1. Introduction
Sedentary behavior and physical activity (PA) are modifiable risk factors for a number of serious diseases and conditions, including cardiovascular disease, obesity, diabetes, and some cancer (U.S. Department of Health and Human Services, 1996). PA has also been shown to reduce symptoms, improve physical functioning and promote psychological well-being and increased quality of life for persons who have already developed chronic diseases or conditions (Mazzeo et al., 1998; Rejeski and Mihalko, 2001; Penninx et al., 2002; U.S. Department of Health and Human Services, 1996). Despite these established benefits of regular PA, the majority of U.S. adults does not engage in and maintain the recommended amount of PA (Centers for Disease Control, 2003). Specific subgroups such as lower socioeconomic status groups, older adults, and ethnic minorities are even less likely to engage in and maintain regular PA and therefore, are at greater risk for developing inactivity-related disease (Brownson et al., 2000).
Other groups at high risk for disease and disability related to inactivity are individuals with severe and persistent mental illness (SPMI) such as schizophrenia. Brown and colleagues (1999), found that fewer persons with schizophrenia engaged in any meaningful PA during a given week relative to persons of similar age and SES. Another study found that individuals with SPMI were less physically active compared to age-gender-race-matched individuals in the general population when assessed by self-report (Daumit et al., 2005). The reasons for reduced levels of regular physical activity in this group are multifaceted, and likely include aspects of the psychiatric disorders, side effects of medications, and lifestyle issues.
Insufficient energy expenditure through reduced PA and excessive sedentary behaviors in this population may further compound problems frequently observed in this group. Overweight and obesity were more prevalent in a community-based sample of persons with SPMI than in the general population (26% versus 18%) after accounting for age, race, and tobacco smoking behavior (Daumit et al., 2003). Moreover, antipsychotic medications have been shown to be associated with higher incidence of medical illnesses for which improvements in regular PA have demonstrated positive effects (Haupt and Kane, 2007). For example, atypical antipsychotics have been found to be associated with weight gain, glucose tolerance changes, and hyperlipidemia, which all are risk factors for diabetes and cardiovascular disease (Meyer and Nasrallah, 2003) and which all are amenable to intervention in part through regular PA.
Few studies have addressed accurately measuring PA or intervening to improve PA in persons with schizophrenia. Although weight control programs have been tested in this population, few experimentally evaluate PA interventions, and many only address diet and nutrition (McDevitt et al., 2005; Littrell et al., 2003; McCreadie et al., 2005; Evans et al., 2005; Menza et al., 2004). When PA is addressed, studies typically measure it using simple self-reports of time engaged in PA, usually walking (Vreeland et al., 2003). Recently, however, there have been a few reports assessing the reliability and validity of PA self-report measures in persons with SPMI. For example, Soundy and colleagues (2007) found high test-retest reliability (single-measure interclass coefficient (ICC)=.97) over a 4-week period for the 7-day recall measure (7-DR) (Blair, 1984) in a small group of individuals with SPMI (n=14). They also found adequate concurrent validity (Kendall’s tau=0.43) between the 7-DR and total energy expenditure as measured by accelerometry (Menza et al., 2004). Similarly, Dubbert and colleagues (2006) found evidence for acceptable test-retest reliability (ICC, r=.84) for expended energy on the Community Healthy Activities Model Program for Seniors (CHAMPS) (Stewart et al., 2001) in a relatively small sample of outpatient male veterans with SPMI and severe impairment of psychosocial functioning (n=20). They also found a modest, but not statistically significant, correlation between energy expended measured on the CHAMPS and accelerometry (Spearman’s rho =0.40). In a sample of persons with schizophrenia (n=35), Faulkner et al. (2006) assessed the reliability and validity of the International Physical Activity Questionnaire (Craig et al., 2003), a commonly used self-report PA measure in adults, and found adequate test-retest reliability (Spearman’s rho=.68) and concurrent validity of 0.37 between total minutes of PA assessed on the IPAQ and accelerometry.
These studies, however, have some limitations, including small sample size and heterogenous diagnostic groups. Moreover, instruments developed for the general population have several limitations when applied to PA assessment in predominantly sedentary adults, such as those with schizophrenia. Because inactive persons engage in less intensive activities more frequently than moderate or vigorous ones and perform them on a less regular basis, their recall of PA is less accurate (Harada et al., 2001). Furthermore, accurate recall requires intact working memory and executive functioning, both of which are commonly impaired in persons with schizophrenia. Self-report measures developed specifically for less active individuals, such as the Yale Physical Activity Scale (YPAS) (DiPietro et al., 1993) circumvent some of these problems by employing prompts and cued recall and also by inquiring about light activities and sedentary behavior.
