SYNOPSIS
Objectives
This article describes a model for a school-based program designed to reduce dental access disparities and examines its financial feasibility in states with different Medicaid reimbursement rates.
Methods
Using state and national data, the expected revenues and expenses for operating the program in different states were estimated. Hygienists with support staff provided screening and preventive services in schools using portable equipment and generated surplus funds that were used to supplement payments to community clinics and private practices for treating children.
Results
The program is financially feasible in states when the ratio of Medicaid fees is 60.5% of mean national fees. Of the 13 states examined, one-third have adequate Medicaid fees to support the program.
Conclusion
The model program has considerable promise for reducing access disparities at a lower cost per child than current Medicaid programs.
Approximately 23 million children are eligible for Medicaid and State Children's Health Insurance Program (SCHIP) dental benefits.1 About 34% of these children visit a dentist one or more times per year. In contrast, nearly 55% of privately insured children visit dentists annually.2 There are also large disparities in oral health. For children 12 to 19 years of age, 27% from low-income families (<100% of the federal poverty level [FPL]) have untreated tooth decay compared with 12% from higher-income families (>200% FPL).3
The reasons for these access disparities are well-known. The two national strategies for providing low-income children access to care—Medicaid dental insurance and the dental safety net system—have significant limitations. Dental Medicaid programs are substantially underfunded in most states, which is evident in the low expenditures per Medicaid-eligible child with a visit ($272) compared with privately insured children with a visit ($635).2 Because most Medicaid programs have very low fees, relatively few dentists participate, and this is the primary reason for the low utilization rates.4
The second basic strategy to address access disparities is public and voluntary sector operated dental safety net clinics. The size of the dental safety net system is not precisely known, but a recent article suggests that it has the capacity to treat about eight million people per year.5 Thus, the dental safety net can care for only a small percentage of the underserved population.
This article presents a new strategy for reducing access disparities. In this model, dental hygienists and support staff provide screening and preventive services to children in schools using portable equipment and generate positive net revenues from these services. With these funds, children with caries and other conditions requiring dental services receive care in private offices, community clinics, schools, and mobile vans and, if necessary, dentists or dental clinics are reimbursed at more competitive levels by supplementing standard Medicaid payments.
The goal of the model program is to bring dental care utilization rates of low-income children to the level seen in middle-income children. This requires increasing the percentage of low-income Medicaid- and SCHIP-eligible children who visit a dentist at least once annually from 34% to about 55%, the level for children with private insurance.2 For the purpose of the financial model, the goal is to increase utilization to 55%.
The literature on school-based dental delivery systems consists mainly of descriptions of screening and preventive programs (e.g., topical fluoride and sealants).6–8 Few school programs provide restorative and other services,9 but at least four follow the general model presented in this article. These programs are in Connecticut (Personal communication, Margaret Drozdowski, Community Health Center Inc., December 2007), Rochester, New York (Personal communication, Cyril Meyerwitz, Eastman Dental Center, University of Rochester, July 2007), Southern Massachusetts (Personal communication, Richard Niederman, The Forsyth Institute, December 2007), and Minneapolis (Apple Tree Dental). Data evaluating these programs have not been published.
METHODS
Model description
Target population
The program targets schools with large numbers of Medicaid- and SCHIP-eligible children, aged 3 to 18 years. For the months that schools are closed, the program provides care to children in Head Start programs, summer camps, and other institutional settings. Low-income children who are not eligible for public insurance are not included in the model, except when the program is run by a federally qualified health center (FQHC).
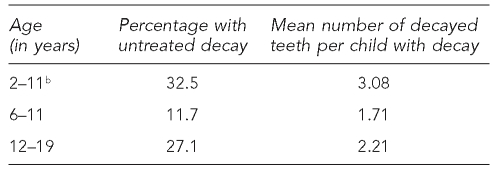
Many children living in poverty have relatively good oral health, and less than 40% require restorative services. Table 1 gives the percentage of children from low-income families (<100% FPL) by age with untreated decayed deciduous or permanent teeth and the mean number of decayed teeth. Depending on the age group, about 60% to 90% of children are caries-free, and those with decay average three or fewer carious teeth.3
Table 1. Percentage of children from low-income families (<100% FPL) with untreated decayed deciduous or permanent teeth and the mean number of decayed teeth per child with decay, by agea.
aNational Health and Nutrition Examination Survey, 1999–2004
bDeciduous teeth
FPL = federal poverty level
The proper use of dental preventive services substantially reduces the incidence of caries in children. Over several years of exposure to preventive services, caries incidence is expected to decline substantially for children in the higher caries risk groups.10–12 The long-term impact of preventive services on the incidence of tooth decay is not included in the financial model. As such, the model overestimates the number of children needing restorative services and program expenses and underestimates net revenues.
