Abstract
Objective
To evaluate the association of Attention-Deficit/Hyperactivity Disorder (ADHD) and severity of physical dependence on nicotine in a controlled study of adolescents and young adults with ADHD.
Study design
In controlled longitudinal family studies of ADHD, we examined self-reports on the modified Fagerstom Tolerance Questionnaire (mFTQ) for degrees of physical dependence on nicotine.
Results
We obtained mFTQ data from 80 ADHD probands and 86 control probands (mean age= 19.2). Smokers with ADHD had significantly higher scores on the mFTQ, indicative of more severe physical dependence on nicotine compared with control smokers. Similarly, among current smokers, there was a positive linear relationship between mFTQ score and symptoms of both inattentive and hyperactive ADHD symptoms. Environmental factors such as current parental smoking, peer smoking, and living with smokers all increased the risk for smoking in youth with ADHD more than in controls.
Conclusion
Male and female smokers with ADHD manifest more severe physical dependence on smoking compared with controls. Important environmental factors appear to add to the smoking risk in ADHD.
Keywords: ADHD, smoking, nicotine, Fagerstrom Tolerance Questionnaire (FTQ)
Cigarette smoking among adolescents and young adults has long been recognized as a serious public health problem1. Recent nationwide surveys of high school students revealed that 22% of 12th-graders were smoking 2. In addition to the direct health effects, cigarette smoking often represents an early stage in the developmental sequence into illicit drug use3, 4. We recently found smoking to be a significant risk factor for the subsequent use and abuse of drugs - particularly in youth with Attention-Deficit Hyperactivity Disorder (ADHD)5.
Over the past decade, studies have demonstrated important bidirectional relationships between ADHD and cigarette smoking6-11. As children with ADHD reach adolescence, they are significantly more likely to smoke and at an earlier age than controls (before age 15: ADHD=25%, non-ADHD=9%)6. Prior studies have generally not examined potential differences in the risk and characteristics of cigarette smoking between boys and girls with ADHD. Yet data suggest that girls with ADHD may have a substantially higher age-matched risk for associated problems such as substance use than boys, despite having lower rates of conduct disorder12, 13.
The aim of the present study was to evaluate the risk and severity of cigarette smoking in adolescents and young adults with ADHD who were part of an ongoing controlled, longitudinal study of ADHD. Based on the literature7, 8, we hypothesized that a greater frequency of cigarette smoking would be identified in subjects with ADHD; and based on findings of a greater severity of substance use problems associated with ADHD14, 15 – that among smokers, a more severe form of nicotine dependence, measured by higher scores on a smoking questionnaire, would be associated with ADHD.
Methods
Subjects
Subjects were derived from two longitudinal case-control family studies of ADHD 16, 17. A three-stage ascertainment procedure was used to select subjects: referral, telephone screening, and structured interview18. Because this study had begun prior to the finalization of DSM-IV, our baseline assessment used DSM-III-R-based structured interviews but we supplemented these with questions that would allow us to make DSM-IV diagnoses. The present study reports on the 5-year follow-up of the female subjects (mean age at baseline=11.7 yrs) and the 10-year follow-up of the male subjects (mean age at baseline=11.0 yrs), which occurred simultaneously during the same five-year time period (Boys study: N=217, Girls study: N=235). Parents and adult offspring provided written informed consent to participate, and parents also provided consent for children under the age of 18. Children and adolescents provided written assent to participate. The human research committee at Massachusetts General Hospital approved this study protocol.
Psychiatric assessments including ADHD for the follow-up data presented here relied on the Schedule for Affective Disorders and Schizophrenia for School Aged Children - Epidemiologic Version (K-SADS-E) for subjects under 18 and the Structured Clinical Interview for DSM-IV (SCID) (supplemented with modules from the K-SADS-E to assess retrospectively childhood onset of symptoms and diagnoses including ADHD) for subjects 18 years of age and older16. In both children and adults, we considered a positive diagnosis if DSM-IV diagnostic criteria were unequivocally met. Clinically significant ADHD symptoms were based on the DSM-IV (9 Inattentive and 9 Hyperactive/Impulsive total) and derived from age-appropriate structured interviews (see above). The raters were blind to the clinical status of the subject, the ascertainment site and all prior assessments.
