein, which compromised venous return in the left arm, with extreme displacement of the trachea and the aortic arch due to the large goitre.
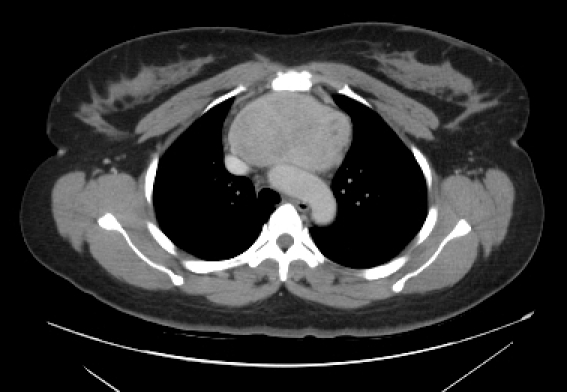
FIG. 1. Computed tomography scan showing the goitre as a large retrosternal mass extending into the anterior superior mediastinum.
On examination, she was found to be asymptomatic, hemodynamically stable and clinically euthyroid. Her medical history was significant for nodular thyroid disease: a right hemithyroidectomy had been performed in 2001. There was no history of neck irradiation or environmental exposure. Her only medication was warfarin sodium for the DVT. She had no known allergies. Her family history included an aunt with suspected benign thyroid goitre.
The patient underwent surgery to remove her true intrathoracic goitre. Initially, the left thyroid lobe was removed, followed by central compartment and mediastinal dissection, with both recurrent nerves traced into the chest and with vascular control of the major vessels in the neck bilaterally. Owing to limited transcervical delivery, the cervical incision was extended, and a midline sternotomy was created with a reciprocating pneumatic saw.
The mass was mobilized from the pericardium, the mediastinal pleurae and great vessels with the use of a combination of blunt and sharp techniques. The vascular supply was from pericardial and thymic vessels, which were divided after control with hemoclips. At the superior-most aspect of the dissection, the innominate vein was effaced. The innominate vein and the distal left subclavian veins were encircled for vascular control. The venous tributaries to the mass were divided, and the specimen was removed (Fig. 2). The pericardium was left intact. Two large-bore chest tubes were brought out through separate incisions to drain the retrosternal space. The sternum was reapproximated with stainless steel wires, and the wound was closed in layers.
FIG. 2. Surgical view showing the removal of an intrathoracic goitre.
Postoperatively, she was extubated in the cardiovascular intensive care unit with no complications. At 2-week follow-up, her cervical and sternal incisions were healing well, and the sternum was stable. Thyroid-stimulating hormone, parathyroid hormone and ionized calcium levels were found to be within normal limits. Final histopathologic examination revealed nodular hyperplasia with no evidence of cancer.
Discussion
When a significant enlargement of the thyroid occurs, it tends to start either as discrete adenomas of the thyroid or as multiple adenomatous goitres that tend to be slow growing and may be present for years before they come to the attention of the physician.2 The thyroid can gradually descend in a downward direction since it is bound by the fascial planes in all directions except inferiorly. This allows for expansion along the path of least resistance, directly into the superior mediastinum. Hence, Lahey and Swinton described the neck as “a space with no bottom.”5
The consensus regarding the treatment of substernal goitre is that it is best managed surgically since the complications are relatively rare.2,3 Medical management, including suppression with exogenous thyroid hormone, can reduce the size of the gland by 20%–30%.6 However, this tends to be only temporary. Generally, surgery through a cervical incision is a safe option for most intrathoracic goitres and is indicated to relieve the pressure exerted by a long-standing goitre.1–5 Alternatives to surgery, such as sodium iodide-131 can precipitate acute reactions in the elderly that can cause respiratory distress.3
In the event that the transcervical surgical approach fails, median sternotomy may be done, particularly if thyroid cancer is suspected or the patient is experiencing acute airway compression. Generally, the decision for a more invasive procedure should be made after careful exploration of the neck and complete exposure of the thyroid.
Conclusion
Most intrathoracic goitres can be managed by removal through a cervical incision.1–5 However, in our case, which is unique to the literature, the patient had a true or complete intrathoracic goitre that was causing vascular compression and DVT in the left arm. Thus, a sternotomy was indicated in order to visualize the anatomy of the mediastinum so fatal complications could be prevented.
Competing interests: None declared.
Accepted for publication Feb. 22, 2008
Correspondence to: Dr. P. Pace-Asciak, Department of Otolaryngology, Gordon & Leslie Diamond Health Care Centre, 4th Floor, 2775 Laurel St., Vancouver BC V5Z 1M9; fax 604 875-5018; piap@interchange.ubc.ca or ppaceasc@hotmail.com
References
- 1.deSouza FM, Smith PE. Retrosternal goiter. J Otolaryngol 1983;12:393-6. [PubMed]
- 2.Netterville JL, Coleman SC, Smith JC, et al. Management of substernal goiter. Laryngoscope 1998;108:1611-7. [DOI] [PubMed]
- 3.Allo MD, Thompson NW. Rationale for the operative management of substernal goiters. Surgery 1983;94:969-77. [PubMed]
- 4.Shaha AR, Alfonso AE, Jaffe BM. Operative treatment of substernal goiters. Head Neck 1989;11:325-30. [DOI] [PubMed]
- 5.Lahey FH, Swinton NW. Intra-thoracic goiter. Surg Gynecol Obstet 1934;59:627-37.
- 6.Newman E, Shaha AR. Substernal goiter. J Surg Oncol 1995;60:207-12. [DOI] [PubMed]