Clinical teams
The composition of the clinical teams working in schools will vary based on local conditions. For the purpose of financial modeling, the team consists of one dental hygienist, one dental assistant, one community aide, and 0.5 of a school aide. In several states, hygienists can work in public facilities independently of a dentist and can bill Medicaid for common screening and preventive services. Staff salaries are based on 2005 Department of Labor reports on Connecticut wages for these occupations.13
Dental hygienists do screening examinations, review bite-wing radiographs, and identify children requiring visits to general or pediatric dentists. Dental assistants are responsible for assisting dental hygienists. Using two chairs (based on available space), this includes seating patients, taking bite-wing radiographs, recording clinical findings and services, maintaining supplies and equipment, and sterilizing equipment.
School aides are assigned to two hygiene teams and are responsible for enrolling children in the program, checking patient Medicaid eligibility, scheduling hygiene and dental visits, and program coordination. Community aides can function in several different capacities: (1) serving as case managers to help parents take their children to the dentist, (2) accompanying children from schools to dental facilities, (3) arranging for mobile dental vans to come to schools, and (4) arranging for dentists to come to the schools and provide restorative and other services.
Dentist services are provided in safety net clinics, private practices, mobile dental vans, or schools. Whatever the setting, dentists review the hygienists' findings, do a comprehensive examination that may include additional diagnostic radiographs and tests, restore carious teeth, and provide other services as needed. Dentists are reimbursed for these services, based on the Medicaid fee schedule and negotiations with the organization running the program, and may receive supplemental payments.
Dental equipment and supplies
Efficient program operation requires the use of two portable chairs and some backup equipment to reduce downtime from the need to repair and maintain critical pieces of equipment. Purchased at list prices, the equipment is amortized over five years. The supplies are calculated at $6/patient visit. Total cost for equipment and supplies comes to $23,000, and liability insurance costs $2,000 per hygiene team per year.
System management
Organizations that manage the model program could be FQHCs or other community clinics, community hospitals, dental schools, private dentists, or private companies. The management group employs the hygiene team staff, contracts with the dentists, bills Medicaid/SCHIP for hygiene services, pays dentists or clinics the contracted supplement, and operates centralized information systems and quality assurance programs. The actual cost for providing these services is unknown, but for a clinical organization, the estimate used in this analysis is 8% of gross expenses.
FQHCs are especially well-positioned financially to administer the proposed program because in most states, they are reimbursed per patient visit at a higher rate than Medicaid fees. Further, they receive a federal grant to cover losses from providing care to low-income children who are not covered by public insurance. The main limitation of FQHCs is that they are few in number, and most have large patient backlogs.
RESULTS
Financial model
This section considers the financial feasibility of the model in several states. The analyses use 2005 expense data from Connecticut, because these data were not readily available for the other states. Connecticut is one of the wealthiest states in the nation, so expenses are relatively higher in Connecticut than in most other states. Thus, expenses are overestimated, and net program revenues are underestimated for the other states. Total program expenses and revenues per hygiene team and the total cost to the Medicaid program are presented.
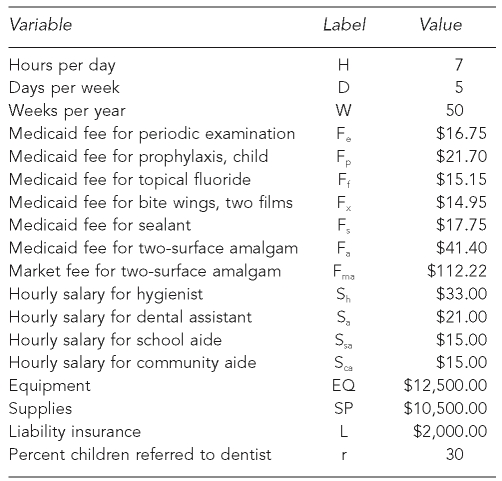
Expenses and revenues
The basic set of expense and revenue values and the formula for calculating these values are shown in Table 2. The assumptions are that the dental hygiene team treats 14 patients per day, five days per week, for 250 days per year, and that staff are paid at market competitive rates, including fringe benefits. The hygiene team provides services for 1,750 hours per year, generates nearly $139 per hour, and has gross revenues of $243,040; dentist revenues are $86,940. For 3,500 visits, total revenues are $329,980—$189 per child or $94.28 per visit.
