Abstract
Background
Previous research indicates that many patients with hypertension ran out of medications and had difficulties getting refills immediately after Hurricane Katrina. The extended effect of Hurricane Katrina on antihypertensive medication adherence is not well characterized.
Methods
Data were analyzed for 2194 participants who completed the baseline survey for the Cohort Study of Medication Adherence among Older Adults between August 2006 and September 2007. Based on pre-Katrina zip codes, the study population was categorized into high and low affected areas. Low medication adherence was defined as a score less than 6 on the 8-item Morisky Medication Adherence Scale.
Results
Prevalence of low adherence was similar among participants living in high and low affected areas. Low medication adherence was similar for participants with greater than or less than 25% of the residence damaged by Hurricane Katrina and for participants with and without symptoms of post-traumatic stress disorder. In high affected areas, non-significant associations were present for those who had moved since the storm and those with a friend or immediate family member who had died in the month following the storm. These factors were not associated with low medication adherence in low affected areas. In both high and low affected areas, lower scores on the hurricane coping self-efficacy scale were associated with low medication adherence (p <0.05).
Conclusions
The effect of Hurricane Katrina on patient adherence to antihypertensive medication was limited in the second year following the storm. Intrinsic patient factors, such as low coping self-efficacy, remain important factors associated with low adherence.
Keywords: medication adherence, hypertension, Hurricane Katrina
Introduction
Hurricane Katrina made landfall on August 29, 2005 affecting a large area of southeastern Louisiana including the densely populated areas of New Orleans and its surrounding parishes. Over 1 million residents were displaced, and those returning to the area face many challenges with recovery efforts that will last for years.
Data from the Centers for Disease Control and Prevention indicate that over 200,000 people in the area impacted by the storm had hypertension [1]. Studies conducted immediately after Katrina report that patients with chronic diseases suffered from several problems related to medication adherence [2, 3]. Although the long recovery period following Hurricane Katrina may continue to affect patients’ adherence to their medication, few data are available on the extended effects of a disaster on medication adherence. Older individuals with hypertension comprise a unique group for whom responses to disasters are not well described. Therefore, we examined the association of storm- and recovery-related factors with antihypertensive medication adherence among older adults from southeastern Louisiana 1 to 2 years following Hurricane Katrina. To do so, we analyzed data from the baseline survey of the Cohort Study of Medication Adherence in Older Adults (CoSMO).
Methods
Study Population
Potential participants for CoSMO were identified using the administrative databases of a large managed care organization that provides insurance for patients’ healthcare in southeastern Louisiana. Inclusion criteria were as follows: adults 65 years of age and older with valid contact information, English-speaking, no cognitive impairment, current enrollment in the managed care organization with at least 2 years of continuous enrollment, community-dwelling, diagnosis of hypertension, current prescription for antihypertensive medication, no current diagnosis of or current treatment for malignancy (other than skin cancer), and able to complete the telephone survey (e.g., not hard of hearing or too sick to participate). From August 2006 through September 2007, 4473 eligible individuals with valid contact information were asked to participate in the survey study; 2279 refused and 2194 were successfully recruited and enrolled into CoSMO. Those who refused to participate were more likely to be male (50.4% versus 41.5% of participants, p<0.01), white (84.5% versus 68.8% of participants, p<0.01), and older (76.3 years versus 74.5 years for participants, p<0.01). There were no differences in participation rates between people living in high and low affected areas (p>0.05). The CoSMO study was approved by the Institutional Review Board of Ochsner Clinic Foundation. All participants provided verbal informed consent prior to completing the study questionnaire.
Data Collection
Baseline data for CoSMO were collected through a telephone interview conducted by trained and certified research staff using a standardized script and survey. Of relevance to the current analysis, the study interview included questions on socio-demographics, participants’ experiences following Hurricane Katrina, and medication adherence.
Socio-demographics
Participants were asked their age, gender, and race-ethnicity. The highest education level each participant achieved was ascertained, and participants were categorized as having less than or some high school education, being a high school graduate or having some college, or being a college graduate. Additionally, marital status was determined and participants were categorized as being currently married or not.
