Abstract
Background
The contemporary magnitude and prognostic implications of complete heart block (CHB) in patients with acute myocardial infarction (AMI) are unknown. As part of a community-based study of patients hospitalized with AMI in the Worcester, Massachusetts, metropolitan area, changes over time in the incidence rates of CHB complicating AMI, and the prognostic impact of CHB on short-term survival, were examined.
Methods
The study population consisted of 13,663 residents of the Worcester metropolitan area hospitalized with AMI at all greater Worcester medical centers during 15 annual periods between 1975 and 2005.
Results
The average age of the hospitalized study sample was 69 years and 58% were men. The overall proportion of patients with AMI who developed CHB was 4.1%. The incidence rates of CHB complicating AMI declined appreciably over time, with the greatest decline in these incidence rates occurring during the most recent years under study. In 2005, 2.0% of patients hospitalized with AMI developed CHB compared to 5.1 % in the initial study year of 1975. Patients with AMI who developed CHB had higher in-hospital death rates (43.2%) than did those who did not develop CHB (13.0%) (p<.001). The hospital death rates associated with CHB declined appreciably over time, particularly during the most recent years under study. Several patient characteristics were associated with an increased risk for developing CHB during hospitalization for MI.
Conclusions
Our findings indicate recent encouraging declines in the incidence rates of CHB complicating AMI and improving trends in the hospital prognosis of these patients.
Introduction
Complete heart block (CHB) is an important clinical complication in patients hospitalized with acute myocardial infarction (AMI). Prior studies have suggested that approximately 4% to 7% of patients hospitalized with AMI will develop CHB1–5. Hospital death rates in patients who develop CHB have consistently been shown to be higher in comparison to those who do not develop this conduction abnormality1–10.
A limited number of studies have examined changing trends in the incidence rates of CHB in the setting of AMI, particularly from the more generalizable perspective of a population-based investigation and during recent periods. An observational study in Israel showed a slight reduction in the incidence rates of CHB between the early 1980’s and the mid-1990’s in patients hospitalized with AMI in coronary care units throughout this country3. In a previous publication from the Worcester Heart Attack Study, we demonstrated that the hospital incidence rates of CHB in greater Worcester residents hospitalized with AMI declined over varying time intervals beginning in the mid-1970’s1,2.
While CHB is associated with a poor hospital prognosis after AMI1–6, few studies have examined whether the short-term prognosis associated with CHB has changed during recent periods, particularly as the management of patients with AMI continues to evolve. Moreover, most prior studies that have examined the magnitude and/or outcomes associated with CHB have been conducted in single hospital settings with small sample sizes, raising questions about the generalizability of the study findings.
The objectives of the present study are to extend our earlier findings from the Worcester Heart Attack Study1,2 and examine the overall magnitude and impact, as well as 30 year trends (1975–2005), in the incidence and hospital case-fatality rates associated with CHB in residents of a large New England metropolitan area hospitalized with AMI. Data from the Worcester Heart Attack Study, a population-based epidemiologic investigation, were utilized11–14.
Methods
The Worcester Heart Attack Study is an ongoing population-based investigation that is describing the clinical epidemiology of AMI among residents of the Worcester metropolitan area hospitalized at all 16 greater Worcester (MA) medical centers11–14. Fewer hospitals (n=11) have been included during recent study years due to hospital closures, mergers, or conversion to chronic care facilities. The details of this study have been described previously11–14. In brief, the medical records of residents of the Worcester metropolitan area (2000 census estimate = 478,000) hospitalized for possible AMI at all greater Worcester medical centers were individually reviewed. These patients were identified through the use of passive disease surveillance at each participating medical center. This entailed the review of computerized hospital discharge diagnosis databases and review of coronary care unit logs.
The diagnosis of AMI was validated according to the presence of 2 out of 3 predefined criteria. These criteria consisted of the presence of clinical findings consistent with a diagnosis of AMI, serial changes in the electrocardiogram consistent with an evolving MI, and increases in the serum levels of various cardiac enzymes. Troponin assays were adopted for use in the confirmation of AMI on a more widespread basis for patients hospitalized with AMI in 2003 and 2005 as these assays were not introduced to general hospital practice during earlier study years.
Data have been collected in this observational study on an approximate biennial basis since the initial study year of 1975, and continuing to the most recent year of investigation in 2005. The study years were originally selected due to funding availability and for purposes of examining changing trends in our principal study outcomes on an approximate alternate yearly basis. Patients who developed AMI secondary to an interventional procedure or surgery were excluded.
