Abstract
Background
The aim of our study was to evaluate the results of lateral tibial plateau fractures treated with arthroscopically assisted percutaneous osteosynthesis (AAPO).
Methods
Twenty-one patients (14 men and 7 women) with a mean age of 41 years underwent AAPO to repair low-energy Schatzker I–III tibial plateau fractures. Under pneumatic tourniquet, we reduced and fixed the fracture with 1 or 2 subchondral cannulated screws. Accompanying lesions included 10 meniscus tears, which we partially excised in 9 patients and repaired in 1 patient. On the second postoperative day, patients began range-of-motion exercises. We encouraged partial and full weight-bearing by the sixth and tenth weeks, respectively. The mean follow-up period was 38 (range 12–96) months, and we evaluated the patients using Rasmussen's clinical and radiologic criteria. We used a t test for statistical analysis.
Results
There were 13 excellent (62%), 6 good (28%) and 2 fair (10%) clinical results, and 11 excellent (52%), 7 good (33%) and 3 fair (14%) radiologic results. We observed mild or moderate arthritic changes in 5 patients (24%). There were no infection or wound problems, but we removed hardware in 4 patients.
Conclusion
Arthroscopically assisted treatment of lateral tibial plateau fractures yields satisfactory results and can be accepted as an alternative and effective method for the treatment of low-energy tibial plateau fractures.
Abstract
Contexte
Notre étude visait à évaluer les résultats de fractures des plateaux tibiaux externes traitées par ostéosynthèse percutanée assistée par arthroscopie (OPAA).
Méthodes
Vingt-et-un patients (14 hommes et 7 femmes) de 41 ans en moyenne ont subi une OPAA afin de réparer des fractures des plateaux tibiaux Schatzker I–III causées par un choc de faible énergie. Après avoir appliqué un tourniquet pneumatique, nous avons réduit et fixé la fracture au moyen de 1 ou 2 vis cannelées sous-chondrales. Les lésions accompagnant la fracture ont inclus 10 déchirements du ménisque, que nous avons excisé en partie chez 9 patients et réparé chez 1 patient. Le 2e jour après l'intervention, les patients ont commencé à effectuer des exercices d'amplitude de mouvement. Nous avons encouragé les patients à supporter une partie et la totalité de leur poids au cours de la 6e et de la 10e semaines respectivement. La période de suivi moyenne s'est établie à 38 (plage de 12 à 96) mois et nous avons évalué les patients au moyen des critères cliniques et radiologiques de Rasmussen. Nous avons utilisé le t test pour effectuer l'analyse statistique.
Résultats
Il y a eu 13 résultats cliniques excellents (62 %), 6 bons (28 %) et 2 moyens (10 %) et 11 résultats radiologiques excellents (52 %), 7 bons (33 %) et 3 moyens (14 %). Nous avons observé des changements arthritiques bénins ou moyens chez 5 patients (24 %). Il n'y avait pas de problème d'infection ou de plaie, mais nous avons retiré du matériel chez 4 patients.
Conclusion
Le traitement des fractures des plateaux tibiaux externes assisté par arthroscopie produit des résultats satisfaisants et peut être accepté comme solution de rechange efficace au traitement des fractures des plateaux tibiaux causées par un choc de faible énergie.
There have been many options for the treatment of proximal tibial fractures in orthopedic literature, including conservative treatment, external fixation, open reduction– internal fixation (ORIF) and arthroscopically assisted percutaneous osteosynthesis (AAPO).1–4 The ultimate goal of the intra-articular fracture treatment should be the precise restoration of the joint surface and stable fixation to allow immediate postoperative non–weight-bearing exercises. The difficulty in achieving precise reduction using conservative methods and the higher morbidity associated with traditional surgical applications have led to the development of semi-invasive techniques.1,5,6 The treatment of tibial plateau fractures with AAPO is one method that is associated with lower morbidity, less extensive surgical dissection and long-term immobilization. Furthermore, arthroscopy allows the surgeon to diagnose and treat concomitant soft-tissue pathologies synchronously.5–8
The aim of our study was to evaluate the results of lateral tibial plateau fractures treated with AAPO.
