Abstract
Immunotherapeutic strategies to combat neurodegenerative disorders have galvanized the scientific community since the first dramatic successes in mouse models recreating aspects of Alzheimer disease (AD) were reported. However, initial human trials of active amyloid-beta (Aβ) vaccination were halted early because of a serious safety issue: meningoencephalitis in 6% of subjects. Nonetheless, some encouraging preliminary data were obtained, and rapid progress has been made toward developing alternative, possibly safer active and passive immunotherapeutic approaches for several neurodegenerative conditions. Many of these are currently in human trials for AD. Despite these advances, our understanding of the essential mechanisms underlying the effects seen in preclinical models and human subjects is still incomplete. Antibody-induced phagocytosis of pathological protein deposits, direct antibody-mediated disruption of aggregates, neutralization of toxic soluble proteins, a shift in equilibrium toward efflux of specific proteins from the brain, cell-mediated immune responses, and other mechanisms may all play roles depending on the specific immunotherapeutic scenario.
Keywords: Alzheimer disease, vaccination, monoclonal antibody
INTRODUCTION
The remarkable power of therapeutics designed to enhance aspects of the immune response has been recognized at least since the time of Jenner (1798). Triumph after triumph has come from the realm of infectious diseases since then. More recently, the basic strategies of active vaccination, and by extension, the use of monoclonal antibodies for passive vaccination, have been applied to neoplastic, autoimmune, and atherosclerotic diseases. Considering that the number of individuals greater than age 65 is increasing markedly throughout the world, it is quite natural that the modern immunotherapeutic armamentarium should be brought to bear on the problems of Alzheimer disease (AD) and other neurodegenerative disorders. Hundreds of previous reviews have been published on the topic of immunotherapeutics in neurodegenerative diseases.1 The pathogenesis of these diseases has also been reviewed extensively (e.g., Skovronsky et al. 2006). Here we address selected critical issues that bear directly on the development of effective active and passive immunotherapeutics for human patients with neurodegenerative disorders.
ACTIVE Aβ VACCINATION IN TRANSGENIC MICE MODELING ASPECTS OF AD PATHOLOGY: INITIAL FINDINGS
The first report of an immunotherapeutic approach to a neurodegenerative disease in vivo was published in 1999. The experiments involved active vaccination with aggregated amyloid-beta (Aβ) in PDAPP mice, transgenic animals that develop extracellular Aβ deposition in the form of plaques similar in many respects to those seen in human AD patients (Games et al. 1995, Johnson-Wood et al. 1997). The initial results were dramatic: Immunization starting either before or after plaque deposition had a clear beneficial effect on the AD-like plaque pathology (Figure 1a). High anti-Aβ antibody titers in serum were detected, and phagocytic cells were found engulfing Aβ aggregates in vaccinated animals' brains (Schenk et al. 1999). Quickly thereafter, two groups simultaneously published independent reports showing improvements in behavioral abnormalities using similarly vaccinated amyloid precursor protein (APP) transgenic mice (Figure 1b–c ; see Supplemental Table 1. Follow the Supplemental Material link from the Annual Reviews home page at http://www.annualreviews.org). Strikingly, behavioral performance was even more strongly improved than were brain Aβ levels or plaque pathology; some performance deficits in TgCRND8 (Chishti et al. 2001) and Tg2576 (Hsiao et al. 1996) mice were almost entirely normalized, whereas Aβ plaques were reduced but not eliminated (Janus et al. 2000, Morgan et al. 2000).
Figure 1.

Effects of active vaccination in transgenic mice modeling aspects of Alzheimer disease. (a) Reduction in Aβ plaque deposition in the cortex of PDAPP mice following vaccination with aggregated Aβ1–42 (right) compared with saline-injected mice (left) at the same age. Adapted from figure 4b,c of Schenk et al. (1999). (b) Improved behavioral performance in TgCRND8 mice following vaccination with aggregated Aβ1–42 (red circles, right panel) compared with TgCRND8 mice vaccinated with the irrelevant islet-associated polypeptide (IAPP, red circles, left panel). Performance of similarly vaccinated nontransgenic mice (gray circles) was mostly unchanged. The figure shows latency to reach the hidden platform in the Morris water maze (Morris et al. 1984); each daily session consisted of four trials per mouse. Adapted from figure 2e of Janus et al. (2000). (c) Improved behavioral performance in Tg2576 mice following vaccination with aggregated Aβ1–42 (purple triangles) compared with Tg2576 mice vaccinated with the irrelevant keyhole limpet hemocyanin (blue squares). Aβ-vaccinated Tg2576 mice performed nearly as well as nontransgenic mice (green circles). The figure shows number of errors in the radial arm water maze during working memory (trials 1–4) and retention (trial 5) testing on days 10 and 11 of training. Adapted from figure 1b of Morgan et al. (2000). Reprinted by permission of Macmillan Publishers Ltd.
THE AN1792 TRIALS OF ACTIVE Aβ VACCINATION IN HUMAN AD PATIENTS
This approach was translated remarkably rapidly to the human clinical arena. A phase I (safety) study in patients with mild-moderate sporadic AD was performed in the year 2000. Eighty subjects, in their 70s on average, were randomly assigned to one of four combinations of AN1792 (the same aggregated Aβ1–42 preparation used in the transgenic mice) plus the QS21 surface active saponin adjuvant or placebo. Four vaccinations over a six-month period were administered intramuscularly. Four deaths occurred in the active treatment group but none was considered related to the vaccination. Other adverse events possibly related to vaccination included confusion and hallucinations, hostility, and convulsions, but all of these have been reported to occur also in untreated AD patients (Bayer et al. 2005). Overall the treatment was well tolerated during this trial, and the strategy was advanced to a phase II trial.
After the phase II trial was well underway, one actively vaccinated patient from the phase I trial developed a subacute encephalopathy, did not recover to baseline, and died from non-CNS causes. At autopsy, the patient was found to have T-lymphocyte predominant meningoencephalitis (Nicoll et al. 2003). Meningoencephalitis is not an expected occurrence in AD and has not been reported in any unvaccinated AD patients to our knowledge, although investigators have reported perivascular inflammation in some cases of cerebral amyloid angiopathy with Aβ deposition in brain blood vessels (Eng et al. 2004). This event occurred after the vaccine formulation was changed to include the preservative polysorbate 80. At around the same time, another report showed similar encephalitis in 6% (18/300) of the actively immunized patients in the phase II study, which also used the polysorbate 80-containing formulation (Orgogozo et al. 2003). The phase II study was then terminated after only 1-3 of the planned 6 vaccinations had been given. Twelve of the patients recovered within weeks, whereas six patients suffered disabling cognitive or neurological sequelae. Analysis of the interrupted trial revealed that Aβ antibody titer was not correlated with the signs and symptoms of meningoencephalitis. These adverse events had not been predicted on the basis of the preclinical studies performed prior to initiation of the clinical trials.
- Active vaccination
introducing an exogenous substance to stimulate the immune system to mount a response
- Passive Vaccination
introducing exogenous antibodies directly into an animal or person to produce a benefit similar to that of active vaccination
- AD
Alzheimer disease
- Amyloid-beta (Aβ)
a 38-43 amino acid peptide derived by proteolytic cleavage of the amyloid precursor protein
- PDAPP mice
transgenic line overexpressing a human amyloid precursor protein mutant (V717F) linked to one form of familial, autosomal dominant AD
- APP
amyloid precursor protein
- TgCRND8 mice
transgenic line overexpressing human amyloid precursor protein with two mutations, double mutant K670N/M671L and the V717F driven by a prion promoter
- Tg2576 mice
transgenic line overexpressing a human amyloid precursor protein double mutant (K670N/M671L) linked to another form of familial, autosomal dominant AD
In the phase I study, there was a trend toward slower cognitive decline in the actively vaccinated patients compared with controls. However, active vaccination did not bring the cognitive performance of these elderly, demented individuals back to near normal, as had been reported for some of the transgenic mice. One possible explanation was that in the phase I trial, serum anti-Aβ antibody titers were low, above 1:1000 in only ∼60% of the elderly human AD patients, whereas most of the relatively young mice in the early preclinical vaccination trials had titers over 1:10,000 (Schenk et al., 1999). Of note, in a preclinical study of significantly older transgenic mice, Austin et al. (2003) found lower antibody titers following active vaccination, and they saw no effect on behavioral performance. Another study found that immunization in older mice was less effective at clearing plaques than was immunization in younger mice, even though all ages produced high anti-Aβ antibody titers (Das et al. 2001).
