SYNOPSIS
Objective
We examined patterns of enrollment, use, and frequency of use in school-based health centers (SBHCs), as well as the referral, diagnosis, and disposition of SBHC visits among newly implemented SBHCs.
Methods
Four rural and four urban school districts implementing SBHCs were examined from 2000 to 2003. Total school enrollment for students was 13,046. SBHC enrollment and medical encounter data were tracked using a Web-based medical database. Descriptive analyses were conducted to evaluate primary care access and utilization patterns.
Results
A total of 7,460 (57.2%) students were enrolled in their SBHCs, of which 4,426 used the SBHC at least once for a total of 14,050 visits. SBHC enrollment was greater in urban districts but rate of utilization was higher in rural districts. Black students, students with public or no health insurance, and students with asthma or attention deficit disorder had higher enrollment and utilization. Rural parents referred more children to SBHCs than urban parents. Teachers referred more students who were black, had asthma, had no public or health insurance, or had acute-type health issues. Total visits increased during the three years, with the largest increase in mental health services. Students who were younger, white, attended rural schools, had public or health insurance, or had infections were more likely to be sent home. Those with chronic conditions and visits for mental health were more likely to be returned to class.
Conclusion
Utilization patterns suggest improved access to needed health care for disadvantaged children. SBHCs are an important part of the safety net for the populations they are intended to serve.
The National Assembly on School-Based Health Care (NASBHC) Census from 2004–2005 reports a total of 1,709 school-based health centers (SBHCs) in the U.S.,1 but this number still covers only a percentage of the 13 million children living in poverty and eight million additional children living without health insurance.2 While the SBHC model has not yet received widespread recognition and support,3 it stems from the assumption that service delivery in schools improves access and overall health among children, especially for those with the greatest need.4–7 There is also evidence that delivery of health care within schools may reduce more expensive types of care, such as emergency room use8–12 and inpatient hospital care.11 This may be a function of increased preventive care including the likelihood of having at least one physician visit and an annual dental examination.10
For those who are contemplating the establishment of an SBHC, it is important to have information on access and utilization patterns to better ensure the success of programs through informed program design, implementation, and targeting of services. Existing literature provides some information on access and utilization patterns. In an early study of health-care use among kindergarten through fifth-grade students, Gilman and Nader found the majority of visits for traumas and minor health problems, such as headaches and stomachaches, occurred at school.13 For chronic illnesses, 50% of illness maintenance occurred in the school while 16% occurred in the community, principally at practitioners' offices. However, the majority of acute crises such as severe asthmatic attacks were cared for in the community, while only 31% were cared for in schools. Baquiran et al. compared frequent and average SBHC users in the Bronx, New York, and found that frequent users were generally older but did not differ by gender, race, or insurance status.14 Frequent users also generated more visits for mental health and chronic conditions, while average users generally visited for preventive care, acute care, and injuries. However, this study did not compare users to nonusers.
In a study of SBHC visits for underserved Hispanic elementary students in Denver, the most prevalent diagnostic categories were preventive health including health screening, immunizations, and physical examinations (57.0%), followed by acute physical health problems including respiratory problems, ear infections, skin problems, and symptoms (56.9%).15 In an established SBHC serving a disadvantaged community in Atlanta, where 98.0% of the student population qualified for free or reduced lunch, five-year usage rates were highest for respiratory problems followed by health supervision, skin problems, and symptoms (i.e., abdominal and chest pain, cough, and headache).16 They found that students with asthma had lower rates of usage while those with emotional diagnoses had higher rates of usage, concluding that a high proportion of services provided by SBHCs would focus on mental health issues.
While these studies focused on urban centers, there is also evidence that SBHCs can increase service use in suburban and rural populations.17 For example, Crespo and Shaler identified higher rates of enrollment and utilization in rural SBHCs compared with urban SBHCs in West Virginia.18,19 But whether these differences were a function of differential access to health care outside of school or other factors such as differences in health insurance remains unclear.
This study addresses four issues regarding SBHC access and utilization to better inform the design and targeting of services. First, it explores how student enrollment and utilization patterns vary across urban and rural schools, student characteristics, insurance status, and chronic health conditions. For example, do children with and without health insurance or with chronic illnesses utilize SBHCs at different rates? Second, it identifies sources of referrals of students to SBHCs for services and examines whether referral sources differ across student characteristics and presenting health conditions. Third, it assesses the most frequent resulting diagnoses for visits and examines how these may evolve over time. Fourth, it examines factors associated with whether children are being sent back to class or being dismissed after an SBHC visit. These issues are addressed through data collected on students enrolled in eight elementary and middle school districts with SBHCs.
