SYNOPSIS
Objectives.
School-based health centers (SBHCs) play an increasingly major role in providing mental health services for students. This study evaluated the impact of SBHCs on mental health-care services and psychosocial health-related quality of life (HRQOL).
Methods.
Four SBHC intervention and two matched non-SBHC school districts were examined from 1997 to 2003. The SBHC intervention began in 2000. Data included child and parent pediatric HRQOL and Ohio Medicaid claims. A longitudinal quasi-experimental time-series repeated measures design was used for this study, involving analysis of covariance to assess health costs and regression analyses for HRQOL scores.
Results.
After the SBHC program, proportions of students accessing mental health-care services for urban and rural SBHC intervention schools increased 5.6% (χ2=39.361, p<0.0001) and 5.9% (χ2=5.545, p<0.0001), respectively, compared with increases of 2.6% (χ2=2.670, p=0.1023) and 0.2% (χ2=0.006, p=0.9361) for urban and rural non-SBHC schools, respectively. Using data from 109 students with mental health problems based on Medicaid claims, the study found SBHC students had significantly lower total health-care costs (F=5.524, p=0.005) and lower costs of mental health services (F=4.820, p=0.010) compared with non-SBHC students. While improvements over time in HRQOL for SBHC students compared with non-SBHC students and students from non-SBHC schools were observed, only some were statistically significant.
Conclusions.
SBHC programs increase the proportion of students who receive mental health services and may improve pediatric HRQOL. SBHC students with mental health problems had lower total Medicaid reimbursements compared with non-SBHC students.
Students with mental health problems often incur large public expenditures. During the last half-century, literature has clearly shown that children from low-income families have higher prevalence of mental health problems than other children.1 For example, Rutter in Great Britain found that children experiencing economic hardship had significantly higher levels of mental health problems.2 Examining 6- to 18-year-old children, the Midtown Manhattan Survey of Psychiatric Impairment in Urban Children in New York City found strong evidence that children from families on welfare were almost twice as likely to manifest impaired health and behavior ratings.3–5 The Ontario Child Health Study found children from families with very low incomes and/or receiving welfare were significantly more likely to have at least one of four disorders—hyperactivity, conduct disorder, emotional disorder, and somatization—compared with other children.6,7 Race/ethnicity, while often difficult to disentangle from poverty, is also predictive of child psychopathology.8,9
While the need appears greatest among socioeconomically disadvantaged children, it is this very group that is often inadequately covered for health services including mental health, substance abuse treatment, and preventive health visits.10,11 Moreover, they are also overrepresented in the corrections system. For example, in 2003, more than 15,000 children with mental disorders were incarcerated in detention centers. This compelled more than 130 national and state advocacy organizations representing children, families, and correctional officers to call on the U.S. Congress to address gaps in services for students with mental disorders.12 One potential intervention to redirect resources from incarceration to prevention could be through school-based health centers (SBHCs), which provide physical and mental health-care services for children in need.
SBHCs provide essential primary health care for students and are in a unique position to reduce barriers to care for disadvantaged children. The recent census by the National Assembly on School-Based Health Centers (NASBHC) identified 1,709 SBHCs nationwide in the 2004–2005 school year.13 Many of these were established with financial support from various sources including the federal government, foundations, Medicaid, and other health insurers.13,14 Numerous studies have documented that SBHCs can effectively reduce health-care access barriers, hospitalizations, and emergency room (ER) visits among youth.15–22 A study conducted in Georgia reported that there was a significant decrease in Medicaid expenses for inpatient, non-emergency department transportation, drug, and ER visits for students enrolled in the SBHC program compared with students not enrolled in the SBHC program.16
These in-school services can also address barriers such as stigma, noncompliance, and inadequate access to mental health services for youth.23–26 For example, survey studies in Colorado schools found that students with SBHCs were more likely to make mental health visits to the centers, had fewer urgent or emergency visits in the community,19 and had less difficulty obtaining primary care than students in a comparison school.18 Of 1,235 SBHCs responding to the 2004–2005 NASBHC survey,14 65% (805) offered on-site mental health services through licensed clinical social workers, psychologists, and/or substance abuse counselors. Almost all of these SBHCs (91%) offered mental health diagnoses, grief and loss therapy, crisis intervention, and assessments. In addition, 62% offered long-term therapy and 54% offered medication management or administration. Among the SBHCs without on-site mental health services, the majority offered referrals (63%), mental health diagnoses (63%), and screening (62%), while only 13% offered long-term therapy.
Although SBHCs have demonstrated value to school-age children in the community, the effect of SBHCs on accessibility of mental health-care services and costs had not been adequately documented or evaluated quantitatively. The objectives of this study were to evaluate the effect of SBHCs on accessibility of mental health-care services and health-related quality of life (HRQOL) and to compare total health-care Medicaid reimbursement and costs for mental health services over time among students with mental health problems. By examining costs before and after implementation of an SBHC program, we were able to examine changes in patterns and costs of service use of students in schools with and without an SBHC. Most studies have not distinguished between students in schools with SBHCs who use SBHC services and those who do not use the services. In this analysis, we compared three groups: SBHC users, SBHC non-users, and the non-SBHC comparison group before and after SBHC program implementation. The central hypotheses were: (1) the presence of SBHCs increases primary mental health-care use and decreases the need for overall hospitalizations and ER visits, (2) the total health expenses for students either decrease over time or remain relatively unchanged, and (3) pediatric HRQOL increases over time.
METHODS
The study design was a longitudinal quasi-experimental repeated measure time-series. The target population was school-age students enrolled in schools in the Greater Cincinnati area and also in Ohio Medicaid or State Children's Health Insurance Program (SCHIP) from academic years 2001–2003.
