Abstract
Previous observational research confirms abundant variation in primary care practice. While variation is sometimes viewed as problematic, its presence may also be highly informative in uncovering ways to enhance health care delivery when it represents unique adaptations to the values and needs of people within the practice and interactions with the local community and health care system. We describe a theoretical perspective for use in developing interventions to improve care that acknowledges the uniqueness of primary care practices and encourages flexibility in the form of intervention implementation, while maintaining fidelity to its essential functions.
Keywords: health care delivery, nonlinear dynamics, quality of health care
The Veterans Health Administration (VHA), the largest integrated health care system in the United States, provides care to more than 6 million veterans. Each veteran is assigned a primary care provider who is responsible for coordinating access to services, meeting specific health care needs, and providing services that promote wellness and reduce risk for preventable illness.1 An analysis of care within VHA, however, demonstrates significant and sometimes undesirable variation at the facility level in many of the processes and intermediate outcomes of both chronic disease management and prevention.2
Past initiatives to enhance care in VHA and elsewhere have been based, to a significant extent, on the continuous quality improvement (CQI) model. This approach has important conceptual and analytical limitations, however. First, the conceptual framework for quality improvement, rooted in an industrial (manufacturing) model, uses a mechanical view of the systems that humans create and focuses on incremental change to reduce variation. Its application in health care has also tended to be mechanistic, with undesirable variation in health service delivery (e.g., units achieving outcomes below the group mean) often regarded as an alteration in normal functioning.3–6 However, standardizing care without identifying desirable variation or unique adaptations that take advantage of local opportunities and strengths (sometimes referred to as “positive variation” or “positive deviance”7,8) misses an important opportunity to identify and investigate unanticipated circumstances or locally adapted practice configurations associated with better health care outcomes.9 The importance of the context within which a practice is situated is evident when efforts to apply an intervention developed in 1 setting yield unexpected results in another. For this reason, others have emphasized the need to understand the interplay between context, structure, and process as a necessary antecedent to designing and implementing interventions that seek to improve outcomes.10,11
The Plan-Do-Study-Act (PDSA) cycle of CQI is a sequential, iterative learning model representative of the scientific method with some of the characteristics of the mechanistic conceptual model described above. In operationalizing this technique in health care settings, the approach within a single PDSA cycle, however, often assumes the presence of a “simple” cause-effect relationship between “Plan A” and “Effect B,” by testing 1 hypothesis at a time. Subsequent changes are typically formulated using a cause and effect diagram with the base assumption that a process can be understood by its causal relationships, which in turn can be traced back or reduced to individual elements.12 A relatively simplistic interpretation of the analytic approach assumes that the influence of other factors can be reliably held constant through mathematical modeling techniques such as linear regression.13 Insights from the social and behavior sciences, however, suggest that the process of implementing change or the diffusion of innovation involve social interactions that are rarely linear and are often unpredictable.10,13–15 Developing CQI interventions that are consistently effective across settings may therefore be difficult unless the moderating and complex effects of “real-world” factors are considered in study design and analytical models.
Although previous quality improvement initiatives have contributed valuable insights and useful approaches to improve health care, rethinking its basic assumptions may prove useful in charting a direction for future efforts. In the sections that follow, we outline a framework using “complexity theory”16–18 that characterizes primary care practices as complex adaptive systems, provides examples of the components of these systems, illustrates the potential utility of complexity theory in developing interventions to improve care, and suggests a different perspective in understanding their implementation.
WHAT IS COMPLEXITY THEORY?
Complexity theory is not a theory per se, but rather a loose set of concepts, heuristics, and analytic tools.16,17 We will describe 2 closely related and complementary aspects of this theory with applications to health care delivery: mathematical complexity, based in chaos theory and its related mathematics; and aggregate complexity, which deals with the interplay of individual elements resulting in systems with complex behavior.16 Some have viewed the former as the quantitative component of complexity and the latter as a more qualitative feature.18 Both have the potential to provide insights that are useful in guiding the design and implementation of interventions to enhance the delivery of care.