Knowledge of how to measure the full range of PA and sedentary behavior in individuals with schizophrenia is essential if interventions to improve these behaviors are to be implemented and evaluated. The purpose of this study was three-fold: 1) To examine the level of physical activity in persons with schizophrenia relative to a non-psychiatric comparison group using both self-report and objective measures; 2) To establish the test-retest reliability of the YPAS in a sample of individuals with schizophrenia; 3) To assess the concurrent validity of the YPAS in this group by comparing it with objective data collected via accelerometry.
We hypothesized that the persons with schizophrenia spend less time engaged in PA than the comparison group as measured by both the YPAS and the accelerometer, that the YPAS would demonstrate high test-retest reliability, and that the YPAS would show concurrent validity with other subjective and objective measures of PA.
2. Method
2.1 Participants
Community dwelling men and women, age 40 or older, with a DSM-IV (American Psychiatric Association, 2000) diagnosis of schizophrenia or schizoaffective disorder and persons with no known psychiatric diagnosis were eligible to participate in this study. Individuals were excluded if they had a known diagnosis of dementia and/or were not able to give informed consent. All participants were ambulatory and had no known current, severe medical conditions. From a sample of 124 persons, who were involved in ongoing research at an academic research center (schizophrenia/schizoaffective, n=70; normal comparison, n=54), we selected a subset of individuals stratified by the absence or presence of actigraph data and matched on gender and age (± 10 years) in a 2:1 schizophrenia:comparison ratio. The data from a total of 81 participants (schizophrenia or schizoaffective disorder (n=54) and comparison group (n = 27)) were analyzed.
This study had approval from the appropriate institutional review boards, and all participants provided written informed consent prior to enrolling in the study.
2.2 Assessments
We obtained relevant demographic and clinical data by interview and medical record review, when appropriate. For the participants with schizophrenia, positive and negative symptoms of schizophrenia, as well as general psychopathology, were assessed with the Positive and Negative Syndrome Scale (PANSS) (Kay et al., 1987). Self-reported height and weight were colleted to determine Body Mass Index (BMI) for each individual. Physical activity was assessed using two self-report measures, the Yale Physical Activity Scale (DiPietro et al., 1993) and Stage of Motivational Readiness Scale (Marcus et al., 1992), and one objective indicator, accelerometry. Non-psychiatric comparisons completed the YPAS and interview, and a subsample participated accelerometry measurement.
2.2.1 Yale Physical Activity Scale
The YPAS is based on self-report and measures five activity dimensions (Vigorous Activity, Leisurely Walking, Moving on Feet, Standing, and Sitting) that occur in a typical week in the past month. Eight summary scores are calculated: Total time spent per week in all physical activities, weekly energy expenditure in kcal per week, five individual Indices for the activity dimensions, and a Total Activity Dimension Index. Indices are calculated from the frequency, duration and intensity of the activities.
2.2.2 Stage of Motivational Readiness Scale
We assessed PA motivational readiness with a five-item scale that classifies individuals into one of five stages of change that are based on intention and behavior--Precontemplation, Contemplation, Preparation, Action, and Maintenance (Marcus et al., 1992). Regular PA was defined according to the American College of Sports Medicine criteria: Any physical activity performed for 30 minutes per session for most days of the week (American College of Sports Medicine, 1990).
2.2.3 Accelerometer
For the objective measurement of PA, we used an Actigraph Accelerometer (model 7164) (formerly Computer Science and Applications (CSA)), a small (5.1 × 3.8 × 1.5 cm), lightweight (45 g), uni-axial accelerometer on a belt around the waist and records the occurrence and intensity of movement. The Actigraph has been shown to be valid for quantifying activity levels in laboratory and field settings (Nichols et al., 2000). Participants were asked to wear an accelerometer for seven days concurrent with the other assessments of physical activity. The Actigraph stored acceleration counts at 1-minute intervals. A monitored hour was not considered valid if the number of consecutive minutes of 0 counts exceeded 30 minutes. Acceleration counts were translated into minutes of light, moderate and vigorous physical activity using accepted cut points of 101, 1952, and 5725, respectively (Freedson et al., 1998). Daily hours of sedentary behavior were estimated by summing minutes with acceleration counts between 0 and 100 for valid hours of monitoring. Data from the monitors were considered valid if the monitor was worn for at least 3 of the 7 days and for at least 10 hours each day. A range of 3 to 7 days of monitoring has been found to give reliable estimates of physical activity (Trost et al., 2005).
