Cardiovascular disease is the leading cause of death and disability in Canada (1,2). The increasing age of our population and unhealthy eating habits are associated with increases in obesity, diabetes and hypertension. This has led to dire predictions of increases in deaths and hospitalizations from cardiovascular disease, and has enormous implications for health care resource allocation (2). Globally, increases in cardiovascular disease have led to predictions that cardiovascular disease will be the leading cause of death and disability around the world within 20 years (3). Some have predicted that the steady progress toward increased longevity will be reversed by our currently unhealthy lifestyles (4).
In contrast with our lifestyles, advances have been made in medical therapies to prevent cardiovascular death and disability. These advances have been seen in both primary and secondary prevention. Further, our understanding of knowledge translation on prevention and treatment of cardiovascular disease has significantly advanced. Forums on cardiovascular health promotion have repeatedly stated that cardiovascular disease is largely preventable (4,5,6).
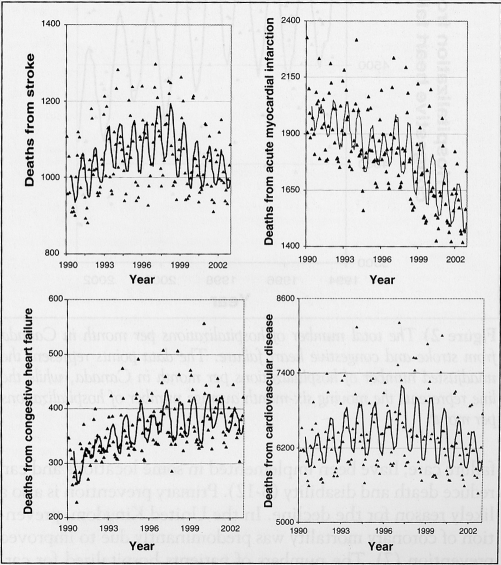
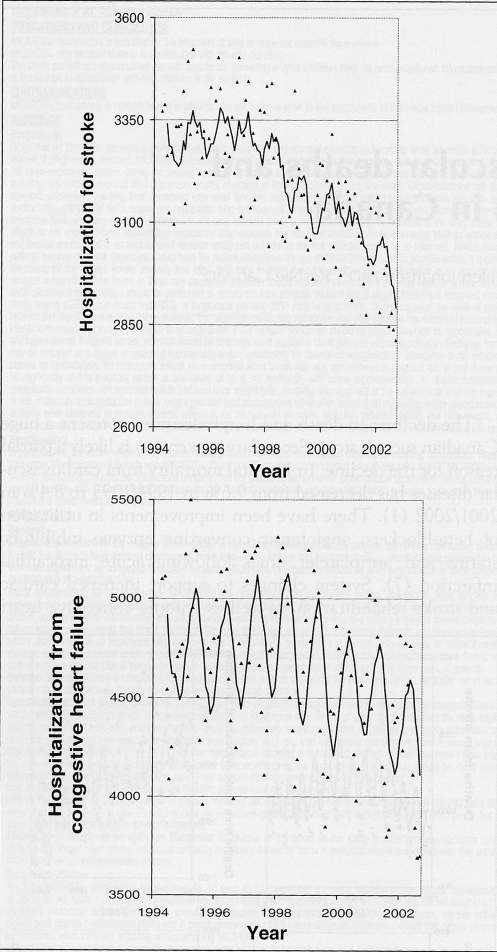
The Canadian Hypertension Education Program (CHEP) was developed to improve the management of hypertension and, hence, prevent cardiovascular events. As part of the CHEP, there is ongoing monitoring of deaths and hospitalization from stroke, congestive heart failure and acute myocardial infarction. Many of the analyses are in progress but in this editorial, we report the crude unadjusted mortality and hospitalization rates for these conditions. To our surprise, we found that since the late 1990s, there has been a decline in the total number of deaths from cardiovascular disease and specifically, stroke and congestive heart failure, both of which were rising earlier in the 1990s (Figure 1). Deaths from acute myocardial infarction have been declining throughout the 1990s (Figure 1). Further, there has been a decline in total hospitalizations for stroke and congestive heart failure since the late 1990s (Figure 2). Changes in coding for acute myocardial infarction currently make interpretation of our administrative data on hospitalization for acute myocardial infarction unreliable.
Figure 1.
The total number of deaths per month in Canada from stroke, congestive heart failure, acute myocardial infarction and cardiovascular disease. The data points represent the unadjusted number of deaths in Canada per month, while the line represents the moving six-month average number of monthly deaths
Figure 2.
The total number of hospitalizations per month in Canada from stroke and congestive heart failure. The data points represent the unadjusted number of hospitalizations per month in Canada, while the line represents the moving six-month average number of hospitalizations per month
The declines in death and hospitalization represent a huge Canadian success story. Secondary prevention is likely a partial reason for the decline. In-hospital mortality from cardiovascular diseases has decreased from 9.6% in 1994/1995 to 8.4% in 2001/2002 (1). There have been improvements in utilization of beta-blockers, angiotensin-converting enzyme inhibitors, statins and antiplatelet drugs following acute myocardial infarction (7). System changes to support increased cardiac and stroke rehabilitation, as well as chronic congestive heart failure care, have been implemented in some locations and can reduce death and disability (8–12). Primary prevention is also a likely reason for the decline. In the United Kingdom, prevention of coronary mortality was predominantly due to improved prevention (7). The numbers of patients hospitalized for cardiovascular diseases were also reduced, supporting improved prevention (1). Reductions in smoking and large increases in the use of statins, and in particular antihypertensive therapies, have occurred and would be expected to reduce event rates (2,13–15). The observational nature of the data preclude cause and effect conclusions, but further refined analysis using adjusted data and time series analysis are planned.