Overall in the multicenter phase II study, there likewise was not a major effect on cognitive performance (Gilman et al. 2005). A single-center analysis of a subgroup of 30 patients appeared to indicate stabilization on some measures of cognitive status in 6 patients with robust antibody responses (Hock et al. 2003). However, the 9 patients who received active vaccination but did not mount a significant antibody response actually performed worse than would have been expected from the natural history of the disease; their mini-mental status exam scores declined by an average of 6 points out of 30 in 1 year (Hock et al. 2003), whereas the overall placebo group declined by an average of 1.5 points (Gilman et al. 2005). In the phase II study analysis, ∼20% of the patients had significant serum antibody titers (>1:2200) after 1-3 vaccinations. Even among this subgroup of patients who were considered responders, the primary clinical outcome measures, including the mini-mental status examination, revealed no effect of active vaccination compared with placebo. A few of the tests in the neuropsychological battery relating to episodic memory showed differences favoring active vaccination, although the study found no dramatic cognitive improvement in any domain examined. Of note, analyses excluding the 22% of the responders who developed encephalitis did not change the reported results.
Importantly, active immunization resulted in generation of anti-Aβ antibodies that appeared predominantly directed against the N-terminus of Aβ and bound to both soluble and insoluble forms of Aβ (Lee et al. 2005). These antibodies were similar in many respects to those raised during active vaccination of transgenic mice (Bard et al. 2003).
Neuropathological analysis of the brains of a few deceased patients revealed several striking findings suggesting that the vaccination strategy was in fact having some effect on human AD pathology. The first patient to come to autopsy from the phase I study had a patchy distribution of cortical Aβ plaques, in contrast with the more uniform distribution of plaques in several cortical regions in typical AD (Nicoll et al. 2003). Some regions of cortex were nearly free of plaques. Plaque pathology was extensive in the basal ganglia and cerebellum, which are areas not especially prone to plaque pathology. Cerebral amyloid angiopathy and neurofibrillary tangles were persistent, even in areas relatively free of parenchymal Aβ plaques. Although this patient may have had an unusual form of the disease (Klunk et al. 2007), a more likely explanation is that the vaccination-induced immune response caused a clearance of Aβ deposits out of cortex, possibly resulting in a redistribution into other structures. As seen in vaccinated transgenic mice, the brain contained apparent phagocytic cells with closely associated punctate Aβ staining (Nicoll et al. 2003).
A second case report from a vaccination-related meningoencephalitis patient revealed similar findings, with the addition of multi-nucleated giant cells appearing to engulf Aβ deposits (Ferrer et al. 2004). Tris and guanidine-soluble Aβ levels in extracts from these brains were higher than in several unvaccinated patients (Patton et al. 2006). In the brain of a third patient who, importantly, did not develop clinical signs of meningoencephalitis (he died of unrelated causes 18 months after his first vaccination), there was still a marked reduction in Aβ plaque pathology in some regions of cortex as compared with typical AD patients. Cerebral amyloid angiopathy and tangle pathology were again persistent. This patient mounted a vigorous anti-Aβ antibody response, based on his serum anti-Aβ antibody titers. No evidence of multinucleated giant cells or subclinical T-cell meningoencephalitis was found (Masliah et al. 2005a).
An unresolved question exists about the nature of the effects of vaccination on AD pathology in the vast majority of patients who survived. Cerebrospinal fluid studies revealed decreases in tau levels in a subset of patients (Gilman et al. 2005). This decrease may suggest reduced neurodegeneration, but the interpretation of this finding is not clear. Amyloid imaging was not available at that time but could have been helpful. A volumetric MRI study over a one-year period somewhat surprisingly revealed that vaccinated patients had a greater decrease in brain volume than did placebo patients. When patients with encephalitis were excluded, the results remained significant. A moderate correlation between anti-Aβ antibody titer and volume loss was found; higher maximum IgG titers were associated with greater volume loss (Fox et al. 2005). What accounts for these MRI findings is again not clear. Acceleration of volume loss has been associated with progression to later clinical stages of AD, but there was no evidence of accelerated neurodegeneration in the vaccinated patients. More interestingly, if Aβ deposits take up a substantial portion of the substance of the cortex in AD, removal of these deposits could account for the reported volume loss.
- Morris Water Maze
rodent behavioral test that assesses spatial learning and memory by evaluating ability to swim to a small platform in a pool of opacified water
PASSIVE Aβ VACCINATION IN TRANSGENIC MICE MODELING ASPECTS OF AD PATHOLOGY
Shortly after the publication of the initial preclinical active vaccination trial, two reports indicated that passive vaccination by systemic infusion of monoclonal antibodies directed at Aβ could similarly decrease Aβ plaque pathology in transgenic mice (Bard et al. 2000, DeMattos et al. 2001) (see also Supplemental Table 2). Passive vaccination strategies also successfully improved the behavioral performance of these transgenic animals. However, effects on plaque pathology were dissociated from effects on behavior. For example, six weekly injections of m266, the antibody to the central domain of Aβ used by DeMattos et al., produced marked normalization of certain behavioral impairments without any apparent effects on plaque pathology. Even a single injection of this antibody produced beneficial effects that were apparent one day after treatment (Dodart et al. 2002). Likewise, three injections of BAM-10, another monoclonal antibody, rapidly improved Morris water maze performance in another transgenic mouse model without apparently affecting levels of any of the soluble species of Aβ measured by enzyme-linked immunosorbent assay (ELISA) in brain extracts. These mice had not yet developed plaques but already had worse behavioral performance than did their wild-type littermates (Kotilinek et al. 2002). Janus et al. (2000) had similarly demonstrated that active vaccination starting before the development of plaque pathology improved behavior without reduction in brain Aβ levels.
These reports and others that followed (Hartman et al. 2005, Lee et al. 2006, Oddo et al. 2006b, Chen et al. 2007) indicated that in the mouse models, effects on behavior did not necessarily correlate with effects on either plaque pathology or soluble brain Aβ levels as measured by ELISA. The first dissociation between effects on behavior and effects on plaques was initially considered likely to be due to neutralization of some form of toxic, soluble Aβ in the brain. The second dissociation between effects on behavior and effects on soluble Aβ levels as measured by ELISA suggested that this might not be the entire explanation either. A central role for rare but highly toxic soluble Aβ species (e.g., protofibrils, oligomers, ADDLs, Aβ* species) not easily measured by conventional ELISAs has been posited as an overarching framework to explain these findings (Walsh & Selkoe 2004). The potential importance of other aspects of AD pathology such as neurofibrillary tangles and the effects of tau abnormalities on axonal transport have also been revisited in this context (Lee & Trojanowski 2006, Oddo et al. 2006a). A fundamental issue that complicates interpretation of all these results is that we do not know whether behavioral abnormalities seen in APP transgenic mice are analogous to any of the cognitive deficits seen in humans with AD.
One potential concern associated with administration of certain anti-Aβ antibodies is intracerebral hemorrhage. Hemorrhages associated with cerebral amyloid angiopathy (CAA) were increased in APP transgenic mice treated with some antibodies, especially those that bind Aβ-containing plaques (Pfeifer et al. 2002, Wilcock et al. 2004b, Racke et al. 2005). This finding raises a new safety concern that may be relevant to humans because ∼90% of human AD patients have concomitant CAA, and similar intracranial hemorrhages were seen in one actively vaccinated patient (Ferrer et al. 2004). Most of these hemorrhages were small, and the clinical significance of these microbleeds is not entirely certain; they can be found frequently in asymptomatic patients with CAA (Towfighi et al. 2005). Likewise, one preclinical passive vaccination study reported that although there were larger numbers of microhemorrhages and worsening CAA in antibody-treated mice, these did not negate the generally positive effects of treatment on behavioral performance (Wilcock et al. 2004b).
POTENTIAL MECHANISMS UNDERLYING EFFECTS OF IMMUNOTHERAPEUTICS
Investigators have proposed a wide variety of mechanisms to explain various aspects of the effects of passive and active vaccination strategies. Most of this work has been based on mouse models used for preclinical development of AD treatments. Early reports of active vaccination trials presented immunohistochemical evidence for phagocytosis of Aβ deposits; small, densely staining Aβ plaques were seen in association with major histocompatability complex (MHC) II-labeled cells resembling activated microglia and monocytes (Schenk et al. 1999). This and the high anti-Aβ titers found in these mice suggested that antibody-directed clearance of plaques by phagocytosis (Figure 2a) could be a central mechanism. When administered systemically, a small fraction of certain anti-Aβ monoclonal antibodies gained access to the brain and bound plaques. In vitro experiments using monoclonal antibodies and cultured microglia supported the possibility that these antibodies trigger phagocytosis of Aβ deposits (Bard et al. 2000). Apparent phagocytosis of Aβ plaques was also observed in the brains of two patients who were treated with AN1792 and came to autopsy (Nicoll et al. 2003, Ferrer et al. 2004).