METHODS
Sample
This study includes eight school districts or subdistricts that implemented new SBHCs in the 2000–2001 school year, of which four were rural and four were urban. Three urban school districts and one rural school district were located in Southwestern Ohio while three rural school districts and one urban school district were located in Northern Kentucky. Characteristics and service delivery models of each SBHC as well as any change in the models over the three years reflect a wide variety consistent with the NASBHC Census.1,7,20,21 (A detailed look at the characteristics and service profiles of SBHCs across the first three years of implementation is available on the Health Foundation of Greater Cincinnati's website at http://www.healthfoundation.org/sbhcstudy.html.) Each SBHC was open from Monday through Friday and operated during the school year from September through May. Any medical request during the weekend was directed to either a neighborhood health center or other primary care physicians. Five of the SBHCs served only kindergarten through eighth grade, while three also served high school students. All SBHCs were linked to a health provider, and SBHC staff included at least one on-site nurse practitioner (NP) and a collaborating physician who may or may not have been on-site for any time. The presence of other on-site staff varied across SBHCs. For example, six of the eight SBHCs had a social worker/counselor on-site at least on a part-time basis for mental health services, while only one SBHC had a dentist on-site.
Services provided on-site by all SBHCs included episodic care and well-child checks, but other types of services including preventive services, dental services, chronic condition counseling, behavioral and mental health assessments, and classroom education varied in their on-site provision. For example, one site was established as a school-linked health center with its primary goal to link students with primary care practitioners within the community, while another site provided full on-site preventive, education, dental, behavioral, and mental health services. Finally, there were also variations in billing practices including fee-for-service, insurance filing, and co-pays, with some SBHCs not billing at all during the three-year period, some implementing billing in the second or third year, and others billing right at implementation.
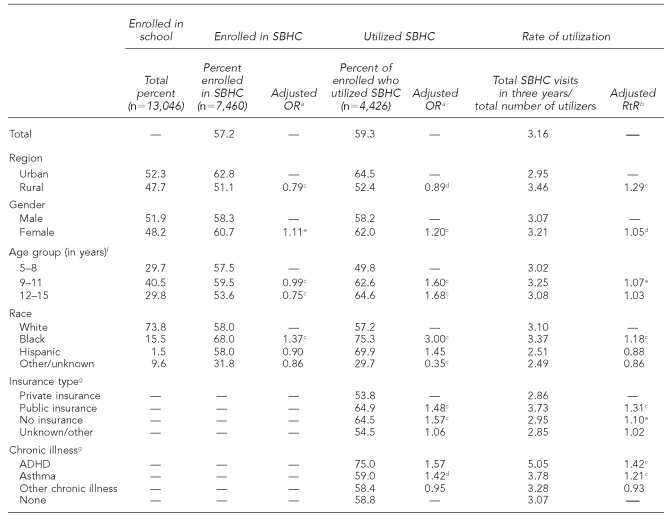
The analysis included students from age 5 (kindergarten) to 15 (grade eight). The total number of students attending the eight SBHC school districts who were eligible for enrollment was 13,046 (Table 1). To be enrolled in the SBHC, parents were provided an enrollment/consent form in their school package at the beginning of any of the three school years (2000–2001, 2001–2002, and 2002–2003). If parents did not complete the enrollment form at the beginning of each school year, verbal consent to treat was sought if the student presented to the SBHC for a health problem during the school year. In addition to providing parental consent for the SBHC to treat, the enrollment form collected information about student demographics, health insurance coverage, primary care physician contact, prescribed medication use, and the presence of specific chronic conditions.
Table 1. Distribution of students enrolled in and utilizing SBHC services and rates of utilization.
aOR adjusted for all other variables presented in Table.
bRtRs adjusted for all other variables presented in Table.
cp<0.001
dp<0.05
ep<0.01
fAge group is based on first-year record for student.
gThe percentage of students with data on insurance status and chronic illness used as the denominator to calculate utilization was based only on those students enrolled at the beginning of the school year (n=6,474), as this information was extracted directly from the completed and signed parent SBHC enrollment form.
SBHC = school-based health center
OR = odds ratio
RtR = rate ratio
ADHD = attention deficit hyperactivity disorder
Data collection
All demographic and encounter data across all eight SBHCs were tracked using the same online database (Health Management—Welligent).22 This database was developed and maintained by the health informatics researchers at the Center for Pediatric Research in Norfolk, Virginia. Annual student enrollment and demographic information (including student age, gender, race, and grade) updates were sent to Welligent from each school district information technology department. Information from the parent-completed SBHC enrollment forms—including health insurance information, SBHC consent form, presence of any chronic illness, medications, and primary care physician—was entered by SBHC staff into the online Welligent database. In the case of parental verbal consent to treat during the year among students who did not have a completed enrollment form, enrollment data were often missing. In addition to enrollment information, all SBHCs entered details of each SBHC student health encounter including referral source, presenting health problem, International Classification of Diseases, Ninth Revision (ICD-9) diagnosis code, and whether the child returned to class or was dismissed.
Measures
Enrollment in the SBHC was defined as having a completed enrollment form or verbal permission from a parent or guardian to provide service. These data were entered into the Welligent database. Users were defined as those students who had one or more documented visits to the SBHC as captured by Welligent. Utilization was measured as the number of SBHC visits entered into Welligent with rates of utilization calculated using the total number of visits as the numerator divided by the number of users (students who were enrolled and had at least one visit).