2.3 Procedure
After giving informed consent, all participants were administered the YPAS and the Stages of Motivational Readiness Scale. A subset received the Actigraphs. The participants were seen for a second visit approximately one week later at which time the Actigraphs were returned and the YPAS and the Stages of Motivational Readiness Scale were administered a second time.
2.4 Data Analysis
All statistical tests were conducted using SPSS (Version 12.0) and were interpreted at the 0.05 two-tailed significance level, unless otherwise specified. Continuous variables were examined for normality and homogeneity of variance and transformed, if necessary, to meet these assumptions. Chi-square and analysis of variance (ANOVA) were conducted for comparisons between the two groups (psychiatric, non psychiatric) on categorical and continuous variables, respectively. Pearson correlations were calculated to assess test-retest reliability and the degree of association between YPAS scores and Actigraph variables. In order to have adequate cell size for the analysis by motivational stage of readiness, we collapsed PA stages of change from five to four (Cardinal and Sachs, 1996): Precontemplation, Contemplation, Preparation and Action/Maintenance.
3. Results
3.1 Demographic and Clinical Characteristics
The age of persons in the schizophrenia and comparison groups was generally in the early 50’s, and both groups were predominately Caucasian (See Table 1). Most of the schizophrenia sample lived in residential facilities, and approximately one-half had ever married. In contrast, all of the persons in the comparison group lived independently, and about 78% had ever married. As expected, the comparison group had more years of education than the schizophrenia group. In the schizophrenia group, the mean PANSS Positive subscale score was 12.5 (s.d. = 6.0), the average Negative subscale score was 14.3 (s.d.=4.5), and the mean General Psychopathology score was 27.0 (s.d.=7.3). All PANSS scores fell in the 10th percentile (low range), which is typical of community-dwelling persons with schizophrenia who are psychiatrically stable (Kay et al., 1988).
Table 1.
Comparison of demographic and clinical variables in persons with and without schizophrenia.
| Schizophrenia N=54 Mean (SD) or % |
Comparison N=27 Mean (SD) or % |
Chi-square or F-value | p-value | |
|---|---|---|---|---|
| Age (years) |
50.7 (6.4) |
52.2 (8.6) |
.727 |
.396 |
| Ethnicity (%Cauc.) |
81.5 |
66.7 |
2.20 |
.138 |
| Gender (%male) |
59.3 |
59.3 |
.000 |
1.00 |
| Education (years) |
11.9 (1.5) |
13.5 (1.6) |
19.87 |
.000 |
| Living Situation (% Independ.) (% Assisted) |
7.4 92.6 |
100 0 |
-- |
-- |
| Marital Status (% Ever Married) |
51.9 |
77.8 |
5.063 |
.021 |
| Body Mass Index | 30.5 (7.1) | 27.8 (4.4) | 2.40 | .127 |
3.2 Physical Activity Measures
3.2.1 Yale Physical Activity Scale
Table 2 shows the scores on the YPAS and the accelerometry variables for both groups. For the schizophrenia group, the mean number of hours per week spent doing any physical activity, including low-intensity activities and chores, was less than half of that of the comparison group, and consequently, so was the total estimated energy expenditure.
Table 2.
Means and standard deviations on the YPAS and accelerometry between persons with and without schizophrenia.