MATHEMATICAL COMPLEXITY
Health care delivery consists of numerous simple and complex “systems” or processes, ranging from those that are deterministic to those with features of randomness. A deterministic system is one that has predictable outcomes. Given the same starting conditions and the same equation, the same results are expected (e.g., the inoculation of a virus into tissue culture medium regularly results in cell disruption and viral replication). Complex nonlinear systems, in contrast, are difficult to fully characterize because of the potential for multiple interactions and recursive feedback loops between components or agents within and outside the system. Furthermore, many of these systems exhibit actions that follow nonlinear, unpredictable trajectories, but possess underlying patterns that are detectable and based in probabilities related to constraints placed on each system. For example, it may not be possible to predict with certainty the exact temperature at noon in mid-summer of a given year in a specific Midwestern U.S. city, but one might anticipate warm weather rather than cold. Similarly, patient care consists of numerous processes in which multiple factors or agents exert influence on their availability, application, and sequence in highly variable ways, which results in outcomes that are less than fully predictable.
Chaos occurs when a nonrandom or deterministic system behaves in an apparently random manner.16 A classic example is the relationship between populations of predators and prey, which can be described with a simple (logistic) equation. Under certain conditions, the size of these populations is cyclical and synchronized. Under others, their relationship to each other appears completely random. In chaotic systems, processes often yield nonlinear results and demonstrate a dynamic quality16 that reflects adaptation to changes in the interactions and initial conditions that first existed when these systems were established. Although not predictable with certainty, the behavior of these systems can be described within limits because they often appear to nearly (but never quite) repeat themselves. These patterns and the paths that the system takes have been described as “attractors” and “trajectories,” respectively.18
Each group of individuals working as a clinical team, whether in a solo practice setting or in a VA community-based outpatient clinic, has its own pattern of behaviors that emerge over time and co-evolve within its own practice environment. Additionally, each has its own set of rules that are implicit or explicit, guides its actions, and potentially competes with other mandates facing the practice. For example, members of many practices might view their mission as providing care to underserved, vulnerable subgroups in the population, but most realize they cannot survive as a service organization without successfully minimizing costs or obtaining local government financial support (another model). Each model strives to achieve several end points (attractors) that reflect the motivators and values of the practice. However, because of ongoing conflict between the values associated with each model, practice behavior at any given time may not be predictable as it pays more attention to achieving 1 goal over another and then switches back. This behavior may never exactly repeat, but patterns are usually discernable.12
A second important characteristic of chaotic systems is the presence of self-similarity across different scales of measurement. This is most apparent in the concept of fractals, an object whose parts resemble smaller copies of the whole, identified through closer examination.19,20 Biological examples of fractals exist throughout nature and include branching structures such as blood vessels in the vascular tree or respiratory passages in the lungs.21 The repetition of similar units at increasing levels of resolution is often referred to as “self-similarity” and was first described by the mathematician Mandelbrot,19 who used principles such as the inverse power law to identify and quantify this characteristic.
Many aspects of health care demonstrate self-similar features. For example, VHA is a system organized in a self-similar hierarchy consisting of community-based outpatient clinics affiliated with specific medical centers, linked to regional networks, within a nation-wide system. Similarly, delivery of specific services such as smoking cessation counseling demonstrates this characteristic through peaks and valleys in provider counseling efforts that occur hour by hour during the workday even among experienced personnel and persist when reviewed using different time scales (e.g., weeks, months, or years). Behavioral counseling, like the delivery of other health care services, is difficult to predict with precision even when other determinants are known because these processes are controlled by nonlinear rather than linear dynamics, in which multiple individuals (e.g., physicians, nurses, front desk staff, and patients) interact within an office, clinic, or health care system (i.e., context) that is continually evolving.
Quality improvement efforts often seek to enhance patient satisfaction through timely assessment and treatment. To assess the presence of mathematical complexity in data from a recent CQI project at our facility, we analyzed service times for 2,371 consecutive patients seen in an outpatient urgent care center during September 2004. Service time was defined as the duration in minutes from signing in to the time of disposition for each patient either to home or hospital bed.