Referral source was collected in Welligent with check-box options to indicate teacher, parent, school nurse, self, or other. In some schools, the school nurse operated independently of the SBHC and would serve as a source of referral. SBHC visit diagnoses were added into Welligent using ICD-9 codes. ICD-9 codes were then collapsed into two sets of groupings: 18 general disease categories and 30 specific diagnoses, including infections, mental health, nervous system, respiratory, and injuries/poisonings. Details on the diagnostic categories are available on the Health Foundation of Greater Cincinnati's website at http://www.healthfoundation.org/sbhcstudy.html. Visit disposition was entered into Welligent again using check boxes to indicate whether the child was sent back to class or dismissed and sent home. All Welligent data entries were inspected and cleaned by the SBHC research staff to ensure accuracy and consistency of data entry among the individual SBHCs.
Analysis
All analyses were conducted using SAS® 8.2.23 The analysis proceeded in two parts. First, using the individual student as the unit of analysis (n=13,046), we examined SBHC enrollment trends, utilization patterns, and rates of utilization across urban and rural districts, as well as student characteristics including gender, race, age, health insurance type, and specific chronic illnesses. Information on both health insurance status and chronic health conditions was collected from the SBHC student enrollment forms, preventing any assessment as to whether the likelihood of enrollment was differentially distributed across insurance or chronic health problems. However, once enrolled, we were able to examine differences in SBHC use. Likelihood of enrollment and likelihood of utilization were both examined using PROC LOGISTIC (descending) producing odds ratios (ORs). Rate of utilization was examined using PROC GENMOD specifying a Poisson distribution of the dependent variable producing a rate ratio (RtR) predicting the likelihood of each additional visit. All ORs and RtRs were fully adjusted for all other variables in the table.
Second, using the SBHC visit as the unit of analysis (n=14,050), we employed a contingency table analysis to examine the three components of each visit—referral source, SBHC visit diagnoses, and visit disposition. Using a standard test of overall significance (Chi-square at p<0.001), comparisons identified differences across year, region, gender, age group, race, insurance status, and chronic illness. For referrals and outcomes, we also included the general diagnostic category as a predictor.
RESULTS
Student SBHC enrollment and utilization
Across the three school years (2000–2001, 2001–2002, and 2002–2003) and the eight school districts, 13,046 students were eligible to be enrolled in an SBHC, of which 7,460 (57.2%) were enrolled. Of those enrolled, 4,426 (59.3%) used the SBHC at least once in the three-year period. The total number of health encounters among students who utilized the SBHC was 14,050, with a mean of a little more than one visit per year (3.16 visits per user) (Table 1). Adjusting for other factors, urban students were significantly more likely than rural students to be enrolled in an SBHC (OR=1.27) and more likely to have used the SBHC at least once (OR=1.12). However, rural students had a significantly higher rate of utilization if they accessed the SBHC (RtR=1.29).
Girls were significantly more likely to be enrolled (OR=1.11) and to utilize (OR=1.20) the SBHC, and they also had a higher rate of utilization (RtR=1.05). Age was categorized to compare primary, senior elementary, and middle school students (kindergarten to third grade, grades four to six, and grades seven to eight). Likelihood of enrollment was lower among older age groups, but if enrolled, the older cohorts were more likely to utilize the SBHC than the younger groups. A significantly greater percentage of black students were enrolled compared with white students (OR=1.37). Black students were also more likely to utilize the SBHC (OR=3.00) and had a significantly higher rate of usage than white students (RtR=1.18). Among those enrolled in the SBHCs, those with public insurance or no health insurance were more likely to use the SBHC (OR=1.48 and 1.57, respectively) and had higher rates of utilization (RtR=1.31 and 1.10, respectively) compared with students who had private health insurance.
Of the 7,460 children enrolled, only 6,474 students had a fully completed enrollment form. Of the 6,474, only 676 (10.4%) were identified by the parent as having specific chronic health conditions. Of the 676 identified in the SBHC encounter tracking system, only 433 had utilized the SBHC. But among those students with a documented chronic condition who used the SBHC, those with a parent-reported diagnosis of attention deficit hyperactivity disorder (ADHD) had a greater utilization rate (RtR=1.42) than children without a chronic health condition. Students with parent-reported asthma were both more likely to utilize the SBHC (OR=1.42) and use it more often (RtR=1.21) than children with no parent-reported chronic illness.