| Schizophrenia (n=54) |
Comparison (n=27) |
F-value | p-value | |
|---|---|---|---|---|
| YPAS | ||||
| Time+ (hr/wk) | 11.2 (11.8) | 32.5 (27.5) | 36.00 | .001 |
| Energy + (kcal/wk) | 3174.2 (5072.9) | 7968.6 (6886.3) | 29.70 | .001 |
| Vigorous Activity Index+ | 10.2 (15.4) | 22.4 (20.4) | 10.76 | .002 |
| Leisurely Walking Index+ | 11.9 (11.1) | 17.2 (14.2) | 1.43 | .235 |
| Moving Index | 6.2 (4.3) | 9.1 (3.6) | 9.59 | .003 |
| Standing Index+ | 3.0 (2.4) | 5.3 (2.9) | 11.75 | .001 |
| Sitting Index | 2.5 (1.0) | 2.3 (.86) | 1.28 | .261 |
| Total Activity Index | 34.2 (22.4) | 56.2 (28.2) | 14.58 | .001 |
| Accelerometry | (n=16) | (n=6) | ||
| Counts minute during wear time | 337.7 (240.5) | 365.3 (117.2) | .070 | .795 |
| Ave. Sedentary (hours/day) | 8.9 (2.9) | 8.2 (1.3) | .347 | .563 |
| Ave. Light activity (hours/day) | 4.0 (1.0) | 5.4 (1.0) | 7.44 | .013 |
| Ave. Moderate (minutes/day) | 32.0 (28.3) | 31.6 (19.2) | .001 | .975 |
| Ave. Vigorous+ (minutes/day) | 4.1 (8.3) | 5.4 (8.4) | .140 | .712 |
log transformed
When examining the YPAS Indices for the activity domains, as well as the Total Activity Index, we found a number of differences between the groups. The schizophrenia group had lower scores on the Vigorous Activity, Moving on Feet, and Standing Indices than the comparison group, whereas the groups scored similarly on the Sitting Index. The schizophrenia group reported lower scores on the Leisurely Walking Index, but it was not significant.
3.2.2 Accelerometry
A total of 54 participants received Actigraph monitors; however due to monitor malfunctions and too little data (less than 3 days of records), data from 17 participants were not included in analyses. Of the 37 participants (schizophrenia n=17; comparison n=20) with valid accelerometer data (3–7 days of at least 10 hours per day), a total of 22 were selected for analysis based on matching for gender and age. There were 16 persons in the schizophrenia group; six in the comparison group.
There were no differences between the two groups on the mean number of days the monitor was worn (6.1, s.d. = 1.2), the mean total number of valid hours of monitoring (90.3, s.d.= 32.4), or the accelerometer counts per minute during wear time (346.4, s.d. = 206.4).
The accelerometers indicated the schizophrenia group had lower light activity hours per day relative to the comparison group. Average daily minutes of moderate or vigorous PA did not differ between the groups, nor did the number of sedentary hours per day or mean activity counts.
3.2.3 Physical Activity Motivation Readiness
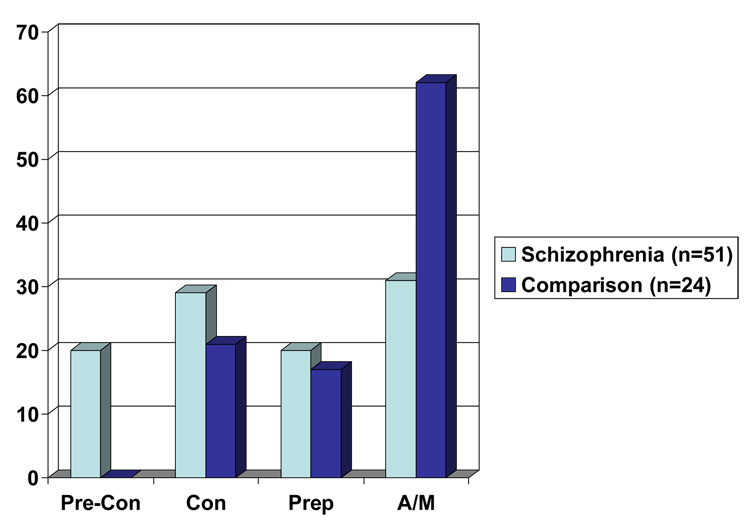
Similar to group differences found on the YPAS, we found significant differences between those with and without schizophrenia on the assessment of PA motivational readiness, as seen in Figure 1. About 62% of the non-psychiatric comparison group was classified as in the Active/Maintenance group compared to just over 30% of those in the schizophrenia group. Conversely, none of the comparison group participants were classified as “Precontemplation”, whereas 20% of those in the schizophrenia group were.
Figure 1.
Percentages of persons with and without schizophrenia as a function of stage of motivational readiness.
3.3 YPAS Test-Retest Reliability
Test-retest reliability coefficients were significant for five of the eight YPAS scores for the normal comparison group (r’s .64–.90) while the correlation coefficient for the Sitting Index was only .29 (See Table 3). The correlation coefficients for the Moving and Standing Indices were in the adequate range for the comparison group, but failed to reach significance because of the lack of power due to the small sample size. For the schizophrenia group, three of the eight YPAS scores had significant reliability coefficients ranging from .40–.62. For all YPAS scores test-rest reliability was lower for the schizophrenia group compared to the comparison group.