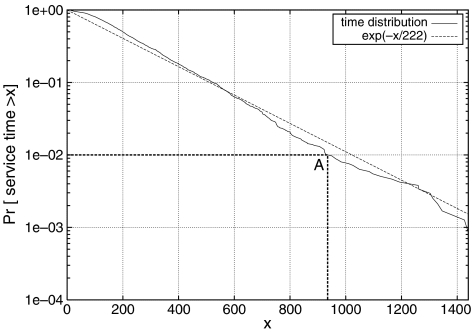
To start, one might characterize these data using a sample mean and standard deviation. Graphing these data, however, reveals significant skewness and an exponential distribution (Fig. 1) commonly seen in complex processes in which events are not fully independent: the duration of an evaluation for 1 patient depends upon or is influenced by time spent caring for previous patients. To understand this finding better and to ascertain whether these data reflected mathematical complexity, a closer assessment demonstrated that a pattern of bursts in service times observed during a single day closely resembled patterns of bursts occurring over a series of days (data not shown). We then used a time series analysis and tools available in a package of statistical programs22 to distinguish chaotic behavior from random variation by calculating the Hurst parameter H, a measure ranging from 0.5 to 1.0 when self-similarity is present. Using several analytic techniques to generate this parameter, we observed that values for 6 of 7 estimates exceeded 0.6 and 3 estimates exceeded 0.7, supporting the conclusion that our data exhibited self-similarity characteristic of mathematical complexity. Had our analysis included the actual times of day at which patients signed in, we might have been able to quantify associations between these patterns and potential explanatory factors, such as variable staffing patterns and slowdowns in other work areas providing services to patients seen in this clinic.
FIGURE 1.
Complementary cumulative distribution of patient service times: the vertical axis gives the frequency with which the patient service time was greater than the value on the horizontal axis. For example, point A denotes that in 1% of the measured instances, the patient service time was more than 935 minutes. The service times were fit to an exponential distribution (denoted in the figure as exp(−x/222)) with a high degree of goodness of fit (R2=.98).
AGGREGATE COMPLEXITY
Mathematical complexity is present in many processes common to primary care, yet the systems of care patients encounter and those in which providers work consist of numerous such processes. Aggregate complexity is a term used to refer to the study of systems16 consisting of multiple concurrent and dynamic interactions or processes influenced by mathematical complexity.
Primary care practices have been described as “complex adaptive systems” because they have features adhering to the principles of complexity theory.9,13,14,18 These systems consist of collections “of individual agents that have the freedom to act in ways that are not always predictable and whose actions are interconnected such that 1 agent's actions change the context for other agents.”23 Other attributes typically include embeddedness, distributed control, connectivity, emergent behavior, nonlinearity, dependence on initial conditions, and coevolution. Systems are embedded or nested in larger systems; many systems encompass still smaller systems. There is no single centralized control mechanism that governs every aspect of system behavior, even in a seemingly hierarchical structure of a single system. Instead, control is said to be distributed among the agents making up the system, all of whom are connected through working relationships or other interactions. The interrelationships among adaptive elements of the system produce patterns of behavior, but not in a totally predictable fashion. Novel behaviors can emerge that could not be anticipated by knowing the agents individually. Consequently, the whole system is qualitatively different than the sum of its component parts.24 In addition, these patterns have implications for change in systems: because multiple connections within and between systems exist, the behavior of a specific practice is influenced by both internal and external factors. Within these systems there is also tension between the status quo and the need to adapt to changing conditions. Theoretical work suggests that systems “at the edge of chaos,” i.e., between equilibrium and complete disorder, may in fact be the most adaptive and creative.25 Empirical evidence of this can be found in organizations composed of practices able to absorb the influences of internal and external factors without changing (appearing to be resistant to change) and others near the edge of chaos open to and ready for change.26 Complexity theory suggests that this intricate web of interactions exhibits nonlinearity (e.g., small actions may have large effects on overall system behavior, while large actions have the potential to result in little overall effect) and that they are sensitive to the initial conditions existing at each practice.
