Abstract
To maximize the benefits of preventive therapy, lipid and hypertension guidelines increasingly recommend that high-risk individuals be targeted for treatment. An individual’s risk of developing cardiovascular disease depends on many risk factors, such as age, sex, blood pressure, blood lipid levels, body weight, physical fitness, smoking habits and familial predisposition. Multivariable statistical models have therefore been developed to better estimate the global risk of future coronary events and stroke. A Canadian model is not currently available because a prospective cohort of sufficient size has not been followed in Canada. Therefore, global risk assessment among Canadians can only be completed using models developed in the United States or Europe. In the present review, cardiovascular risk tools are identified that may be appropriate for Canadians, including those based on the Framingham model, the Cardiovascular Life Expectancy Model, the United Kingdom Prospective Diabetes Study (UKPDS) model and the Systematic COronary Risk Evaluation (SCORE) model. The accuracy of the Framingham model and the Cardiovascular Life Expectancy Model are also evaluated using data from a small, prospective Canadian cohort. Finally, a framework is proposed to assist health care professionals in choosing the global risk tool most appropriate for their patients.
Keywords: Cardiovascular risk, Dyslipidemic, Hypertension, Risk factors
Abstract
Pour maximiser les bienfaits de la thérapie préventive, les lignes directrices sur la lipidémie et l’hypertension recommandent de plus en plus de cibler les personnes très vulnérables pour les traiter. Le risque personnel de souffrir d’une maladie cardiovasculaire dépend de nombreux facteurs de risque, tels que l’âge, le sexe, la tension artérielle, le taux de lipides sanguins, le poids, la condition physique, les habitudes reliées au tabagisme et les prédispositions familiales. Des modèles statistiques multivariables ont donc été mis au point pour mieux évaluer le risque global de futurs problèmes coronariens et accidents vasculaires cérébraux. Il n’existe pas de modèle canadien parce qu’aucune cohorte de taille suffisante n’a été suivie au Canada. Par conséquent, l’évaluation globale du risque chez les Canadiens ne peut être effectuée qu’à l’aide de modèles mis au point aux États-Unis ou en Europe. Dans la présente analyse, les outils de risque cardiovasculaire susceptibles de convenir aux Canadiens sont présentés, soit ceux qui se fondent sur le modèle de Framingham, le modèle d’espérance de vie cardiovasculaire, le modèle de l’étude prospective UKPDS sur le diabète au Royaume-Uni et le modèle SCORE d’évaluation systématique du risque coronarien. L’exactitude du modèle de Framingham et du modèle d’espérance de vie cardiovasculaire est évaluée à l’aide de données tirées d’une petite cohorte canadienne prospective. Enfin, une structure est proposée afin d’aider les professionnels de la santé à choisir l’outil de risque global qui convient le mieux à leur patient.
Despite the continuing improvements in treating cardiovascular disease among Canadians, coronary artery disease and stroke remain among the most common causes of premature mortality and disability in adults. Accordingly, the treatment of modifiable risk factors, such as hypertension and dyslipidemia, to prevent or delay the development of cardiovascular disease remains an essential component of medical therapy and public health policy.
The clinical benefits of risk factor modification to prevent cardiovascular events have been clearly demonstrated in randomized clinical trials. Nonetheless, these benefits may be associated with important treatment complications, minor side effects and the substantial, direct health care costs of lifelong therapy. To maximize the net benefits of preventive therapy, evolving treatment guidelines increasingly recommend that health care professionals target high-risk individuals for therapy. In this way, the potential risks of therapy are offset by a substantial reduction in the risk of cardiovascular disease (1). Targeting high-risk individuals also maximizes the cost-effectiveness of treatment.
An individual’s risk of developing cardiovascular disease depends on many risk factors, such as age, sex, blood pressure, blood lipid levels, body weight, physical fitness, smoking habits and familial predisposition. Multivariable statistical models, based on prospective cohort data, have therefore been developed to better estimate the global risk of future coronary events and stroke. A Canadian model is not currently available for calculating the risk of cardiovascular disease among Canadian men and women. Therefore, global risk assessment among Canadians can only be completed using statistical tools based on adults followed in the United States or Europe. Members of the Canadian Hypertension Society recognize that global risk assessment has become an essential component of contemporary hypertension therapy. However, in the absence of Canadian multivariable risk equations, it remains unclear whether currently available risk assessment tools can be used to improve the effectiveness and cost-effectiveness of hypertension treatment.