SBHC visit referrals
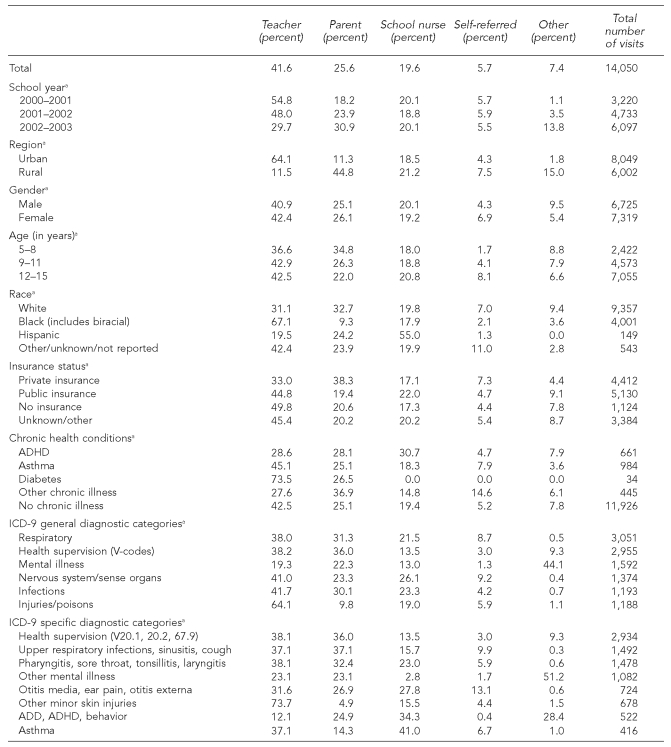
Almost half of all SBHC visit referrals came from teachers (41.6%) (Table 2). Parent/family referrals made up 25.6% of all referrals, and other school health personnel (principally the school nurse) accounted for 19.6% of referrals. Self-referrals by the student comprised 5.7% of all SBHC student health encounters. Other referrals included counselors, school administration, other students, and social workers.
Table 2. SBHC visit referral patterns by year, region, student sociodemographics, insurance status, chronic health conditions, and medical diagnoses.
ap<0.001
SBHC = school-based health center
ADHD = attention deficit hyperactivity disorder
ICD-9 = International Classification of Diseases, Ninth Revision
ADD = attention deficit disorder
While the absolute numbers of referrals increased for every group from year one to year three, the referrals by teachers as a percentage of the total declined coinciding with an increased percentage of referrals by parents. Parents were more likely to refer younger children, while older children were more likely to present on their own. Black students were more likely to be referred by teachers, while white students were more likely to be referred by parents. Those with no health insurance or public insurance were more likely to be referred to the SBHC by their teachers compared with students who had private health insurance.
The most prevalent general diagnostic categories were respiratory (i.e., pharyngitis and upper respiratory), health supervision (V-codes including well-child checks, follow-up visits, and ADHD maintenance), mental disorders, nervous system/sense organs, injuries/poisons, and infections. For specific diagnostic categories, the most prevalent categories were health supervision, upper respiratory infections, pharyngitis, other mental illness, otitis media, minor skin injuries, ADHD, and asthma. Teachers referred the greatest percentage of SBHC encounters in the injury/poisoning (64.1%) and minor skin injuries (73.7%) categories. For other ICD-9 general and specific categories, teachers and parents referred similar percentages with the exception of nervous system and asthma as well as ADHD/attention deficit disorder (ADD), where parents referred a greater proportion. For the three categories of mental illness (general mental illness, other mental illness, and ADHD/ADD), there was also a high percentage of referrals from school nurses and others which, upon further inspection, comprised principally counselors and social workers. The largest percentage of self-referrals was for otitis media (13.1%).
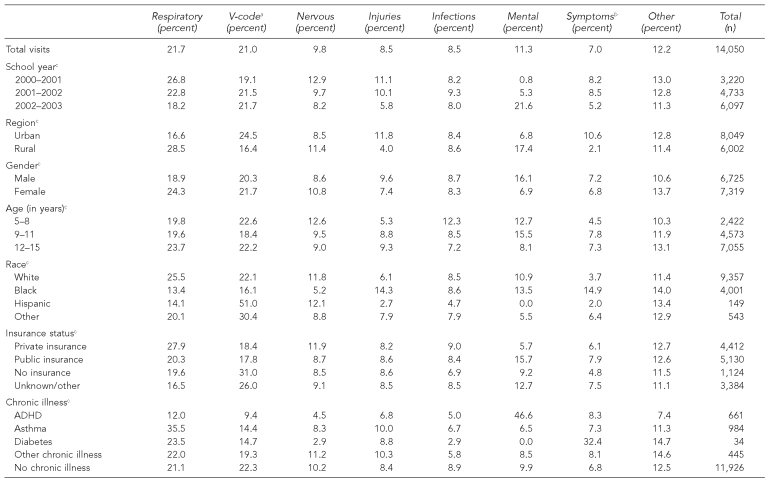
SBHC medical encounters by ICD–9 general diagnostic categories
In terms of absolute numbers, overall visits increased substantially across all diagnostic categories from year one to year three. The largest ICD-9 general categories for SBHC visits were for respiratory and V-codes (e.g., physicals, follow-ups, and wellness checks). There was a substantial increase in mental health visits in year three and a corresponding reduction in the relative percentage of visits for respiratory, nervous system/sense organs, injuries, and symptoms (Table 3).