Several factors contribute to the uniqueness of each complex adaptive system. The initial conditions for each, for example, may result from efforts by practice personnel to meet a particular need in a specific location, influenced by the context (e.g., the larger health care system to which each belongs, the social and economic conditions within the local community, and national conditions) at a particular point in time. Second, the mix of “agents” within and between practices (e.g., physicians, staff, and patients), their attitudes, skills, individual self-efficacy, and the nature of the interactions between agents may differ.27 A different mix of the same number of individuals with the same job descriptions in an identical structure might exhibit very different behavior. Third, the context within which each clinic is embedded may further influence its function by providing resources, constraints, motivation, and disincentives that vary significantly across settings.27 Because of a web of interrelationships, individual elements may change over time28 and the system's patterns of behavior may also “co-evolve.” Dynamic coevolution of each factor described above may contribute further to the complexity of these interactions through multiple feedback loops, associations that are nonlinear, and results that are as difficult to predict as for those involving single processes.
USING COMPLEXITY THEORY TO DEVELOP NEW INTERVENTIONS FOR QUALITY IMPROVEMENT
As suggested previously, the ecology of primary care practice is complicated.24,29 Previous work demonstrates the challenges associated with changing clinician behavior to improve care,30–32 with most practice-level interventions showing only limited or modest success.33–37 Because opportunities for change vary at each practice, complexity theory predicts that interventions successfully addressing problems or barriers in 1 setting may have limited utility elsewhere. To bring value, therefore, the design of these interventions must take existing conditions, practice configuration, and dynamics into consideration.
Previous work to enhance delivery of preventive services in community-based primary care practices provides an example of a successful intervention, based on complexity theory, that used knowledge about each study site to shape the intervention.38 This study, given the acronym “STEP-UP” (Study To Enhance Prevention by Understanding Practice) started with an assessment of each practice, and gave attention to the operations, structure, and interrelationships between personnel as a means of identifying characteristics that should be considered in tailoring the intervention to the site. Following the completion of a process that used both quantitative and qualitative data collection techniques, research staff helped practices identify both successes and missed opportunities created by their current approach. Presenting a menu of tools and approaches to help enhance preventive service delivery based on strategies tested in other trials, and a process of facilitation by the research team assisted practices in identifying a focus and plan for change efforts that made sense in their context. While this process bears similarity to traditional CQI, the STEP-UP intervention also incorporated important elements of complexity theory, such as sensitivity to initial conditions, and an awareness of the importance of interactions between participants and the context in which they worked in shaping the intervention at each site.
IMPLEMENTING INTERVENTIONS IN COMPLEX ADAPTIVE SYSTEMS
Recognizing that practices are unique requires a different perspective on the definition of successful intervention implementation. Given the individuality of group practices and the unique adaptation of each to their local context, measuring the number of surveys completed or sessions attended may miss whether the key functional aspects of an intervention are actually occurring (e.g., the transfer of information, development of specific skills, increased awareness of new techniques).39 Assessing fidelity in the implementation of such interventions, therefore, requires an emphasis on identifying these functions and on developing ways to determine that each has taken place.
The nature of complex systems suggests that evaluation of the implementation process would benefit from use of both qualitative and quantitative methods. Identifying emergent and unanticipated practice behaviors in STEP-UP, for example, might have been difficult had predetermined quantitative measures been used in isolation. Mixed methods approaches, however, offer complementary insights into understanding the discontinuous processes that arise in some practices and result in positive deviance or desirable variation, or that explain the basis for long-term improvements that were observed at some study sites. A notable feature of STEP-UP, for example, was the sustainability of the intervention effect over 24 months of follow-up.40 Qualitative analysis of field notes and interviews suggested that a sustained effect, observed at nearly all intervention sites, was possibly related to the individualization of the intervention to the unique values, structures, and processes of each practice, and the incorporation of these new processes, identified and implemented by stakeholders in the practice, into the culture of the organization.41
CONCLUSION
A working knowledge of the principles of complexity theory and their application to primary care practice, especially within large health care systems such as VHA, offers a way to make sense of occurrences in everyday practice that may otherwise seem paradoxic. In its focus on multiple interactions and context rather than on single cause-effect mechanisms, this perspective supports development of tailored interventions to improve nonlinear processes of care. Identifying essential functional tasks or processes and monitoring their implementation offers a means of assessing intervention fidelity, recreating programs successfully in other settings, and in understanding conditions under which positive deviance or desirable variation arises.
Acknowledgments
Source of Funding: This project was partly funded from Veterans Administration Health Service (HSR&D) grants to Dr. Litaker (Career Development Award) and Dr. Aron (REA 01-100).