Hurricane-related factors
Participants’ experiences with and responses to Hurricane Katrina were assessed through a disaster-experience survey designed for the current study, the Hurricane Coping Self-Efficacy (HCSE) scale and the post-traumatic stress disorder (PTSD) CheckList – Civilian Version (PCL-17). Using the zip code for each participant’s residence before Hurricane Katrina, recorded in the managed care organization’s administrative databases, we categorized participants as residing in high or low affected areas. Parishes (counties) encompassing the greater New Orleans area including Orleans parish and 4 adjacent parishes were defined as high affected by Hurricane Katrina and the remaining parishes as low affected.
Participants were asked about the percentage of their residence that was damaged by Hurricane Katrina and the aftermath of the storm. To capture the interruption of their lives caused by the storm, participants were asked whether they were living in the same residence as before the storm. Additionally, participants were asked whether an immediate friend or family member died within 1 month of Hurricane Katrina.
Post-Traumatic Stress Disorder
The PCL-17 scale has been described in detail previously [4]. In brief, this scale consists of 17 items, which are combined into 3 sub-scales (5 items assessing ‘intrusion/re-experiencing,’ 7 items assessing ‘avoidance,’ and 5 items assessing ‘hyperarousal’), that address continuing psychological problems that people may experience in the aftermath of a disaster or other traumatic event. Response options to each question are ‘not at all’, ‘a little bit’, ‘moderately’, ‘quite a bit’, and ‘extremely’. A symptom was deemed present when an item was reported as being experienced moderately, quite a bit, or extremely. PTSD was defined using the Diagnostic and Statistical Manual IV criteria as follows: at least 1 symptom of intrusion/re-experiencing (e.g., repeated dreams or images of the storm; Criterion B), at least 3 symptoms of avoidance/numbing (e.g., avoiding thinking or talking about the storm; Criterion C), and at least 2 symptoms of hyperarousal (e.g., feeling jumpy or easily startled; Criterion D) [5].
Hurricane Coping Self-Efficacy scale
The HCSE scale was developed after Hurricanes Andrew and Opal [6], and its use has been validated following Hurricane Katrina [7]. The version of the HCSE used in the current study is comprised of 10 items that address a person’s ability to perform day-to-day tasks and cope with psychological stresses following a hurricane. Responses are scored on a 7-point Likert scale, with 1 anchored at ‘Not at all capable,’ 4 being ‘Moderately capable,’ and 7 being ‘Totally capable’. Scores for the 10 items are summed resulting in a HCSE score range from 10–70, with higher scores indicating a greater perceived ability to cope with the aftermath of the hurricane. For the current analysis, HCSE scores were categorized into tertiles using population cut-points.
Medication Adherence
Self-reported medication adherence was ascertained using the 8-item Morisky Medication Adherence Scale [8]. This adherence measure was designed to facilitate the identification of barriers to and behaviors associated with adequate adherence to chronic medications. The scale has been determined to be reliable (α= 0.83), associated with blood pressure control in participants with hypertension (p-value<0.05) [8], and has high concordance with antihypertensive medication pharmacy fill rates [9]. Scores can range from 0 to 8. Established cut-points were determined based on associations with blood pressure control to facilitate use of the scale in clinical practice [8]. As has been done previously [8, 9], low adherence was defined in the current study as scores less than 6.
Statistical Analysis
Separate analyses were conducted for participants from high and low affected areas. Participant characteristics including demographics, Hurricane Katrina- related factors together with symptoms of PTSD and HCSE, and low medication adherence were calculated. The statistical significance of differences in these characteristics for participants from high and low affected areas was determined, after adjustment for age, gender, and race using maximum likelihood methods. The prevalence of low adherence was calculated by hurricane-related factors, with the statistical significance of differences determined after age, gender, race adjustment. Multivariable log binomial regression models, adjusted for age, gender, race, education and marital status, were used to determine the association of Hurricane Katrina-related factors with low medication adherence. In secondary analyses, the associations between Hurricane Katrina-related factors and low medication adherence were assessed for white and black CoSMO participants, separately. All statistical analyses were performed using SAS version 9.1.3 (Cary, NC).