Figure 2.

Potential mechanisms underlying effects of immunotherapeutics in models of Alzheimer disease. These represent only a subset of the possibilities and are not meant to be considered mutually exclusive; more than one may be in operation at any given time or several may play important roles at different stages of therapy. (This figure was produced with the assistance of MedPIC at Washington University School of Medicine.) For further explanation, see Supplemental Material online.
Further studies indicated that fragment crystalizable (Fc) receptor-mediated phagocytosis is unlikely to be the only mechanism involved in plaque clearance. Bacskai et al. (2002) emonstrated that direct application of F(ab')2 fragments of the anti-Aβ antibody 3D6 to the surface of the brains of plaque-bearing mice resulted in clearance of Aβ deposits equivalent to the effects of application of full-length 3D6. F(ab')2 fragments generally have the same antigen-binding effects as full-length antibodies but lack the Fc portion of the antibody believed to be essential for triggering antibody-mediated phagocytosis via interactions with the Fc receptor on microglia and macrophages. This finding suggested that antibody binding could potentially directly disrupt Aβ aggregates, shifting the equilibrium between aggregates and monomeric Aβ toward the more readily cleared and degraded monomers (Figure 2b). This idea is supported by in vitro data demonstrating that anti-Aβ antibodies mixed with synthetic Aβ could prevent (Solomon et al. 1996, Legleiter et al. 2004) or reverse (Solomon et al. 1997) aggregation of Aβ fibrils. Although most antibodies that bind to insoluble Aβ aggregates and clear plaques have epitopes directed against the N-terminus of Aβ, many N-terminal antibodies bind to both soluble and insoluble Aβ and may thus have more than one mechanism of action (see below).
- Fragment crystalizable (Fc)
portion of immunoglobulin that binds to cells and is important in complement activation but is not involved in specific antigen binding
- F(ab')2
fragment of an immunoglobulin molecule that specifically binds to the antigen but does not contain the Fc portion
Interestingly, direct injection of F(ab')2 fragments of a different antibody (2286) resulted in diffuse plaque clearance but did not affect fibrillar Aβ deposit clearance (Wilcock et al. 2004a). These and other results suggest that there may be multiple, possibly sequential mechanisms of direct antibody-mediated plaque removal. Application of intact anti-Aβ antibody was reported to clear diffuse Aβ deposits within 24 h but clear fibrillar deposits only later at 72 h (Wilcock et al. 2003). Only the later phase was accompanied by a surge in the numbers of CD45-positive stained microglial cells. Fc-independent mechanisms appear capable of mediating the effects of active vaccination (Das et al. 2003) and systemic passive vaccination (Tamura et al. 2005) as well.
As noted above, dissociations between plaque clearance or Aβ levels measured by ELISA and behavioral effects have been well documented (Janus et al. 2000, Dodart et al. 2002, Kotilinek et al. 2002). The findings that exogenous administration of some specific forms of soluble Aβ could rapidly induce abnormalities in synaptic plasticity and in behavioral performance (Walsh et al. 2002, Cleary et al. 2005, Lesne et al. 2006) suggested that therapeutics that target specific soluble Aβ species may underlie these effects (Figure 2c). Experiments that unequivocally test the importance of this class of mechanisms in vivo have not been reported to our knowledge. There is, however, some supporting experimental evidence (Klyubin et al. 2005, Lee et al. 2006, Oddo et al. 2006a,b), and this is an area of active inquiry. A central question is still which if any of these protofibrils, oligomers, ADDLs, Aβ* species, etc., are present in the human brain, at which concentrations, and at which stages of disease. Oligomeric species of Aβ are challenging to measure, and detergents such as those used in extraction procedures or gel electrophoretic analyses lead to artificial assemblies (Hepler et al. 2006). This adds further uncertainty to the interpretation of these results.
Some evidence indicates that the effects of certain anti-Aβ antibodies may not actually require that these antibodies enter the brain. For example, the monoclonal antibody m266 has a very high affinity for soluble Aβ, can remove all free Aβ present in the blood of PDAPP mice, and does not bind Aβ plaques when given peripherally (DeMattos et al. 2001) or even when applied directly to AD brain sections (Racke et al. 2005). This and potentially other antibodies that bind to soluble Aβ may act as a “peripheral sink,” preventing transport of Aβ from blood back into the brain (Figure 2d) and thereby enhancing net clearance of Aβ (DeMattos et al. 2001). Much work has gone into investigations of the mechanisms of Aβ clearance from the brain into the blood (Deane et al. 2003), and net clearance can involve not only a peripheral sink effect but also an active Fc receptor-mediated process at the blood-brain barrier (Deane et al. 2005). This process could further favor Aβ clearance without requiring antibody persistence in the brain.
Although most of the above discussion has focused on antibody-mediated effects, antibody-independent, cell-mediated effects may underlie some of the benefits seen following active vaccination (Figure 2e). This could also be a mechanism by which nonspecific immunization results in plaque clearance (Frenkel et al. 2005). Cell-based immunotherapeutic approaches have demonstrated benefits in animal models of Parkinson disease (Benner et al. 2004) and amyotropic lateral sclerosis (Angelov et al. 2003).
Overall, there may be many mechanisms that can affect Aβ plaques, soluble Aβ levels, and/or behavioral performance. These may act concomitantly or sequentially, be differentially important depending on the stage of disease or type of antibody, and may be more or less relevant depending on factors such as the specific animal model system used and the animals' ages. Other mechanisms not discussed here in depth such as effects on Aβ-mediated vasoconstriction or modulation of CNS cytokine production may also be involved. Some, all, or none of these mechanisms may be relevant to treatment of human disease. Substantial numbers of additional clinical trials in human patients with translational mechanistic studies incorporated into their designs will be required to sort this out.
ACTIVE AND PASSIVE VACCINATION STRATEGIES IN ANIMAL MODELS OF OTHER NEURODEGENERATIVE DISEASES
Several laboratories have investigated immunotherapeutic strategies targeting proteins known or suspected to be involved in the pathogenesis of other neurodegenerative diseases (see Supplemental Table 3). All these approaches are still in preclinical development to our knowledge.
Prion Diseases
Farthest advanced is work on transmissible spongiform encephalopathies, such as Creutzfeld-Jacob disease in humans and scrapie in other species. Because the native prion protein (PrP) is widely expressed throughout life and creates immune tolerance, it was initially challenging to produce effective active and passive vaccinations in experimental animals (reviewed in Bade & Frey 2007). Several clever strategies were used to overcome this hurdle, including genetically engineering mice to produce single-chain anti-PrP antibodies (Heppner et al. 2001), infusing monoclonal antibodies produced using PrP knockout mice (White et al. 2003), and actively vaccinating mice with highly immunogenic papilloma virus-derived particles displaying PrP epitopes (Handisurya et al. 2007), among many others. Overall, there has been substantial progress in preclinical models. For example, active mucosal vaccination of mice using a recombinant attenuated salmonella strain expressing mouse PrP delayed or prevented clinical disease following oral challenge with an otherwise universally fatal oral dose of a mouse scrapie strain (Goni et al. 2005). Likewise, passive vaccination of mice using intraperitoneal injection of monoclonal anti-PrP antibodies starting after inoculation with scrapie brain homogenates but before onset of symptoms prevented clinical disease development (White et al. 2003). To our knowledge, none of the experimental approaches has as yet demonstrated alleviation of symptomatic disease (Bade & Frey 2007).