REFERENCES
- 1.Perlin J, Kolodner R, Roswell R. The Veterans Health Administration: quality, value, accountability, and information as transforming strategies for patient-centered care. Am J Manag Care. 2004;10:828–36. [PubMed] [Google Scholar]
- 2.Krein S, Hofer T, Kerr E, Hayward R. Whom should we profile? Examining diabetes care practice variation among primary care providers, provider groups, and health care facilities. Health Serv Res. 2002;37:1125–7. doi: 10.1111/1475-6773.01102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Solberg L, Brekke M, Kottke T, Steel R. Continuous quality improvement in primary care: what's happening? Med Care. 1998;36:625–35. doi: 10.1097/00005650-199805000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Solberg LI, Kottke TE, Brekke ML, et al. Failure of a continuous quality improvement intervention to increase the delivery of preventive services. A randomized trial. Eff Clin Pract. 2000;3:105–15. [PubMed] [Google Scholar]
- 5.Kritchevsk SB, Simmins BP. Continuous quality improvement. Concepts and applications for physician care. JAMA. 1992;267:55–6. doi: 10.1001/jama.266.13.1817. [DOI] [PubMed] [Google Scholar]
- 6.Palmer RH, Louis TA, Hsu LN, et al. A randomized controlled trial of quality assurance in sixteen ambulatory care practices. Med Care. 1985;23:751–70. doi: 10.1097/00005650-198506000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Macklis R. Successful patient safety initiatives: driven from within. Group Pract J. 2001;50:1–5. [Google Scholar]
- 8.Marsh D, Schroeder D, Dearden K, Sternin J, Sternin M. The power of positive deviance. Br Med J. 2004;329:1177–9. doi: 10.1136/bmj.329.7475.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller W, McDaniel R, Crabtree B, Stange K. Practice jazz: understanding variation in family practices using complexity science. J Fam Pract. 2001;50:872–80. [PubMed] [Google Scholar]
- 10.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patrick DL, Chiang YP. Measurement of health outcomes in treatment effectiveness evaluations: conceptual and methodological challenges. Med Care. 2000;38(suppl):14–25. doi: 10.1097/00005650-200009002-00005. [DOI] [PubMed] [Google Scholar]
- 12.Dooley K, Johnson TL, Bush D. TQM, chaos, and complexity. Human Syst Manag. 1995;14:287–302. [Google Scholar]
- 13.Miller W, Crabtree B, McDaniel R, Stange K. Understanding change in primary care practice using complexity theory. J Fam Pract. 1998;46:369–76. [PubMed] [Google Scholar]
- 14.Plsek P. Accelerating Quality Improvement in Health Care-Strategies to Speed the Diffusion of Evidence-Based Innovations. Washington, DC, USA: [September 19, 2005]. Complexity and the adoption of innovation in health care. Available at http://www.nihcm.org/plsek.pdf 2003. [Google Scholar]
- 15.Rogers E. A prospective and retrospective look at the diffusion model. J Health Commun. 2004;9:13–9. doi: 10.1080/10810730490271449. [DOI] [PubMed] [Google Scholar]
- 16.Manson S. Simplifying complexity: a review of complexity theory. Geoform. 2001;32:405–14. [Google Scholar]
- 17.Phelan S. What is complexity science really? Emergence. 2003;3:120–36. [Google Scholar]
- 18.Kernick D. Complexity and Healthcare Organization: A View from the Street. Oxford, UK: Radcliffe Publishing; 2004. [Google Scholar]
- 19.Mandelbrot B. The Fractal Geometry of Nature. San Francisco: W.H. Freeman and Co.; 1982. [Google Scholar]
- 20.Liebovitch L. Fractals and Chaos Simplified for the Life Sciences. New York: Oxford University Press; 1998. [Google Scholar]
- 21.Aron DC. Chaos, complexity and cardiology. In: Holt T, editor. Complexity for Clinicians. Oxford, UK: Radcliffe Press; 2004. [Google Scholar]
- 22.Karagiannis T, Faloutsos M. SELFIS: a tool for self-similarity and long-range dependence analysis. 2002. First workshop on fractals and self-similarity in data mining: issues and approaches;