Socioeconomic status (SES) was measured using the 5-point Hollingshead scale, in which higher scores indicate lower SES. Family intactness was recorded as a binary variable showing if a subject’s parents had ever been divorced or separated.
Fagerstrom Tolerance Questionnaire
The Fagerström Tolerance Questionnaire (FTQ) is a reliable and valid, self-reporting instrument for assessing cigarette use, severity of physical dependence on nicotine19. Screening questions divide subjects by having smoked cigarettes at least once in one’s lifetime (ever smoked), and by having smoked in the past month (current smokers). Current smokers then complete 8 items evaluating smoking habits. The questionnaire was scored according to the modified FTQ (mFTQ), which consists of seven items from the original 8-item FTQ (mFTQ does not include the question “What brand of cigarettes do you smoke?”). A higher mFTQ score indicates a greater degree of physical dependence for smoking19 (range: 0-9). A subject was defined as being mFTQ dependent when the score was 4 or greater, indicating the midpoint of moderate dependence20. We also added additional items including exposure to smoking questions asking if parents, people they live with, or friends smoke and past smoking items such as age at onset of smoking. Subjects were mailed the FTQ to be completed at home and returned on or before the day of their assessments.
Statistical Analysis
Because our subjects spanned two sex-specific studies with different mean ages, we restricted our sample to subjects within overlapping age ranges, in order to minimize collinearity of age and sex. We truncated the sample age distribution by eliminating 65 female subjects aged 10-14 and 46 male subjects aged 26-31, thus eliminating the difference in mean age between males and females. Subjects who did not complete and return the mFTQ in form packets (N=175) were dropped from analyses. The dropped subjects were significantly different based on sex as more females successfully completed and returned mFTQs (χ2(1)=6.1, p=0.01). There were no differences in age, SES, ADHD status or family intactness between included and dropped subjects.
We used Pearson χ2 tests for categorical variables and two-sided Fisher exact tests in cases of low-frequency responses. Student’s t-tests were used to compare mFTQ scores and ages of onset between groups. We used linear regression models to evaluate the relationship between ADHD symptoms and mFTQ scores as well as to include all relevant covariates in analyses. We modeled mFTQ score with linear regression including an interaction term for exposure to smoking and ADHD status. We fitted logistic regression models for associations between ADHD symptoms and rates of cigarette use. We used an alpha-level of 0.05 to assert statistical significance and indicated any trends at p<0.10; all statistical tests are two-tailed. We calculated all statistics using STATA 9.0 (Stata Corporation, 2005).
Results
We assessed 341 subjects and obtained mFTQ data from 80 ADHD probands and 86 control probands between the ages of 15 and 25. There were no significant differences between ADHD and control subjects in age (19.3±2.7 and 19.2±2.8 years, respectively, p=0.73), socioeconomic status (2.0±1.2 and 1.7±0.8, p=0.27) or sex ratio (43% (34) males and 38% (33) males, respectively; p=0.59). The ADHD cohort consisted of 70 (out of 80) subjects who reported receiving pharmacologic medication as treatment for ADHD in their lifetime (duration: 8.6±4.1 years). Within the ADHD group there were no differences between current smokers and non-smokers with respect to severity of ADHD (χ2(2)=1.8, p= 0.40).
Smoking Prevalence
Based on responses to the mFTQ, there were significant differences in rates of having ever smoked and current smoking between ADHD and control subjects (Table I). Lifetime prevalence of smoking was more common in subjects with ADHD compared with controls (Table I). Similarly, current smoking (past month) was more common in subjects with ADHD compared with controls (Table I).