Data Collection
Demographic, medical history, and clinical data were abstracted from the hospital medical records of geographically eligible patients with confirmed AMI by trained study physicians and nurses. Information was collected about patient's age, sex, race, height and weight, comorbidities (e.g., angina, diabetes, hypertension, heart failure, stroke), AMI order (initial vs. prior), type (Q wave vs. non–Q wave), and location (anterior vs inferior/posterior), receipt of hospital medications and coronary interventional procedures, and hospital discharge status. Information was collected about the occurrence of clinically significant hospital complications including stroke, heart failure, atrial fibrillation, and cardiogenic shock. Complete heart block was defined according to standard electrocardiographic criteria that included the absence of atrioventricular conduction on at least one 12-lead electrocardiogram with the atrial rate greater than the ventricular rate1,2. Printouts of continuous cardiac monitoring strips documenting CHB were also reviewed by our trained data abstractors. A physician diagnosis of CHB as recorded in participating hospitals medical records was required for the confirmation of CHB in conjunction with electrocardiographic confirmation. Due to our methods of data abstraction, we were unable to determine the duration of CHB or the different etiologies possibly contributing to the development of CHB (e.g., reperfusion related).
Data Analysis
We examined differences in the demographic and clinical characteristics, treatment practices, and hospital outcomes between patients who developed CHB during hospitalization for AMI as compared to those who did not develop this conduction disturbance through the use of chi square and t tests for discrete and continuous variables, respectively.
We examined the association between CHB and hospital mortality using multivariable regression analysis to control for the influence of several potentially confounding factors. Candidate variables for inclusion in the regression models included patient’s age, sex, prior comorbidities, AMI associated characteristics, medications received during hospitalization, and coronary interventional procedures (including cardiac pacing). Candidate variables associated with the outcomes of interest (p<0.25 after univariate analysis) were included in our regression models. Variables with a p value >0.05 were eliminated in a stepwise fashion so that only variables with a statistically significant association with the outcome of interest were included in the final regression models.
Trends in the incidence and hospital death rates associated with CHB were also examined in a similar manner using logistic regression analysis, simultaneously controlling for a variety of demographic and clinical factors that may have either affected the risk of developing, or dying after, CHB.
Results
A total of 13,663 greater Worcester residents were hospitalized with AMI over the 30 year period under study (1975–2005). The average age of the study sample was 69 years, 58% were men, and the majority (95%) were Caucasian. Across all study years, 4.1% of greater Worcester residents hospitalized with AMI developed CHB.
Baseline characteristics
Overall, patients with CHB were significantly less likely to have a prior history of angina, but were more likely to have a history of diabetes, in comparison to those without CHB (Table I). Complete heart block was more likely to occur in patients with a Q wave MI and in those with an inferior/posterior MI. Patients who developed CHB were more likely to report nausea, diaphoresis, but less likely to report dyspnea, at hospital presentation in comparison to those did not develop CHB. Patients with CHB had significantly lower blood pressures, but higher average serum glucose findings, at the time of hospital admission. Patients with CHB were more likely to be hospitalized for a longer duration than patients without CHB (Table I).
Table I.