Table 3. Most prevalent ICD-9 general diagnostic categories by year, region, student sociodemographics, insurance status, and chronic health conditions (n=14,050).
aV-codes include visits for follow-up exams, well-child checks, and routine child checks.
bSymptoms include transient conditions and ill-defined conditions in which no diagnosis classification can be made.
cp<0.001
ICD-9 = International Classification of Diseases, Ninth Revision
ADHD = attention deficit hyperactivity disorder
Students in rural schools had a greater percentage of visits for respiratory, nervous system, and mental health visits, while urban students had a higher percentage of visits for V-codes such as health checks and follow-ups. Girls had more visits for respiratory problems while boys had more visits for mental health issues. Older children had a higher percentage of visits for respiratory and injury/poisoning. Younger children had a higher percentage of visits for nervous system/sense organ-related issues and infections. White students had a greater percentage of visits for respiratory problems, black students had a higher percentage of visits for injuries and symptoms, and Hispanic children had a high percentage of V-code visits. Those with private health insurance had a greater percentage of visits for respiratory problems while those with public insurance had more visits for mental health issues. Those without health insurance had the highest percentage of V-code visits for health maintenance. Finally, among students who had parent-reported chronic conditions, the majority of their SBHC visits appeared to align with their specific conditions. For example, students with asthma had a high proportion of visits for respiratory issues while students with ADHD had a high proportion of visits for mental health issues. However, all students with parent-reported chronic conditions also had diagnosis patterns similar to their non-chronically ill peers, suggesting they were using the SBHC for general health issues as well as issues related to their chronic condition.
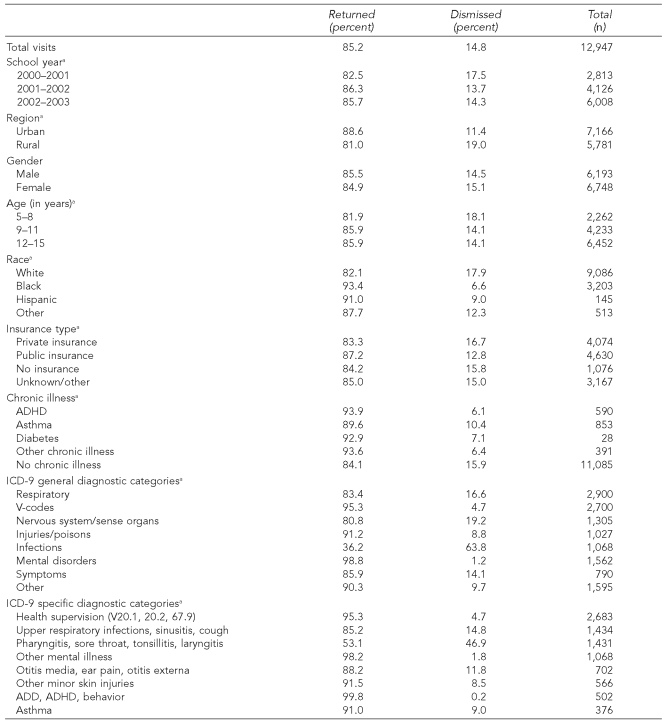
SBHC end-of-visit outcomes
Of the 14,050 SBHC visits, outcome data were available on whether students were returned to class or dismissed from school for 12,947 (92.1%) visits. The remaining visits were documented as “other outcomes” and described by individual text entries in Welligent (2.2% of visits) or had no outcome data entered (5.6% of visits). Among the 12,947 student SBHC encounters, students were returned to class 85.2% of the time, and this percentage steadily increased from year one to year three (Table 4). Only 14.8% of all cases were dismissed from school. Students who were more likely to be dismissed and sent home were younger, attending rural schools, white, or had public insurance. Among children with chronic illnesses, those with asthma had the highest dismissal rate, but this was significantly lower than the dismissal rate of children with no chronic illness. As would be expected, diagnoses were related to visit outcomes. Students with infections were least likely to return to class (36.2%) while those with ICD-9 codes indicating mental health were returned to class 98.8% of the time.
Table 4. SBHC visit disposition by year, region, student sociodemographics, insurance status, chronic health conditions, and medical diagnoses.
NOTE: Of the 14,050 total SBHC visits, outcome data on whether students were returned to class or dismissed from school were available for 12,947 visits.
ap<0.001
SBHC = school-based health center
ADHD = attention deficit hyperactivity disorder
ICD-9 = International Classification of Diseases, Ninth Revision
ADD = attention deficit disorder
DISCUSSION
This study profiled the characteristics of children who use SBHCs as well as the characteristics of the SBHC visit, including how students get referred for services, the usual visit diagnoses, and the visit disposition. Among the eight SBHCs in this study, in their first three years of operation, the mean number of visits among students using the SBHC was a little more than one per year. Consistent with previous work, enrollment and utilization were differentially skewed to favor students who traditionally have poorer access to customary medical services—those students who are generally targeted by these initiatives.1,4–7 In this study, students with public health insurance or no health insurance were more likely to utilize the SBHC and had significantly higher rates of utilization compared with students who had private insurance, suggesting improved access for these disadvantaged groups. The higher likelihood of SBHC enrollment, SHBC use, and frequency of SBHC use among black students compared with white students further supports this notion, as race is commonly used as a proxy measure for social disadvantage.24
Rural students had lower overall enrollment rates. But if they used the SBHC, their utilization rate was higher than urban students, which is consistent with previous findings that also found higher rates of use in rural areas.17,18 The findings in this study suggest that utilization in rural communities may be less dependent on insurance status as an overall lack of access to health-care services in their community. This is further supported by the findings that rural students had a significantly greater percentage of visits for acute illnesses and mental health issues compared with urban students. As such, if the family recognizes and accepts the SBHC as a provider for health care for their child, the SBHC may compensate for reduced availability of health services in their local rural community. Because only 27% of all SBHCs serve rural populations,1 supporting and expanding their use in rural districts may provide a viable policy solution for lawmakers who are looking to increase access in rural, medically underserved communities.