Table I.
mFTQ Smoking Characteristics
| CONTROL N=86 N(%) | ADHD N=80 N(%) | χ2 | df | p | |
|---|---|---|---|---|---|
| Lifetime Smoking1 | 38(44) | 55(69) | 10.2 | 1 | 0.001 |
| Current Smoking1 | 15(17) | 33(41) | 11.4 | 1 | 0.001 |
| mFTQ Dependence (score ≥4)1 | 1(1) | 17(21) | 17.3 | 1 | <0.001 |
| CONTROL SMOKERS N=15 Mean±SD | SMOKERS with ADHD N=33 Mean±SD | t | df | p | |
| mFTQ score2 | 2.1±1.3 | 4.0±1.8 | 3.5 | 46 | 0.001 |
Pearson χ2 tests
Wilcoxon rank-sum test
mFTQ Score
Subjects with ADHD had greater rates of smoking dependence according to the mFTQ (Table I). When restricting analyses to current smokers, subjects with ADHD had significantly higher mFTQ scores indicative of more severe nicotine addiction compared with controls (Table I). These differences in rates of smoking dependence and mFTQ scores were maintained after controlling for conduct disorder (p=0.008 and p=0.01, respectively). On the questionnaire’s individual scored items, subjects with ADHD had significantly higher scores on two of the seven items compared with control smokers: greater number of cigarettes smoked daily (ordered logistic regression: z=2.9, p=0.003) and more often smoking while sick (Fisher exact test, p=0.04). There was also a trend for the ADHD group to smoke sooner after waking than the control group (t=1.8, p=0.09).
ADHD Symptoms and Subtypes
Current smoking rates were directly related to the overall number of current overall, inattentive, and hyperactive/impulsive ADHD symptoms across all subjects (Figure 1; Table II). Similarly, among current smokers, there was a positive linear relationship between mFTQ score and total ADHD symptoms (Table II) – which was significant for both ADHD subtypes. Within subjects with ADHD, the only symptom found to be significantly more prevalent in current smokers compared with non-smokers was “difficulty playing/being quiet” (smokers: 69%; non-smokers: 40%; χ2(1)=6.1, p=0.01). Control subjects displayed fewer inattentive and hyperactive/impulsive symptoms than subjects with ADHD (ADHD: Inattentive=7.5±2.1, Hyperactive=6.1±2.6; Control: Inattentive=1.4±2.2, Hyperactive=1.3±1.9).
Figure 1.
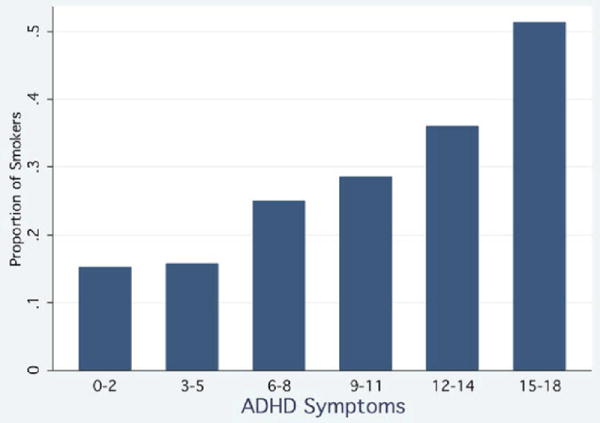
Association between total ADHD symptoms and smoking rates; Wald test for logistic regression model: N=166, χ2(1)=14.0, p<0.001.
Table II.