The data came from an outcomes study and a cost study. The outcomes study compared changes in student health during three years in four school districts (seven schools in total) with newly implemented SBHCs to two other school districts (six schools in total) matched on urban/rural status, percentage of nonwhite students, and percentage of students in the free or reduced school lunch program (from 37% to 88%, mean=63.5%).27 The two comparison school districts did not have an SBHC program during the study period based on an agreement between The Health Foundation of Greater Cincinnati and school district administrators. This study collected information on pediatric HRQOL and SBHC encounters.
The cost study examined Medicaid costs across these same SBHC and comparison schools.28 Each SBHC was open from Monday through Friday and operated during the school year from September to May. Any requests during the weekend were directed to neighborhood health centers or other primary care physicians. SBHC staff included at least one nurse practitioner and a collaborating physician who were responsible for documenting students' clinic encounter data, which provided the other critical information for this study. Four SBHCs provided mental health and psychiatric referrals, three provided behavior and mental health assessments and crisis intervention, and two provided individual counseling and had an on-site social worker or counselor. Mental health services in these schools were provided in different academic years (the first or second year of SBHC operations) due to resource availability.
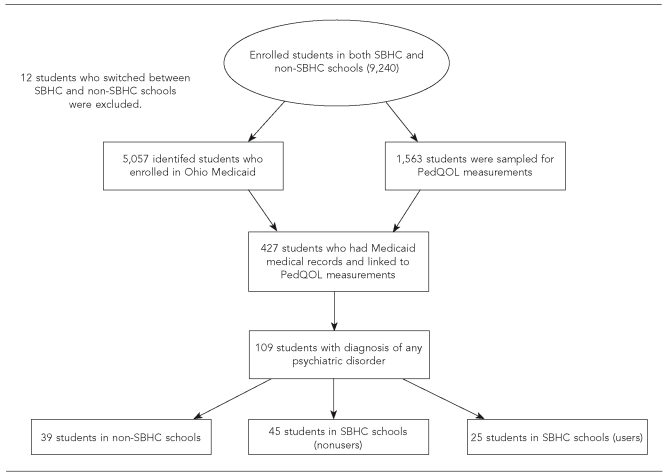
Schools provided student enrollment databases identifying student names and demographics for each school year from 2000–2001 to 2002–2003. There were a total of 9,240 unique students. These were linked with Ohio Medicaid claim databases of all children who filed Medicaid and/or SCHIP claims during these three years and the three years prior to the implementation of SBHCs for a total of 5,069 unique students (Figure 1). The match was based on children's name, gender, race, date of birth, and county code. Twelve students who switched between SBHC and non-SBHC comparison schools were excluded. The automated Medicaid claims database included all pharmacy, medical, hospital inpatient, emergency visit, and outpatient institutional claims. Use of Medicaid claims data for health economic and outcomes research has been well documented. Of the 5,057 students, 427 students and their parents were surveyed using the pediatric quality of life (PedsQL) measure.29 Of those, 109 students were identified as having mental health problems during the study period based on the student having a diagnosis in the Medicaid claims data from International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 290.xx through 316.xx. These mental health problems included attention deficit hyperactivity disorder (ADHD) and depressive, conduct, emotion, and adjustment disorders. All inpatient and outpatient institutional claims, physician office visits, prescription drugs, and other procedure claims from 1997 to 2003 for those students were extracted from the Medicaid claims database.
Figure 1. Flow chart of selecting cohort students with mental health problems, 1997–2003.
SBHC = school-based health center
PedQOL = pediatric quality of life
The final study sample included 39 students in non-SBHC schools (SBHCR=1), 45 students in schools with SBHCs who did not use the centers (SBHCR=2), and 25 students in schools with SBHCs who used the centers (SBHCR=3). The research was approved by the University of Cincinnati Medical Center Institutional Review Board.
Measures
Four outcome measures (dependent variables) were used for this study:
The proportion of students who accessed Medicaid mental health services before and after the SBHCs opened was used as a proxy to measure accessibility, which was defined as the total number of students who had any mental health services claims (based on Medicaid claims records) divided by the total number of students who were enrolled in both Medicaid and the study schools.
Annual total health-care reimbursement per student was defined as the total dollar amount that Medicaid paid for emergency services, inpatient/outpatient care, physician encounters, mental health services, prescription drugs, laboratory procedures, or diagnoses during each school year from September to August.
Annual cost of mental health services per student was defined as the total dollar amount that Medicaid paid for mental health hospital care or general mental health-care and support services, but not including prescription drug costs, during each academic year from September to August. Because all prescription drugs are documented in the Medicaid pharmacy claims file, it was difficult to clearly separate mental health-related drug claims.
Psychosocial and physical HRQOL as reported by students and parents using the PedsQL 4.0 was used to measure perceived changes in pediatric quality of life.29
Due to delays for medical claims processing and Health Insurance Portability and Accountability Act (HIPAA) regulation changes, we were unable to collect or use Medicaid claims data from June 2003 to August 2003. Consequently, the study period was shortened to September 1, 1997, through May 31, 2003, or to a little less than six years. Accordingly, for two of the dependent variables (health-care reimbursement amount and cost of mental health services), we estimated the costs for the final year to be the total from the first three quarters times 4/3 for the time-series repeated measures.
For each Medicaid claim reimbursement from 1997 to 2003, total health-care reimbursement and costs for mental health services were adjusted using the medical component of the Consumer Price Index (MCPI) as the dollar value in 2003 based on data from the Bureau of Labor Statistics. The inflation-adjusted discount rate was calculated using a 3.0% discount rate and the annual MCPI rate for each year of this study.30 The annual MCPI rates of change were 4.6% in 2002, 4.7% in 2001, 4.2% in 2000, 3.7% in 1999, 3.4% in 1998, and 2.8% in 1997.31,32
Pediatric HRQOL was assessed annually from 2000–2001 to 2002–2003 using the 23-item PedsQL 4.0, a field-tested, age-standardized tool designed specifically for use with community and school populations.29 Students were administered a questionnaire in person at their school by the SBHC Evaluation Project staff that included a self-reported HRQOL measure. Parents completed annual telephone questionnaires that included a proxy HRQOL measure of their children as well as additional demographic data and questions about chronic health conditions of the child. The PedsQL 4.0 provides a measure of students' overall HRQOL from 0 (being the lowest) to 100 (being the highest), which included physical (eight items) and psychosocial (15 items) dimensions. The Cronbach's alpha coefficients (reliability coefficients) ranged from α=0.72 for the child physical dimension to α=0.88 for both the child and parent-reported total scale for year one. These scores were similar with Varni et al.,33,34 who reported Cronbach's alpha for the total scale between α=0.88 for the child report and α=0.90 for the parent proxy report.