Table 3.
Pearson correlation coefficients for the one-week test-retest reliability of YPAS in persons with and without schizophrenia.
| Schizophrenia N=19 | Comparison N=10 | |
|---|---|---|
| Time+ (hr/wk) | .62** | .90** |
| Energy+ (kcal/wk) | .60** | .91** |
| Vigorous Activity Index | .40** | .69** |
| Leisurely Walking Index | .04 | .95** |
| Moving Index | .10 | .60 |
| Standing Index | .34 | .58 |
| Sitting Index | .36 | .29 |
| Total Activity Index | .36 | .64* |
log transformed
p<.05;
p<.01
3.4 Concurrent Validity
We examined concurrent validity in two ways: 1) by examining the relationship between YPAS and accelerometry scores for both groups, and 2) by examining YPAS as a function of motivational readiness. Pearson’s correlation coefficients indicated no significant relationships between YPAS Vigorous Index scores and the average daily minutes of vigorous activity as measured by accelerometry for either the schizophrenia or the comparison groups. When we examined the relationship of YPAS Vigorous and Leisurely Index scores to average daily minutes of moderate activity as measured by accelerometry, we did not find significant relationships between Leisurely Index scores and accelerometry for either group. A significant relationship for only the normal comparison group was found between the YPAS Moving Index scores and the average daily minutes of light activity as measured by accelerometry (r=.930, p<.007). Finally, no relationship for either group was found between Standing and Sitting Indices of the YPAS and average minutes of sedentary activity measured by accelerometry.
When we examined the YPAS measures as a function of motivational readiness within the schizophrenia group, we observed several differences (Table 4). Those individuals categorized as in the combined “Active/Maintenance” group reported on the YPAS spending more time per week being physically active and consequently, expended more energy, as well as having higher Total Activity Indices. The Scores on the Vigorous Activity and Moving on Feet Indices were also higher for the “Active/Maintenance” group but only reached a trend level of significance. We found no differences on any of the demographic variables or BMI among the four-stage classification within the schizophrenia group.
Table 4.
Means and standard deviations of YPAS scores in middle-aged and older adults with schizophrenia as a function of stage of motivational readiness.
| Precon | Con | Prep | Act/Main | F-value | p-value | |
|---|---|---|---|---|---|---|
| Time+ | 5.1 (2.3) |
7.0 (5.8) |
10.8 (5.6) |
16.9 (14.1) |
5.87 | .002 |
| Energy+ | 1245.3 (689.0) |
1349.7 (1063.3) |
5365.3 (9219.8) |
4098.2 (4049.9) |
5.86 | .002 |
| Vigorous+ | 9.5 (19.2) |
4.0 (6.3) |
8.5 (6.7) |
18.1 (21.0) |
2.29 | .091 |
| Leisurely+ | 8.0 (6.0) |
11.2 (13.2) |
11.6 (5.8) |
16.5 (13.3) |
.518 | .672 |
| Moving | 5.1 (4.3) |
4.5 (3.0) |
6.6 (3.7) |
8.3 (5.0) |
2.38 | .081 |
| Standing | 3.0 (2.9) |
2.1 (1.2) |
3.8 (2.4) |
3.4 (3.1) |
1.10 | .359 |
| Sitting | 2.7 (1.1) |
2.3 (1.2) |
2.5 (0.7) |
2.7 (1.1) |
.420 | .739 |
| Total | 28.3 (23.3) |
24.1 (15.4) |
33.0 (13.4) |
51.9 (25.3) |
5.84 | .002 |
PreCon = Precontemplation; Con =Contemplation; Prep = Preparation; Act/Main=Action and Maintenance
log-transformed
4. Discussion
We found that persons with schizophrenia spent less than half the time engaged in PA and expended less than half of the kilocalories per week relative to a non-psychiatric comparison group as measured by the Yale Physical Activity Scale, a self-report measure of PA. No group differences, however, were seen using accelerometry, an objective measure of PA. Test-retest reliability for the YPAS was comparable between the schizophrenia and comparison groups for summary measures, such as Time, Energy, and Total Activity Index. On the other YPAS Indices, however, the comparison group demonstrated adequate test-retest reliability, while the schizophrenia group did not. Concurrent validity for the YPAS was found with other self-report, but not objective, measures of physical activity in persons with schizophrenia.