Not only does it appear that SBHCs may reduce barriers to access for disadvantaged groups and rural populations, they may also provide improved access for children with chronic health problems.13–15,25 In this study, students with chronic conditions used the SBHC for issues related to their specific chronic health condition as well as general health issues. Those with asthma had high rates of SBHC use for respiratory issues as expected, but also had a number of visits for other ICD-9 categories similar to other students. Those with ADHD had high rates of use for mental health services but also had visits for other services.
This overall patterning across groups is consistent with previous research suggesting that SBHCs may compensate for the inadequate community availability of services for disadvantaged children, children in rural areas, and children with chronic illnesses.26–28 Moreover, they may reduce school absence for health visits among these groups that should have positive scholastic benefits.29,30 Providing services on-site for chronically ill children resulted in SBHC utilization rates and class return rates that were equal to or higher than those for students without chronic conditions. For parents, the SBHC may partially relieve them of their substantial burden of care for children with chronic health conditions that likely require more time off work to take children to appointments for illness maintenance. While these SBHCs may not be the primary care provider due to their seasonal nature or operation during school hours only, they can function as a coordinated medical home with the primary care provider for most chronically ill children.3 The SBHC can monitor and ensure proper maintenance regimes for the child, reducing more expensive, acute care.8,9,31 In fact, Guo et al. found that two different subsets of chronically ill children enrolled in Medicaid with access to an SBHC—one set with asthma and one set with mental health problems—had lower hospitalization and emergency room costs than Medicaid-enrolled children with no SBHC access.9,31
For children with public health insurance or no health insurance as well as students in rural communities, community-based health services can be more difficult to access due to their unavailability and parental constraints. Among socially and economically disadvantaged families, parents who are likely in lower-paying jobs with less freedom and autonomy would not have the ability or flexibility in their work schedule to take time off to bring their child to the doctor for health problems. This would be compounded if their child had a chronic health condition requiring additional care. Time away from school and work for rural families is increased further due to the necessity of traveling to urban areas for some care. Because many needs can be attended to at the SBHC, the center and school may provide added support for these parents. Additionally, for families that have no employer-provided health insurance benefits, the SBHC may provide services such as well-child checks that the child might not otherwise receive due to cost barriers. For disadvantaged children, higher SBHC usage and higher class return rates support this argument. It was interesting, however, that rural students had a lower rate of class return after visits. This may be due to their higher percentage of visits for acute infectious care diagnoses such as pharyngitis that require students to be sent home.
Finally, the high number of teacher referrals during the three years, as well as the high percentage of referrals relative to parents in the first year, may indicate a perception by teachers of the SBHC's capacity to address pressing student health issues.32 Because teachers are with the students every day, they are in an excellent position to identify problems at an earlier stage and draw upon the available resources. Whether they would make these referrals without the presence of an SBHC is unknown. However, because teachers were more likely to refer students who were urban, black, or without private health insurance, they may have been less likely to identify and address some issues prior to the implementation of an SBHC because of the lack of family resources and community-based services to address any issue. The decreasing proportion of teacher referrals during the three years combined with the increased proportion of parent referrals may be an indication of a growing parental awareness and acceptance of SBHCs as a health resource for their children. Without the support of the SBHC and teachers, parents might be reluctant or unable to initiate treatment for a variety of reasons.
For example, during the three years, the largest increase in the number of visits to SBHCs was for mental health services. In fact, mental health visits accounted for less than 1% of visits in year one but almost 22% of visits in the final year. Moreover, the percentage of referrals by parents for mental health problems as identified by ICD-9 groupings was significantly higher than by teachers. As such, the SBHC may be an ideal venue to better identify, assess, and treat mental health-care needs,33,34 deal with barriers such as stigma and compliance,20 and promote an interdisciplinary approach by integrating the delivery of expanded school mental health programs.35
This change over time in services could be a sign of increased acceptance of the SBHC by parents within the community of the SBHCs in their delivery of services. Through their work with students, they can help parents identify needs such as mental health, and expand specific services that are unavailable or largely inaccessible in the community safety net.15,20,36 Moreover, these changes in service delivery over the three years may reflect the newness and maturation of these SBHCs as they evolve from their initial service delivery model and financial constraints to address identified needs. The stability of well-child visits (ICD-9 V-codes) contrasted with the increase in mental health visits over these first three years illustrates this change. Upon opening, a central focus of many of these SBHCs was to deliver primary care services and well-child checks but, as discussed previously, the models evolved to address other areas of identified need such as mental and dental health, where identification of the need was great and access for these services in the community was limited or largely unavailable.