Results
Overall, 69% of participants enrolled in CoSMO were living in high affected areas when Hurricane Katrina made landfall. Participants living in high affected areas were older and more likely to be women, white and not married compared to their counterparts in low affected area (Table 1). The percent of participants with greater than 25% damage to their residence, living in a different residence than before the storm, who experienced the death of a friend or immediate family member in the month following Hurricane Katrina and had symptoms of PTSD was higher in the high affected areas. The distribution of HCSE scale scores were not significantly different in high and low affected areas. The prevalence of low adherence was similar among participants living in high and low affected areas.
Table 1.
Demographic characteristics and prevalence of Hurricane Katrina-related factors.
| Mean (SD) or Percentage
|
p-value† | ||
|---|---|---|---|
| High affected area (N=1516) | Low affected area (N=678) | ||
| Age, years | 75.2 (5.6) | 74.6 (5.4) | 0.02 |
| Women | 61.4 | 51.9 | <0.01 |
| White | 72.7 | 61.6 | <0.01 |
| Education | |||
| Less than high school | 20.0 | 22.4 | |
| High school graduate or some college | 58.8 | 56.9 | 0.36 |
| College graduate or more | 21.2 | 20.7 | |
| Not married | 45.2 | 38.6 | 0.04 |
| Had >25% damage to residence | 45.9 | 14.9 | <0.01 |
| Living in a different residence than before the storm | 23.2 | 8.7 | <0.01 |
| Death of a friend or immediate family member | 21.9 | 11.4 | <0.01 |
| Symptoms of PTSD present | 6.7 | 3.1 | <0.01 |
| Hurricane Coping Self-Efficacy Score | |||
| ≥65 | 30.8 | 33.8 | |
| 56 – 64 | 32.9 | 29.6 | 0.34 |
| <56 | 36.3 | 36.6 | |
| Low Morisky Medication Adherence Score | 13.3 | 16.1 | 0.19 |
Abbreviation: SD – standard deviation, PTSD – Post-traumatic stress disorder
All p-values (except age, gender, and race) are adjusted for age, gender, and race
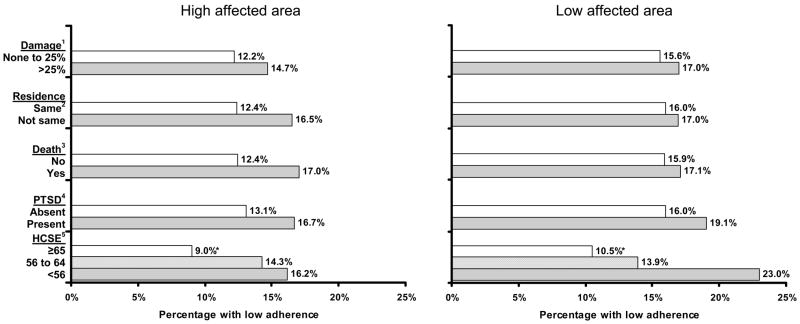
In high affected areas, low adherence was more common among participants with each of the Hurricane Katrina-related exposures. However, the only factor that was statistically significantly associated with lower adherence after age, gender, race adjustment was lower HCSE scores (Figure 1). With the exception of HCSE, none of the Hurricane Katrina-related factors studied were associated with low antihypertensive medication adherence in the low affected areas.
Figure 1. Prevalence of low adherence by different Hurricane Katrina-related factors.
Damage = Damage to residence after Hurricane Katrina;
Residence = Current residence same as before the storm;
Death = Death of a friend or immediate family member;
PTSD = Post traumatic stress disorder;
HCSE = Hurricane coping self-efficacy score
After adjustment for age, gender, race, education, and marital status, the prevalence ratios of low adherence associated with living in a different residence than before the storm and having a friend or immediate family member die in the month following the storm were 1.30 and 1.33, respectively, (Table 2) for participants living in high affected areas when Hurricane Katrina made landfall. Additionally, lower HCSE scores were significantly associated with progressively higher prevalence ratios of low medication adherence in both the high and low affected areas.
Table 2.