Characteristics of Patients With Acute Myocardial Infarction (AMI) According to the Presence of Complete Heart Block (CHB): Worcester Heart Attack Study
| CHB |
|||
|---|---|---|---|
| Characteristics | Present (+) (n=565)† | Absent (−) (n=13098)† | |
| P value | |||
| Age (mean, yrs) | 69.8 | 68.9 | 0.11 |
| Men | 311 (55.1) | 7680 (58.6) | 0.09 |
| Caucasian | 530 (95.7) | 12028 (95.2) | 0.36 |
| Body mass index (mean)˚ | 26.4 ± 5.8 | 27±5.9 | 0.06 |
| Medical history | |||
| Angina pectoris | 114 (20.2) | 3291 (25.1) | 0.008 |
| Hypertension | 307 (54.3) | 7562 (57.8) | 0.11 |
| Heart failure | 99 (17.5) | 2503 (19.1) | 0.35 |
| Diabetes mellitus | 180 (31.9) | 3658 (27.9) | 0.04 |
| Stroke | 45 (8.0) | 1287 (9.8) | 0.14 |
| AMI characteristics | |||
| Initial | 381 (67.4) | 8517 (65.0) | 0.24 |
| Q wave | 373 (66.0) | 5200 (39.7) | <0.001 |
| Inferior/posterior | 429 (75.9) | 8748 (66.8) | <0.001 |
| Acute symptoms* | |||
| Any chest pain | 94 (69.1) | 3811 (72.6) | 0.37 |
| Nausea | 56 (41.2) | 1635 (31.2) | 0.013 |
| Dyspnea | 65 (47.8) | 3052 (58.1) | 0.016 |
| Diaphoresis | 64 (47.1) | 1968 (37.5) | 0.023 |
| Hospital admission findings (mean, mm Hg) | |||
| Systolic blood pressure | 125 ± 38 | 143 ± 34 | <0.001 |
| Diastolic blood pressure | 68 ± 22 | 78 ± 21 | <0.001 |
| Laboratory tests (mean, mg/dl)** | |||
| Serum creatinine | 1.6 ± 1.1 | 1.5 ± 2.2 | 0.16 |
| Blood urea nitrogen | 28 ± 21 | 26 ± 20 | 0.09 |
| Serum glucose | 207 ± 129 | 184 ± 132 | 0.02 |
| Cholesterol | 202 ± 59 | 208 ± 58 | 0.06 |
| Length of stay (mean, days) Medication | 12 ±12 | 10±9 | 0.37 |
| ACE Inhibitors** | 128 (22.7) | 4004 (30.6) | <0.001 |
| Aspirin | 291 (51.5) | 8566 (65.4) | <0.001 |
| β Blockers | 227 (40.2) | 8229 (62.8) | <0.001 |
| Calcium channel blockers∞ | 117 (28.1) | 4017 (37.8) | <0.001 |
| Digoxin | 138 (24.4) | 3397 (25.9) | 0.42 |
| Diuretics | 269 (47.6) | 6262 (47.8) | 0.93 |
| Thrombolytic therapy∞ | 87 (22.9) | 1570 (15.8) | <0.001 |
| Procedure | |||
| Cardiac catheterization | 152 (26.9) | 4089 (31.2) | 0.03 |
| Coronary artery bypass surgery∞ | 12 (2.6) | 464 (4.0) | 0.10 |
| Coronary angioplasty∞ | 84 (22.1) | 1970 (19.8) | 0.28 |
| Pacing | |||
| Temporary | 302 (53.6) | 542 (4.1) | <0.001 |
| Permanent/both | 57 (10.1) | 468 (3.6) | |
Data available from 1995 to 2005.
Data available from 1997 to 2005.
Data available from 1990 to 2005.
Data available from 1986 to 2005.
Values are shown as n (%) unless labeled otherwise.
Patients with CHB were significantly less likely to be treated with a number of effective cardiac medications and undergo cardiac catheterization compared to patients who did not develop CHB during their hospitalization (Table I). On the other hand, patients with CHB were more likely to receive thrombolytic therapy and cardiac pacing compared to those without CHB.
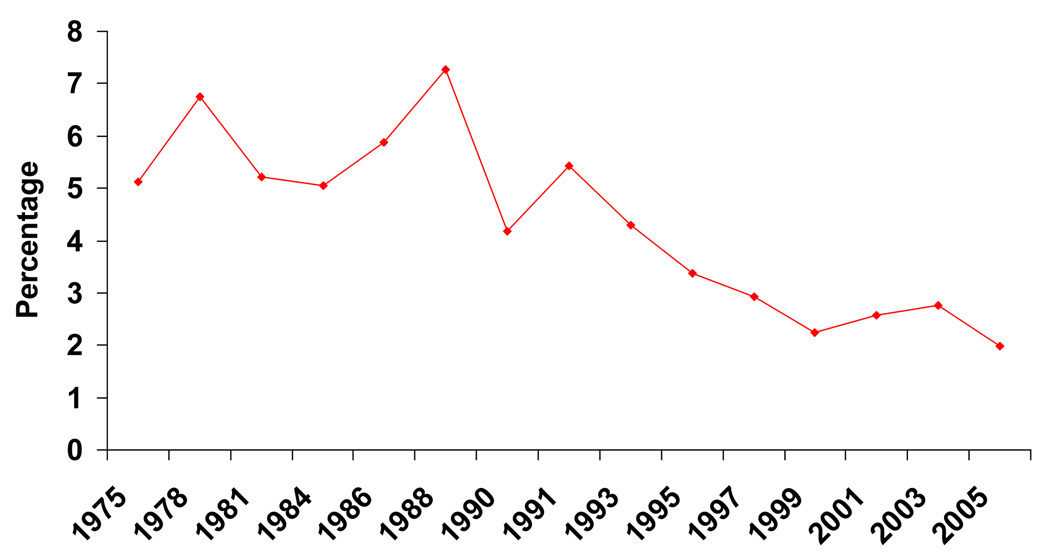
Incidence Rates of Complete Heart Block
The incidence rates of CHB declined appreciably over time with the greatest decline in these incidence rates occurring between the early 1990’s and 2005 (Figure 1).