In the present review, cardiovascular risk assessment models are identified that may be appropriate for Canadians. Each model’s strengths and weaknesses are considered in a framework of assisting health care professionals in choosing the global risk tool most appropriate for their patients. As a means of external validation, we compared the accuracy of two risk models in a prospectively followed cohort of Canadians. Finally, specific issues for future research were identified to support the development of better risk assessment strategies for Canadian adults.
STUDY DESIGN
Evaluating cardiovascular models
At the request of the Canadian Hypertension Society, a committee of clinicians and researchers was assembled to review currently available cardiovascular risk assessment tools and make recommendations for their use by Canadian health care professionals. The committee included Steven Grover (Chair), Brenda Hemmelgarn, Lawrence Joseph, Alain Milot and Guy Tremblay. Committee members recommended key publications for inclusion in the report based on their individual expertise and the annual critical appraisals conducted for the Global Risk Assessment subcommittee of the Canadian Hypertension Education Program. These critical appraisals included an annual comprehensive MEDLINE search of all published articles on cardiovascular risk assessment. After circulating the publications to all committee members, a preliminary document was developed.
Available risk assessment models were considered across six major criteria. First, the likelihood that the cohort used to develop a model would be representative of Canadian men and women was considered. Second, the risk factors required for measurement had to be readily available in a Canadian primary care clinical setting. Third, the clinical outcomes predicted by the model had to be clinically important to Canadian health care professionals and patients. Fourth, readily available applications of the model that could be used by Canadian health care professionals were necessary.
The fifth and sixth criteria focused on the accuracy of the model. External validity was demonstrated if the model was specifically developed on one cohort of individuals and then validated on a second cohort independent of the first. If external validation was not available, then internal validation was considered when the model was used to predict events among individuals in the same cohort on which the model was developed. The ultimate test of any model for Canadians will be evidence of external validation on a Canadian cohort.
External validation on a Canadian cohort
Among available risk models, the accuracy of two models to estimate the risk of fatal coronary events on a prospectively followed cohort of Canadians was selected and compared. Models included the published Framingham Heart Study risk equations and the Cardiovascular Life Expectancy Model (CLEM), based on American data from the Lipid Research Clinics (LRC) Follow-Up Cohort (2,3). These models were selected because they were able to use the baseline data available in the Canadian cohort (age, sex, total cholesterol/high-density lipoprotein [HDL] ratio, blood pressure, and the presence of cigarette smoking and/or diabetes) and predict fatal events, which were the only available outcome. The resulting analyses also included individuals with diabetes at baseline to maximize the number of outcomes included in the validation.
The two risk assessment models were tested on Hamilton-and Toronto-based Canadian subjects (n=1173) who were between 30 and 67 years of age and were enrolled in the LRC Follow-Up Cohort study (4). Once the 10-year risk was calculated for each subject with each model, the results were compared with the fatal coronary events actually observed in this Canadian cohort. Receiver operating characteristic curves were used to calculate the discriminating ability of each model. Subjects were then rank ordered according to their risk level and stratified into risk quartiles. To evaluate the calibration of each model, the mean estimated fatal coronary risk of each quartile was then compared with the mean event rate actually observed over 10 years of follow-up.
RESULTS
Overview of cardiovascular models
Four models are summarized in the present report. Focusing on coronary events, there is the Framingham Heart Study model (2,5–7), the CLEM based on the LRC Follow-Up Cohort (3) and the United Kingdom Prospective Diabetes Study (UKPDS) model (8). Each of these studies has also published a model to predict the future risk of stroke (3,9,10). Finally, the risks of fatal stroke and fatal coronary events are combined in the risk of fatal cardiovascular events, provided by the Systematic COronary Risk Evaluation (SCORE) model (11).
A description of the cohort used for each model is provided in Table 1. The Framingham cohort included over 5000 American men and women between the ages of 30 and 74 years who were free of cardiovascular disease; these individuals were followed for up to 12 years. The CLEM included over 3000 men and women between the ages of 35 and 74 years, and were recruited from the United States and Canada. Individuals with and without previously diagnosed cardiovascular disease were included in the cohort and followed for approximately 12 years. The UKPDS cohort focused only on individuals with newly diagnosed diabetes mellitus but without a recent myocardial infarction, angina or congestive heart failure. Over 4000 men and women between the ages of 25 to 65 years were followed for approximately 10.5 years. The SCORE cohort included over 200,000 men and women without previous myocardial infarction recruited from 12 European countries. Individuals between the ages of 19 and 80 years were followed for approximately 10 years.