The covariates included the child's age as of September 30, 2002. Gender was coded as a dichotomous variable (male = 1 and female = 0). Race was also defined as a dichotomous variable (African American = 1, white and other races = 0) because of predominant Hispanic white in the other races categories. The number of enrollment months was defined for each child enrolled in the Medicaid program during the study period. Enrollment categories included aid for disabled or blind; Aid to Families with Dependent Children for low-income children from birth through age 18 and pregnant women; Ohio's SCHIP, which covers low-income children up to 150% of the federal poverty guidelines; and managed care organizations (MCOs), which included children enrolled in private MCOs supported by the Ohio Medicaid program. As recipients could have been in multiple programs during the study period, the recipient's aid category was defined by the percentage of enrollment months for which the recipient was enrolled in each program.
Data analysis
The demographic characteristics, psychiatric comorbidity frequencies, and child-reported and parent-reported pediatric HRQOL scores were compared among three groups of students: non-SBHC, SBHC users, and SBHC nonusers. One-way analysis of variance was used for continuous data such as age, months enrolled, and percentages of enrollment categories, and a Chi-square test was used for other dichotomous variables. To measure accessibility for mental health services, Chi-square tests of independence compared proportions of students in urban and rural areas who received any mental health services before and after the SBHCs opened.
A repeated measures analysis of covariance (ANCOVA) was performed to evaluate the differences in total health-care reimbursement and cost for mental health services for three years before and after the SBHCs opened. After controlling the covariates, the primary factor of interest in the repeated measures ANCOVA was the TIME*SBHC group interaction term (SBHC GROUP*TIME; where SBHC GROUP = 1 for comparison group, 2 for SBHC nonusers, and 3 for SBHC users) indicating a difference in change over time among SBHC groups. Covariates included age, gender, race, and Medicaid enrollment categories (SCHIP, aid for disabled or blind, and MCO). For this ANCOVA analysis, the statistical power was greater than 0.80 with alpha level 0.05 and medium effect size of 0.15.35
Finally, a general linear panel regression was employed to examine changes in both psychosocial and physical HRQOL among students identified with a mental disorder. Panel regression permitted examination of the longitudinal data while adjusting for intra-class correlations over time within individuals. Separate regression models examined both student and parent proxy-reported pediatric HRQOL during the three years after the SBHC program. All statistical analyses were conducted using both SPSS®36 and SAS®.37
RESULTS
On average, 37% (range = 20% to 81%) of students who received treatment in the four SBHCs were Medicaid recipients during the study period. ADHD and other mental disorders comprised a large percentage of SBHC encounters along with other diseases such as asthma, otitis media, urinary tract infection, and respiratory disorder.38 The percentage of SBHC encounters for students with mental health problems ranged from 4% to 19%.
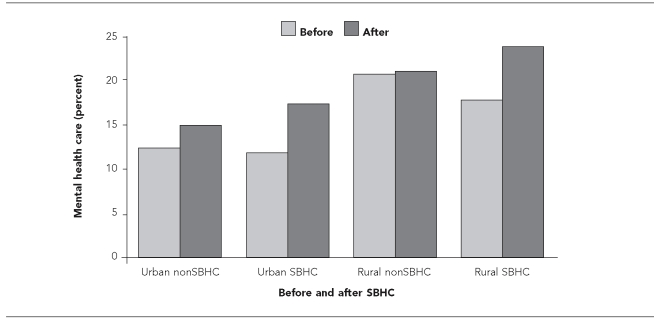
In four SBHC and two non-SBHC schools, 5,057 students (54.7% of total enrolled students) were identified as being in the Ohio Medicaid program. Based on Medicaid medical claims, major mental health problems included ADHD and depressive, conduct, emotion, and adjustment disorders. After the SBHCs opened in September 2000, the proportion of those students who accessed any mental health-care services increased 5.6% (χ2=39.361, p<0.0001) for two urban SBHC schools and increased 5.9% (χ2=5.545, p<0.0001) for one rural SBHC school. Meanwhile the proportion of students who accessed any mental health-care services increased 2.6% (χ2=2.670, p=0.1023) for one urban non-SBHC school and increased 0.2% (χ2=0.006, p=0.9361) for one rural non-SBHC school (Figure 2).
Figure 2. Percentage of students who accessed mental health services before and after SBHC program implementation, by rural and urban areas (n=5,057)a.
aAll data for this figure are based on Medicaid medical claims with diagnosis codes from 1997 to 2003.