Figure 1.
Incidence Rates of Complete Heart Block (CHB) Complicating Acute Myocardial Infarction
The demographic as well as clinical characteristics of greater Worcester residents hospitalized with AMI at all area medical centers have changed over time14. Patients hospitalized during recent years of this community-based study were older (mean age = 65 years in 1975/78; mean age = 72 years in 2003/05), more likely to be women (38% women in 1975/78; 46% women in 2003/05), and to have a greater prevalence of major comorbidities previously diagnosed14. Due to this changing patient profile, we carried out a multivariable adjusted regression analysis for purposes of examining changing trends in the incidence rates of CHB while controlling for a variety of potentially confounding factors that might affect the risk of developing CHB. The results of this analysis confirmed our previously observed univariate findings revealing marked declines in the incidence rates of CHB during the most recent years under study (Table II). We also examined changing trends in the incidence rates of CHB in a variety of demographic and clinical subgroups of interest. Recent declines in the incidence rates of CHB were apparent in patients of different ages, men and women, those with selected comorbidities, as well as in those with various AMI associated characteristics (data not shown). The incidence rates of CHB in patients hospitalized with AMI in our most recent study cohort of 2005 were not significantly different in patients with (1.9%), as compared to those without (2.2%), positive troponin findings.
Table II.
Association Between Time Period of Hospitalization and Occurrence of Complete Heart Block Complicating Acute Myocardial Infarction (AMI): Worcester Heart Attack Study
| Crude Odds Ratios (ORs) (95%CI) |
Adjusted ORs (95%CI)** |
|
|---|---|---|
| Study year(s) | ||
| 1975/1978˚ | 1.0˚ | 1.0˚ |
| 1981/1984 | 0.85 (0.64,1.15) | 0.88 (0.65,1.20) |
| 1986/1988 | 1.10 (0.82,1.48) | 1.24 (0.91,1.68) |
| 1990/1991 | 0.80 (0.59,1.09) | 0.88 (0.64,1.21) |
| 1993/1995 | 0.63 (0.46,0.86) | 0.76 (0.55,1.05) |
| 1997/1999 | 0.42 (0.30,0.59) | 0.48 (0.33,0.68) |
| 2001/2003 | 0.43 (0.31,0.60) | 0.54 (0.38,0.76) |
| 2005 | 0.32 (0.19,0.53) | 0.38 (0.22,0.65) |
Referent period
Adjusted for age, sex, race, history of cardiovascular disease, AMI order, type, and location, and clinical complications during hospitalization (e.g., heart failure, stroke, or atrial fibrillation)
Hospital Complications and Case-Fatality Rates
Patients with CHB were more likely to develop significant clinical complications during the index hospitalization including left heart failure, cardiogenic shock, and atrial fibrillation in comparison to those who did not develop CHB (Table III). Complete heart block remained independently associated with an increased risk of dying during hospitalization for AMI, as well as with the occurrence of heart failure, cardiogenic shock, and atrial fibrillation, after controlling for other important risk and prognostic factors (Table V). Adjusting for various comorbidities and AMI associated characteristics attenuated, but did not eliminate, the increased risk of developing each of these hospital endpoints.
Table III.
Hospital Complications of Acute Myocardial Infarction (AMI) According to the Presence of Complete Heart Block (CHB): Worcester Heart Attack Study
| CHB |
||||
|---|---|---|---|---|
| Complication | Present (+) (n=565)† | Absent (−) (n=13,098)† | Multivariable Adjusted OR* | Multivariable Adjusted OR∞ |
| Left Heart Failure | 290 (51.3) | 5111 (39.0) | 1.53 (1.28,1.83)** | 1.25 (1.03,1.53)** |
| Cardiogenic Shock | 142 (25.1) | 763 (5.8) | 5.34 (4.34,6.58) | 2.38 (1.87,3.03) |
| Stroke˚ | 8 (2.1) | 155 (1.6) | 1.49 (0.72,3.06) | 1.03 (0.47,2.25) |
| Atrial Fibrillation | 150 (26.6) | 2193 (16.7) | 1.84 (1.51,2.25) | 1.24 (1.00,1.55) |
| Death | 244 (43.2) | 1702 (13.0) | 4.99 (4.13,6.01) | 2.86 (2.32,3.53) |
Data available from 1986–2005.