TABLE 1.
Description of cardiovascular risk assessment models
| Risk model | Cohort | Risk factors | Outcomes | Validation | Canadian validation or calibration | Applications |
|---|---|---|---|---|---|---|
| A. Individuals without CVD or diabetes | ||||||
| Framingham model – CHD, 1991 (2) | 2489 men and 2857 women free of CVD from Framingham, Massachusetts, USA (ages 30 to 74 years, mean approx 49 years, follow-up 12 years) | Sex-specific, age, SBP, smoking, diabetes, TC/HDL or LDL/HDL or TC, HDL | Total CHD or hard CHD (excluding angina) | External validation among Americans and Europeans | Calibration using CHHS | 10-year risk of total |
| Framingham model – stroke, 1991 (9) | 2372 men and 3362 women without previous stroke from Framingham, Massachusetts, USA (ages 55 to 84 years, mean approx 65.5 years, follow-up 10 years) | Sex-specific, age, SBP, smoking, diabetes, antihypertensive Tx, atrial fibrillation, LVH | Stroke or TIA | 10-year risk of stroke for those without prior stroke, ages 54 to 86 years. Available in charts, software and Web sites | ||
| Cardiovascular Life Expectancy Model – CHD, 1998 (3) | 3678 men and women in the LRC Follow-Up Cohort; 15% random sample from the USA and Canada (ages 35 to 74 years, follow-up 12.2 years) | Sex, age, SBP and DBP, smoking, diabetes, TC/HDL or LDL/HDL, previous CVD | Fatal CHD | External validation on published clinical trials and US Life Tables | Calibration using CHHS | 10-year risk of fatal CHD or total CHD, ages 35 to 79 years. CVD risk-adjusted life expectancy |
| Cardiovascular Life Expectancy Model – stroke, 1998 (3) | 3678 men and women in the LRC Follow-Up Cohort; 15% random sample from the USA and Canada (ages 35 to 74 years, follow-up 12.2 years) | Age, SBP and DBP, smoking, LDL/HDL, previous CVD | Fatal stroke | External validation on published clinical trials and US Life Tables | Calibration using CHHS | 10-year risk of fatal stroke or total stroke, ages 35 to 79 years. CVD risk-adjusted life expectancy |
| SCORE – CVD, 2003 (11) | 117,098 men and 88,080 women without previous MI from 12 European countries (ages 19 to 80 years, follow-up 10 years) | Sex, age, SBP, smoking, TC, HDL | Fatal CVD | Internal validation among southern Europeans and northern Europeans. External validation using all-cause mortality among patients in an American cardiac rehabilitation setting | 10-year risk of fatal CVD, ages 40 to 65 years. Available in charts, software and Web sites | |
| B. Individuals with CVD | ||||||
| Cardiovascular Life Expectancy Model – CHD, 1998 (3) | 3678 men and women in the LRC Follow-Up Cohort; 15% random sample from the USA and Canada (ages 35 to 74 years, follow-up 12.2 years) | Sex, age, SBP and DBP, smoking, diabetes, TC/HDL or LDL/HDL, previous CVD | Fatal CHD | External validation on published clinical trials | Calibration using CHHS | 10-year risk of fatal CHD or total CHD, ages 35 to 79 years. CVD risk-adjusted life expectancy. Available in software and Web sites |
| Cardiovascular Life Expectancy Model – stroke, 1998 (3) | 3678 men and women in the LRC Follow-Up Cohort; 15% random sample from the USA and Canada (ages 35 to 74 years, follow-up 12.2 years) | Age, SBP and DBP, smoking, LDL/HDL, previous CVD | Fatal stroke | External validation on published clinical trials | Calibration using CHHS | 10-year risk of fatal stroke or total stroke, ages 35 to 79 years. CVD risk-adjusted life expectancy. Available in software and Web sites |
| Framingham model – CHD, 2000 (6) | 4823 men and 5333 women from Framingham, Massachusetts, USA (ages 35 to 74 years, follow-up =4 years) | Sex-specific, age, SBP, smoking, diabetes, TC/HDL | Total hospitalized CHD | 10-year risk of total CHD for those without CVD, ages 30 to 74 years. Available in charts, software and Web sites | ||
| Framingham model – stroke, 1991 (9) | 2372 men and 3362 women without previous stroke from Framingham, Massachusetts (ages 55 to 84 years, mean approx 65.5 years, follow-up 10 years) | Sex-specific, age, SBP, smoking, diabetes, antihypertensive Tx, atrial fibrillation, LVH | Stroke or TIA | 10-year risk of stroke for those without prior stroke, ages 54 to 86 years. Available in charts, software and Web sites | ||