Parkinson Disease and Amyotrophic Lateral Sclerosis
Several strategies similar to those used in AD have been tested in mouse models of Parkinson disease and amyotrophic lateral sclerosis (see Supplemental Table 3). Active vaccination with human α-synuclein in a familial Parkinson disease mouse model characterized by accumulation of α-synuclein aggregates provided some benefit in terms of pathological outcomes (Masliah et al. 2005b). Likewise, active vaccination with misfolded mutant superoxide dismutase 1 (SOD-1) in a familial amyotrophic lateral sclerosis mouse model carrying an SOD-1 mutation reduced loss of spinal cord neurons and caused a modest but statistically significant increase in life expectancy (Urushitani et al. 2007). Some benefits of nonspecific active vaccinations with Copaxone-based regimens have been reported (Angelov et al. 2003, Benner et al. 2004) in ALS and Parkinson models, although safety concerns have been raised (Haenggeli et al. 2007). The effects of passive vaccination approaches to these diseases have not been reported to our knowledge, but this clearly represents an avenue for future research.
- Copaxone (also termed glatiramer acetate and copolymer-1)
synthetic random polypeptide consisting of the amino acids tyrosine, glutamate, alanine and lysine
Acute CNS Insults that May Trigger Neurodegeneration
Aβ may play a pathogenic role in other conditions besides AD, and some of the same immunotherapeutics under development for AD have been assessed as potential neuroprotectants for other central nervous system insults such as seizures and traumatic brain injury (TBI). For example, pretreatment with an anti-Aβ monoclonal antibody reduced seizure-related neuronal loss in the hippocampi of Tg2576 mice (Mohajeri et al. 2002). Likewise, our collaborative group treated young PDAPP mice with the anti-Aβ antibody m266 starting shortly before and continuing weekly after moderately severe experimental TBI. The m266-treated mice displayed markedly improved behavioral performance in the Morris water maze, reduced loss of hippocampal CA3 cells, and increased apparent neurogenesis in the dentate gyrus (Brody et al. 2005). An extensive epidemiological and pathological literature links TBI and the subsequent risk of AD (Jellinger 2004).
ONGOING CLINICAL DEVELOPMENT OF IMMUNOTHERAPEUTIC STRATEGIES TO COMBAT AD
Passive Vaccination
Farthest advanced at the time of this writing is the Elan/Wyeth trial of AAB-001 (Bapineuzumab), which was entering phase III testing in 2007. This approach involves passive immunization with an Aβ N-terminal directed, humanized monoclonal antibody. The murine version of this antibody binds to both soluble and aggregated Aβ (Bard et al. 2000, Racke et al. 2005). The N-terminal 8 amino acids of Aβ were the predominant epitope recognized by antibodies in the sera from 45 vaccinated patients in the AN1792 trial (Lee et al. 2005), which also bound to both soluble and aggregated Aβ. Thus, passive vaccination with an N-terminal antibody with similar features may be expected to mimic aspects of the antibody portion of the response to active vaccination. Phase I results have been reported only in abstract form (Ninth Int. Geneva/Springfield Symp. Alzeimer Ther. 2006), and the multiple-dose phase II trial has not yet been completed. A small amyloid imaging substudy is also part of this trial.
Next most advanced to our knowledge is the Eli Lilly and Co. phase II trial of LY2062430, which involves passive vaccination with an Aβ central domain directed, humanized monoclonal antibody. Systemic administration of the closely related central domain mouse monoclonal antibody m266 rapidly improved behavioral performance (Dodart et al. 2002, Bales et al. 2006) and decreased plaque formation (DeMattos et al. 2001) in preclinical studies. Thus far, this antibody has not been shown to reverse existing plaque pathology or bind directly to plaques. On the other hand, this antibody did not worsen intracerebral hemorrhage or vascular pathology in older APP transgenic mice (Racke et al. 2005). Unlike the AAB-001 trial, patients on anticoagulants or with contraindications to MRI are not specifically excluded from the LY2062430 trial (http://www.clinicaltrials.gov). The phase I results have been reported only in abstract form, and no safety concerns were raised (10th Int. Conf. Alzheimer's Dis. Relat. Disord. 2006).
The Pfizer/Rinat phase I trial of RN-1219 (PF-04360365), another humanized monoclonal antibody recognizing Aβ, excludes patients with hemorrhages, infarctions, or extensive white matter changes on MRI (http://www.clinicaltrials.gov). Detailed information about this antibody has not been publicly disclosed. Likewise, few details are available regarding the Hoffman-La Roche/MorphoSys phase I trial of R-1450 (http://www.centerwatch.com), a fully human monoclonal antibody developed using the MorphoSys HuCAL platform (Knappik et al. 2000). The protocol registry for this trial does not list MRI-based or anticoagulation-related exclusion criteria.
Active Vaccination
Refined active vaccination strategies for AD are also still considered viable options. The Elan/Wyeth ACC-001 phase I active vaccination trial started in the fall of 2005. The vaccine reportedly was designed to elicit specific antibody responses while minimizing the deleterious inflammatory responses seen in the AN1792 trial. This approach uses an Aβ fragment attached to a carrier protein (http://www.alzforum.com). Two other phase I active vaccination trials are underway: the CAD-106 trial led by a Novartis/Cytos collaboration and the V950 trial initiated by Merck.
FDA-Approved Immunotherapeutics
The safety concerns raised by AN1792, as well as several other new drugs in recent years, have spurred interest in using FDA-approved therapeutics with established safety records for new indications (e.g., Rothstein et al. 2005). Dodel et al. (2002) have found that human intravenous immunoglobulin (IVIg) contains some endogenously produced anti-Aβ antibodies, along with a great variety of other antibodies. Two small phase I studies of IVIg infusions have been completed (Dodel et al. 2004), and a phase II study is underway as of this writing. An amyloid-imaging substudy with the PET ligand Pittsburg Compound-B (Klunk et al. 2004) is also part of this trial (http://www.clinicaltrials.gov).
FUTURE DIRECTIONS
Preclinical Predictors of Clinical Efficacy
One major question remains how to decide which preclinical therapeutics to move into clinical trials. The issue is that we do not have a solid understanding of which outcomes in preclinical models will best predict efficacy in human patients. Aβ plaques in many mouse models are very similar to those in human AD patients. However, it is not clear whether reducing Aβ plaque burden in the brains of patients with concomitant tangle pathology, reduced numbers of synapses, and extensive neuronal loss will have a meaningful benefit in terms of memory and other cognitive functions. In addition, the behavioral performance deficits in the mouse models are quite different in many respects from the clinical symptoms in human patients, thus the importance of targeting these deficits has been hotly debated. Specifically, many mouse models show early behavioral performance deficits on tests of memory and other cognitive function at young ages, often before substantial plaque pathology is observed (Smith et al. 1998, Lesne et al. 2006). In contrast, significant Aβ plaque pathology is likely present for a decade or longer before cognitive symptoms are apparent in humans (Braak & Braak 1997, Price & Morris 1999, Price et al. 2001).
Based on the data available in humans, cognitive symptoms correlate best with the onset and progression of neuronal and synaptic loss later in life (Masliah et al. 2001, Price et al. 2001, Scheff & Price 2003). However, no mouse model developed to date fully recapitulates these aspects of the disease.
Recently, attention from several groups has turned to Aβ-targeted immunotherapeutic effects on additional aspects of AD-related pathology seen in the mouse models. Preclinical studies have reported improvements in abnormalities of the geometry of neuronal processes (Lombardo et al. 2003), early tau pathology (Oddo et al. 2004), loss of synaptophysin immunoreactivity (Buttini et al. 2005), and neuritic dystrophy (Brendza et al. 2005). More advanced tau pathology was not affected by anti-Aβ antibody treatment (Oddo et al. 2004) nor did it appear that there was a clear reduction in tau pathology in the vaccinated human patients in the AN1792 trial.
Thus it is not clear at this time whether preclinical immunotherapeutics should be advanced to clinical trials on the basis of efficacy in (a) reducing Aβ plaque and/or tangle pathology, (b) blocking effects of soluble oligomeric Aβ species, (c) alleviating behavioral deficits, or (d) preventing neuronal and/or synaptic loss. An immunotherapeutic strategy may need to be successful at only some or all of these to offer a meaningful benefit to human patients. Although the panoply of available animal models may be useful, none currently recapitulates all aspects of human AD.
Because of the enormous resources being devoted to AD, effective clinical therapeutics for this condition may be developed by trial and error without a thorough mechanistic understanding of their actions. Although any effective therapeutic would be most welcome, the ability to generalize the approach to other, less common, or as-yet-undiscovered neurodegenerative conditions would be markedly enhanced if the mechanistic principles underlying efficacy were understood. Thus, further detailed investigation of the pathophysiology of neurodegenerative diseases in human patients and careful exploration of the effects of immunotherapeutic strategies in both mice and humans are clearly required.