Adjusted for age, sex, race, and study year.
Adjusted for age, sex, race, study year, history of cardiovascular disease, AMI type, order, and location, and cardiac pacing.
95% confidence intervals.
Values are shown as n (%) unless labeled otherwise.
Since the length of hospital stay has declined appreciably in patients hospitalized with AMI at all greater Worcester medical centers over the periods under study (mean = 18 days in 1975; mean= 5 days in 2005), we also examined the overall impact of CHB on 30 day death rates after hospital admission. The 30 day all-cause mortality rates after hospital admission were 43.4% for patients with, and 15.3% for patients without, CHB over our entire study period, paralleling the results of our overall hospital mortality findings.
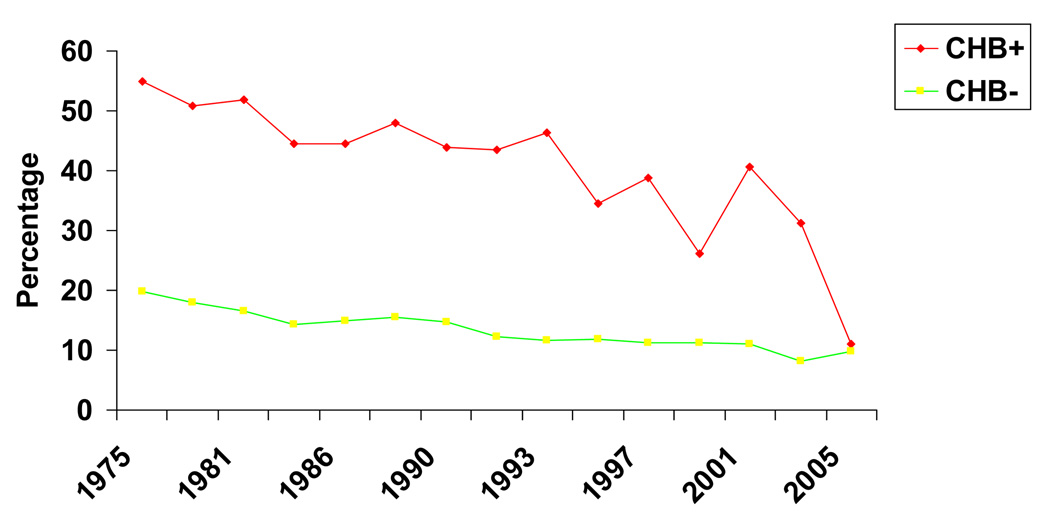
Since 1975, hospital death rates have declined in patients with, as well as in those without, CHB over the period under study but to a greater extent in patients with CHB (Figure 2). A multivariable adjusted regression analysis was performed for purposes of examining changing trends in hospital death rates due to CHB over the years under study while controlling for the changing characteristics of our patient population. Declining trends in hospital CFR’s were observed in patients with CHB, particularly from the mid-1990’s on in comparison to the baseline period (1975/1978) after controlling for several demographic and clinical factors of prognostic importance (Table IV). Similarly, declining trends in hospital CFR’s were observed for patients with an anterior as well as in those with an inferior/posterior MI. For example, in 1975/78, approximately 46% of patients with an inferior/posterior MI who developed CHB died during hospitalization compared to 23% of those with an inferior/posterior MI complicated by CHB during our 2 most recent study years of 2003/2005.
Figure 2.
Hospital Case-Fatality Rates (CFR) According to the Presence of Complete Heart Block (CHB) in Patients Hospitalized With Acute Myocardial Infarction
Table IV.