| C. Individuals with diabetes | ||||||
| Cardiovascular Life Expectancy Model – CHD, 1998 (3) | 3678 men and women in the LRC Follow-Up Cohort; 15% random sample from the USA and Canada (ages 35 to 74 years, follow-up 12.2 years) | Sex, age, SBP and DBP, smoking, diabetes, TC/HDL or LDL/HDL, previous CVD | Fatal CHD | External validation on published clinical trials and national survival statistics | Calibration using CHHS | 10-year risk of fatal CHD or total CHD, ages 35 to 79 years. CVD risk-adjusted life expectancy |
| Cardiovascular Life Expectancy Model – stroke, 1998 (3) | 3678 men and women in the LRC Follow-Up Cohort; 15% random sample from the USA and Canada (ages 35 to 74 years, follow-up 12.2 years) | Age, SBP and DBP, smoking, LDL/HDL, previous CVD | Fatal stroke | External validation on published clinical trials and national survival statistics | Calibration using CHHS | 10-year risk of fatal stroke or total stroke, ages 35 to 79 years. CVD risk-adjusted life expectancy |
| SCORE – CVD, 2003 (11) | 117,098 men and 88,080 women without previous MI from 12 European countries (ages 19 to 80 years, follow-up 10 years) | Sex, age, SBP, smoking, TC, HDL, model uses diabetes multiplier (2× for men, 4× for women) | Fatal CVD | Internal validation among southern Europeans and northern Europeans. External validation using all-cause mortality among patients in an American cardiac rehabilitation setting | 10-year risk of fatal CVD, ages 40 to 65 years. Available in charts, software and Web sites | |
| UKPDS – CHD, 2001 (8) | 2643 men and 1897 women with newly diagnosed DM without recent MI, angina or CHF from the UK (ages 25 to 65 years, mean approx 52 years, follow-up 10.5 years) | Sex, age, SBP, smoking, TC/HDL, HbA1c, diabetes duration, ethnic group | Fatal CHD and nonfatal MI | Internal validation on UKPDS survival rates | 10-year risk of fatal CHD or nonfatal MI, ages 35 to 65 years with diabetes. Available in charts, software and Web sites | |
| UKPDS – stroke, 2001 (10) | 4549 men and women without previous stroke from the UK (ages 25 to 65 years, mean approx 52 years, follow-up 10.5 years) | Sex, age, SBP, smoking, TC/HDL, diabetes duration, atrial fibrillation | Stroke | Internal validation on UKPDS survival rates. External validation on events in WESDR cohort | Risk of stroke over the next 4 to 20 years, ages 35 to 65 years with diabetes. Available in charts, software and Web sites | |
approx Approximately; CHD Coronary heart disease; CHHS Canadian Heart Health Surveys; CVD Cardiovascular disease; DM Diabetes mellitus; DPB Diastolic blood pressure; HbA1c Hemoglobin A1c; HDL High-density lipoprotein; LDL Low-density lipoprotein; LRC Lipid Research Clinics; LVH Left ventricular hypertrophy; MI Myocardial infarction; SBP Systolic blood pressure; SCORE Systematic COronary Risk Evaluation; TC Total cholesterol; TIA Transient ischemic attack; Tx Treatment; UKPDS United Kingdom Prospective Diabetes Study; USA United States of America; WESDR Wisconsin Epidemiologic Study of Diabetic Retinopathy
Risk factors common to all of the models include age, sex, smoking habits, total cholesterol and systolic blood pressure. The total cholesterol/HDL ratio or low-density lipoprotein/HDL ratio is used by the Framingham model, UKPDS model and CLEM. Using the SCORE model, a risk assessment score can be completed with total cholesterol and HDL or total cholesterol alone. The presence of diabetes is a common independent risk factor in all models except for SCORE, in which a diabetes multiplier is available or the model can be restricted to adults without diabetes. Framingham also provides a second model that can be used only among individuals free of diabetes. Additional risk factors that are used sporadically include the presence of antihypertensive therapy, atrial fibrillation, left ventricular hypertrophy, previous cardiovascular disease, hemoglobin A1C and the duration of diabetes.