Methods
Between June 1998 and January 2004, we treated lateral tibial plateau fractures with AAPO in 21 patients (14 men and 7 women). The patients had a mean age of 41 (range 23–77) years. Of the 21 patients, 16 (76%) sustained injuries during motor vehicle collisions and 5 (24%) had work-related injuries. Based on the classification described by Schatzker and colleagues,9 there were 7 type I, 10 type II and 4 type III fractures. None of the fractures was open. The inclusion criterion was low-energy proximal tibial fracture with articular step-off greater than 3 mm, condylar widening greater than 5 mm or varus/valgus instability greater than 10° without coincidental systemic injury. We excluded nondisplaced fractures, Schatzker type IV–VI fractures and fractures with extensive articular comminution from the study. We obtained informed consent from all patients preoperatively.
In the emergency department, we obtained anteroposterior (AP) and lateral radiographs of injured and uninjured knees. In all patients, we obtained 3-dimensional computed tomography (CT) scans to determine the exact fracture pattern and the directions of fracture lines, and to plan preoperatively for the optimal placement of screws and wires. Surgery was delayed until the swelling of extremities subsided, as determined by clinical observation. On average, patients had surgery on the third day after admission to hospital (range 1–7 d). Two authors (C.K and H.Ö.) performed all the surgeries and carried out the follow-up evaluations.
Technique
Before the surgical procedure, we examined the knee to evaluate the ligamentous stability. We performed arthroscopy of the knee joint using standard arthroscopic portals after the inflation of the tourniquet on the radiolucent table. We did not use an arthro pump, and the fluid was introduced with the use of gravity inflow. We established outflow via the arthroscopic cannula sheath to minimize the intra-articular pressure. We irrigated the joint and evacuated blood clots. We reduced split fractures by closed manipulation together with percutaneous pinning using the joystick technique. To treat depressed fractures, we used an anterior cruciate ligament guide to localize the centre of the depressed articular surface and the cortical window. We elevated these fractures through the cortical window using special custom-made impactors under the control of arthroscopy. In patients with type II and type III fractures, we filled the defect with cortico-cancellous allograft. We fixed the fracture with 6.5-mm cannulated screws under the control of C-arm fluoroscopy. After fracture fixation, we examined the intra-articular soft tissues. We repaired accompanying peripheral lateral meniscus tears using the inside-out technique in 1 patient, and we partially excised the torn menisci in 9 patients. We placed suction drains in the joint and closed the wound. The mean duration of surgery was 89 (range 58–115) minutes.
We used first-generation cephalosporin for antibiotic prophylaxis for 24 hours, starting just before the administration of anesthesia. After we removed the drain, patients began active quadriceps exercises. All patients used a continuous passive motion device until they were discharged from hospital. We recommended that patients refrain from weight-bearing activity and that they use hinged knee braces after the edema resolved and the wound healed. The average length of say in hospital was 7 (range 4–14) days. We encouraged partial and full weight-bearing by the sixth and tenth weeks, respectively.
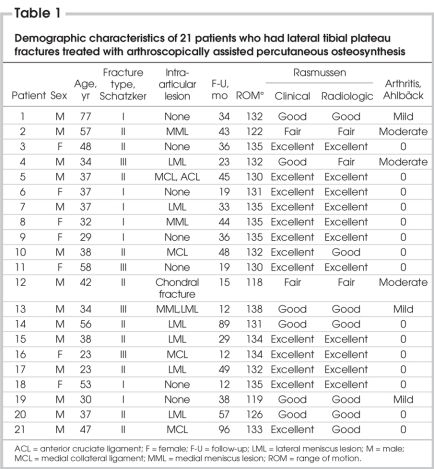
Patient follow-up occurred in 6-week intervals at the outpatient clinic. We examined patients clinic-ally and radiologically in the first 6 months after surgery (Fig. 1, Fig. 2, Fig. 3). The average follow-up period was 38 (range 12–96) months. We determined union clinically by painless palpation. At the last follow-up visit, we evaluated the patients clinically and radiologically using the criteria recommended by Rasmussen.10 We estimated the severity of osteoarthritis based on the narrowing of joint space, as described in a study by Ahlbäck.11 A mild degree was a relative narrowing less than 50%, a moderate degree was a narrowing greater than 50% and a severe degree was when the joint was completely obliterated (Table 1). We asked patients whether they were satisfied or unsatisfied with the intervention.