Association between ADHD Symptoms and Smoking Rates/Severity
| Outcome Variable | Independent Variable | Test-statistic | df | p |
|---|---|---|---|---|
| Current Smoking1 | Total Sxs | χ2 = 14.0 | 1 | <0.001 |
| Current Smoking1 | Inattentive Sxs | χ2 = 12.1 | 1 | <0.001 |
| Current Smoking1 | Hyperactive Sxs | χ2 = 13.7 | 1 | <0.001 |
| mFTQ score2 | Total Sxs | F = 8.1 | 1, 46 | 0.007 |
| mFTQ score2 | Inattentive Sxs | F = 7.5 | 1, 46 | 0.009 |
| mFTQ score2 | Hyperactive Sxs | F = 7.5 | 1, 46 | 0.009 |
Logistic regression model
Linear regression model
Sex Differences in Smoking
Albeit we had a larger percentage of females relative to males in our sample, there was a trend to more severe nicotine dependence in female compared with male smokers with ADHD (mFTQ scores: 4.5±1.8 and 3.4±1.8, respectively, z=1.7, p=0.09). Across all subjects with ADHD, there were no differences in rates of mFTQ smoking dependence, current smoking or lifetime smoking between males and females
Exposure to Smoking
On items in the mFTQ measuring exposure to cigarette smokers, we found three environmental factors associated with the mFTQ score. Having more friends who smoke, living with smokers, and having parents who smoke were all associated with a greater physical dependence across all subjects (Friends: p<0.001; Living with: p<0.001; Parents: p=0.007). There were significant interaction effects on mFTQ score between each of the three environmental factors and ADHD status (Figure 2) indicating that exposure to smoking had a significantly greater difference in mean mFTQ scores in subjects with ADHD compared with controls.
Figure 2.
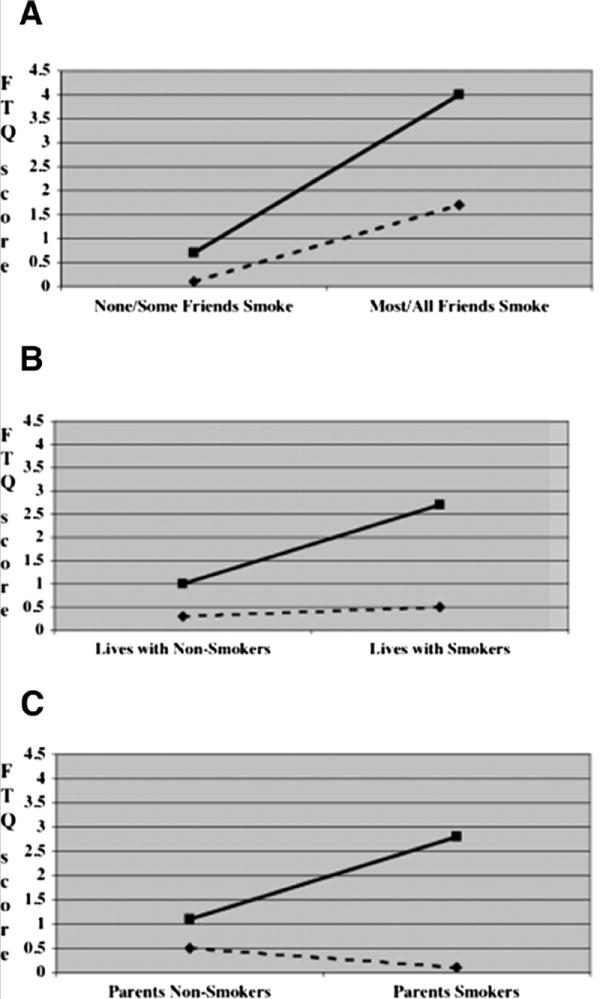
(a) Mean mFTQ score in young adults stratified by peer smoking and ADHD status; Control N = 84, ADHD N =74; F(1,154)=14.2, p<0.001. (b) Mean mFTQ score in young adults stratified by living with smokers and ADHD status; Control N = 84, ADHD N =74; F(1,154)=7.1, p=0.008. (c) Mean mFTQ score in young adults stratified by parental smoking and ADHD status; Control N = 81, ADHD N =72; Parents: F(1,149)=12.1, p<0.001.