Urban nonSBHC = students subtotal in urban schools without SBHC program (n=913); 2.6% changed, χ2=2.670, p=0.1023
Urban SBHC = students subtotal in urban schools with SBHC program (n=3,148); 5.6% changed, χ2=39.361, p<0.0001
Rural nonSBHC = students subtotal in rural schools without SBHC program (n=471); 0.2% changed, χ2=0.006, p=0.9361
Rural SBHC = students subtotal in rural schools with SBHC program (n=525); 5.9% changed, χ2=5.545, p<0.0001
SBHC = school-based health center
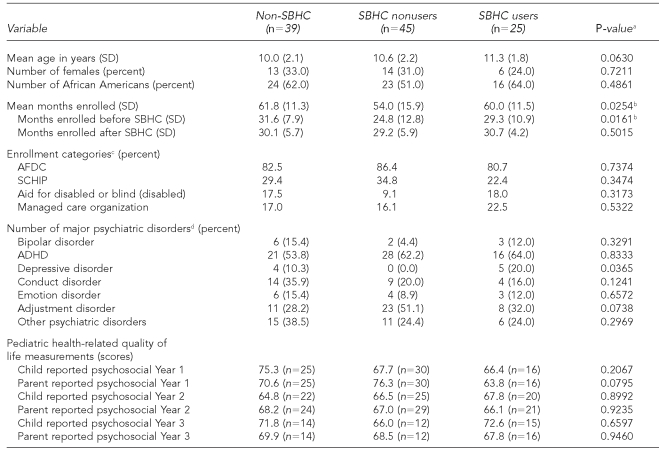
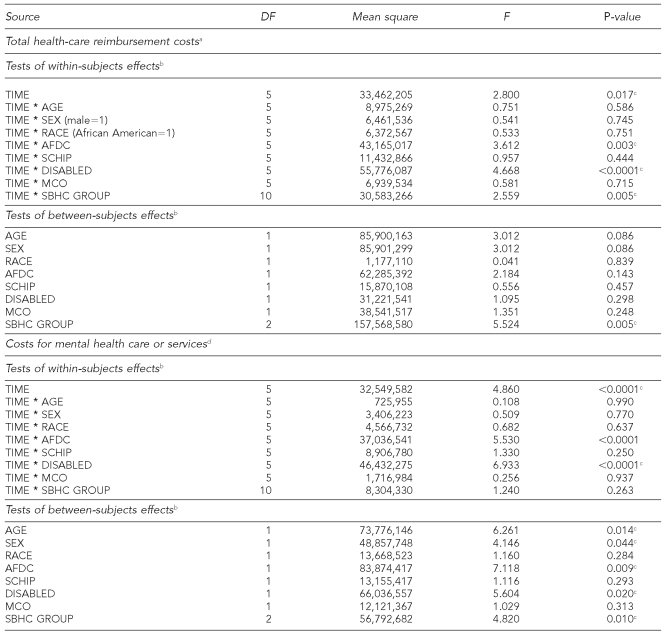
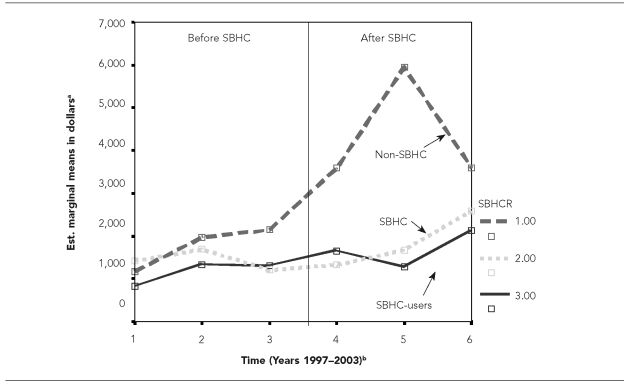
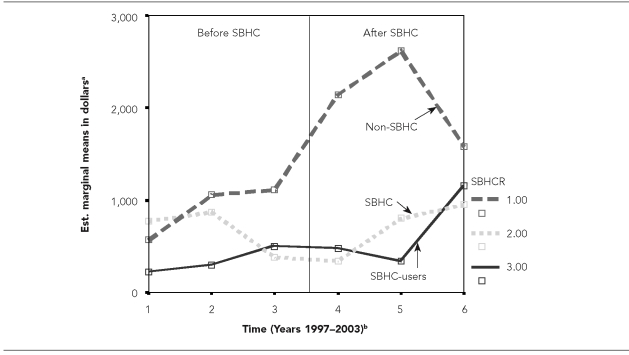
Because many students did not enroll continuously in one school during the study period, we conducted time-series repeated measures ANCOVAs based on 109 students who had both Medicaid medical claims and HRQOL survey measurements. In this cohort, 30.3% were female, 57.8% were African American, and the mean age was 10.5 years (standard deviation [SD] = 2.1) (Table 1). Demographics and characteristics across SBHC users, SBHC nonusers, and comparison schools were similar in terms of age, sex, race, Medicaid enrollment, and psychiatric comorbidities. Repeated measures analyses revealed that there were significant differences in total health-care reimbursements and costs (time, F=2.80, p=0.017) (F =F-statistic value) for mental health-care services (time, F=4.86, p<0.0001) over time after the SBHCs opened in 2000 (Table 2). After controlling the covariates, the interaction term SBHC GROUP*TIME was statistically significant for total health-care reimbursement (F=2.56, p=0.005) indicating a significant difference between groups over time. Both SBHC users and nonusers had lower total health-care reimbursement (F=5.52, p=0.005) and lower costs of mental health service (F=4.82, p=0.010) than students in non-SBHC comparison schools (Table 2, Figures 3 and 4).
Table 1. Demographics and characteristics for students with mental health problems among three groups (SBHC nonusers, SBHC users, and non-SBHC) (n=109).
aComparison among students in non-SBHC schools, SBHC nonusers, and SBHC users using one-way analysis of variance for continuous data such as age, months enrolled, percentages of enrollment categories, and pediatric quality of life scores, and Chi-square tests for other dichotomous variables.
bThere was no statistically significant difference between non-SBHC and SBHC user groups.
cThe percentage of months that a child was enrolled in each category. Students could have been in multiple programs during the study period.
dDiagnosis of mental illnesses was based on primary diagnoses in either institutional or medical office visits for each child during the study period.
SBHC = school-based health center
SD = standard deviation
AFDC = Aid to Families with Dependent Children
SCHIP = State Children's Health Insurance Program
ADHD = attention deficit hyperactivity disorder
Table 2. Repeated measures analysis of covariance of health-care reimbursement costs for students with mental health problems (n=109).