Table 2. Financial model: initial values, Connecticut, 2005.
H*D*W = number of children
HR (hygienist's revenues) = H*D*W (2 [Fe + Fp + Ff + Fx] + 0.1 Fs)
DR (dentist's revenues) = H*D*W*r*4 Fa
TR (total revenues) = HR + DR
HE (hygienist's expenses) = H*D*W (Sh + Sa + Sca + 1/2 [Ssa])
DE (dentist's expenses) = H*D*W*r*4 Fma
TE (total expenses) = HE + DE +EQ + SP + L
Break even – TR = TE + 8% TE
Expenses per hygiene team are $158,875 ($133,875 for salaries and $25,000 for equipment, supplies, and liability insurance) and $235,662 for dentist services. Expenses for dentist services are calculated at market prices. Total operating expenses for 3,500 visits (1,750 children) are $394,537. With administrative expenses of 8%, total expenses are $426,100, or $243 per child.
Break-even analysis
Total expenses exceed total revenues by $96,120. The prevailing Medicaid fees in Connecticut are too low for hygiene teams to generate sufficient surpluses to bring Medicaid fees to the level prevailing at the market. It should be noted that Connecticut Medicaid fees are among the lowest in the country and are expected to increase in fiscal year 2008. For total revenues to be equal to total expenses, Medicaid fees need to be raised by 29%. Then Connecticut Medicaid fees will be about 61% of mean national fees in 2003.
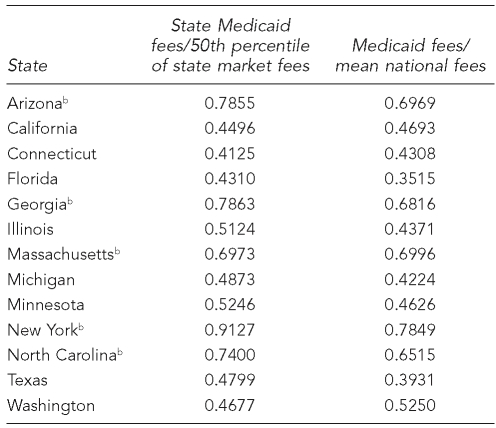
Other states
To assess the financial viability of this model, prevailing Medicaid fees were examined in relation to prevailing market fees for a number of other states. The most recent readily available Medicaid fees by state are for the year 2003. The fees available for each state are the 50th percentile of prevailing market fees. To assess the financial feasibility of the school-based dental care delivery model in a state, the ratio of Medicaid fees and market fees was determined. For the state of Connecticut, total expenses are equal to total revenues when the ratio of Medicaid fees is about 61% of mean national fees. This threshold is used to assess the financial viability of the model in other states. The ratio between Medicaid fees (2003) and the mean national market fees (2005) was also calculated. Table 3 presents these two ratios for a selected number of states. Both ratios were created by dividing the simple mean of Medicaid fees for a screening examination, prophylaxis, topical fluoride, sealant, bite-wing x-rays (two films), and a two-surface amalgam by the simple mean of market fees for the same dental services. As can be seen, a number of states have a ratio higher than that required (i.e., 61%) for revenues to be at least equal to expenses.
Table 3. Ratio of Medicaid fees (2003) and 50th percentile of market fees by state (2003) and national market fees (2005)a.
aData on state Medicaid fees and the 50th percentile of state market fees come from the year 2003. The data on state Medicaid fees and mean national market fees come from the years 2003 and 2005, respectively.
bStates with adequate Medicaid fees to support the model school-based program
Sensitivity analysis
Sensitivity analysis was conducted on several key variables, as detailed in the following text.