Onset of Smoking
Subjects with ADHD reported a significantly earlier onset of smoking compared with controls (ADHD=13.9±2.7yrs, Control=15.2±2.0yrs, t(90)=2.4, p=0.02) – that was no longer significant when controlling for conduct disorder (CD; p=0.28). ADHD subjects with CD, compared with ADHD subjects without CD, had a significantly earlier onset of smoking (12.8±2.5yrs, and 14.8±2.6yrs, t(52)=2.8, p=0.007).
Discussion
The current findings support our hypotheses and replicate previous work highlighting that ADHD is a risk factor for early-onset and higher rates of cigarette smoking. Our data extend findings by showing more severe cigarette smoking associated with ADHD. We also found important relationships between ADHD symptoms, the environment, and the risk for smoking.
These findings further the research on ADHD as a major risk for earlier onset- and more severe cigarette smoking10, 11. Smokers with ADHD had significantly higher mFTQ scores, indicative of a more severe form of cigarette smoking relative to controls. Our examination of the intrinsic characteristics of ADHD related to smoking revealed that subjects with more ADHD symptoms including both inattentive and hyperactive/impulsive cluster symptoms reported greater FTQ scores. Our data replicates epidemiological work by Kollins et al7, showing a direct relationship between probability of smoking and both inattentive and hyperactive/impulsivity cluster symptoms. Interestingly, using different methodology, like Kollins et al 7, we found a linear relationship across our entire sample. Our data also support findings by Upadhyaya et al 21 who reported that among college students the presence of current symptoms of ADHD were directly related to risk for cigarette smoking (and substance use). Likewise, Tercyak et al 8 found a strong association in a community sample of adolescents between an increase in ADHD inattentive symptoms and an increased risk for cigarette smoking. Whereas Galera et al 22 found an association between cigarette smoking and ADHD symptoms in girls but not boys, in the current study, we did not find that sex mediated the relationship between ADHD, smoking risk, or severity.
The significant interaction between ADHD and environmental factors related to cigarette smoking is noteworthy. Similar to others8, we found that a relationship with a parent or peer smoker increased the severity of smoking across all subjects but that mFTQ scores were clinically and statistically higher in subjects with ADHD compared with controls. For instance, the likelihood to smoke in ADHD was over two-fold higher in the presence of parental smoking. Hence, ADHD appears to make an individual more vulnerable to the environment by nature of exposure to either peers or parental smoking. Our data are similar to others showing heightened vulnerability to Substance Use Disorders specifically in ADHD related to social class 23 or exposure of young adolescent to parental substance abuse at specific developmental periods 24. Our data also replicated findings that individuals with ADHD had the onset of cigarette smoking 1.5 years prior to non-ADHD controls. For instance, Downey et al 25 showed that adult smokers with ADHD began smoking at a younger age than non-ADHD smokers. Like Millberger et al 6, 26, we also found that the very early onset of cigarette smoking in our youth with ADHD was related to comorbid CD.
Although limited by an overrepresentation of reporting from females relative to males, we found interesting trends to more severe smoking in females with ADHD compared with males with ADHD. If replicated, our current data support others suggesting higher age-matched risk for substance use in girls relative to boys12, 13, 27 – that has been linked to earlier cigarette smoking5.Our findings are particularly interesting in that the girls with ADHD in our sample 28 had lower rates of CD compared with the boys with ADHD.
Although the reasons for the link between smoking and ADHD remain unclear, theoretical considerations suggest that the two conditions might share common underlying mechanisms. Notably, the putative underlying mechanisms of ADHD and the pharmacologic effects of nicotine in the brain are believed to share common neurotransmitter system29. For example, Krause et al30, using positron emission tomography, showed similar effects of nicotine and methylphenidate on the dopamine transporter protein. Moreover, a large preclinical literature supports the prominent effects of nicotine and nicotinic modulators on various aspects of cognition including attention, working memory and other executive functions29. There is also evidence that common genes may create a vulnerability to both ADHD and nicotine dependence, as mothers who smoked during pregnancy increased their child’s risk for hyperactivity31. Of interest, recent human data indicate a positive effect of nicotine32 or nicotinic modulators29 on ameliorating symptoms of ADHD.