Our results are consistent with the reports of reduced PA in persons with schizophrenia or other SMPI compared to the general population (Daumit et al., 2005). The average total amount of energy expended per week by schizophrenia group as measured by the YALE in our study (3174.2, s.d.= 5072.9) was similar to the kilocalories per week reported by the CHAMPS (2710.6, s.d.= 2092.6 at time 2) (Dubbert et al., 2006) and by the 7-D PAR (3020.2, s.d.= 890.6) (Soundy et al., 2007).
The amount of PA reported by the comparison group in this study was similar to that found by DiPietrio and colleagues (1993) in their initial investigation of the YPAS. They found that healthy older adults (mean age 71 years) participated in about 34 hours per week and had a mean energy expenditure of 7613 kilocalories per week doing any physical activity. The comparison group also scored similarly to DiPietio’s normative group on the YPAS Indices.
We found no differences between persons with schizophrenia and the comparison group on dimensions of PA using accelerometry, despite the group differences on the YPAS Total Time, Total Energy, and Total Activity Index, as well as most of the other activity dimension Indices. As measured by accelerometry, both groups spent as much time engaged in moderate and vigorous activity per day as a sample of younger adults (mean age about 30) but more than a group of older persons (mean age about 76) (Davis and Fox, 2006), which is expected given the average age in our sample is in the early 50’s. Given the small sample size, it is possible that our schizophrenia group may not be representative; those that wore the actigraphs may have been more active than those who refused. Moreover, the lack of a significant correlation between the YPAS Vigorous Index and the amount of time engaged in vigorous activity as measured by accelerometry may have been influenced by the restricted range of values in the sample.
Our findings are not consistent with the results of the study by Faulkner and colleagues (2006) who found a significant, albeit modest, relationship (Spearman’s rho = 0.37) between the International Physical Activity Questionnaire (IPAQ), self-report PA measure and accelerometry on number of minutes of PA per week. The IPAQ, however, only assesses moderate and vigorous PA. It may be possible that YPAS is more likely to capture light activity than the accelerometer, and persons with schizophrenia are engaging is less light activity than the comparison group. Some researchers (Levine et al., 2006) have suggested that light activity may be a major contributor to total energy expenditure and relate to overweight. It is also important to note that accelerometry data were collected on a subsample of the schizophrenia and comparison group in this study. Future work should include a larger accelerometry sample to better understand the relationship between the YPAS and objective measures like accelerometry.
We found the YPAS demonstrated test-retest reliability for the Total Time, Total Energy, and Total Activity Index for both groups; however, the YPAS was reliable for the other activity dimension Indices for only the comparison group. This is important in that the Total Time, Total Energy, and Total Activity Indices were found to be the most stable of all Indices for the scale development sample (DiPietro et al., 1993).
Results from this study provide preliminary evidence of the reliability and validity of the YPAS for persons with schizophrenia. Because there is reason to believe that use of the IPAQ has potential limitations in individuals with schizophrenia (i.e., only inquires about moderate activity rather than light and sedentary activities which are more appropriate for people with schizophrenia), instruments, such as the YPAS or the CHAMPS, developed for use in older sedentary populations that inquire about specific behaviors (e.g., mopping, vacuuming) across a range of PA, as well as sedentary behavior provide an alternative to the IPAQ.
This study has several limitations, including a small sample size, no anthropometric or physiologic data, a small subsample of accelerometry data, the control group may have been less active than the general population, and inherent limitations of the YPAS for patients with schizophrenia (i.e., some activities, such as time spent gardening, may be less appropriate for patients with schizophrenia living in a residential facility).
Methods of assessing physical activity in behavioral research in the general population, while improving, are still suboptimal. The field is moving from reliance on self-report to incorporate more objective measures such as accelerometers and heart rate monitors. Because of practical and cost-related issues self-report measures will continue to be used, but increasingly these will be instruments that have been validated by concurrent objective assessments. Measuring PA of people with schizophrenia, in whom cognitive impairment and the social and functional limitations are common, poses many challenges. Thus, use of the YPAS in this population should be augmented with other more valid measures of PA.