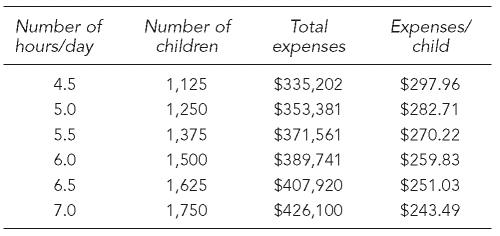
Hours, days, and weeks of operation
Schools may not be available seven hours per day and five days per week. Thus, the estimate of 14 patients per day may be high. Table 4 presents total expenses and expenses per child when a hygiene team provides care to schoolchildren from 4.5 hours per day to 7.0 hours per day. Expenses for salaries, fringe benefits, equipment, supplies, and liability insurance are based on 1,750 hours, or 250 days per year. For Medicaid fees, the adjusted Connecticut fees are used, and dentists are paid for their services at market rates.
Table 4. Hours providing care per day by hygiene team and number of children treated, total expenses, and expenses per child per year, Connecticut, 2005.
As shown in Table 4, total expenses per child per year vary from $297.96 (4.5 hours per day) to $243.49 (7.0 hours per day). A 10% increase in the number of hours worked per day results in a 5% increase in total revenues and about a 5% decrease in expenses per child.
Variation in the number of days per week is not expected to significantly affect total expenses per child. A hygiene team may operate for one or more days in the same school and then move to another school. Similarly, variation in the number of weeks per year a hygiene team operates may not affect total expenses per child, if hygiene teams are hired for time periods of less than a year or used in other public institutional settings for disadvantaged children during the summer months (e.g., summer camps).
Equipment, supplies, and salaries
Variation in expenses for equipment and supplies influences the financial feasibility of the school-based dental care delivery model. A 10% increase in expenses for equipment and supplies results in less than a 1% increase in total expenses (data not shown). Variation in expenses for salaries plays a much more important role. A 10% increase in salaries and fringe benefits results in a little more than a 3% increase in total expenses (data not shown).
Oral health
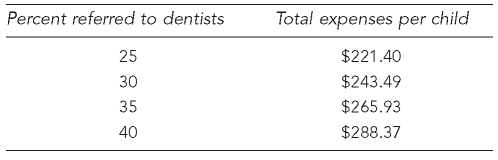
Variation in children's oral health determines their need for restorative and other dentist-level services and, therefore, impacts total expenses. Table 5 estimates total expenses, corresponding to different referral levels to dentists and number of needed services, respectively. A 10% increase in the percentage of children referred to dentists results in a 3% increase in expenses per child; a 10% increase in the number of two-surface amalgams required per child results in about a 3% increase in expenses per child.
Table 5. Percent of children referred to dentists and total expenses per child per year.
DISCUSSION
The primary value of financial modeling is to determine if a proposed program is feasible. Modeling does not prove or ensure that the plan will work when implemented. The results of this modeling effort suggest that the proposed school-based dental program has a reasonably good chance of being successful financially if Medicaid fees are at a certain level. Specifically, the program is financially feasible in states when the ratio of Medicaid fees is 61% of mean national fees. In this study, current Connecticut Medicaid fees were not adequate, but they were sufficient in several other states.
The sensitivity analyses indicated that the model program is financially dependent on the number of patients treated per day, staff salaries, and children's oral health status. Equipment and supply costs were less important. Of these variables, the key driver of net revenues is the number of patients treated per day. The estimate of 14 patients per day may be high on average because at some schools, children are not available seven hours per day. This problem can be addressed by scheduling younger children for more than two patients per hour or making arrangements with school officials to extend the time children are available. At least for new programs, a mean of 12 patients per day may be more realistic, and the sensitivity analysis indicated that two fewer patients per day results in a 5% decrease in total revenues.
Another determinant of program expenses is the number and type of staff on hygiene teams. The staffing model used in this analysis was based on discussions with clinical experts. However, other staffing combinations (e.g., type and number) are possible, and until the model is implemented for several years, the preferred staffing arrangement cannot be determined. Most likely, there is no one best staffing model. Rather, the number and types of staff will depend on local conditions.
In this regard, the use of mid-level dental providers to treat underserved populations is receiving increased national attention. While they may have a role in school-based programs, mid-level dental providers are not licensed in any state and, as such, this issue is beyond the scope of this article.
An important dimension of the staffing model is the need for an on-site dentist to supervise hygienists. Connecticut allows hygienists to work independently in schools and other public venues. In some states, hygienists must be under the indirect supervision of a dentist, and in still others a dentist must be physically present at all times. This variation among states has obvious implications for the models' financial feasibility.