Considering the well-documented morbidity and mortality associated with cigarette smoking, the continued findings of not only higher risk but also earlier onset and more severe cigarette smoking in ADHD merit discussion. Moreover, given recent findings documenting that smoking in youth with ADHD is an especially potent predictor of subsequent substance use and abuse in ADHD 33, prevention, identification, and early intervention of cigarette smokers with ADHD seems warranted. Even though the most prudent approach to reducing the risk for cigarette smoking in ADHD remains unclear, it appears clinically reasonable to educate youth and their families about the risk of cigarette smoking in ADHD, to optimally treat ADHD symptoms, and to provide ongoing monitoring and early aggressive treatment of cigarette smoking.
The results of this study need be considered in the light of their methodological limitations. Although subjects were a mean age of 19 years, not all subjects were completely through the period of risk. Smoking severity was by a self-report questionnaire (mFTQ) with more females than males responding, and not breath or urine measures. Among subjects with ADHD, a lack of current ADHD symptoms may represent remission, treatment effects, or underreporting (sensitivity)-especially in situations without parental indirect reports. Our sample sizes were relatively small, particularly when comparing smokers with and without ADHD and treated and untreated subjects with ADHD. Treatment was determined by direct and indirect report and may not reflect actual adherence to treatment.
Despite these limitations, our results show that ADHD is associated with earlier onset and more severe cigarette smoking compared with matched non-ADHD controls. A direct relationship between ADHD symptoms and the risk and severity of cigarette smoking exists. Given the significant risk that youth with ADHD have for developing a severe form of nicotine dependence, clinically relevant prevention and early intervention strategies aimed at cigarette smoking in youth with ADHD are necessary. Future research should examine the environmental and neurobiological interaction between ADHD and nicotine use, as well as effects of treatment, prevention and early intervention strategies on smoking in these high-risk youth. Additional research is also needed to examine correlations between ADHD severity and dimensional smoking measures, and the age effects on physical dependence to nicotine in adolescents and adults with ADHD.
Acknowledgments
This project was supported in part by grants R01 DA14419; DA016264 (T. Wilens) and 5U10DA015831 (T. Wilens CTN, site PI; R. Weiss, Northern New England PI) from the National Institute on Drug Abuse, Bethesda, MD.
Footnotes
Potential conflicts of interest information available at www.jpeds.com
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention (CDC) Summary of notifiable diseases, United States 1994. Morbidity and Mortality Weekly Report. 1994;42:1–73. [PubMed] [Google Scholar]
- 2.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Results on Adolescent Drug Use-Overview of Key Findings 2006 (NIH Publication No 07-6202) Vol. 2006. Bethesda, MD: National Institute on Drug Abuse; 2007. [Google Scholar]
- 3.Kandel D, Yamaguchi K. From beer to crack: Developmental patterns of drug involvement. American Journal of Public Health. 1993;83:851–855. doi: 10.2105/ajph.83.6.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kandel DB, Kessler RC, Margulies RZ. Antecedents of adolescent initiation into stages of drug use: A developmental analysis. Journal of Youth and Adolescence. 1978;7(1):13–40. doi: 10.1007/BF01538684. [DOI] [PubMed] [Google Scholar]