NOTE: SBHC GROUP = 1 for students in non-SBHC schools, SBHC GROUP = 2 for students in SBHC schools, and SBHC GROUP = 3 for students who used SBHCs during the intervention period. Interaction effects between time and covariance variables include TIME*AGE, TIME*SEX, TIME*RACE, TIME*AFDC, TIME*SCHIP, TIME*DISABLED, TIME*MCO, and TIME*SBHC GROUP.
aPrimary dependent variable = total health-care cost (reimbursement amount in 2003 dollars).
bModel design = Intercept + SBHC GROUP + RACE + SEX + AGE + AFDC + DISABLED + SCHIP + MCO. Within-subjects design = TIME.
cStatistically significant at alpha level 0.05
dSecondary dependent variables = costs for mental health services (reimbursement amount in 2003 dollars), costs for prescription drugs, costs for hospitalization, and costs for emergency room visits.
DF = degree of freedom
F = Fisher's test statistic
AFDC = Aid to Families with Dependent Children
SCHIP = State Children's Health Insurance Program
MCO = managed care organization
SBHC = school-based health center
Figure 3. Mean total health-care reimbursement costs per child across SBHC groups over six years (three years before and three years after SBHC implementation) for students with mental disorders (n=109).
aEstimated marginal means are mean total costs per child.
bTimes 1, 2, and 3 refer to 1997, 1998, and 1999—academic years before the SBHC program; Times 4, 5, and 6 refer to 2000, 2001, and 2002—academic years after the SBHC program.
SBHC = school-based health center
SBHCR=1 for students in non-SBHC schools, SBHCR=2 for students in SBHC schools, and SBHCR=3 for students who used SBHCs during the intervention period.
Figure 4. Mean mental health-care reimbursement costs per child across SBHC groups over six years (three years before and three years after SBHC implementation) for students with mental disorders (n=109).
aEstimated marginal means are mean costs for mental health care per child.
bTimes 1, 2, and 3 refer to 1997, 1998, and 1999—academic years before the SBHC program; Times 4, 5, and 6 refer to 2000, 2001, and 2002—academic years after the SBHC program.
SBHC = school-based health center
SBHCR=1 for students in non-SBHC schools, SBHCR=2 for students in SBHC schools, and SBHCR=3 for students who used SBHCs during the intervention period.
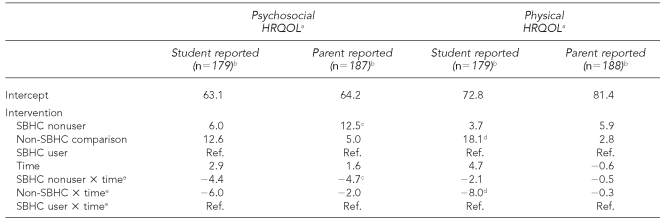
Finally, we regressed pediatric psychosocial and physical HRQOL as reported by both student and parent on SBHC status and time to examine changes among those students with a documented mental health problem. Of the 109 sampled students, only 65%, 61%, and 38% had completed both child-reported and parent-reported HRQOL surveys in academic years 2000, 2001, and 2002, respectively, so we employed a pair-wise deletion algorithm to maintain observations in the models. Pair-wise regression allowed for all cases to remain in the analysis if they had data for at least one year as opposed to a list-wise deletion algorithm that would delete any case from the analysis if it were missing any data in any given year.
Table 1 shows that there were no statistically significant cross-sectional differences among SBHC users, SBHC nonusers, and non-SBHC groups. In the panel regression models in Table 3, the focus is on the interaction between SBHC group and time. For psychosocial HRQOL, parent reports indicated a moderate significant improvement among SBHC users compared with nonusers (p<0.10). While there was a noticeable improvement in the child-reported psychosocial HRQOL among SBHC users over time compared with nonusers and comparison school students, all effects were nonsignificant. Examining physical HRQOL, student SBHC users showed significant improvement over time vs. comparison schools (p<0.05). There was no significant effect for parent-reported pediatric HRQOL.
Table 3. Panel regression analyses of student self-reported and parent proxy-reported psychosocial and physical HRQOL scores on SBHC use.
aRegression coefficients are unstandardized regression coefficients representing unit changes in the pediatric quality of life measure of HRQOL.
bSample size indicates the number of total observations used from a total number of 327 observations (109 respondents 3 3 years) employing a pair-wise deletion method.
cp<0.10
dp<0.05
eReported coefficients are intervention SBHC*TIME interactions with one degree of freedom.