FIG. 1. Preoperative anteroposterior radiograph of a 58-year-old woman with a type III fracture.

FIG. 2. Early postoperative anteroposterior radiograph showing sufficient reduction after the defect was filled by graft and strengthened by a screw.

FIG. 3. Anteroposterior radiograph obtained 19 months after surgery, showing an excellent result.
Table 1
Statistical analysis
We used the t test for statistical analysis, and we considered results of p < 0.05 to be statistically significant.
Results
We achieved union in all patients without any additional procedure. We found no ligamentous instability at the last follow-up visit. The mean range of motion in the injured knee was 131° (range 118°–135°) compared with a range of motion of 136° (range 135°–140°) in the noninjured knee. We observed no statistical difference in the range of motion between both sides (p > 0.05).
Of the 21 patients, 14 (67%) had associated intra-articular soft tissue lesions, and 9 had meniscus lesions (2 medial, 6 lateral and 1 both). Owing to the detachment of meniscosynovial junction, 1 of the lateral meniscus lesions required repair using the inside-out technique with polydioxanone suture. We partially resected the other meniscus lesions. In addition, there were 4 mild-degree medial collateral ligament lesions and 1 partial anterior cruciate ligament lesion in 4 patients, which we treated conservatively. One patient had a chondral fracture on the lateral femoral condyle, which we treated with abrasion chondroplasty.
We determined osteoarthritis according to the study by Ahlbäck.11 We observed no severe osteoarthritis. We detected mild changes in 3 patients (14%) and moderate changes in 2 patients (10%). Work and recreational activities were affected to a minor degree for these patients. There were no complications, including infection, compartment syndrome or deep vein thrombosis, directly associated with the arthroscopy. However, in 4 patients, we removed the screws after the fracture healed owing to skin irritation. We performed these procedures at least 1 year after the initial surgery.
All the patients were satisfied with the treatment. Based on the criterion described by Rasmussen,10 there were 13 excellent (62%), 6 good (28%) and 2 fair (10%) clinical results, and 11 excellent (52%), 7 good (33%) and 3 fair (14%) radiologic results. We observed that fair radiological results were associated with a loss of reduction of no more than 3 mm in 2 patients with type II and type III fractures. The third patient had a type II tibial plateau fracture and a chondral fracture preoperatively that resulted in a fair outcome.
Discussion
The major risk of proximal tibia fractures is osteoarthritis related to either instability due to varus/valgus deformity or incongruence of the joint surface. For this reason, tibial plateau fractures require anatomic reduction of articular surfaces, restoration of axial alignment and stable fixation, allowing immediate active and passive exercises to obtain satisfactory results. In whichever way the fractures are treated, the ultimate goal of the treatment should be to preserve the normal range of motion in the knee.12–14
Generally, operative treatment is advised for fractures with articular step-off and/or separation more than 3–5 mm and varus/valgus instability more than 10°.6,15
Traditional surgery, including open reduction and internal fixation, has yielded adequate results with extensive surgical dissection.2,16 Moreover, in some cases, trans-section of menisci has been reported to achieve the required articular vision. Arthrotomy is the main component of this technique, and problems secondary to arthrotomy such as prolonged stiffness, increased pain and wound complications can be observed.1,15,16
Arthroscopically assisted percutaneous fixation, which was first recommended by Caspari17 and Jennings,18 has gradually become popular since its initial use as a diagnostic tool. The advantages of AAPO include the direct vision of the intra-articular fracture, a more accurate reduction, lower morbidity compared with ORIF, better assessment and immediate treatment of intra-articular soft tissue lesions, prevention of soft-tissue complications and the possibility of washing out the joint content, including chondral debris and hematoma.3,7,19,20 Fowble and colleagues1 reported that the results of the arthroscopic treatment were superior to ORIF. They pointed out that there was a higher percentage of anatomic reduction, lower rates of complication and a shorter delay to full weight-bearing among patients who underwent AAPO than among those who had ORIF.