- 5.Biederman J, Monuteaux M, Mick E, et al. Is cigarette smoking a gateway drug to subsequent alcohol and illicit drug use disorders? A controlled study of youths with and without ADHD. Biol Psychiatry. 2006;59:258–264. doi: 10.1016/j.biopsych.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Milberger S, Biederman J, Faraone S, Chen L, Jones J. ADHD is associated with early initiation of cigarette smoking in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1997;36:37–44. doi: 10.1097/00004583-199701000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Kollins SH, McClernon FJ, Fuemmeler BF. Association between smoking and attention-deficit/hyperactivity disorder symptoms in a population-based sample of young adults. Arch Gen Psychiatry. 2005 Oct;62:1142–1147. doi: 10.1001/archpsyc.62.10.1142. [DOI] [PubMed] [Google Scholar]
- 8.Tercyak KP, Lerman C, Audrain J. Association of attention-deficit/hyperactivity disorder symptoms with levels of cigarette smoking in a community sample of adolescents. J Am Acad Child Adolesc Psychiatry. 2002;41:799–805. doi: 10.1097/00004583-200207000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Upadhyaya HP, Deas D, Brady KT, Kruesi M. Cigarette smoking and psychiatric comorbidity in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2002;41:1294–1305. doi: 10.1097/00004583-200211000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Fuemmeler BF, Kollins SH, McClernon FJ. Attention deficit hyperactivity disorder symptoms predict nicotine dependence and progression to regular smoking from adolescence to young adulthood. J Pediatr Psychol. 2007 Nov-Dec;32:1203–1213. doi: 10.1093/jpepsy/jsm051. [DOI] [PubMed] [Google Scholar]
- 11.Rodriguez D, Tercyak KP, Audrain-McGovern J. Effects of Inattention and Hyperactivity/Impulsivity Symptoms on Development of Nicotine Dependence from Mid Adolescence to Young Adulthood. J Pediatr Psychol. 2007 Oct 23; doi: 10.1093/jpepsy/jsm100. [DOI] [PubMed] [Google Scholar]
- 12.Biederman J, Faraone SV, Mick E, et al. Clinical correlates of ADHD in females: findings from a large group of girls ascertained from pediatric and psychiatric referral sources. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:966–975. doi: 10.1097/00004583-199908000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Disney ER, Elkins IJ, McGue M, Iacono WG. Effects of ADHD, conduct disorder, and gender on substance use and abuse in adolescence. Am J Psychiatry. 1999;156:1515–1521. doi: 10.1176/ajp.156.10.1515. [DOI] [PubMed] [Google Scholar]
- 14.Wilens T, Biederman J. Alcohol, drugs, and attention-deficit/hyperactivity disorder: A model for the study of addictions in youth. Journal of Psychopharmacology. 2006;20:580–588. doi: 10.1177/0269881105058776. [DOI] [PubMed] [Google Scholar]
- 15.McGough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder: findings from multiplex families. Am J Psychiatry. 2005 Sep;162:1621–1627. doi: 10.1176/appi.ajp.162.9.1621. [DOI] [PubMed] [Google Scholar]
- 16.Biederman J, Faraone SV, Mick E, et al. Clinical correlates of ADHD in females: Findings from a large group of girls ascertained from pediatric and psychiatric referral sources. J Am Acad Child Adolesc Psychiatry. 1999;38:966–975. doi: 10.1097/00004583-199908000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Biederman J, Faraone S, Milberger S, et al. Predictors of persistence and remission of ADHD into adolescence: Results from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1996;35:343–351. doi: 10.1097/00004583-199603000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Faraone SV, Tsuang MT. Methods in Psychiatric Genetics. In: Tohen M, Tsuang MT, Zahner GEP, editors. Textbook in Psychiatric Epidemiology. New York, NY: John Wiley; 1995. pp. 81–134. [Google Scholar]