HRQOL = health-related quality of life
SBHC = school-based health center
Ref. = reference category
DISCUSSION
The objectives of this study were to evaluate the effect of SBHCs on total Medicaid reimbursement and on costs for mental health services over time among students with mental health problems. To our knowledge, this study is the first attempt to document the quantitative impact of SBHCs on the total health-care reimbursement cost and HRQOL among students with mental health problems. We proposed a set of hypotheses indicating that access to primary health care through SBHCs would change patterns of use from more expensive, reactive-type care to more preventive, primary care. Moreover, this pattern change would either reduce overall Medicaid costs or be cost-neutral. Both of these hypotheses were supported in this analysis. The final hypothesis indicated that, with this change in care, we would see improvements in pediatric HRQOL among students using the SBHC compared with other students. This hypothesis was only partially supported in this study. We are hesitant to propose any firm conclusions on this specific analysis of HRQOL, however, because the diminished sample size reflects diminished statistical power. SBHCs did appear to have an influence based on student self-rated physical HRQOL and parent-rated pediatric psychosocial HRQOL. In fact, the increases in student self-rated psychosocial HRQOL among the SBHC user group over time was far above what Varni and colleagues33 indicate as a minimal clinical effect of four points HRQOL score change. Moreover, in the full sample, we found a significant SBHC group by time interaction indicating an improvement across all dimensions of student-reported HRQOL over time among SBHC users compared with the comparison school students.27
Implications
These results have several implications. First, SBHCs provide essential and meaningful mental health services and counseling, as was shown in our other study.38 These services may help prevent more costly acute events for students with mental disorders, which indicates that there may be an economic or financial benefit for Medicaid or SCHIP to support SBHCs in providing meaningful mental health services for students. This finding is supported by others as well.16–19 Based on previous research, the need for child mental health services is great.7,39–42 For example, rates of ADHD range from 3% to 6%,41,42 while rates of depressive disorder range from 5% to 15%.40,43
Second, the SBHC model provides essential primary care and mental health services, which increases health-care accessibility for all students. It is unclear why there was a substantial increase in total and mental health costs for students in non-SBHC schools in years four through six, with dramatic peaks for both in year five (Figures 3 and 4). Students may require more total health-care and mental health services as they get older due to adolescent psychiatric comorbid conditions. We have good reason to believe that the difference in use of mental health services that occurred was due to the SBHC intervention because the Ohio Medicaid mental health coverage for all students is the same in the Greater Cincinnati area. But more importantly, the SBHCs reduce barriers to care and offer additional benefits to children from socioeconomically disadvantaged families.10,11 This increased access can help overcome the many barriers to getting health care that differentially affect students from low-income families. According to the recent Kids Count report by the Annie E. Casey Foundation,44 18% of all children in the U.S. in 2005 lived in poverty. This represents approximately 13 million children. Moreover, eight million children do not have health insurance, and two-thirds of uninsured children live below 250% of the federal poverty level. Assuming that each of the current 1,700 SBHCs across the U.S.13 serves about 1,000 students in any given school district, this accounts for only 1.7 million children. This also leaves well in excess of 10 million children without access or severely limited access to primary and preventive health care. And because disadvantaged children are at greatest risk to manifest mental health problems and are more likely not to have them identified due to barriers in accessing proper care, SBHCs are at the front line to provide preventive health services.
While there has been a steady increase in SBHCs since the 1980s, funding resources are limited. Support mostly comes from the federal government, private and public foundations, Medicaid, health insurance companies, and the Healthy Schools/Healthy Communities program of the Bureaus of Primary Health and Maternal and Child Health.45 NASBHC has been instrumental in trying to address funding and has suggested that SBHC services should be covered by SCHIP under Medicaid or related MCOs.46–49
Prevention of costly mental health problems not only has economic implications but also important societal benefits. Many on-campus suicides and massacres involving students with mental health problems have occurred in the past decade.50,51 Many students and teachers have lost their lives in these tragedies. While we do not say that any or all of these tragedies could have been prevented by having an SBHC in the school, they should be a wake-up call for our society to provide appropriate and essential mental health-care services for students regardless of the service delivery system. We would argue, however, that SBHCs appear to be an effective and efficacious system of delivery that addresses the needs of the school population and especially those from low-income families with more barriers to health care.52
Limitations
While this study does provide some insight into the cost and health benefits of SBHCs, there were some limitations. First, this study was limited to school-age children from kindergarten to eighth grade enrolled in both Greater Cincinnati public schools and the Ohio Medicaid program. The final study sample size was relatively small. Therefore, we are unable to generalize these findings to students in high school or college, or to students across other districts in the U.S.
Second, we were dependent on the ICD-9 codes from clinic encounter data to verify accuracy of diagnoses of mental health problems. It is possible that there are some misclassifications of disease diagnoses. Third, because the primary data sources were the HRQOL survey data and Medicaid medical claims database, we were unable to assess students with other insurance plans or no insurance.
Fourth, due to limitations of the Medicaid claims data, we were unable to measure many other clinical parameters of mental health treatment. The pediatric HRQOL scores were used as a proxy to measure the changes of students' physical and psychosocial behaviors. However, with the high numbers of missing observations, the statistical power to examine changes in HRQOL across groups may be insufficient, making us cautious about these findings. Further investigation is also warranted to assess the relationship between the SBHC program and students' school attendance and academic performance.
CONCLUSION
SBHCs appear to play a significant role in providing valuable mental health services for students in many schools. The accessibility of mental health services increased significantly for students after the implementation of an SBHC program, while the total health-care reimbursement cost for students remained lower than that of students in non-SBHC schools. As such, SBHCs should be seen as a viable, effective, and efficacious health service delivery model to help address a lack of mental health services and barriers to accessing timely care for disadvantaged students.
Acknowledgments
The authors are grateful to Patricia O'Connor and Ann McCracken (The Health Foundation of Greater Cincinnati), the Ohio Department of Jobs and Family Services, and to Tracy Huentelman and Kristin Line. The authors also thank Raymond Jang, Robert Cluxton, Thomas Young, Kathleen E. Adams, Arthur Kendall, Linda Juszczak, Daniel Mullins, John Schlitt, Melvin Mark, and Anand Desai for their expert consultations and comments on the research design and data analyses; Wei Pan, Mark Carrozza, Mona Ho, Gregory Roth, and Beth-Ann Witherow for their data programming and statistical support; and Sharmane Guo and Christine Mulvin for editorial support.
Footnotes
This research was funded by a grant from The Health Foundation of Greater Cincinnati. Terrance Wade is supported by the Canada Research Chairs program.