Ohdera and colleagues21 reported no difference in the duration of surgery, the range of motion in the knee and clinical results between patients who had AAPO and those who had ORIF; however, they noted faster and easier rehabilitation among those who had AAPO. Lubowitz and colleagues22 reported that AAPO of selected tibial plateau fractures allows anatomic reduction and rigid internal fixation with less morbidity than ORIF.
It was reported that not all plateau fractures are amenable to AAPO. Schatzker type V and VI fractures, called high-energy fractures, are associated with a potential risk of compartment syndrome resulting from fluid extravasation.6,12,19 Tornetta19 insisted that AAPO, a very technically demanding procedure that requires a certain level of expertise to perform, is best used in low-energy Schatzker type I, II and III fractures. However, Chan and colleagues23 reported that arthroscopically assisted reduction and bilateral plate fixation of 18 complex tibial plateau fractures resulted in 89% satisfactory results according to Rasmussen's system. Furthermore, they reported no important complications related to compartment syndrome, though lateral paresthesia occurred in 2 patients. To prevent compartment syndrome, the use of only the gravity inflow and adequate outflow technique via the cannula sheath is recommended.12,15,23
Based on Rasmussen's clinical and radiologic criteria, we obtained satisfactory results (90% excellent and 86% good). We observed mild or moderate osteoarthritis in 5 patients (24%). These results are comparable with other series. Scheerlinck and colleagues14 reported 92% satisfactory rates that demonstrated a joint line narrowing rate of 28.9%. Hung and colleagues15 found 93.5% satisfactory results according to the Hospital for Special Surgery Knee Score.
The concomitant intra-articular soft-tissue injury rate has been reported to be between 52% and 72%.15,23–25 In our study, 14 patients (67%) had soft-tissue lesions. Both observation and immediate repairing of the intra-articular soft-tissue injuries can be regarded as one of the main advantages of AAPO.
All the fractures healed without angular deformity or ligamentous laxity. In addition, we observed no complications, including infection or compartment syndrome, related to arthroscopy.
In conclusion, AAPO can be accepted as an effective, semi-invasive surgical method with a low rate of complication for the treatment of Schatzker type I, II and III tibial plateau fractures.
The preliminary result of this study was presented as a poster presentation at the 7th congress of the European Federation of National Associations of Orthopaedics and Traumatology (EFORT), June 4–7, 2005, in Lizboa, Portugal.
Contributors: Drs. Kayali, Öztürk and Agus designed the study. All authors acquired the data, which Drs. Kayali and Agus analyzed. Drs. Kayali, Öztürk, Altay and Agus wrote the article, which Drs. Drs. Kayali, Öztürk, Reisoglu and Agus reviewed. All authors gave final approval for publication.
Competing interests: None declared.
Accepted for publication Apr. 24, 2007
Correspondence to: Dr. C. Kayali, 6445 sokak No: 10 D:4, 35550 Karsiyaka Izmir / Turkey; fax 90 232 433 07 56; cemilkayali@yahoo.com
References
- 1.Fowble CD, Zimmer JW, Schepsis AA. The role of arthroscopy in the assessment and treatment of tibial plateau fractures. Arthroscopy 1993;9:584-90. [DOI] [PubMed]
- 2.Karas EH, Weiner LS, Yang EC. The use of an anterior incision of the meniscus for exposure of tibial plateau fractures requiring open reduction and internal fixation. J Orthop Trauma 1996;10:243-7. [DOI] [PubMed]
- 3.Ruth JT. Fractures of the tibial plateau. Am J Knee Surg 2001;14:125-8. [PubMed]
- 4.Sirkin MS, Bono C, Reilly M, et al. Percutaneous fixation of tibial plateau fixation. Clin Orthop Relat Res 2000;375:60-8. [DOI] [PubMed]
- 5.Handelberg FWJ, Scheerlink T, Casteleyn PP. Fractures of the upper tibia and arthroscopic techniques. Tech Knee Surg 2003;2:109-16.