Challenges
The two biggest operational challenges in running the model program successfully are enrolling adequate numbers of Medicaid-eligible children at each school and arranging for children needing restorative and other services to see a dentist. With respect to enrollment, a discussion of this issue with a national expert on school-based health programs indicates that over several years, as the program becomes an integral part of school activities, perhaps 50% to 80% of eligible children will enroll in the program (Personal communication, Julia Lear, Center for Health and Health Care in Schools, The George Washington University, December 2007). For obvious reasons, it makes sense to focus the program on schools with larger numbers of Medicaid- and SCHIP-eligible children.
The second major challenge is making sure that children with unfilled decayed teeth are treated by dentists. The use of the case manager may be the simplest and least expensive approach to arrange for parents to take their children to the offices of private dentists or community clinics. However, it requires considerable parental cooperation, and the experience of the school-based program now being run in Connecticut indicates that case managers are able to arrange for about 40% of the children to obtain services (Personal communication, Margaret Drozdowski, Community Health Center Inc., December 2007). Driving children from school to clinics and practices to obtain dentist services is another option, but it is likely to increase program administrative expenses substantially, and it may be difficult to obtain parents' permission. A more promising strategy is bringing dentists to schools. This can be accomplished by using a van with dental operatories or by having dentists work in schools using portable dental equipment. These different approaches are not mutually exclusive, and the most effective strategy for getting children to dentists probably depends on local conditions.
Program management
In terms of program management, many organizations could assume responsibility for one or more schools. For example, FQHCs are ideal because federal laws allow FQHCs to treat eligible children in schools and to charge FQHC reimbursement rates. FQHCs receive a visit rate per child that is substantially higher than billing Medicaid for most services. As such, many FQHCs may have less difficulty covering program expenses.
The major limitation FQHCs have is their capacity to assure that children needing the services of dentists receive them. This is because most FQHC dental clinics are fully booked. In states where FQHCs have an adequate supply of dentists, employing dentists to deliver care in schools using portable equipment or in mobile vans located at schools has the greatest potential for solving the dentist access problem.
Individual practitioners or groups of private dental practitioners could take responsibility for several schools within their community that have large numbers of Medicaid-eligible children. Local practitioners know their community and can arrange to take responsibility for the number of schools and children that they can manage. Because there are so many practicing dentists, if even a small percentage of them participated in the program, large numbers of children would obtain needed services. Of course, this assumes adequate Medicaid reimbursement rates, so that participating local dentists break even or generate modest surpluses. Third, independent organizations such as hospitals, health departments, insurance companies, and dental schools could manage the program.
In the economic model presented in this article, the estimated marginal increase in central administrative expenses for dental clinics or practices to run the model program was 8%. This is just an informed guess, but it is probably accurate. When hygiene team staff are not affiliated with local dental clinics and practices, central administrative costs may be higher.
The model presented in this article is now in the second year of operation in Connecticut. Many Medicaid-eligible children in more than 100 schools are now receiving screening and preventive services in schools and dentist services in FQHC-directed clinics, vans, or school clinics. Plans are to formally evaluate the program within the next few years.
Program advantages
The school-based model has several distinct advantages. First, far fewer dentists are needed to provide care to children. As an estimate, the school-based and the traditional dental care systems require 15 vs. 50 full-time-equivalent dentists per 100,000 children, respectively. This is because hygiene teams rather than dentists care for the majority of children who only need screening and preventive services.
Second, the unit cost of providing dental care to children is substantially reduced. The financial model estimates that the cost per child with a visit is about $243 in the school-based system vs. $424 in the traditional system. This means that for the Medicaid funds available in each state, the lower costs per child will allow thousands more children to obtain dental care.
Third, the school model is much less dependent on parents taking their children to dental offices and clinics. This is a significant issue in low-income areas, where single-parent families have many economic and social challenges.
Fourth, and most importantly, the school-based program is expected to greatly improve children's oral health. All participating children receive comprehensive preventive services, and most have decayed teeth and other problems treated by dentists. It is important for programs of this type to use a risk-based protocol so that the number of preventive visits per child and the number and types of preventive services are based on caries risk.
The impact of preventive services on reducing caries and program costs was not incorporated into the financial model, but clearly, if the target population is reasonably stable over time, large reductions in caries can be expected. Likewise, program costs should decline after the initial surge of decay is treated and the effects of preventive services take hold. Also, with improved oral health (and less dentally related pain) student performance in school is likely to improve, because children will have fewer absences and will be better able to focus on their schoolwork.
The primary disadvantage of the proposed model dental program is the large increase in total dental Medicaid expenditures as more children obtain care. Clearly, significant reductions in dental access disparities will increase total expenditures.