Outcomes that are forecast by each model include fatal cardiovascular events (coronary events and stroke) in SCORE, fatal coronary disease and fatal stroke in CLEM, total coronary events, stroke or transient ischemic attacks in the Framingham model, and stroke, fatal coronary events and nonfatal myocardial infarction in the UKPDS model.
External validation of the Framingham model has been completed among American and European cohorts (5,12). For SCORE, internal calibration was completed among southern and northern Europeans (11). External calibration of SCORE using all-cause mortality has also been completed among a cohort of patients followed in an American cardiovascular rehabilitation program (13). In the UKPDS model, forecasted stroke has been validated externally using data from the Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) cohort (10), and internal validation for coronary events was completed on the UKPDS cohort (8). Fatal coronary events and stroke in the CLEM have been externally validated on published data from nine randomized clinical trials (3,14,15). Forecasted life expectancy has also been compared with national survival statistics using United States Life Tables (16).
To date, there have been no published studies demonstrating the validity of these models on the Canadian population. Both the Framingham Heart Study and the Cardiovascular Life Expectancy Model have been applied to data from the Canadian Heart Health Surveys (17) so that individual risk estimates can be compared with population estimates for individuals of the same age and sex (18,19).
Common applications for each risk model include risk charts, software for use on desktop computers, personal digital assistant applications and public domain Web sites. Most applications are available primarily in English. However, the CLEM is also available in French.
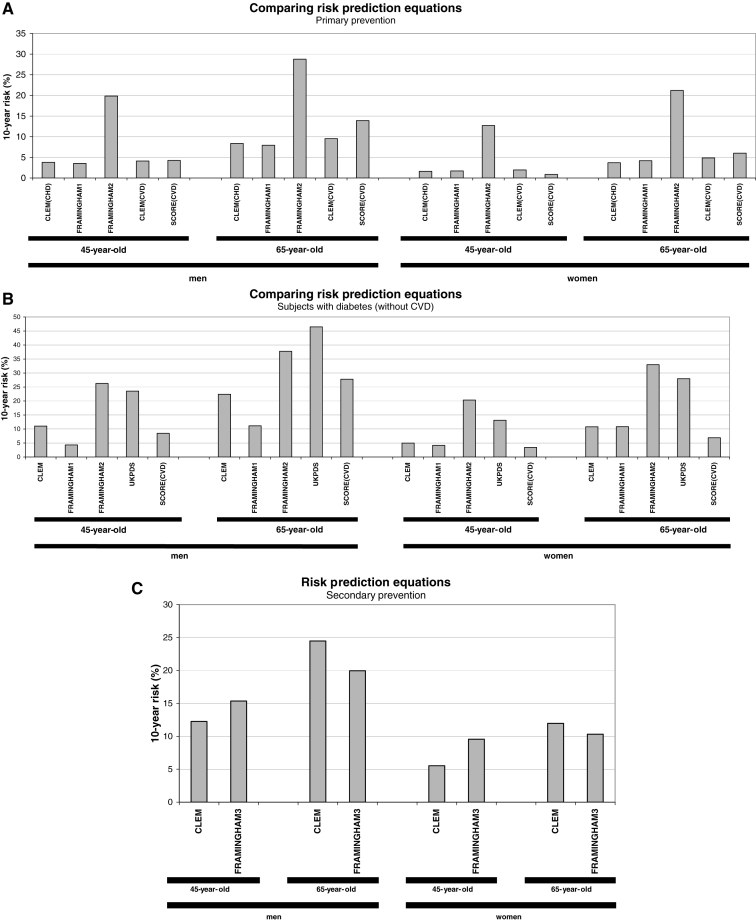
To better understand the similarities and differences between the risk models, 10-year coronary risk was calculated using each model. Hypothetical hypertensive patients were considered, including a 45-year-old woman, a 45-year-old man, a 65-year-old woman and a 65-year-old man (Figure 1). The absolute 10-year coronary risk for individuals without cardiovascular disease or diabetes (Figure 1A), individuals with diabetes (Figure 1B) and individuals with cardiovascular disease (Figure 1C) were then compared, using each model as appropriate.
Figure 1.