- 6.McClellan RT, Comstock CP. Evaluation and treatment of tibial plateau fractures. Curr Opin Orthop 1999;10:10-21.
- 7.van Trommel MF, Simonian PT, Potter HG, et al. Arthroscopically-aided lateral meniscal repair and reduction of lateral tibial plateau fracture: long-term follow up with MR imaging. Knee 1998;5:241-4.
- 8.Asik M, Cetik O, Talu U, et al. Arthroscopy-assisted operative management of tibial plateau fractures. Knee Surg Sports Traumatol Arthrosc 2002;10:364-70. [DOI] [PubMed]
- 9.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture: the Toronto experience 1968–1975. Clin Orthop Relat Res 1979;138:94-104. [PubMed]
- 10.Rasmussen PS. Tibial condylar fractures: impairment of knee joint function as an indication for surgical treatment. J Bone Joint Surg Am 1973;55:1331-50. [PubMed]
- 11.Ahlback S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Diagn (Stockh) 1968;(Suppl 277):7-72. [PubMed]
- 12.Guanche CA, Marman AW. Technical notes. Arthroscopic management of tibial plateau fractures. Arthroscopy 1993;9:467-71. [DOI] [PubMed]
- 13.Houben PFJ, Linden ES, Wildenberg FAJM, et al. Functional and radiological outcome after intra-articular tibial plateau fractures. Injury 1997;28:459-62. [DOI] [PubMed]
- 14.Scheerlinck T, Ng CS, Handelberg F, et al. Medium-term results of percutaneous, arthroscopically-assisted osteosynthesis of fractures of the tibial plateau. J Bone Joint Surg Br 1998;80:959-61. [DOI] [PubMed]
- 15.Hung SS, Chao EK, Chan YS, et al. Arthroscopically assisted osteosynthesis for tibial plateau fractures. J Trauma 2003;54:356-63. [DOI] [PubMed]
- 16.Stevens DG, Beharry R, McKee MD, et al. The long-term functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma 2001;15:312-20. [DOI] [PubMed]
- 17.Caspari RB, Patrick MJ, Hutton TL, et al. The role of arthroscopy in the management of tibial plateau fractures. Arthroscopy 1985;1:76-82. [DOI] [PubMed]
- 18.Jennings JE. Arthroscopic management of tibial plateau fractures. Arthroscopy 1985;1:160-8. [DOI] [PubMed]
- 19.Tornetta P. Arthroscopic elevation with grafting. J Orthop Trauma 2002;16:444-6. [DOI] [PubMed]
- 20.Muezzinoglu US, Guner G, Gurfidan E. Arthroscopixally assisted tibial plateau fracture management: a modified method. Arthroscopy 1995;11:506-9. [DOI] [PubMed]
- 21.Ohdera T, Tokunaga M, Hiroshima S, et al. Arthroscopic management tibial plateau fractures – comparison with open reduction method. Arch Orthop Trauma Surg 2003;123:489-93. [DOI] [PubMed]
- 22.Lubowitz JH, Elson WS, Guttmann D. Current concepts part I: arthroscopic management of tibial plateau fractures. Arthroscopy 2004;20:1063-70. [DOI] [PubMed]
- 23.Chan YS, Yuan LJ, Hung SS, et al. Arthroscopic-assisted reduction with bilateral buttress plate fixation of complex tibial plateau fractures. Arthroscopy 2003;19:974-84. [DOI] [PubMed]
- 24.Honkonen SE. Degenerative arthritis after tibial plateau fractures. J Orthop Trauma 1995;9:273-7. [DOI] [PubMed]
- 25.Tscherne H, Lobenhoffer P. Tibial plateau fractures. Management expected results. Clin Orthop Relat Res 1993;(292):87-100. [PubMed]