What are the implications? First, we think a very brief pause to celebrate is required because we have an interlude in the previous steady increases in cardiovascular death and hospitalization. The data are encouraging that a much broader, more extensively resourced effort supported by extensive system change to implement proven therapies in treatment and prevention will further reduce death, disability and more costly health care resource usage. These Canadian data suggest that applying resources to the prevention of cardiovascular death and disability is fruitful, even in a country with one of the lowest cardiovascular disease rates (4). However, we must remain cautious in our enthusiasm. Canada has an aging population, poor dietary habits prevail, there has not been a large increase in physical activity, obesity is increasing, and it is very likely that the prevalence of hypertension and diabetes is increasing (16,17). These trends could lead to increases in death and disability from cardiovascular disease and speak strongly to the need to address diet, physical activity and obesity with population health strategies.
Enhanced surveillance will allow for more insights into the successes and gaps in preventing cardiovascular death and disability and will support the development of more focused programs to address these increasing risks to our health.
ACKNOWLEDGEMENTS
These data are part of a collaborative effort of the CHEP Outcomes Research Task Force to develop a national hypertension surveillance program. Dr Campbell is supported in part by a CIHR Rx&D Canadian Chair in Hypertension Prevention and Control.
REFERENCES
- 1.Johansen H, Thillaiampalam S, Nguyen D, Sambell C. Diseases of the circulatory system – hospitalization and mortality. Health Rep. 2005;17:49–53. [PubMed] [Google Scholar]
- 2.Heart and Stroke Foundation of Canada. The changing face of heart disease and stroke in Canada 2000. Ottawa: Heart and Stroke Foundation of Canada; 1999. [Google Scholar]
- 3.Chockalingam A, Balaguer-Vintro I, Achutti A, et al. The World Heart Federation’s white book: Impending global pandemic of cardiovascular diseases: Challenges and opportunities for the prevention and control of cardiovascular diseases in developing countries and economies in transition. Can J Cardiol. 2000;16:227–9. [PubMed] [Google Scholar]
- 4.The Osaka Declaration. Health, Economics and Political Action: Stemming the Global Tide of Cardiovascular Disease. Fourth International Heart Health Conference; Osaka, Japan. 2001. < http://www.phac-aspc.gc.ca/ccdpc-cpcmc/cindi/pdf/osaka_e.pdf> (Version current at March 21, 2006) [Google Scholar]
- 5.International Heart Health Conference Advisory Board. The Victoria Declaration on Heart Health. British Columbia: Health and Welfare Canada; 1992. pp. 1–56. [Google Scholar]
- 6.The Catalonia Declaration: Investing in Heart Health. Advisory Board. 2nd International Heart Health Conference; Barcelona, Spain. June, 1995; Barcelona: Department of Health and Social Security, Autonomous Government of Catalonia; 1996. [Google Scholar]
- 7.Unal B, Critchley JA, Capewell S. Modelling the decline in coronary heart disease deaths in England and Wales, 1981–2000: Comparing contributions from primary prevention and secondary prevention. BMJ. 2005;331:614. doi: 10.1136/bmj.38561.633345.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haskell WL, Alderman EL, Fair JM, et al. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinical cardiac events in men and women with coronary artery disease. The Stanford Coronary Risk Intervention Project (SCRIP) Circulation. 1994;89:975–990. doi: 10.1161/01.cir.89.3.975. [DOI] [PubMed] [Google Scholar]
- 9.Rich MW. Multidisciplinary heart failure clinics: Are they effective in Canada? CMAJ. 2005;173:53–4. doi: 10.1503/cmaj.050705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hunt SA, Abraham WT, Chin MH, et al. Bethesda: American College of Cardiology Foundation; 2005. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) [DOI] [PubMed] [Google Scholar]
- 11.Antman EM, Anbe DT, Armstrong PW, et al. Bethesda: American College of Cardiology/American Heart Association; 2004. ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction) [DOI] [PubMed] [Google Scholar]
- 12.Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: Secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143:659–72. doi: 10.7326/0003-4819-143-9-200511010-00010. [DOI] [PubMed] [Google Scholar]
- 13.Campbell NR, Tu K, Brant R, Duong-Hua M, McAlister FA Canadian Hypertension Education Program Outcomes Research Task Force. The impact of the Canadian Hypertension Education Program on antihypertensive prescribing trends. Hypertension. 2006;47:22–8. doi: 10.1161/01.HYP.0000196269.98463.fd. [DOI] [PubMed] [Google Scholar]
- 14.Campbell NR, McAlister FA, Brant R, et al. Canadian Hypertension Education Process and Evaluation Committee. Temporal trends in antihypertensive drug prescriptions in Canada before and after introduction of the Canadian Hypertension Education Program. J Hypertens. 2003;21:1591–7. doi: 10.1097/00004872-200308000-00025. [DOI] [PubMed] [Google Scholar]
- 15.Carroll MD, Lacher DA, Sorlie PD, et al. Trends in serum lipids and lipoproteins of adults, 1960–2002. JAMA. 2005;294:1773–81. doi: 10.1001/jama.294.14.1773. [DOI] [PubMed] [Google Scholar]
- 16.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L NEDCOM, the Netherlands Epidemiology and Demography Compression of Morbidity Research Group. Obesity in adulthood and its consequences for life expectancy: A life-table analysis. Ann Intern Med. 2003;138:24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 17.Katzmarzyk PT. The Canadian obesity epidemic, 1985–1998. CMAJ. 2002;166:1039–40. [PMC free article] [PubMed] [Google Scholar]