Acknowledgments
This work was supported in part by the National Institute of Mental Health grants MH66248, MH071539, MH71544, and MH063139. We would also like to thank Dilip Jeste, Director, Geriatric Psychiatry Advanced Center for Innovative Services and Interventions Research, for infrastructure support for recruitment and data collection.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American College of Sports Medicine. Position stand on the recommended quantity and quality for exercise for developing and maintaining cardiorespiratory and muscular fitness in healthy adults. Med.Sci.Sports Exerc. 1990;22:265–274. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Blair SN. How to assess exercise habits and physical fitness. In: Matarazzo JD, Miller NE, Weiss SM, editors. Behavioral health: A handbook of health enhancement and disease prevention. New York: John Wiley & Sons; 1984. pp. 427–447. [Google Scholar]
- Brown S, Birtwistle J, Roe L, Thompson C. The unhealthy lifestyle of people with schizophrenia. Psychol Med. 1999;29:697–701. doi: 10.1017/s0033291798008186. [DOI] [PubMed] [Google Scholar]
- Brownson RC, Jones DA, Pratt M, Blanton C, Heath GW. Measuring physical activity with the behavioral risk factor surveillance system. Med Sci Sports Exerc. 2000;32:1913–1918. doi: 10.1097/00005768-200011000-00015. [DOI] [PubMed] [Google Scholar]
- Cardinal BJ, Sachs ML. Effects of mail-mediated, stage-matched exercise behavior change strategies on female adults' leisure-time exercise behavior. J.Sports Med.Phys.Fitness. 1996;36:100–107. [PubMed] [Google Scholar]
- Centers for Disease Control. Prevalence of physical activity, including lifestyle activities among adults - United States, 2000–2001. MMWR. 2003;52:768. [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Daumit GL, Crum RM, Guallar E, Powe NR, Primm AB, Steinwachs DM, Ford DE. Outpatient prescriptions for atypical antipsychotics for African Americans, Hispanics, and whites in the United States. Arch Gen Psychiatry. 2003;60:121–128. doi: 10.1001/archpsyc.60.2.121. [DOI] [PubMed] [Google Scholar]
- Daumit GL, Goldberg RW, Anthony C, Dickerson F, Brown CH, Kreyenbuhl J, Wohlheiter K, Dixon LB. Physical activity patterns in adults with severe mental illness. J.Nerv.Ment.Dis. 2005;193:641–646. doi: 10.1097/01.nmd.0000180737.85895.60. [DOI] [PubMed] [Google Scholar]
- Davis MG, Fox KR. Physical activity patterns assessed by accelerometry in older people. Eur J Appl Physiol. 2006 Oct 25; doi: 10.1007/s00421-006-0320-8. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- DiPietro L, Caspersen CJ, Ostfeld AM, Nadel ER. A survey for assessing physical activity among older adults. Med.Sci.Sports Exerc. 1993;25:628–642. [PubMed] [Google Scholar]
- Dubbert PM, White JD, Grothe KB, O'Jile J, Kirchner KA. Physical activity in patients who are severely mentally ill: Feasibility of assessment for clinical and research applications. Arch Psychitr Nurs. 2006;20:205–209. doi: 10.1016/j.apnu.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Evans S, Newton R, Higgins S. Nutritional intervention to prevent weight gain in patients commenced on olanzapine: a randomized controlled trial. Aust N Z J Psychiatry. 2005;39:479–486. doi: 10.1080/j.1440-1614.2005.01607.x. [DOI] [PubMed] [Google Scholar]
- Faulkner G, Cohn T, Remington G. Validation of a physical activity assessment tool for individuals with schizophrenia. Schizophr Res. 2006;82:225–231. doi: 10.1016/j.schres.2005.10.020. [DOI] [PubMed] [Google Scholar]
- Freedson PS, Melanson E, Sirad J. Calibration of the Computer Science and Applications, Inc. accelerometer. Res Q Exerc Sport. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- Harada ND, Chiu V, King AC, Stewart AL. An evaluation of three self-report physical activity instruments for older adults. Med.Sci.Sports Exerc. 2001;33:962–970. doi: 10.1097/00005768-200106000-00016. [DOI] [PubMed] [Google Scholar]
- Haupt DW, Kane JM. Metabolic risks and effects of atypical antipsychotic treatment. J Clin Psychiatry. 2007;68:e24. doi: 10.4088/jcp.1007e24. [DOI] [PubMed] [Google Scholar]