Adjusted prevalence ratios of low adherence by different Hurricane Katrina-related factors for CoSMO participants from high and low affected areas.
| High affected Area | Low affected Area | |||
|---|---|---|---|---|
| PR (95% CI) | p-value | PR (95% CI) | p-value | |
| Damage to residence >25% vs. none to 25% damage | 1.10 (0.84, 1.45) | 0.47 | 0.85 (0.52, 1.39) | 0.51 |
| Living in a different vs. same residence as before storm | 1.30 (0.98, 1.72) | 0.07 | 0.97 (0.54, 1.76) | 0.93 |
| Friend/immediate family member died vs. didn’t die | 1.33 (1.00, 1.77) | 0.05 | 0.92 (0.54, 1.56) | 0.75 |
| Symptoms of PTSD present vs. absent | 1.17 (0.74, 1.83) | 0.51 | 1.03 (0.42, 2.52) | 0.95 |
| Hurricane Coping Self-Efficacy Score | ||||
| ≥65 | 1.00 (ref.) | 1.00 (ref.) | ||
| 56 to 64 vs. ≥65 | 1.55 (1.08, 2.23) | <0.01 | 1.25 (0.75, 2.09) | <0.01 |
| <56 vs. ≥65 | 1.73 (1.22, 2.46) | 1.91 (1.21, 3.01) | ||
Adjusted for age, race, gender, education and marital status.
Abbreviation: PR = Prevalence ratio; CI = Confidence Interval
Secondary Analyses
In both high and low affected areas, blacks were more likely than whites to have had greater than 25% damage to their residence, have relocated after the storm, have experienced the death of a friend or a family member, and have had symptoms of PTSD. In high affected areas, blacks with >25% damage to their residence and living in a different residence than before the storm were 1.55 (95% CI: 0.90 – 2.68) and 1.47 (95% CI: 0.94 – 2.28) times more likely to have low medication adherence. In addition, blacks in high affected areas with HCSE scores in the lowest tertile were 2.02 (95% CI: 1.07 – 3.81) times more likely to have low medication adherence compared to blacks in high affected areas with HCSE scores in the highest tertile. With the exception of HCSE (where whites living in high affected areas with HCSE scores in lowest tertile were 2.52 (95% CI: 1.34 – 4.76) times more likely to have low medication adherence compared to whites with HCSE scores in highest tertile), no association was present between Hurricane Katrina-related factors and low medication adherence among whites. Tests for interaction assessing differences in the associations of Hurricane Katrina-related factors with low medication adherence across race groupings were not statistically significant (each p value >0.10).
Discussion
The current study examined the effects of several Hurricane Katrina-related exposures on antihypertensive medication adherence 1 to 2 years following the storm in a population of older, insured individuals in southeast Louisiana. Among participants taking antihypertensive medication, the prevalence of low adherence was similar among participants from high versus low affected areas. In high affected areas, no association with low adherence was present for the degree of damage to participants’ residences and the presence of symptoms of PTSD. In participants in high affected areas, only minimal, marginally significant associations with low adherence were present for those living in a different residence than before the storm or experiencing the death of a friend or family member. In participants in low affected areas, no association with low adherence was present with these factors. A strong, graded association between lower scores on the HCSE scale and low medication adherence was present among participants from high and low affected areas.
In a previous study by our group, several challenges encountered by patients with hypertension in the immediate aftermath of Hurricane Katrina were identified [2]. Many patients did not bring their medication when they evacuated, they ran out of medications, and they had difficulty getting refills. These are clearly important concerns that require diligent planning efforts and the need for physicians to be aware of the challenges patients may encounter immediately following a disaster. Furthermore, Kessler and colleagues found 31.2% of Katrina survivors had hypertension with 21.7% of these adults reported cutting back on antihypertensive treatment in the post-disaster period [3]. However, few data are available on the extended impact of a region-wide disaster on medication adherence in older individuals with chronic diseases.
In both high and low affected areas 1 to 2 years after the hurricane, lower scores on the HCSE scale were associated with low adherence. The HCSE scale was designed to capture how individuals respond to the challenges of recovery following a hurricane, which may reflect how individuals respond to any challenging situation [6]. However, scores on the HCSE scale may also reflect a patient’s inherent disposition. Further research is needed to understand the degree to which scores on this scale represent responses to the natural disaster and its aftermath versus coping self-efficacy in general. Nevertheless, it may be important to consider intrinsic patient factors, including low coping self-efficacy, as important factors associated with low adherence in extended post-disaster situations.