Association between Time Period of Hospitalization and Hospital Case-Fatality Rates in Patients Developing Complete Heart Block Complicating Acute Myocardial Infarction
| Study year(s) | Crude Odds Ratios (ORs) ( 95%CI) | Adjusted ORs (95%CI)* |
|---|---|---|
| 1975/1978˚ | 1.0˚ | 1.0˚ |
| 1981/1984 | 0.86 (0.48,1.54) | 0.74 (0.39,1.40) |
| 1986/1988 | 0.78 (0.44,1.37) | 0.60 (0.31,1.15) |
| 1990/1991 | 0.70 (0.39,1.27) | 0.54 (0.28,1.06) |
| 1993/1995 | 0.63 (0.34,1.16) | 0.49 (0.25,0.96) |
| 1997/1999 | 0.45 (0.23,0.90) | 0.39 (0.18,0.84) |
| 2001/2003 | 0.51 (0.27,0.97) | 0.36 (0.17,0.76) |
| 2005 | 0.11 (0.03,0.52) | 0.13 (0.03,0.67) |
Referent period
Adjusted for age, sex, race, history of cardiovascular disease, AMI order, type, and location, cardiac pacing, and hospital complications (e.g., heart failure, cardiogenic shock, atrial fibrillation
We also examined changing 30 day total mortality rates after hospital admission, separately for patients with and without CHB, due to previously observed declines in the average length of hospital stay during the periods under study. The 30 day death rates after hospital admission were 48.7% and 17.4%, respectively, for patients with and without CHB during the mid- 1970’s through mid-1980’s (1975–1984) and 33.3% and 13.9% for patients hospitalized between 1999 and 2005, with and without CHB, respectively.
Discussion
The results of this observational study in residents of a large New England metropolitan area hospitalized at all area medical centers with AMI demonstrate declining trends in both the incidence and hospital death rates of CHB over the 30 year period under investigation.
Characteristics of Patients With Complete Heart Block
In our study, patients with CHB had a different profile of selected comorbidities, physiologic findings, and AMI associated characteristics than patients who did not develop CHB.
In the present study, there were, however, no significant differences in the demographic characteristics of patients who did and did not develop CHB in the setting of AMI. These findings differ from the results of our earlier investigations in which greater Worcester residents hospitalized with CHB were older and included more women than patients without CHB1,2. In a study in Israel which compared the characteristics of more than 3,300 patients hospitalized with AMI throughout Israel between 1992 and 1996, with nearly 5,800 patients who were hospitalized with AMI throughout Israel in the early 1980’s, patients with CHB were older and were more likely to be women3. Findings from the TIMI II study also suggest that patients with heart block were slightly older than those who did not develop this conduction disturbance9.
In our study, patients with CHB were less likely to have had angina previously diagnosed, but were more likely to have had diabetes previously diagnosed, compared to patients who did not develop CHB. These findings are consistent with our earlier work1,2 but differ slightly from the study in Israel which suggested that patients with CHB were more likely to have a history of angina, but less likely to have a history of diabetes3. Our findings are consistent with the results of previous studies where CHB was more likely to occur in patients with an initial, inferior/posterior, Q wave MI1–3,7. Patients who developed CHB in our study reported a different symptom profile than those without CHB, had significantly lower blood pressure findings, and significantly higher serum glucose levels than patients who did not develop CHB. It remains of importance to identify patients at increased risk for CHB so that these patients might be placed under more careful surveillance and use of effective treatment strategies optimized to improve the prognosis of these patients. The results of our study suggest that several of these high risk patient groups can be readily identified.
Incidence rates of CHB
The incidence rates of CHB in prior studies of patients with AMI range from 4–%1–5. A limited number of studies have, however, examined changing trends in the incidence rates of CHB, particularly during recent periods. Data from the studies in Israel, which examined the incidence rates of CHB in patients hospitalized with AMI in a prethrombolytic (1981–1983) as compared to a thrombolytic (1992–1996) era, indicated that the incidence rates of CHB declined slightly over time from 5.3% to 3.7%3. In our earlier study of greater Worcester residents hospitalized with AMI at all area medical centers, the proportion of patients who developed CHB declined by approximately one half between the mid-1970’s and mid-1990’s1,2.
The results of the present study demonstrate that the incidence rates of CHB in greater Worcester residents hospitalized with AMI have declined even more rapidly during the most recent decade under study. These encouraging declines are likely due to the increasing use of aggressive coronary reperfusion strategies and effective cardiac medications and/or due to changes in the natural history of AMI. For example, the proportion of patients who were treated with effective cardiac medications and coronary reperfusion approaches in the present study was considerably higher than had been previously reported from our study1,2. Declining trends in the incidence rates of CHB in the present study were observed in all patient groups examined, suggesting the consistency of these trends and likely improved management of all patients hospitalized with AMI. The results of our study also suggest that previously noted age and gender disparities in the development of CHB appear to have dissipated over time. This likely reflects increasing utilization of effective medical and revascularization therapies over the period under study, particularly in high risk patient subgroups including women and the elderly14.