A Risk prediction estimates in primary prevention among patients without cardiovascular disease or diabetes. CLEM(CHD) and CLEM(CVD) refer to the Cardiovascular Life Expectancy Model estimates of coronary death or cardiovascular death, respectively, based on the Lipid Research Clinics dataset (3). Framingham1 and Framingham2 refer to estimates for coronary death and all coronary events, respectively, based on the Framingham dataset (2). SCORE(CVD) refers to cardiovascular death estimates based on the Systematic COronary Risk Evaluation dataset (11). B Risk prediction estimates in primary prevention among diabetic patients without cardiovascular disease. CLEM refers to the Cardiovascular Life Expectancy Model estimates of coronary death based on the Lipid Research Clinics dataset. UKPDS refers to coronary events based on the United Kingdom Prospective Diabetes Study dataset (8). SCORE(CVD) refers to cardiovascular death estimates based on the SCORE dataset using a diabetes multiplier (2× for men, 4× for women). C Risk prediction estimates in secondary prevention among patients with cardiovascular disease. CLEM refers to the Cardiovascular Life Expectancy Model estimates of coronary death over 10 years based on the Lipid Research Clinics dataset. Framingham3 refers to estimates for all coronary events over four years based on the Framingham dataset
External validation of models on a Canadian cohort
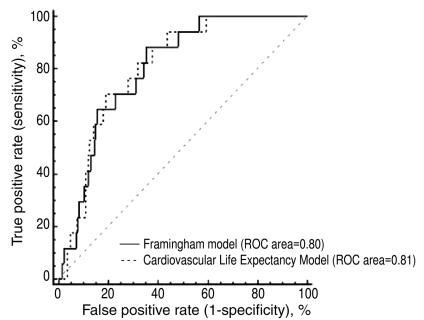
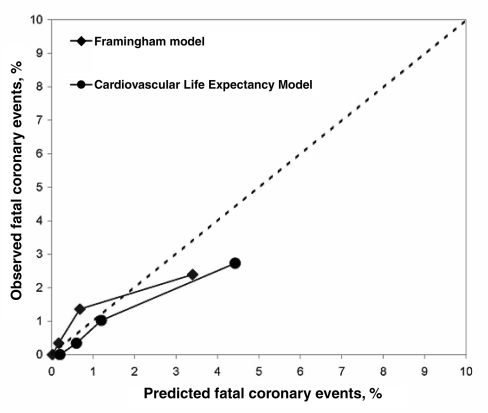
The baseline characteristics of Canadians enrolled in the LRC study are summarized in Table 2. There were 17 coronary deaths among the Canadian LRC subjects. The Framingham and CLEM models demonstrated very similar results despite being developed on two independent cohorts. The area under the receiver operating characteristic curves for the Framingham and CLEM models were 0.80 (95% CI 0.78 to 0.83) and 0.81 (95% CI 0.78 to 0.83), respectively, indicating reasonably good discriminating ability for both models (Figure 2). Model calibration based on the observed 10-year incidence rate of coronary deaths versus the predicted rate was also reasonably accurate (Figure 3).
TABLE 2.
Baseline characteristics of Canadian subjects (n=1173) in the Lipid Research Clinics Follow-Up Cohort
| Characteristic | Mean value | Minimum | Maximum |
|---|---|---|---|
| Female sex, % | 28 | ||
| Age, years | 44 | 30 | 67 |
| Total cholesterol, mmol/L | 5.77 | 2.88 | 13.68 |
| HDL cholesterol, mmol/L | 1.28 | 0.54 | 2.72 |
| Systolic blood pressure, mmHg | 121 | 83 | 211 |
| Diastolic blood pressure, mmHg | 78 | 47 | 119 |
| Using blood pressure medication(s), % | 4 | ||
| Currently smoking cigarettes, % | 49 | ||
| Known diabetes, % | 5 |
HDL High-density lipoprotein
Figure 2.
Receiver operating characteristic (ROC) curves demonstrating the discriminating ability of the Framingham model and the Cardiovascular Life Expectancy Model when forecasting coronary death among Canadians in the Lipid Research Clinics Follow-Up Cohort
Figure 3.
Calibration of the Framingham model and the Cardiovascular Life Expectancy Model. Each model was used to estimate the risk of each Canadian subject in the Lipid Research Clinics Follow-Up Cohort, and all subjects were then rank-ordered from the lowest to highest risk. Dividing the cohort into risk quartiles, the mean risk estimated for each quartile was compared with the coronary death rate actually observed
Unfortunately, the small number of cardiac events in this Canadian cohort provided rather limited data on which to validate these risk models. The validation was also limited by the narrow range of values in each risk quartile, providing only preliminary evidence of reasonable calibration among individuals who, on average, were at low to moderate risk (less than 5% risk of fatal coronary disease over 10 years of follow-up, which corresponds to a risk of coronary death and nonfatal myocardial infarction of less than 15%). It therefore remains to be determined to what extent these models accurately predict the 10-year risk of fatal coronary disease and nonfatal myocardial infarction among individuals whose actual event rate is between 10% and 20% or above 20%.