Clinical Trial Design
A second major question revolves around the design of the clinical trials themselves. Should patients with relatively rare, heritable forms of the disorders be enrolled first? Nearly all the preclinical animal models are based on the genes implicated in these subsets of patients, and therefore one could argue that therapeutics developed using such animal models are most likely to work in the human diseases bearing the most resemblance to them. Or should the more common, sporadic, later-onset forms of the diseases be attacked first, in the hopes of bringing the greatest benefit soonest to the largest numbers of people?
Likewise, should symptomatic patients be enrolled, or should efforts focus on identifying presymptomatic patients with genetic, biomarker-based or imaging evidence of disease pathophysiology? An argument for presymptomatic treatment states that in preclinical studies, many therapeutic approaches have been more effective in younger mice with less advanced disease than in older mice with more advanced disease. Because the central nervous system has limited regenerative capacity, neuronal and synaptic loss is not likely to be reversible once it has occurred, and the most effective immunotherapeutic approaches will therefore require prevention of such losses. The analogy to treating coronary artery disease before the development of ischemic cardiomyopathy and consequent congestive heart failure is salient. Although none of our current approaches for detecting presymptomatic patients with nonautosomal dominant familial neurodegenerative disorders has been fully validated at present, encouraging progress along these lines has been made using noninvasive PET-based imaging of fibrillar Aβ structures and measurement of cerebrospinal fluid levels of Aβ42 and tau (Klunk et al. 2004, Fagan et al. 2006, Fagan et al. 2007). Thus this approach may be feasible in the near future.
Economic Issues
A third, but clearly important issue is an economic one. The expense of giving weekly or monthly monoclonal antibody infusions for years or decades could be considerable. The price of commonly used monoclonal antibodies on the market today is typically hundreds to thousands of dollars per dose, and this price does not include the costs associated with starting intravenous lines and monitoring infusions. This is not to say that the approach is not feasible; cancer treatments routinely involve monitored intravenous infusions of very expensive medications. However, cycles of chemotherapy usually last weeks to months, rather than years to decades. On the other hand, if these treatments can keep patients out of nursing homes longer, allow them to take better care of their other health issues, and potentially even keep them in the workforce longer, the economic effect could still be a net benefit. Nonetheless, the specter of effective therapeutics affordable only to an elite few has its harbinger in issues about the availability of Herceptin in certain health care systems (Hutchinson & DeVita 2005). Active immunization, despite the safety issues that have arisen, would likely be much more cost-effective than passive immunotherapy. Small molecules or other approaches unrelated to immunotherapeutics may prove still more economically efficient in the long run.
CONCLUSION
Overall, the field of active and passive immunotherapeutics for neurodegenerative disorders has been a vibrant one. However, a review of the timeline in the field of immunotherapeutic development for neoplastic disorders suggests that we may still have a long way to go. To date, cancer research has subsumed an even greater net effort than has research in the neurodegenerative disorders. Yet a full 20 years elapsed from when the results of first trials of monoclonal antibodies in animal models were reported in 1977 until the first FDA approval of a monoclonal antibody-based therapeutic for a human cancer in 1997 (see Figure 3). Thus, far from being near the end of the road in terms of fundamental research on neurodegenerative disorders, it seems more likely that we are solidly in the middle of the journey, with many miles to go before we rest.
Figure 3.
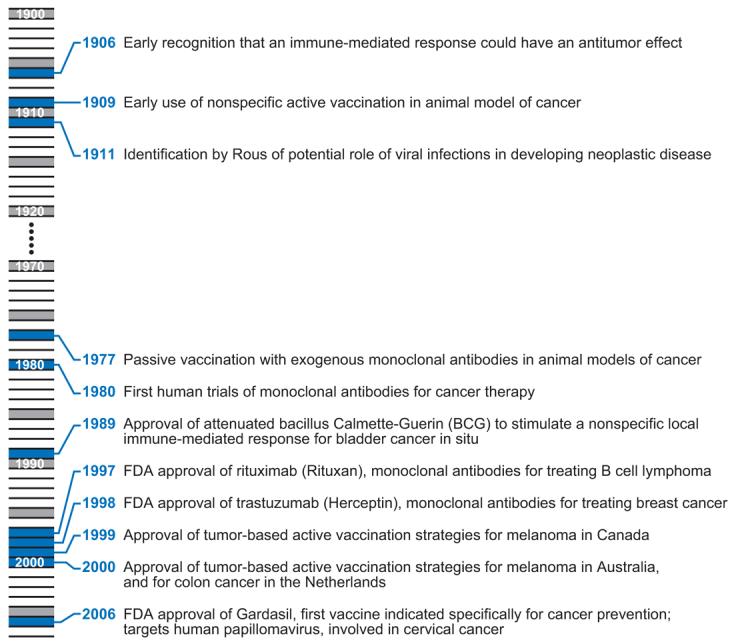
Putting the timeline in perspective: immunotherapeutic strategies for neoplastic disorders.
FUTURE ISSUES.
How can patients with neurodegenerative disorders be identified in the earliest, even preclinical stages, and will immunotherapies initiated at these early stages prove especially effective?
Which pathophysiological events are targeted by effective immunotherapeutic strategies in preclinical animal models of disease? Do these same pathophysiological events occur and play important roles in human patients?
Will immunotherapeutic strategies specifically targeting rare but highly toxic soluble assemblies of the proteins believed to play central roles in neurodegenerative diseases offer therapeutic advantages over other targeting strategies?
How can clinical trials in neurodegenerative disorders—which often progress over the span of years to decades—be accelerated? Which biomarkers, clinical assessment strategies, or imaging approaches will make clinical trial design more efficient?
Can the essential aspects of the human immune response be modeled using experimental animals, including the tremendous variability caused by genetic and environmental factors? Will this approach lead to more rapid development of safe and effective therapeutics?
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by NIH grants AG13956, AG20222, and NS049237, a Burroughs Wellcome Career Award in the Biomedical Sciences, The Cure Alzheimer's Fund, and the MetLife Foundation. We thank Ronald Demattos and Edgar Engleman for helpful comments.
Footnotes
A search of PubMed on June 2, 2007, for neurodegenerative disease AND immunotherapy yielded 222 review articles.
DISCLOSURE STATEMENT
David Holtzman is a coinventor on U.S. patent 7,195,761 entitled “Humanized antibodies that sequester abeta peptide” as well as other submitted patents on related topics. Washington University may receive income based on a license of these patents to Eli Lilly.