Limitations
While this study provides information regarding those who use SBHCs and the reasons for use and visit disposition, there were some limitations. First, we were unable to examine whether overall medical use for these students increased or decreased because we do not have information on previous usage nor on usage outside of the SBHC. As such, we were unable to look at the total health-care utilization profile of these children. Consistent with this, the absence of a comparison group to examine differences in utilization prevented us from inferring that the SBHC changed health-care usage by students compared with those who did not have this access. Finally, there was considerable variability in the structure and staffing across these eight SBHCs consistent with the variability across all SBHCs in their services and staffing models documented by the NASBHC Census.1,20 However, they all have the common goal to provide services to children who may otherwise go untreated, which provides the basis for this analysis.
CONCLUSION
Notwithstanding these limitations, the findings provide additional support to the current assumption that SBHCs provide an important additional component to the safety net of providers improving access to health-care services for the children with the greatest need. Improved access to services through SBHCs as front-line care providers can address several barriers for disadvantaged children, including children with no health insurance or public health insurance, children in rural communities, and children with chronic health conditions, with the goals of improving their health7 and their educational success.37
Acknowledgments
The authors thank the School-Based Health Center Evaluation Project advisory group and staff, the participating school districts, and especially the school-based health centers (SBHCs), their staff, and the students and parents who made this project possible.
Footnotes
This study was funded by the Health Foundation of Greater Cincinnati. Terrance Wade was supported by the Canada Research Chairs Program. Kathryn Keller is an employee of the Health Foundation of Greater Cincinnati, which funded this study and, under its school health initiative, provided start-up funding for the participating SBHCs.
REFERENCES
- 1.Juszczak L, Schlitt J, Moore A. School-based health centers: national census school year 2004–05. Washington: National Assembly on School-Based Health Care; 2007. [Google Scholar]
- 2.Report on school-based health centers. Baltimore: Annie E. Casey Foundation; 2006. [Google Scholar]
- 3.Lear JG. Health at school: a hidden health care system emerges from the shadows. Health Aff (Millwood) 2007;26:409–19. doi: 10.1377/hlthaff.26.2.409. [DOI] [PubMed] [Google Scholar]
- 4.Armbruster P, Gerstein SH, Fallon T. Bridging the gap between service need and service utilization: a school-based mental health program. Community Ment Health J. 1997;33:199–211. doi: 10.1023/a:1025033326743. [DOI] [PubMed] [Google Scholar]
- 5.Dryfoos JG. Safe passage: making it through adolescence in a risky society: what parents, schools, and communities can do. New York: Oxford University Press; 1998. [Google Scholar]
- 6.Clauss-Ehlers CS. Promoting ecological health resilience for minority youth: enhancing health care access through the school health center. Psychology in the Schools. 2003;40:265–78. [Google Scholar]
- 7.Wade TJ, Mansour ME, Line K, Huentelman T, Keller KN. Improvements in health-related quality of life among school-based health center users in elementary and middle school. Ambul Pediatr. 2008;8:241–9. doi: 10.1016/j.ambp.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 8.Adams EK, Johnson V. An elementary school-based health clinic: can it reduce Medicaid costs? Pediatrics. 2000;105(4 Pt 1):780–8. doi: 10.1542/peds.105.4.780. [DOI] [PubMed] [Google Scholar]
- 9.Guo JJ, Jang R, Keller KN, McCracken AL, Pan W, Cluxton RJ. Impact of school-based health centers on children with asthma. J Adolesc Health. 2005;37:266–74. doi: 10.1016/j.jadohealth.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan DW, Brindis CD, Phibbs SL, Melinkovich P, Naylor K, Ahlstrand K. A comparison study of an elementary school-based health center: effects on health care access and use. Arch Pediatr Adolesc Med. 1999;153:235–43. doi: 10.1001/archpedi.153.3.235. [DOI] [PubMed] [Google Scholar]
- 11.Santelli J, Kouzis A, Newcomer S. School-based health centers and adolescent use of primary care and hospital care. J Adolesc Health. 1996;19:267–75. doi: 10.1016/S1054-139X(96)00088-2. [DOI] [PubMed] [Google Scholar]
- 12.Young TL, D'Angelo SL, Davis J. Impact of a school-based health center on emergency department use by elementary school students. J Sch Health. 2001;71:196–8. doi: 10.1111/j.1746-1561.2001.tb07316.x. [DOI] [PubMed] [Google Scholar]
- 13.Gilman S, Nader PR. Measuring the effectiveness of a school health program: methods and preliminary analysis. J Sch Health. 1979;49:10–4. doi: 10.1111/j.1746-1561.1979.tb05270.x. [DOI] [PubMed] [Google Scholar]
- 14.Baquiran RS, Webber MP, Appel DK. Comparing frequent and average users of elementary school-based health centers in the Bronx, New York City. J Sch Health. 2002;72:133–7. doi: 10.1111/j.1746-1561.2002.tb06532.x. [DOI] [PubMed] [Google Scholar]
- 15.Kaplan DW, Brindis C, Naylor KE, Phibbs SL, Ahlstrand KR, Melinkovich P. Elementary school-based health center use. Pediatrics. 1998;101:E12. doi: 10.1542/peds.101.6.e12. [DOI] [PubMed] [Google Scholar]
- 16.Johnson V, Hutcherson V. A study of the utilization patterns of an elementary school-based health clinic over a 5-year period. J Sch Health. 2006;76:373–8. doi: 10.1111/j.1746-1561.2006.00128.x. [DOI] [PubMed] [Google Scholar]
- 17.Brown MB, Bolen LM. School-based health centers: strategies for meeting the physical and mental health needs of children and families. Psychology in the Schools. 2003;4:279–87. [Google Scholar]
- 18.Crespo RD, Shaler GA. Assessment of school-based health centers in a rural state: the West Virginia experience. J Adolesc Health. 2000;26:187–93. doi: 10.1016/s1054-139x(99)00053-1. [DOI] [PubMed] [Google Scholar]
- 19.Mahoney G, Kaiser A, Girolametto L, MacDonald J, Robinson C, Safford P, et al. Parent education in early intervention: a call for a renewed focus. Topics in Early Childhood Special Education. 1999;19:131–40. [Google Scholar]
- 20.Schlitt J, Juszczak L, Brondos C, Nystrom R, Klein J, Kaplan D, et al. Creating access to care for children and youth: school-based health center census 1998–1999. Washington: National Assembly on School-Based Health Care; 2000. [Google Scholar]
- 21.Wade TJ, Line K, Huentelman T. School-based health centers (SBHC) evaluation project. A prescription for success. Health Foundation of Greater Cincinnati. 2005. Aug, [cited 2008 Jun 23]. Available from: URL: http://www.healthfoundation.org/publications.html.