CONCLUSIONS AND RECOMMENDATIONS
In the absence of a Canada-specific risk model, it is difficult to base hypertension treatment recommendations on absolute risk thresholds. For instance, if one recommends that all hypertensive individuals with an absolute risk over 20% require therapy, then one must be confident that the risk assessment tool is accurate for Canadians. Even a Canadian risk model will have some inherent imprecision. Accordingly, detailed guidelines based on precise thresholds for treatment are not advisable at this time. Additional caution is necessary when risk is estimated with models that have not been validated on Canadians.
Nonetheless, global risk assessment is an important tool to assist physicians and other health care professionals in identifying hypertensive individuals who are most likely to benefit from therapy (1,20). Each of the four models discussed herein, when used appropriately, can provide useful information in this regard. As long as the model can adequately discriminate between high-risk and low-risk individuals, as evidenced by external validation, or at least internal validation, then it can be used to identify patients at increased risk.
If precise thresholds for initiating therapy are not feasible, then each model can be used to compare the risk of an individual patient with normative data for Canadians of the same age and sex. For instance, the absolute 10-year risk of a hypothetical 45-year-old woman (described in Figure 1A) could be compared with the risk distribution among 45-year-old Canadian women using data from the Canadian Heart Health Surveys (17) or any other representative data set that is available. Individuals may be selected for treatment if the absolute risk is above average or any other agreed-upon threshold, such as the upper tertile, quartile, quintile, etc. Such an approach would provide one additional tool to help patients and health care professionals make more informed decisions. Despite the potential usefulness of global risk assessment, absolute risk levels should not be an absolute substitute for thoughtful clinical judgment or an individual patient’s preference.
APPENDIX.
| Framingham stroke calculator |
| The Framingham Stroke Calculator (21) can be found at <www.nhlbi.nih.gov/about/framingham/stroke.htm> |
| Framingham coronary heart disease risk prediction score sheets |
| The following score sheets (22) can be found at <www.nhlbi.nih.gov/about/framingham/riskabs.htm>: |
|
| Cardiovascular Life Expectancy Model |
| This calculator (22,23) can be found at <www.chiprehab.com> |
| SCORE calculator |
| A SCORE calculator (24) can be found at <www.escardio.org/knowledge/decision_tools/heartscore> |
| UKPDS risk engine |
| This risk engine (25) can be downloaded free of charge at <www.dtu.ox.ac.uk/index.html?maindoc=/riskengine> |
REFERENCES
- 1.Padwal R, Straus SE, McAlister FA. Evidence based management of hypertension. Cardiovascular risk factors and their effects on the decision to treat hypertension: Evidence based review. BMJ. 2001;322:977–80. doi: 10.1136/bmj.322.7292.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson KM, Wilson PW, Odell PM, Kannel WB. An updated coronary risk profile. A statement for health professionals. Circulation. 1991;83:356–62. doi: 10.1161/01.cir.83.1.356. [DOI] [PubMed] [Google Scholar]
- 3.Grover SA, Paquet S, Levinton C, Coupal L, Zowall H. Estimating the benefits of modifying risk factors of cardiovascular disease: A comparison of primary vs secondary prevention. Arch Intern Med. 1998;158:655–62. doi: 10.1001/archinte.158.6.655. [DOI] [PubMed] [Google Scholar]
- 4.Heiss G, Tamir I, Davis CE, et al. Lipoprotein-cholesterol distributions in selected North American populations: The lipid research clinics program prevalence study. Circulation. 1980;61:302–15. doi: 10.1161/01.cir.61.2.302. [DOI] [PubMed] [Google Scholar]
- 5.D’Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P. CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores: Results of a multiple ethnic groups investigation. JAMA. 2001;286:180–7. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 6.D’Agostino RB, Russell MW, Huse DM, et al. Primary and subsequent coronary risk appraisal: New results from the Framingham study. Am Heart J. 2000;139:272–81. doi: 10.1067/mhj.2000.96469. (Erratum in 2002;143:21) [DOI] [PubMed] [Google Scholar]