- 19.Fagerstrom K. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addictive Behaviors. 1978;3:235–241. doi: 10.1016/0306-4603(78)90024-2. [DOI] [PubMed] [Google Scholar]
- 20.Prokhorov AV, Hudmon KS, de Moor CA, Kelder SH, Conroy JL, Ordway N. Nicotine dependence, withdrawal symptoms, and adolescents’ readiness to quit smoking. Nicotine Tob Res. 2001 May;3:151–155. doi: 10.1080/14622200110043068. [DOI] [PubMed] [Google Scholar]
- 21.Upadhyaya HP, Rose K, Wang W, et al. Attention deficit hyperactivity disorder, medication treatment, and substance use patterns among adolescents and young adults. J Child Adolesc Psychopharmacol. 2005;15:799–809. doi: 10.1089/cap.2005.15.799. [DOI] [PubMed] [Google Scholar]
- 22.Galera C, Fombonne E, Chastang JF, Bouvard M. Childhood hyperactivity-inattention symptoms and smoking in adolescence. Drug Alcohol Depend. 2005 Apr 4;78:101–108. doi: 10.1016/j.drugalcdep.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 23.Monuteaux M, Wilens T, Biederman J. Does social class predict substance problems in young adults with ADHD? Am J Addict. doi: 10.1080/10550490701525590. in press. [DOI] [PubMed] [Google Scholar]
- 24.Biederman J, Faraone SV, Monuteaux MC, Feighner JA. Patterns of alcohol and drug use in adolescents can be predicted by parental substance use disorders. Pediatrics. 2000;106:792–797. doi: 10.1542/peds.106.4.792. [DOI] [PubMed] [Google Scholar]
- 25.Downey K, Pomerleau CS, Pomerleau OF. Personality differences related to smoking and adult attention deficit hyperactivity disorder. J of Subst Abuse. 1996;8:129–135. doi: 10.1016/s0899-3289(96)90139-x. [DOI] [PubMed] [Google Scholar]
- 26.Milberger S, Biederman J, Faraone SV, Chen L, Jones J. Further evidence of an association between attention deficit hyperactivity disorder (ADHD) and cigarette smoking: Findings from a high risk sample of siblings. Am J Addict. 1997;6:205–217. [PubMed] [Google Scholar]
- 27.Milberger S, Biederman J, Faraone S, Wilens T, Chu M. Associations between ADHD and psychoactive substance use disorders: Findings from a longitudinal study of high-risk siblings of ADHD children. Am J Addict. 1997;6:318–329. [PubMed] [Google Scholar]
- 28.Biederman J, Monuteaux M, Mick E, et al. Psychopathology in females with attention-deficit/hyperactivity disorder: A controlled, five-year prospective study. Biol Psychiatry. 2006;60:1098–1105. doi: 10.1016/j.biopsych.2006.02.031. [DOI] [PubMed] [Google Scholar]
- 29.Wilens TE, Decker MW. Neuronal nicotinic receptor agonists for the treatment of attention-deficit/hyperactivity disorder: focus on cognition. Biochem Pharmacol. 2007 Oct 15;74:1212–1223. doi: 10.1016/j.bcp.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krause K, Dresel SH, Krause J, Kung HF, Tatsch K. Increased striatal dopamine transporter in adult patients with attention deficit hyperactivity disorder: effects of methylphenidate as measured by single photon emission computed tomography. Neurosci Lett. 2000;285:107–110. doi: 10.1016/s0304-3940(00)01040-5. [DOI] [PubMed] [Google Scholar]
- 31.Kotimaa AJ, Moilanen I, Taanila A, et al. Maternal Smoking and Hyperactivity in 8-Year-Old Children. J Am Acad Child Adolesc Psychiatry. 2003;42:826–833. doi: 10.1097/01.CHI.0000046866.56865.A2. [DOI] [PubMed] [Google Scholar]
- 32.Levin E, Conners C, Sparrow E, et al. Nicotine effects on adults with attention-deficit/hyperactivity disorder. Psychopharmacol. 1996;123:55–63. doi: 10.1007/BF02246281. [DOI] [PubMed] [Google Scholar]
- 33.Biederman J, Monuteaux M, Mick E, et al. Is Cigarette Smoking a Gateway Drug to Subsequent Alcohol and Illicit Drug Use Disorders? A Controlled Study of Youths with and without ADHD. Biol Psychiatry. 2006;59:258–264. doi: 10.1016/j.biopsych.2005.07.009. [DOI] [PubMed] [Google Scholar]