Another disadvantage of the model is that it cannot treat low-income children who are not eligible for public dental insurance and remain fiscally solvent. This is less of a problem for FQHC-run programs, because they receive a federal grant to partially cover the costs of treating low-income, uninsured children.
CONCLUSION
This article examined the financial feasibility of a school-based dental delivery system for low-income children enrolled in the Medicaid program. The proposed system builds on the advantages of schools for delivering screening and preventive services and private practices and community clinics for providing dentist services. The analyses indicate that the model program is financially feasible in states where Medicaid fees average 61% of mean private sector fees.
The primary advantage of the school-based model is a major reduction in access and oral health disparities. Further, the proposed model is a less expensive way of providing dental care to Medicaid-eligible children than the traditional delivery system. However, aggregate Medicaid dental expenditures will increase substantially. If states are serious about reducing access disparities, they will need to provide the necessary funds to support the proposed program.
Acknowledgments
The authors appreciate the advice of Drs. Jack Brown and Albert Guay from the American Dental Association on the design of the study and review of the article.
Footnotes
This article was supported in part by a grant from the Connecticut Health Foundation.
REFERENCES
- 1.Department of Health and Human Services (US) 2007 CMS statistics. Washington: Department of Health and Human Services, Centers for Medicare & Medicaid Services Office of Research, Development, and Information (US); 2007. CMS Pub No 03480. [Google Scholar]
- 2.Manski RJ, Brown E. Dental use, expenses, dental coverage, and changes, 1996 and 2004. Rockville (MD): Agency for Healthcare Research and Quality; 2007. MEPS Chartbook No. 17. [Google Scholar]
- 3.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat 11 2007(248) [PubMed] [Google Scholar]
- 4.American Dental Association. 2000 survey of current issues in dentistry: dentists' participation in Medicaid programs. Chicago: ADA; 2001. [Google Scholar]
- 5.Bailit H, Beazoglou T, Demby N, McFarland J, Robinson P, Weaver R. Dental safety net: current capacity and potential for expansion. J Am Dent Assoc. 2006;137:807–15. doi: 10.14219/jada.archive.2006.0294. [DOI] [PubMed] [Google Scholar]
- 6.Jackson DM, Jahnke LR, Kerber L, Nyer G, Siemens K, Clark C. Creating a successful school-based mobile dental program. J Sch Health. 2007;77:1–6. doi: 10.1111/j.1746-1561.2007.00155.x. [DOI] [PubMed] [Google Scholar]
- 7.Scherrer CR, Griffin PM, Swann JL. Public health sealant delivery programs: optimal delivery and costs of practice acts. Med Decis Making. 2007;27:762–71. doi: 10.1177/0272989X07302134. [DOI] [PubMed] [Google Scholar]
- 8.Locker D, Frosina C, Murray H, Wiebe D, Wiebe P. Identifying children with dental care needs: evaluation of a targeted school-based dental screening program. J Public Health Dent. 2004;64:63–70. doi: 10.1111/j.1752-7325.2004.tb02729.x. [DOI] [PubMed] [Google Scholar]
- 9.Albert DA, McManus JM, Mitchell DA. Models for delivering school-based dental care. J Sch Health. 2005;75:157–61. [PubMed] [Google Scholar]
- 10.Armfield JM, Spencer AJ. Community effectiveness of fissure sealants and the effects of fluoridated water consumption. Community Dent Health. 2007;24:4–11. [PubMed] [Google Scholar]
- 11.Hiiri A, Ahovuo-Saloranta A, Norblad A, Mäkelä M. Pit and fissure sealants versus fluoride varnishes for preventing dental decay in children and adolescents. Cochrane Database Syst Rev. 2006;18 doi: 10.1002/14651858.CD003067.pub2. CD003067. [DOI] [PubMed] [Google Scholar]
- 12.Bader JD, Shugars DA, Bonito AJ. A systematic review of selected caries prevention and management methods. Community Dent Oral Epidemiol. 2001;29:399–411. doi: 10.1034/j.1600-0528.2001.290601.x. [DOI] [PubMed] [Google Scholar]
- 13.Connecticut Department of Labor. Connecticut health care industry analysis. 2005. [cited 2008 Jun 26]. Available from: URL: http://www.scribd.com/word/full/1621033?access_key=key_f76nkyx5w7vbvgolij.