Hospital case-fatality rates and clinical complications
The association between CHB and the occurrence of clinically significant hospital complications has been examined in several previous studies1,5–7,9. In general, patients with CHB were shown to be at greater risk for developing these important clinical complications than patients who did not develop CHB. Similar results were found in our study, even after controlling for the presence of other risk factors for these endpoints. These findings may be partially explained by the larger and more extensive infarctions associated with CHB and/or due to other hemodynamic or other disturbances associated with this conduction abnormality3,6,8. We were unable to determine, however, whether CHB occurred prior to, or as a consequence of, these clinical complications.
In prior studies, the hospital death rate due to CHB in the setting of AMI has been relatively high ranging from approximately 20% to 50%1–3,6,8. Data from Israel have shown that the short term death rate in patients with CHB declined from the pre-thrombolytic (1981–1983; 31%) to the thrombolytic era (1992–1996; 21%). However, these declining trends were attenuated after controlling for other factors of prognostic importance3. In our earlier publications from the Worcester Heart Attack Study, we observed improvements in the hospital survival of patients with CHB from the mid-1970’s (approximately 79% surviving) to mid-1990’s (approximately 87% surviving)1,2. In the present study, we observed more profound declines in the short-term death rates attributed to CHB from the mid-1990’s on.
Previous studies have shown that patients with CHB are between 2–5 times more likely to die during hospitalization for MI compared to patients who do not develop CHB1–3,6,7,15. Our overall results are consistent with these findings, suggesting that the odds of dying in hospital for patients who develop CHB is approximately 3 times higher than for those who did not develop CHB, even after controlling for other prognostic factors. On the other hand, the hospital CFRs associated with CHB complicating AMI have declined over time in the present study. Indeed, the hospital survival rates associated with AMI in the greater Worcester population have consistently improved over time13,14. In the mid to late 1970’s, approximately 79% of patients hospitalized with AMI survived their index hospitalization; this percentage increased to 91% during the 2000’s.
Our study showed that approximately two thirds of patients with CHB complicating an anterior MI died during hospitalization compared to only 37% of patients with an inferior/posterior MI and CHB. This is most likely explained by the differing mechanisms leading to CHB between patients who developed AMI at different anatomic locations. In patients with an anterior MI, CHB is generally propagated by extensive infarction involving the conduction system distal to the AV node. While heart block may contribute to increased mortality in this setting, much of the poorer outcomes observed in these patients is primarily related to the extent of acute left ventricular damage. Indeed pacing, although indicated, has never been clearly shown to be lifesaving in this setting. In patients with an inferior MI, CHB is generally caused by compromised supply to the AV node – in many patients, a stable escape rhythm is established and pacing is not always required. Similar to the situation in patients with an anterior MI, when this conduction disturbance occurs in the setting of a large infarct, excess mortality will be expected but CHB can also occur in much smaller inferior MIs.
Based on these findings, it remains of considerable importance to continue to monitor changing trends in the hospital prognosis of patients with CHB and identify patients at increased risk for dying after CHB. Our findings suggest that high risk patients with CHB can be identified in advance and increased monitoring and use of effective cardiac therapies be utilized in patients considered to be at increased risk for dying after developing CHB.
Study Strengths and Limitations
This study is a population-based investigation with the inclusion of all patients from a well-defined metropolitan area in New England hospitalized with confirmed AMI. We were unable, however, to examine the duration of CHB, the temporal relation between time of initiation of treatment and occurrence of CHB, and the role of extent of underlying coronary artery disease or other etiologies in relation to the development of CHB. We were also unable to systematically assess the possible concern that smaller AMI’s may have been diagnosed during recent study years and the resultant impact of this change in patient mix on the incidence and death rates associated with CHB.
Conclusions
The results of our study suggest that the incidence rates of CHB complicating AMI, and associated hospital mortality rates, have been declining over the past 30 years, especially during the most recent decade. Understanding changing trends in patient’s characteristics, incidence rates of CHB, and associated mortality remains of considerable importance as the management of patients with AMI continues to evolve as do the characteristics of patients hospitalized with AMI.