LITERATURE CITED
- Angelov DN, Waibel S, Guntinas-Lichius O, Lenzen M, Neiss WF, et al. Therapeutic vaccine for acute and chronic motor neuron diseases: implications for amyotrophic lateral sclerosis. Proc. Natl. Acad. Sci. USA. 2003;100:4790–95. doi: 10.1073/pnas.0530191100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin L, Arendash GW, Gordon MN, Diamond DM, DiCarlo G, et al. Short-term beta-amyloid vaccinations do not improve cognitive performance in cognitively impaired APP + PS1 mice. Behav. Neurosci. 2003;117:478–84. doi: 10.1037/0735-7044.117.3.478. [DOI] [PubMed] [Google Scholar]
- Bacskai BJ, Kajdasz ST, McLellan ME, Games D, Seubert P, et al. Non-Fc-mediated mechanisms are involved in clearance of amyloid-beta in vivo by immunotherapy. J. Neurosci. 2002;22:7873–78. doi: 10.1523/JNEUROSCI.22-18-07873.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bade S, Frey A. Potential of active and passive immunizations for the prevention and therapy of transmissible spongiform encephalopathies. Expert Rev. Vaccin. 2007;6:153–68. doi: 10.1586/14760584.6.2.153. [DOI] [PubMed] [Google Scholar]
- Bales KR, Tzavara ET, Wu S, Wade MR, Bymaster FP, et al. Cholinergic dysfunction in a mouse model of Alzheimer disease is reversed by an anti-Abeta antibody. J. Clin. Invest. 2006;116:825–32. doi: 10.1172/JCI27120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bard F, Cannon C, Barbour R, Burke RL, Games D, et al. Peripherally administered antibodies against amyloid beta-peptide enter the central nervous system and reduce pathology in a mouse model of Alzheimer disease. Nat. Med. 2000;6:916–19. doi: 10.1038/78682. [DOI] [PubMed] [Google Scholar]
- Bard F, Barbour R, Cannon C, Carretto R, Fox M, et al. Epitope and isotype specificities of antibodies to beta-amyloid peptide for protection against Alzheimer's disease-like neuropathology. Proc. Natl. Acad. Sci. USA. 2003;100:2023–28. doi: 10.1073/pnas.0436286100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayer AJ, Bullock R, Jones RW, Wilkinson D, Paterson KR, et al. Evaluation of the safety and immunogenicity of synthetic Abeta42 (AN1792) in patients with AD. Neurology. 2005;64:94–101. doi: 10.1212/01.WNL.0000148604.77591.67. [DOI] [PubMed] [Google Scholar]
- Benner EJ, Mosley RL, Destache CJ, Lewis TB, Jackson-Lewis V, et al. Therapeutic immunization protects dopaminergic neurons in a mouse model of Parkinson's disease. Proc. Natl. Acad. Sci. USA. 2004;101:9435–40. doi: 10.1073/pnas.0400569101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braak H, Braak E. Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiol. Aging. 1997;18:351–57. doi: 10.1016/s0197-4580(97)00056-0. [DOI] [PubMed] [Google Scholar]
- Brendza RP, Bacskai BJ, Cirrito JR, Simmons KA, Skoch JM, et al. Anti-Abeta antibody treatment promotes the rapid recovery of amyloid-associated neuritic dystrophy in PDAPP transgenic mice. J. Clin. Invest. 2005;115:428–33. doi: 10.1172/JCI23269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody DL, Mac Donald CL, Fujimoto S, Conte V, Parsadanian M, et al. Anti-Abeta antibody treatment attenuates cognitive impairment in a mouse model of experimental traumatic brain injury; Presented at Annu. Natl. Neurotrauma Soc. Symp., 23rd; Washington DC. 2005. [Google Scholar]
- Buttini M, Masliah E, Barbour R, Grajeda H, Motter R, et al. Beta-amyloid immunotherapy prevents synaptic degeneration in a mouse model of Alzheimer's disease. J. Neurosci. 2005;25:9096–101. doi: 10.1523/JNEUROSCI.1697-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G, Chen KS, Kobayashi D, Barbour R, Motter R, et al. Active beta-amyloid immunization restores spatial learning in PDAPP mice displaying very low levels of beta-amyloid. J. Neurosci. 2007;27:2654–62. doi: 10.1523/JNEUROSCI.3710-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chishti MA, Yang DS, Janus C, Phinney AL, Horne P, et al. Early-onset amyloid deposition and cognitive deficits in transgenic mice expressing a double mutant form of amyloid precursor protein 695. J. Biol. Chem. 2001;276:21562–70. doi: 10.1074/jbc.M100710200. [DOI] [PubMed] [Google Scholar]
- Cleary JP, Walsh DM, Hofmeister JJ, Shankar GM, Kuskowski MA, et al. Natural oligomers of the amyloid-beta protein specifically disrupt cognitive function. Nat. Neurosci. 2005;8:79–84. doi: 10.1038/nn1372. [DOI] [PubMed] [Google Scholar]
- Das P, Howard V, Loosbrock N, Dickson D, Murphy MP, et al. Amyloid-beta immunization effectively reduces amyloid deposition in FcRgamma−/− knock-out mice. J. Neurosci. 2003;23:8532–38. doi: 10.1523/JNEUROSCI.23-24-08532.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das P, Murphy MP, Younkin LH, Younkin SG, Golde TE. Reduced effectiveness of Abeta1-42 immunization in APP transgenic mice with significant amyloid deposition. Neurobiol. Aging. 2001;22:721–27. doi: 10.1016/s0197-4580(01)00245-7. [DOI] [PubMed] [Google Scholar]
- Deane R, Du Yan S, Submamaryan RK, LaRue B, Jovanovic S, et al. RAGE mediates amyloid-beta peptide transport across the blood-brain barrier and accumulation in brain. Nat. Med. 2003;9:907–13. doi: 10.1038/nm890. [DOI] [PubMed] [Google Scholar]
- Deane R, Sagare A, Hamm K, Parisi M, LaRue B, et al. IgG-assisted age-dependent clearance of Alzheimer's amyloid beta peptide by the blood-brain barrier neonatal Fc receptor. J. Neurosci. 2005;25:11495–503. doi: 10.1523/JNEUROSCI.3697-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMattos RB, Bales KR, Cummins DJ, Dodart JC, Paul SM, et al. Peripheral anti-Abeta antibody alters CNS and plasma Abeta clearance and decreases brain Abeta burden in a mouse model of Alzheimer's disease. Proc. Natl. Acad. Sci. USA. 2001;98:8850–55. doi: 10.1073/pnas.151261398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodart JC, Bales KR, Gannon KS, Greene SJ, DeMattos RB, et al. Immunization reverses memory deficits without reducing brain Abeta burden in Alzheimer's disease model. Nat. Neurosci. 2002;5:452–57. doi: 10.1038/nn842. [DOI] [PubMed] [Google Scholar]
- Dodel R, Hampel H, Depboylu C, Lin S, Gao F, et al. Human antibodies against amyloid beta peptide: a potential treatment for Alzheimer's disease. Ann. Neurol. 2002;52:253–56. doi: 10.1002/ana.10253. [DOI] [PubMed] [Google Scholar]
- Dodel RC, Du Y, Depboylu C, Hampel H, Frolich L, et al. Intravenous immunoglobulins containing antibodies against beta-amyloid for the treatment of Alzheimer's disease. J. Neurol. Neurosurg. Psychiatry. 2004;75:1472–74. doi: 10.1136/jnnp.2003.033399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eng JA, Frosch MP, Choi K, Rebeck GW, Greenberg SM. Clinical manifestations of cerebral amyloid angiopathy-related inflammation. Ann. Neurol. 2004;55:250–56. doi: 10.1002/ana.10810. [DOI] [PubMed] [Google Scholar]
- Fagan AM, Mintun MA, Mach RH, Lee SY, Dence CS, et al. Inverse relation between in vivo amyloid imaging load and cerebrospinal fluid Abeta42 in humans. Ann. Neurol. 2006;59:512–19. doi: 10.1002/ana.20730. [DOI] [PubMed] [Google Scholar]
- Fagan AM, Roe CM, Xiong C, Mintun MA, Morris JC, et al. Cerebrospinal fluid tau/beta-amyloid(42) ratio as a prediction of cognitive decline in nondemented older adults. Arch. Neurol. 2007;64:343–49. doi: 10.1001/archneur.64.3.noc60123. [DOI] [PubMed] [Google Scholar]
- Ferrer I, Boada Rovira M, Sanchez Guerra ML, Rey MJ, Costa-Jussa F. Neuropathology and pathogenesis of encephalitis following amyloid-beta immunization in Alzheimer's disease. Brain Pathol. 2004;14:11–20. doi: 10.1111/j.1750-3639.2004.tb00493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox NC, Black RS, Gilman S, Rossor MN, Griffith SG, et al. Effects of Abeta immunization (AN1792) on MRI measures of cerebral volume in Alzheimer disease. Neurology. 2005;64:1563–72. doi: 10.1212/01.WNL.0000159743.08996.99. [DOI] [PubMed] [Google Scholar]