REFERENCES
- 1.Wade TJ, Cairney J. General issues: sociological contributions. In: Ammerman RT, Hersen M, Thomas JC, editors. Comprehensive handbook of personality and psychopathology, volume 3. Child psychopathology. New York: John Wiley & Sons; 2006. pp. 47–63. [Google Scholar]
- 2.Rutter M. Why are London children so disturbed? Proc R Soc Med. 1973;66:1221–5. doi: 10.1177/003591577306601231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Langner TS, Gersten JC, Greene EL, Eisenberg JG, Herson JH, McCarthy ED. Treatment of psychological disorders among urban children. J Consult Clin Psychol. 1974;42:170–9. doi: 10.1037/h0036249. [DOI] [PubMed] [Google Scholar]
- 4.Langner TS, McCarthy ED, Gersten JC, Simcha-Fagan O, Eisenberg JG. Factors in children's behaviour and mental health over time: the family research project. In: Simmons RG, editor. Research in community and mental health. Greenwich (CT): JAI Press; 1979. pp. 127–81. [Google Scholar]
- 5.Srole L, Langer TS, Michael ST, Opler MK, Rennie TAC. Mental health in the metropolis: the midtown Manhattan study. New York: McGraw Hill; 1962. [Google Scholar]
- 6.Offord DR, Boyle MH, Jones BR. Psychiatric disorder and poor school performance among welfare children in Ontario. Can J Psychiatry. 1987;32:518–25. doi: 10.1177/070674378703200704. [DOI] [PubMed] [Google Scholar]
- 7.Offord DR, Boyle MD, Racine Y. Ontario Child Health Study: correlates of disorder. J Am Acad Child Adolesc Psychiatry. 1989;28:856–60. doi: 10.1097/00004583-198911000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Ezpeleta L, Keeler G, Erkanli A, Costello EJ, Angold A. Epidemiology of psychiatric disability in childhood and adolescence. J Child Psychol Psychiatry. 2001;42:901–14. doi: 10.1111/1469-7610.00786. [DOI] [PubMed] [Google Scholar]
- 9.Nyborg VM, Curry JF. The impact of perceived racism: psychological symptoms among African American boys. J Clin Child Adolesc Psychol. 2003;32:258–66. doi: 10.1207/S15374424JCCP3202_11. [DOI] [PubMed] [Google Scholar]
- 10.Newacheck PW, McManus MA, Gephart J. Health insurance coverage of adolescents: a current profile and assessment of trends. Pediatrics. 1992;90:589–96. [PubMed] [Google Scholar]
- 11.Brindis C, Kapphahn C, McCarter V, Wolfe AL. The impact of health insurance status on adolescents' utilization of school-based clinic services: implications for health care reform. J Adolescent Health. 1995;16:18–25. doi: 10.1016/1054-139X(95)94069-K. [DOI] [PubMed] [Google Scholar]
- 12.Senate Committee on Homeland Security and Governmental Affairs (US) Juvenile detention centers: are they warehousing children with mental illness? 2004. Jul 7, [cited 2007 May 10]. Available from: URL: http://hsgac.senate.gov/index.cfm?Fuseaction=Hearings.Detail&HearingID=186.
- 13.Juszczak L, Schlitt J, Moore A. School-based health centers: national census school year 2004-05. Washington: National Assembly on School-Based Health Care; 2007. [Google Scholar]
- 14.Schlitt J, Santelli J, Juszczak L, Brindis C, Nystrom R, Klein J, et al. Creating access to care for children and youth: school-based health center census 1998-1999. Washington: National Assembly on School-Based Health Care; 2000. [Google Scholar]
- 15.Young TL, D'angelo SL, Davis J. Impact of a school-based health center on emergency department use by elementary school students. J Sch Health. 2001;71:196–8. doi: 10.1111/j.1746-1561.2001.tb07316.x. [DOI] [PubMed] [Google Scholar]
- 16.Adams EK, Johnson V. An elementary school-based health clinic: can it reduce Medicaid costs? Pediatrics. 2000;105:780–8. doi: 10.1542/peds.105.4.780. [DOI] [PubMed] [Google Scholar]
- 17.Guo JJ, Jang R, Keller KN, McCracken AL, Pan W, Cluxton RJ. Impact of school-based health centers on children with asthma. J Adolesc Health. 2005;37:266–74. doi: 10.1016/j.jadohealth.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan DW, Brindis CD, Phibbs SL, Melinkovich P, Naylor K, Ahlstrand K. A comparison study of an elementary school-based health center: effects on health care access and use. Arch Pediatr Adolesc Med. 1999;153:235–43. doi: 10.1001/archpedi.153.3.235. [DOI] [PubMed] [Google Scholar]
- 19.Kaplan DW, Calonge BN, Guernsey BP, Hanrahan MB. Managed care and school-based health centers: use of health services. Arch Pediatr Adolesc Med. 1998;152:25–33. doi: 10.1001/archpedi.152.1.25. [DOI] [PubMed] [Google Scholar]
- 20.Meeker RJ, DeAngelis C, Berman B, Freeman HE, Oda D. A comprehensive school health initiative. Image J Nurs Sch. 1986;18:86–91. doi: 10.1111/j.1547-5069.1986.tb00552.x. [DOI] [PubMed] [Google Scholar]
- 21.Fisher M, Juszczak L, Friedman SB, Schneider M, Chapar G. School-based adolescent health care: review of a clinical service. Am J Dis Child. 1992;146:615–21. doi: 10.1001/archpedi.1992.02160170095023. [DOI] [PubMed] [Google Scholar]
- 22.Balassone ML, Bell M, Peterfreund N. A comparison of users and nonusers of a school-based health and mental health clinic. J Adolesc Health. 1991;12:240–6. doi: 10.1016/0197-0070(91)90017-g. [DOI] [PubMed] [Google Scholar]
- 23.Walter HJ, Vaughan RD, Armstrong B, Krakoff RY, Tiezzi L, McCarthy JF. School-based health care for urban minority junior high school students. Arch Pediatr Adolesc Med. 1995;149:1221–5. doi: 10.1001/archpedi.1995.02170240039006. [DOI] [PubMed] [Google Scholar]
- 24.Weist MD, Paskewitz DA, Warner BS, Flaherty LT. Treatment outcome of school-based mental health services for urban teenagers. Community Ment Health J. 1996;32:149–57. doi: 10.1007/BF02249752. [DOI] [PubMed] [Google Scholar]
- 25.Anglin TM, Naylor KE, Kaplan DW. Comprehensive school-based health care: high school students' use of medical, mental health, and substance abuse services. Pediatrics. 1996;97:318–30. [PubMed] [Google Scholar]