Acknowledgments
This research was made possible by the cooperation of the medical records, administration, and cardiology departments of participating hospitals in the Worcester metropolitan area and through funding support provided by the National Institutes of Health (R01 HL35434).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Spencer FA, Jabbour S, Lessard D, et al. Two dedicate long trends (1975–1997) in the incidence, hospitalization, and long term death rates associated with complete heart block complicating acute myocardial infarction: A community wide perspective. Am Heart J. 2003;145:500–507. doi: 10.1067/mhj.2003.4. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg RJ, Zevallos JC, Yarzebski J, et al. Prognosis of acute myocardial infarction complicated by complete heart block (the Worcester Heart Attack Study) Am J Cardiol. 1992;69:1135–1141. doi: 10.1016/0002-9149(92)90925-o. [DOI] [PubMed] [Google Scholar]
- 3.Harpaz D, Behar S, Gottlieb S, et al. Complete atrioventricular block complicating acute myocardial infarction in the thrombolytic era. SPRINT Study Group and the Israeli Thrombolytic Survey Group. Secondary Prevention Reinfarction Israeli Nifedipine Trial. J Am Coll Cardiol. 1999;34:1721–1728. doi: 10.1016/s0735-1097(99)00431-3. [DOI] [PubMed] [Google Scholar]
- 4.Kuo CT, Liu CY, Hsu TS, et al. Immediate prognostic significance of complete atrioventricular block in acute myocardial infarction. Taiwan Yi Xue Hui Za Zhi. 1989;88:712–717. [PubMed] [Google Scholar]
- 5.Aplin M, Engstrøm T, Vejlstrup NG, et al. on behalf of the TRACE Study Group. Prognostic importance of complete atrioventricular block complicating acute myocardial infarction. Am J Cardiol. 2003;92:853–856. doi: 10.1016/s0002-9149(03)00900-7. [DOI] [PubMed] [Google Scholar]
- 6.Melgarejo Moreno A, Galcerá Tomás J, García Alberola A, et al. Prognostic significance of advanced atrioventricular block in patients with acute myocardial infarction. Med Clin (Barc) 2000;114:321–325. doi: 10.1016/s0025-7753(00)71282-6. [DOI] [PubMed] [Google Scholar]
- 7.Behar S, Zissman E, Zion M, et al. Complete atrioventricular block complicating inferior acute wall myocardial infarction: short- and long-term prognosis. Am Heart J. 1993;125:1622–1627. doi: 10.1016/0002-8703(93)90750-4. [DOI] [PubMed] [Google Scholar]
- 8.Clemmensen P, Bates ER, Califf RM, et al. TAMI Study Group. Complete atrioventricular block complicating inferior wall acute myocardial infarction treated with reperfusion therapy. Am J Cardiol. 1991;67:225–230. doi: 10.1016/0002-9149(91)90550-5. [DOI] [PubMed] [Google Scholar]
- 9.Berger PB, Ruocco NA, Jr, Ryan TJ, et al. Incidence and prognostic implications of heart block complicating inferior myocardial infarction treated with thrombolytic therapy: results from TIMI II. J Am Coll Cardiol. 1992;20:533–540. doi: 10.1016/0735-1097(92)90004-7. [DOI] [PubMed] [Google Scholar]
- 10.Dubois C, Piérard LA, Smeets JP, et al. Long-term prognostic significance of atrioventricular block in inferior acute myocardial infarction. Eur Heart J. 1989;10:816–820. doi: 10.1093/oxfordjournals.eurheartj.a059575. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg RJ, Gore JM, Alpert JS, et al. Recent changes in the attack rates and survival rates of acute myocardial infarction (1975–1981); The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 12.Goldberg RJ, Gore JM, Albert JS, et al. Incidence and case fatality rates of acute myocardial infarction (1975–1984): The Worcester Heart Attack Study. Am Heart J. 1988;1155:761–767. doi: 10.1016/0002-8703(88)90876-9. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg RJ, Yarzebski J, Lessard D, et al. A two-decades (1975–1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: A community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg RJ, Spencer FA, Yarzebski J, et al. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study) Am J Cardiol. 2004;94:1373–1378. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 15.Abidov A, Kaluski E, Hod H, et al. for the Israel Working Group on Intensive Cardiac Care. Influence of conduction disturbances on clinical outcome in patients with acute myocardial infarction receiving thrombolysis (results from the ARGAMI-2 study) Am J Cardiol. 2004;93:76–80. doi: 10.1016/j.amjcard.2003.09.016. [DOI] [PubMed] [Google Scholar]