- Frenkel D, Maron R, Burt DS, Weiner HL. Nasal vaccination with a proteosome-based adjuvant and glatiramer acetate clears beta-amyloid in a mouse model of Alzheimer disease. J. Clin. Invest. 2005;115:2423–33. doi: 10.1172/JCI23241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Games D, Adams D, Alessandrini R, Barbour R, Berthelette P, et al. Alzheimer-type neuropathology in transgenic mice overexpressing V717F beta-amyloid precursor protein. Nature. 1995;373:523–27. doi: 10.1038/373523a0. [DOI] [PubMed] [Google Scholar]
- Gilman S, Koller M, Black RS, Jenkins L, Griffith SG, et al. Clinical effects of Abeta immunization (AN1792) in patients with AD in an interrupted trial. Neurology. 2005;64:1553–62. doi: 10.1212/01.WNL.0000159740.16984.3C. [DOI] [PubMed] [Google Scholar]
- Goni F, Knudsen E, Schreiber F, Scholtzova H, Pankiewicz J, et al. Mucosal vaccination delays or prevents prion infection via an oral route. Neuroscience. 2005;133:413–21. doi: 10.1016/j.neuroscience.2005.02.031. [DOI] [PubMed] [Google Scholar]
- Haenggeli C, Julien JP, Lee Mosley R, Perez N, Dhar A, et al. Therapeutic immunization with a glatiramer acetate derivative does not alter survival in G93A and G37R SOD1 mouse models of familial ALS. Neurobiol. Dis. 2007;26:146–52. doi: 10.1016/j.nbd.2006.12.013. [DOI] [PubMed] [Google Scholar]
- Handisurya A, Gilch S, Winter D, Shafti-Keramat S, Maurer D, et al. Vaccination with prion peptide-displaying papillomavirus-like particles induces autoantibodies to normal prion protein that interfere with pathologic prion protein production in infected cells. FEBS J. 2007;274:1747–58. doi: 10.1111/j.1742-4658.2007.05721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman RE, Izumi Y, Bales KR, Paul SM, Wozniak DF, et al. Treatment with an amyloid-beta antibody ameliorates plaque load, learning deficits, and hippocampal long-term potentiation in a mouse model of Alzheimer's disease. J. Neurosci. 2005;25:6213–20. doi: 10.1523/JNEUROSCI.0664-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepler RW, Grimm KM, Nahas DD, Breese R, Dodson EC, et al. Solution state characterization of amyloid beta-derived diffusible ligands. Biochemistry. 2006;45:15157–67. doi: 10.1021/bi061850f. [DOI] [PubMed] [Google Scholar]
- Heppner FL, Musahl C, Arrighi I, Klein MA, Rulicke T, et al. Prevention of scrapie pathogenesis by transgenic expression of anti-prion protein antibodies. Science. 2001;294:178–82. doi: 10.1126/science.1063093. [DOI] [PubMed] [Google Scholar]
- Hock C, Konietzko U, Streffer JR, Tracy J, Signorell A, et al. Antibodies against beta-amyloid slow cognitive decline in Alzheimer's disease. Neuron. 2003;38:547–54. doi: 10.1016/s0896-6273(03)00294-0. [DOI] [PubMed] [Google Scholar]
- Hsiao K, Chapman P, Nilsen S, Eckman C, Harigaya Y, et al. Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice. Science. 1996;274:99–102. doi: 10.1126/science.274.5284.99. [DOI] [PubMed] [Google Scholar]
- Hutchinson L, DeVita VT., Jr Herceptin: HERalding a new era in breast cancer care but at what cost? Nat. Clin. Pract. Oncol. 2005;2:595. doi: 10.1038/ncponc0378. [DOI] [PubMed] [Google Scholar]
- Janus C, Pearson J, McLaurin J, Mathews PM, Jiang Y, et al. Abeta peptide immunization reduces behavioural impairment and plaques in a model of Alzheimer's disease. Nature. 2000;408:979–82. doi: 10.1038/35050110. [DOI] [PubMed] [Google Scholar]
- Jellinger KA. Head injury and dementia. Curr. Opin. Neurol. 2004;17:719–23. doi: 10.1097/00019052-200412000-00012. [DOI] [PubMed] [Google Scholar]
- Jenner E. An inquiry into the causes and effects of the Variolae-Vacciniae, a disease discovered in some of the western counties of England, particularly Gloucestershire, and known by the name of cow pox. 1798 http://www.bartleby.com/38/4/1.html.
- Johnson-Wood K, Lee M, Motter R, Hu K, Gordon G, et al. Amyloid precursor protein processing and Abeta42 deposition in a transgenic mouse model of Alzheimer disease. Proc. Natl. Acad. Sci. USA. 1997;94:1550–55. doi: 10.1073/pnas.94.4.1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klunk WE, Engler H, Nordberg A, Wang Y, Blomqvist G, et al. Imaging brain amyloid in Alzheimer's disease with Pittsburgh Compound-B. Ann. Neurol. 2004;55:306–19. doi: 10.1002/ana.20009. [DOI] [PubMed] [Google Scholar]
- Klunk WE, Price JC, Mathis CA, Tsopelas ND, Lopresti BJ, et al. Amyloid deposition begins in the striatum of presenilin-1 mutation carriers from two unrelated pedigrees. J. Neurosci. 2007;27:6174–84. doi: 10.1523/JNEUROSCI.0730-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klyubin I, Walsh DM, Lemere CA, Cullen WK, Shankar GM, et al. Amyloid beta protein immunotherapy neutralizes Abeta oligomers that disrupt synaptic plasticity in vivo. Nat. Med. 2005;11:556–61. doi: 10.1038/nm1234. [DOI] [PubMed] [Google Scholar]
- Knappik A, Ge L, Honegger A, Pack P, Fischer M, et al. Fully synthetic human combinatorial antibody libraries (HuCAL) based on modular consensus frameworks and CDRs randomized with trinucleotides. J. Mol. Biol. 2000;296:57–86. doi: 10.1006/jmbi.1999.3444. [DOI] [PubMed] [Google Scholar]
- Kotilinek LA, Bacskai B, Westerman M, Kawarabayashi T, Younkin L, et al. Reversible memory loss in a mouse transgenic model of Alzheimer's disease. J. Neurosci. 2002;22:6331–35. doi: 10.1523/JNEUROSCI.22-15-06331.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EB, Leng LZ, Zhang B, Kwong L, Trojanowski JQ, et al. Targeting amyloid-beta peptide (Abeta) oligomers by passive immunization with a conformation-selective monoclonal antibody improves learning and memory in Abeta precursor protein (APP) transgenic mice. J. Biol. Chem. 2006;281:4292–99. doi: 10.1074/jbc.M511018200. [DOI] [PubMed] [Google Scholar]
- Lee M, Bard F, Johnson-Wood K, Lee C, Hu K, et al. Abeta42 immunization in Alzheimer's disease generates Abeta N-terminal antibodies. Ann. Neurol. 2005;58:430–35. doi: 10.1002/ana.20592. [DOI] [PubMed] [Google Scholar]
- Lee VM, Trojanowski JQ. Progress from Alzheimer's tangles to pathological tau points towards more effective therapies now. J. Alzheimers Dis. 2006;9:257–62. doi: 10.3233/jad-2006-9s328. [DOI] [PubMed] [Google Scholar]
- Legleiter J, Czilli DL, Gitter B, DeMattos RB, Holtzman DM, et al. Effect of different anti-Abeta antibodies on Abeta fibrillogenesis as assessed by atomic force microscopy. J. Mol. Biol. 2004;335:997–1006. doi: 10.1016/j.jmb.2003.11.019. [DOI] [PubMed] [Google Scholar]
- Lesne S, Koh MT, Kotilinek L, Kayed R, Glabe CG, et al. A specific amyloid-beta protein assembly in the brain impairs memory. Nature. 2006;440:352–57. doi: 10.1038/nature04533. [DOI] [PubMed] [Google Scholar]
- Lombardo JA, Stern EA, McLellan ME, Kajdasz ST, Hickey GA, et al. Amyloid-beta antibody treatment leads to rapid normalization of plaque-induced neuritic alterations. J. Neurosci. 2003;23:10879–83. doi: 10.1523/JNEUROSCI.23-34-10879.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masliah E, Hansen L, Adame A, Crews L, Bard F, et al. Abeta vaccination effects on plaque pathology in the absence of encephalitis in Alzheimer disease. Neurology. 2005a;64:129–31. doi: 10.1212/01.WNL.0000148590.39911.DF. [DOI] [PubMed] [Google Scholar]
- Masliah E, Mallory M, Alford M, DeTeresa R, Hansen LA, et al. Altered expression of synaptic proteins occurs early during progression of Alzheimer's disease. Neurology. 2001;56:127–29. doi: 10.1212/wnl.56.1.127. [DOI] [PubMed] [Google Scholar]
- Masliah E, Rockenstein E, Adame A, Alford M, Crews L, et al. Effects of alpha-synuclein immunization in a mouse model of Parkinson's disease. Neuron. 2005b;46:857–68. doi: 10.1016/j.neuron.2005.05.010. [DOI] [PubMed] [Google Scholar]