- Kay S, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kay SR, Opler LA, Lindenmayer JP. Reliability and validity of the positive and negative syndrome scale for schizophrenics. Psychiatry Res. 1988;23:99–110. doi: 10.1016/0165-1781(88)90038-8. [DOI] [PubMed] [Google Scholar]
- Levine JA, VanderWeg MW, Hill JO, Kleges RC. Non-exercise activity thermogenesis: The crouching tiger hidden dragon of societal weight gain. Areteriosler Thromb Vasc. 2006;26:729–736. doi: 10.1161/01.ATV.0000205848.83210.73. [DOI] [PubMed] [Google Scholar]
- Littrell KH, Hilligoss NM, Kirshner CD, Petty RG, Johnson CG. The effects of an educational intervention on antipsychotic-induced weight gain. Journal of Nursing Scholarship. 2003;35:237–241. doi: 10.1111/j.1547-5069.2003.00237.x. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Banspach SW, Lefebvre RC, Rossi JS, Carleton RA, Abrams DB. Using the stages of change model to increase the adoption of physical activity among community participants. Am J Health Promot. 1992;6:424–429. doi: 10.4278/0890-1171-6.6.424. [DOI] [PubMed] [Google Scholar]
- Mazzeo RS, Cavanagh P, Evans WJ, Fiatarone M, Hagberg J, McAuley E, Startzell J. ACSM position stand: Exercise and physical activity for older adults. Med.Sci.Sports Exerc. 1998;30:992–1008. [PubMed] [Google Scholar]
- McCreadie RG, Kelly C, Connolly M, Williams S, Baxter G, Lean M, Paterson JR. Dietary improvement in people with schizophrenia: randomized controlled trial. Br J Psychiatry. 2005;187:346–351. doi: 10.1192/bjp.187.4.346. [DOI] [PubMed] [Google Scholar]
- McDevitt J, Wilbur J, Kogan J, Briller J. A walking program for outpatients in psychiatric rehabilitation: A pilot study. Biol Res Nurs. 2005;7:87–97. doi: 10.1177/1099800405278116. [DOI] [PubMed] [Google Scholar]
- Menza M, Vreeland B, Minsky S, Gara M, Radler DR, Sakowitz M. Managing atypical antipsychotic-associated weight gain: 12-month data on a multimodal weight control program. J Clin Psychiatry. 2004;65:471–477. [PubMed] [Google Scholar]
- Meyer JM, Nasrallah HA. Issues surrounding medical care for individuals with schizophrenia: The challenge of dual neglect by patients and the system. In: Meyer JM, Nasrallah HA, editors. Medical Illness and Schizophrenia. Washington, DC,: American Psychiatric Publishing; 2003. [Google Scholar]
- Nichols JF, Morgan CG, Chabot LE, Sallis JF, Calfas KJ. Assessment of physical activity with the Computer Science and Applications, Inc. accelerometer: laboratory versus field validation. Res Q Exerc Sport. 2000;71:36–43. doi: 10.1080/02701367.2000.10608878. [DOI] [PubMed] [Google Scholar]
- Penninx BW, Rejeski J, Pandya J, Miller ME, Di Bari M, Applegate WB, Pahor M. Exercise and depressive symptoms: A comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. Journal of Gerontology: Psychological Sciences. 2002;57B:P124–P132. doi: 10.1093/geronb/57.2.p124. [DOI] [PubMed] [Google Scholar]
- Rejeski WJ, Mihalko SL. Physical activity and quality of life in older adults. J Gerontol A Biol Sci Med Sci. 2001;56:23–35. doi: 10.1093/gerona/56.suppl_2.23. [DOI] [PubMed] [Google Scholar]
- Soundy A, Taylor A, Faulkner G, Rowlands A. Psychometric properties of the 7-Day Physical Activity Recall Questionnaire in individuals with severe mental illness. Archives of Psychatric Nursing. 2007;21:309–316. doi: 10.1016/j.apnu.2007.03.001. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS questionnaire for older adults: Outcomes for interventions. Med.Sci.Sports Exerc. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- Trost SG, Mclver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37:S531–S543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General Executive Summary. Atlanta, GA: U.S. Department of Health and Human Services, Center for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. [Google Scholar]
- Vreeland B, Minsky S, Menza M, et al. A program for managing weight gain associated with atypical antipsychotics. Psychiatr Serv. 2003;54:1155–1157. doi: 10.1176/appi.ps.54.8.1155. [DOI] [PubMed] [Google Scholar]