- 22.Welligent Inc. Health Manager: Version 4.0. Norfolk (VA): Welligent Inc.; 2002. [Google Scholar]
- 23.SAS Institute Inc. SAS: procedures guide. Cary (NC): SAS Institute Inc.; 1999. [Google Scholar]
- 24.Wade TJ, Cairney J. General issues: sociological contributions. In: Ammerman RT, editor. Child psychopathology. New York: John Wiley & Sons; 2006. pp. 47–63. [Google Scholar]
- 25.Webber MP, Carpiniello KE, Oruwairye T, Lo Y, Burton WB, Appel DK. Burden of asthma in inner-city elementary schoolchildren. Do school-based health centers make a difference? Arch Pediatr Adolesc Med. 2003;157:125–9. doi: 10.1001/archpedi.157.2.125. [DOI] [PubMed] [Google Scholar]
- 26.Newacheck PW. Poverty and childhood chronic illness. Arch Pediatr Adolesc Med. 1994;148:1143–9. doi: 10.1001/archpedi.1994.02170110029005. [DOI] [PubMed] [Google Scholar]
- 27.Newacheck PW, Strickland B, Shonkoff JP, Perrin JM, McPherson M, McManus M, et al. An epidemiologic profile of children with special health care needs. Pediatrics. 1998;102(1 Pt 1):117–23. doi: 10.1542/peds.102.1.117. [DOI] [PubMed] [Google Scholar]
- 28.Newacheck PW, Hughes DC, Stoddard JJ. Children's access to primary care: differences by race, income, and insurance status. Pediatrics. 1996;97:26–32. [PubMed] [Google Scholar]
- 29.Geierstanger SP, Amaral G. School-based health centers and academic performance: what is the intersection?; April 2004 Meeting Proceedings. White paper; Washington: National Assembly on School-Based Health Care; 2005. [Google Scholar]
- 30.Fowler MG, Johnson MP, Atkinson SS. School achievement and absence in children with chronic health conditions. J Pediatr. 1985;106:683–7. doi: 10.1016/s0022-3476(85)80103-7. [DOI] [PubMed] [Google Scholar]
- 31.Guo JJ, Wade TJ, Keller KN. Impact of school-based health centers on students with mental health problems. Public Health Rep. 2008;123:768–80. doi: 10.1177/003335490812300613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mansour ME, Kotagal UP, DeWitt TG, Rose B, Sherman SN. Urban elementary school personnel's perceptions of student health and student health needs. Ambul Pediatr. 2002;2:127–31. doi: 10.1367/1539-4409(2002)002<0127:uespsp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 33.Gall G, Pagano ME, Desmond MS, Perrin JM, Murphy JM. Utility of psychosocial screening at a school-based health center. J Sch Health. 2000;70:292–8. doi: 10.1111/j.1746-1561.2000.tb07254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Taras HL American Academy of Pediatrics Committee on School Health. School-based mental health services. Pediatrics. 2004;113:1839–45. doi: 10.1542/peds.113.6.1839. [DOI] [PubMed] [Google Scholar]
- 35.Ostberg V. Children in classrooms: peer status, status distribution and mental well-being. Soc Sci Med. 2003;56:17–29. doi: 10.1016/s0277-9536(02)00006-0. [DOI] [PubMed] [Google Scholar]
- 36.Surgeon General (US) Mental health: a report of the Surgeon General. Washington: Department of Health and Human Services (US); 1999. [Google Scholar]
- 37.McCord MT, Klein JD, Foy JM, Fothergill K. School-based clinic use and school performance. J Adolesc Health. 1993;14:91–8. doi: 10.1016/1054-139x(93)90091-3. [DOI] [PubMed] [Google Scholar]