- 23.Plsek P. Crossing the quality chasm: a new health system for the 21st century. The National Academy of Sciences; 2000. Redesigning health care with insights from the science of complex adaptive systems; pp. 309–17. [Google Scholar]
- 24.Stange KC. The paradox of the parts and the whole in understanding and improving general practice. Int J Qual Health Care. 2002;14:267–8. doi: 10.1093/intqhc/14.4.267. [DOI] [PubMed] [Google Scholar]
- 25.Kauffman S. The Origins of Order. Oxford, UK: Oxford University Press; 1993. [Google Scholar]
- 26.Stacey R. Mapping the Science of Complexity onto Organizations. Complexity and Creativity in Organizations. San Francisco, CA: Berrett-Koehler; 1996. pp. 107–17. [Google Scholar]
- 27.Tallia A, Stange K, McDaniel R, Aita V, Miller W. Understanding organizational designs of primary care practices. J Healthc Manag. 2003;48:45–9. [PubMed] [Google Scholar]
- 28.Stroebel CK, McDaniel R, Crabtree B, Miller W, Nutting P, Stange KC. How complexity science can inform a reflective process for improvement in primary care practices. Jt Comm J Qual Patient Saf. 2005;31:438–46. doi: 10.1016/s1553-7250(05)31057-9. [DOI] [PubMed] [Google Scholar]
- 29.Stange K, Jaen C, Flocke S, Miller W, Crabtree B, Zyzanski S. The value of a family physician. J Fam Pract. 1998;46:363–8. [PubMed] [Google Scholar]
- 30.Berwick DM. Disseminating innovations in health care. JAMA. 2003;289:1969–75. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- 31.Greco PJ, Eisenberg JM. Changing physicians' practices. N Engl J Med. 1993;329:1271–4. doi: 10.1056/NEJM199310213291714. [DOI] [PubMed] [Google Scholar]
- 32.Eisenberg JM. Physician utilization: the state of research about physicians' practice patterns. Med Care. 1985;23:461–83. [PubMed] [Google Scholar]
- 33.Davis D, O'Brien M, Freemantle N, et al. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282:867–74. doi: 10.1001/jama.282.9.867. [DOI] [PubMed] [Google Scholar]
- 34.Davis D, Thomson MA, Oxman A, Haynes R. Evidence for the effectiveness of CME. A review of 50 randomized controlled trials. JAMA. 1992;268:1111–7. [PubMed] [Google Scholar]
- 35.Davis DA, Thomson MA, Oxman AD, Haynes B. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–5. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 36.Haynes RB, McKibbon KA, Kanani R. Systematic review of randomised trials of interventions to assist patients to follow prescriptions for medications. Lancet. 1996;348:383–6. doi: 10.1016/s0140-6736(96)01073-2. [DOI] [PubMed] [Google Scholar]
- 37.Shortell S, Bennett C, Byck G. Assessing the impact of continuous quality improvement on clinical practice: what it will take to accelerate progress. Milbank Q. 1998;76:593–624. doi: 10.1111/1468-0009.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goodwin MA, Zyzanski SJ, Zronek S, et al. A clinical trial of tailored office systems for preventive service delivery: the study to enhance prevention by understanding practice (STEP-UP) Am J Prev Med. 2001;21:20–8. doi: 10.1016/s0749-3797(01)00310-5. [DOI] [PubMed] [Google Scholar]
- 39.Hawe P, Shiell A, Riley T. Complex interventions: how “out of control” can a randomized controlled trial be? Br Med J. 2004;328:1561–3. doi: 10.1136/bmj.328.7455.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stange KC, Goodwin MA, Zyzanski SJ, Dietrich AJ. Sustainability of a practice-individualized preventive service delivery intervention. Am J Prev Med. 2003;25:296–300. doi: 10.1016/s0749-3797(03)00219-8. [DOI] [PubMed] [Google Scholar]
- 41.Ruhe MC, Gotler RS, Goodwin MS, Stange KC. Physician and staff turnover in community primary care practice. J Ambulatory Care Manag. 2004;27:242–8. doi: 10.1097/00004479-200407000-00008. [DOI] [PubMed] [Google Scholar]