- 7.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 8.Stevens RJ, Kothari V, Adler AI, Stratton IM United Kingdom Prospective Diabetes Study (UKPDS) Group. The UKPDS risk engine: A model for the risk of coronary heart disease in Type II diabetes (UKPDS 56) Clin Sci (Lond) 2001;101:671–9. (Erratum in 2002;102:679) [PubMed] [Google Scholar]
- 9.Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: A risk profile from the Framingham Study. Stroke. 1991;22:312–8. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- 10.Kothari V, Stevens RJ, Adler AI, et al. UKPDS 60: Risk of stroke in type 2 diabetes estimated by the UK Prospective Diabetes Study risk engine. Stroke. 2002;33:1776–81. doi: 10.1161/01.str.0000020091.07144.c7. [DOI] [PubMed] [Google Scholar]
- 11.Conroy RM, Pyorala K, Fitzgerald AP, et al. SCORE project group. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 12.Grover SA, Coupal L, Hu XP. Identifying adults at increased risk of coronary disease. How well do the current cholesterol guidelines work? JAMA. 1995;274:801–6. [PubMed] [Google Scholar]
- 13.Aktas MK, Ozduran V, Pothier CE, Lang R, Lauer MS. Global risk scores and exercise testing for predicting all-cause mortality in a preventive medicine program. JAMA. 2004;292:1462–8. doi: 10.1001/jama.292.12.1462. [DOI] [PubMed] [Google Scholar]
- 14.Grover SA, Coupal L, Zowall H, Dorais M. Cost-effectiveness of treating hyperlipidemia in the presence of diabetes: Who should be treated? Circulation. 2000;102:722–7. doi: 10.1161/01.cir.102.7.722. [DOI] [PubMed] [Google Scholar]
- 15.Grover SA, Dorais M, Coupal L. Improving the prediction of cardiovascular risk: Interaction between LDL and HDL cholesterol. Epidemiology. 2003;14:315–20. [PubMed] [Google Scholar]
- 16.Grover SA, Coupal L, Gilmore N, Mukherjee J. Impact of dyslipidemia associated with Highly Active Antiretroviral Therapy (HAART) on cardiovascular risk and life expectancy. Am J Cardiol. 2005;95:586–91. doi: 10.1016/j.amjcard.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 17.MacLean DR, Petrasovits A, Nargundkar M, et al. Canadian heart health surveys: A profile of cardiovascular risk. Survey methods and data analysis. Canadian Heart Health Surveys Research Group. CMAJ. 1992;146:1969–74. [PMC free article] [PubMed] [Google Scholar]
- 18.Grover SA, Dorais M, Paradis G, et al. Lipid screening to prevent coronary artery disease: A quantitative evaluation of evolving guidelines. CMAJ. 2000;163:1263–9. [PMC free article] [PubMed] [Google Scholar]
- 19.Perreault S, Dorais M, Coupal L, Paradis G, Joffres MR, Grover SA. Impact of treating hyperlipidemia or hypertension to reduce the risk of death from coronary artery disease. CMAJ. 1999;160:1449–55. (Erratum in 1999;161:21) [PMC free article] [PubMed] [Google Scholar]
- 20.Topol EJ, Lauer MS. The rudimentary phase of personalised medicine: Coronary risk scores. Lancet. 2003;362:1776–7. doi: 10.1016/S0140-6736(03)14941-0. [DOI] [PubMed] [Google Scholar]
- 21.Wang TJ, Massaro JM, Levy D, et al. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: The Framingham Heart Study. JAMA. 2003;290:1049–56. doi: 10.1001/jama.290.8.1049. [DOI] [PubMed] [Google Scholar]
- 22.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 23.Grover SA, Paquet S, Levinton C, Coupal L, Zowall H. Estimating the benefits of modifying risk factors of cardiovascular disease: A comparison of primary vs secondary prevention. Arch Intern Med. 1998;158:655–62. doi: 10.1001/archinte.158.6.655. (Erratum in 1998;158:1228) [DOI] [PubMed] [Google Scholar]
- 24.Conroy RM, Pyorala K, Fitzgerald AP, et al. SCORE project group. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 25.Stevens RJ, Kothari V, Adler AI, Stratton IM United Kingdom Prospective Diabetes Study (UKPDS) Group. The UKPDS risk engine: A model for the risk of coronary heart disease in Type II diabetes (UKPDS 56) Clin Sci (Lond) 2001;101:671–9. (Erratum in 2002;102:679) [PubMed] [Google Scholar]