- Mohajeri MH, Saini K, Schultz JG, Wollmer MA, Hock C, et al. Passive immunization against beta-amyloid peptide protects central nervous system (CNS) neurons from increased vulnerability associated with an Alzheimer's disease-causing mutation. J. Biol. Chem. 2002;277:33012–17. doi: 10.1074/jbc.M203193200. [DOI] [PubMed] [Google Scholar]
- Morgan D, Diamond DM, Gottschall PE, Ugen KE, Dickey C, et al. Abeta peptide vaccination prevents memory loss in an animal model of Alzheimer's disease. Nature. 2000;408:982–85. doi: 10.1038/35050116. [DOI] [PubMed] [Google Scholar]
- Morris R. Developments of a water-maze procedure for studying spatial learning in the rat. J. Neurosci. Methods. 1984;11:47–60. doi: 10.1016/0165-0270(84)90007-4. [DOI] [PubMed] [Google Scholar]
- Nicoll JA, Wilkinson D, Holmes C, Steart P, Markham H, et al. Neuropathology of human Alzheimer disease after immunization with amyloid-beta peptide: a case report. Nat. Med. 2003;9:448–52. doi: 10.1038/nm840. [DOI] [PubMed] [Google Scholar]
- Oddo S, Billings L, Kesslak JP, Cribbs DH, LaFerla FM. Abeta immunotherapy leads to clearance of early, but not late, hyperphosphorylated tau aggregates via the proteasome. Neuron. 2004;43:321–32. doi: 10.1016/j.neuron.2004.07.003. [DOI] [PubMed] [Google Scholar]
- Oddo S, Caccamo A, Tran L, Lambert MP, Glabe CG, et al. Temporal profile of amyloid-beta (Abeta) oligomerization in an in vivo model of Alzheimer disease. A link between Abeta and tau pathology. J. Biol. Chem. 2006a;281:1599–604. doi: 10.1074/jbc.M507892200. [DOI] [PubMed] [Google Scholar]
- Oddo S, Vasilevko V, Caccamo A, Kitazawa M, Cribbs DH, et al. Reduction of soluble Abeta and tau, but not soluble Abeta alone, ameliorates cognitive decline in transgenic mice with plaques and tangles. J. Biol. Chem. 2006b;281:39413–23. doi: 10.1074/jbc.M608485200. [DOI] [PubMed] [Google Scholar]
- Orgogozo JM, Gilman S, Dartigues JF, Laurent B, Puel M, et al. Subacute meningoencephalitis in a subset of patients with AD after Abeta42 immunization. Neurology. 2003;61:46–54. doi: 10.1212/01.wnl.0000073623.84147.a8. [DOI] [PubMed] [Google Scholar]
- Patton RL, Kalback WM, Esh CL, Kokjohn TA, Van Vickle GD, et al. Amyloid-beta peptide remnants in AN-1792-immunized Alzheimer's disease patients: a biochemical analysis. Am. J. Pathol. 2006;169:1048–63. doi: 10.2353/ajpath.2006.060269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeifer M, Boncristiano S, Bondolfi L, Stalder A, Deller T, et al. Cerebral hemorrhage after passive anti-Abeta immunotherapy. Science. 2002;298:1379. doi: 10.1126/science.1078259. [DOI] [PubMed] [Google Scholar]
- Price JL, Ko AI, Wade MJ, Tsou SK, McKeel DW, et al. Neuron number in the entorhinal cortex and CA1 in preclinical Alzheimer disease. Arch. Neurol. 2001;58:1395–402. doi: 10.1001/archneur.58.9.1395. [DOI] [PubMed] [Google Scholar]
- Price JL, Morris JC. Tangles and plaques in nondemented aging and “preclinical” Alzheimer's disease. Ann. Neurol. 1999;45:358–68. doi: 10.1002/1531-8249(199903)45:3<358::aid-ana12>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Racke MM, Boone LI, Hepburn DL, Parsadainian M, Bryan MT, et al. Exacerbation of cerebral amyloid angiopathy-associated microhemorrhage in amyloid precursor protein transgenic mice by immunotherapy is dependent on antibody recognition of deposited forms of amyloid beta. J. Neurosci. 2005;25:629–36. doi: 10.1523/JNEUROSCI.4337-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothstein JD, Patel S, Regan MR, Haenggeli C, Huang YH, et al. Beta-lactam antibiotics offer neuroprotection by increasing glutamate transporter expression. Nature. 2005;433:73–77. doi: 10.1038/nature03180. [DOI] [PubMed] [Google Scholar]
- Scheff SW, Price DA. Synaptic pathology in Alzheimer's disease: a review of ultrastructural studies. Neurobiol. Aging. 2003;24:1029–46. doi: 10.1016/j.neurobiolaging.2003.08.002. [DOI] [PubMed] [Google Scholar]
- Schenk D, Barbour R, Dunn W, Gordon G, Grajeda H, et al. Immunization with amyloid-beta attenuates Alzheimer-disease-like pathology in the PDAPP mouse. Nature. 1999;400:173–77. doi: 10.1038/22124. [DOI] [PubMed] [Google Scholar]
- Skovronsky DM, Lee VM, Trojanowski JQ. Neurodegenerative diseases: new concepts of pathogenesis and their therapeutic implications. Annu. Rev. Pathol. Mech. Dis. 2006;1:151–70. doi: 10.1146/annurev.pathol.1.110304.100113. [DOI] [PubMed] [Google Scholar]
- Smith DH, Nakamura M, McIntosh TK, Wang J, Rodriguez A, et al. Brain trauma induces massive hippocampal neuron death linked to a surge in beta-amyloid levels in mice overexpressing mutant amyloid precursor protein. Am. J. Pathol. 1998;153:1005–10. doi: 10.1016/s0002-9440(10)65643-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon B, Koppel R, Frankel D, Hanan-Aharon E. Disaggregation of Alzheimer beta-amyloid by site-directed mAb. Proc. Natl. Acad. Sci. USA. 1997;94:4109–12. doi: 10.1073/pnas.94.8.4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon B, Koppel R, Hanan E, Katzav T. Monoclonal antibodies inhibit in vitro fibrillar aggregation of the Alzheimer beta-amyloid peptide. Proc. Natl. Acad. Sci. USA. 1996;93:452–55. doi: 10.1073/pnas.93.1.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamura Y, Hamajima K, Matsui K, Yanoma S, Narita M, et al. The F(ab)'2 fragment of an Abeta-specific monoclonal antibody reduces Abeta deposits in the brain. Neurobiol. Dis. 2005;20:541–49. doi: 10.1016/j.nbd.2005.04.007. [DOI] [PubMed] [Google Scholar]
- Towfighi A, Greenberg SM, Rosand J. Treatment and prevention of primary intracerebral hemorrhage. Semin. Neurol. 2005;25:445–52. doi: 10.1055/s-2005-923538. [DOI] [PubMed] [Google Scholar]
- Urushitani M, Ezzi SA, Julien JP. Therapeutic effects of immunization with mutant superoxide dismutase in mice models of amyotrophic lateral sclerosis. Proc. Natl. Acad. Sci. USA. 2007;104:2495–500. doi: 10.1073/pnas.0606201104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh DM, Klyubin I, Fadeeva JV, Cullen WK, Anwyl R, et al. Naturally secreted oligomers of amyloid beta protein potently inhibit hippocampal long-term potentiation in vivo. Nature. 2002;416:535–39. doi: 10.1038/416535a. [DOI] [PubMed] [Google Scholar]
- Walsh DM, Selkoe DJ. Deciphering the molecular basis of memory failure in Alzheimer's disease. Neuron. 2004;44:181–93. doi: 10.1016/j.neuron.2004.09.010. [DOI] [PubMed] [Google Scholar]
- White AR, Enever P, Tayebi M, Mushens R, Linehan J, et al. Monoclonal antibodies inhibit prion replication and delay the development of prion disease. Nature. 2003;422:80–83. doi: 10.1038/nature01457. [DOI] [PubMed] [Google Scholar]
- Wilcock DM, DiCarlo G, Henderson D, Jackson J, Clarke K, et al. Intracranially administered anti-Abeta antibodies reduce beta-amyloid deposition by mechanisms both independent of and associated with microglial activation. J. Neurosci. 2003;23:3745–51. doi: 10.1523/JNEUROSCI.23-09-03745.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcock DM, Munireddy SK, Rosenthal A, Ugen KE, Gordon MN, et al. Microglial activation facilitates Abeta plaque removal following intracranial anti-Abeta antibody administration. Neurobiol. Dis. 2004a;15:11–20. doi: 10.1016/j.nbd.2003.09.015. [DOI] [PubMed] [Google Scholar]
- Wilcock DM, Rojiani A, Rosenthal A, Subbarao S, Freeman MJ, et al. Passive immunotherapy against Abeta in aged APP-transgenic mice reverses cognitive deficits and depletes parenchymal amyloid deposits in spite of increased vascular amyloid and microhemorrhage. J. Neuroinflamm. 2004b;1:24. doi: 10.1186/1742-2094-1-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