- 26.Office of the Surgeon General (US) Mental health: a report of the Surgeon General. Washington: Department of Health and Human Services (US); 1999. [cited 2008 Jul 1]. Available from: URL: http://www.surgeongeneral.gov/library/mentalhealth/home.html. [Google Scholar]
- 27.Wade TJ, Line K, Huentelman T. A prescription for success: how school-based health centers affect health status and health care use and cost. Cincinnati: The Health Foundation of Greater Cincinnati; 2005. School-based health centers (SBHC) evaluation project. [Google Scholar]
- 28.Guo JJ, Jang R, Cluxton RJ. A prescription for success: how school-based health centers affect health status and health care use and cost. Cincinnati: Health Foundation for Greater Cincinnati; 2004. Evaluation of health outcomes and costs among Medicaid recipients enrolled in school-based health centers. [Google Scholar]
- 29.Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care. 1999;37:126–39. doi: 10.1097/00005650-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Drummond MF, O'Brien BJ, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programs. New York: Oxford University Press; 1997. pp. 52–96. [Google Scholar]
- 31.Bureau of Labor Statistics (US) Consumer price index for all urban consumers, 1997, 1998, 1999, 2000, 2001, 2002. Washington: Department of Labor (US); [cited 2003 Jun 30]. Available from: URL: http://www.bls.gov/cpi/home.htm. [Google Scholar]
- 32.Bureau of Labor Statistics (US) Medical care inflation continues to rise. Washington: Department of Labor (US); 2001. May 29, [cited 2003 Jun 30]. Available from: URL: http://www.bls.gov/opub/ted/2001. [Google Scholar]
- 33.Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3:329–41. doi: 10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 34.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–12. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Stevens JP. Applied multivariate statistics for the social sciences. 4th ed. New York: Routledge; 2001. pp. 510–1. [Google Scholar]
- 36.SPSS Inc. SPSS: Version 11.0 for Windows. Chicago: SPSS Inc.; 2005. [Google Scholar]
- 37.SAS Institute Inc. SAS: Version 9.1 for Windows. Cary (NC): SAS Institute Inc.; 2005. [Google Scholar]
- 38.Wade TJ, Mansour ME, Guo JJ, Huentelman T, Line K, Keller KN. Access and utilization patterns of school-based health centers at urban and rural elementary and middle schools. Public Health Rep. 2008;123:739–50. doi: 10.1177/003335490812300610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grupp-Phelan J, Wade TJ, Pickup T, Ho ML, Lucas CP, Brewer DE, et al. Mental health problems in children and caregivers in the emergency department setting. J Dev Behav Pediatr. 2007;28:16–21. doi: 10.1097/dbp.0b013e31802d0bb2. [DOI] [PubMed] [Google Scholar]
- 40.Smucker MR, Craighead WE, Craighead LW, Green BJ. Normative and reliability data for the Children's Depression Inventory. J Abnorm Child Psychol. 1986;14:25–39. doi: 10.1007/BF00917219. [DOI] [PubMed] [Google Scholar]
- 41.Richters JE, Arnold LE, Jensen PS, Abikoff H, Conners CK, Greenhill LL, et al. NIMH collaborative multisite multimodal treatment study of children with ADHD: I. Background and rationale. J Am Acad Child Adolesc Psychiatry. 1995;34:987–1000. doi: 10.1097/00004583-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 42.Goldman LS, Genel M, Bezman RJ, Slanetz PJ. Diagnosis and treatment of attention-deficit/hyperactivity disorder in children and adolescents. JAMA. 1998;279:1100–7. doi: 10.1001/jama.279.14.1100. [DOI] [PubMed] [Google Scholar]
- 43.Wade TJ, Cairney J, Pevalin DJ. The emergence of gender differences in depression during adolescence: national panel results from three countries. J Am Acad Child Adolesc Psychiatry. 2002;41:190–8. doi: 10.1097/00004583-200202000-00013. [DOI] [PubMed] [Google Scholar]
- 44.Annie E Casey Foundation. Report on school-based health centers. Baltimore (MD): Annie E. Casey Foundation; 2006. [Google Scholar]
- 45.Lear JG. Health at school: a hidden health care system emerges from the shadows. Health Aff (Millwood) 2007;26:409–19. doi: 10.1377/hlthaff.26.2.409. [DOI] [PubMed] [Google Scholar]
- 46.Mental Health in Schools Act of 2007 (S. 1332/H.R. 3430) Washington: 2007. [cited 2008 Jul 1]. Available from: URL: http://www.govtrack.us/congress/bill.xpd?bill=s110-1332. [Google Scholar]
- 47.Healthy Schools Act of 2007 (S. 1669/H.R. 2870) Washington: 2007. [cited 2008 Jul 1]. Available from: URL: http://www.govtrack.us/congress/bill.xpd?bill=h110-2870. [Google Scholar]
- 48.Protecting Children's Health in Schools Act of 2007 (S. 578/H.R. 1017) Washington: 2007. [cited 2008 Jul 1]. Available from: URL: http://www.govtrack.us/congress/bill.xpd?bill=h110-1017. [Google Scholar]
- 49.School-Based Health Clinic Establishment Act of 2007 (S. 600/H.R. 4230) Washington: 2007. [cited 2008 Jul 1]. Available from: URL: http://www.govtrack.us/congress/bill.xpd?bill=s110-600. [Google Scholar]
- 50.CNN News. Hearing today for 2 boys in Arkansas shooting. 1998. Mar 25, [cited 2008 Jul 1]. Available from: URL: http://www.cnn.com/US/9803/25/school.shooting.
- 51.Bazar E, Bello M. Investigators seek motive for Ohio school shooting. USA Today. 2007. Oct 11, [cited 2008 Jul 1]. Available from: URL: http://www.usatoday.com/news/nation/2007-10-10-school-shooting_N.htm.
- 52.Wade TJ, Mansour ME, Line K, Huentelman T, Keller KN. Improvements in health-related quality of life among school-based health center users in elementary and middle school. Ambul Pediatr. 2008;8:241–9. doi: 10.1016/j.ambp.2008.02.004. [DOI] [PubMed] [Google Scholar]