Selected Hurricane Katrina-related factors (i.e. death of a family member or friend, change in residence, and HCSE) may have prolonged effects on antihypertensive medication adherence. Low medication adherence is a potential factor related to poor blood pressure control. Over 10% of the current study population had low adherence. The prevalence of low medication adherence has varied considerably in previous studies, often depending on definitions used and the populations studied. However, investigators consistently report that low medication adherence is common [10, 11, 12]. In non-disaster settings, younger adults [13, 14] and blacks [13, 15] are more likely to have low medication adherence. Additionally, depression, low social support, use of alternative therapies, and lack of lifestyle modifications have been found to be associated with low adherence [16, 17]. Living in a different residence than before Hurricane Katrina and death of a family member or friend within 1 month of the disaster had a modest influence on low adherence in our study conducted 1 to 2 years following Hurricane Katrina. These factors may be important to consider for chronic disease management in the context of antihypertensive medication adherence in patients with uncontrolled blood pressure.
The results of the current analysis need to be interpreted in the context of its limitations. The most notable limitation is the cross-sectional study design. Although CoSMO is a longitudinal cohort study, the baseline interview was conducted 1 to 2 years after Hurricane Katrina made landfall. Therefore, we were unable to assess changes in medication adherence from before to after Hurricane Katrina or from the first to second year following the storm. Another limitation is the reliance on a screening tool for assessing PTSD. While the PCL-17 is well-validated and has been used in many studies, it does not provide a formal diagnosis of PTSD. However, psychiatric interviews to assess PTSD were not feasible in the current study. Additionally, data on prior trauma and stressful events that may have contributed to patients developing PTSD were not collected. Despite the advantages of assessing medication adherence by self-report (e.g., simplicity, speed, and viability of use), there are potential shortcomings of self-report medication adherence including reliance on recall and social desirability with a tendency to overestimate adherence [17]. More work is required to validate the Morisky Medication Adherence Scale in demographically diverse populations. Finally, the current study was limited to older adults with health insurance from a single managed care organization. Those refusing to participate were more likely to be older, white, and women. Low medication adherence is more common among younger adults and at lower socio-economic status. Therefore, caution should be taken in generalizing these findings to younger age groups and those without health insurance.
Despite these limitations, the current study maintains several strengths. The large sample size and inclusion of patients from a large geographic area in southern Louisiana allowed us to perform separate analyses for individuals living in high and low affected areas. All interviews were conducted following a structured telephone script by trained interviewers. Additionally, several domains assessing participants’ experiences during and after Hurricane Katrina were captured.
Conclusion
Compared to the acute effects of Hurricane Katrina on medication adherence immediately following the storm, the extended effects 1 to 2 years after Hurricane Katrina made landfall were minimal. Intrinsic patient factors, such as poor coping skills, were associated with low adherence. These factors may need to be considered in the management of patients with chronic diseases who are also dealing with prolonged recovery following a disaster.
Acknowledgments
Source of Support: The project described was supported by Grant Number R01 AG022536 from the National Institute on Aging. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
References
- 1.Ford ES, Mokdad AH, Link MW, et al. Chronic disease in health emergencies: in the eye of the hurricane. Prev Chronic Dis. 2006;3(2):A46. [PMC free article] [PubMed] [Google Scholar]
- 2.Krousel-Wood MA, Islam T, Muntner P, et al. Medication Adherence in Older Patients with Hypertension after Hurricane Katrina: Implications for clinical practice and disaster management. American Journal of Medical Sciences. 2008 doi: 10.1097/MAJ.0b013e318180f14f. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler RC. Hurricane Katrina's impact on the care of survivors with chronic medical conditions. J Gen Intern Med. 2007;22(9):1225–30. doi: 10.1007/s11606-007-0294-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shapinsky AC, Rapport LJ, Henderson MJ, et al. Civilian PTSD scales: relationships with trait characteristics and everyday distress. Assessment. 2005;12(2):220–30. doi: 10.1177/1073191104273130. [DOI] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, D.C: American Psychiatric Association; 1994. [Google Scholar]
- 6.Benight CC, Ironson G, Durham RL. J Trauma Stress. 2. Vol. 12. 1999. Psychometric properties of a hurricane coping self-efficacy measure; pp. 379–86. [DOI] [PubMed] [Google Scholar]
- 7.Hyre AD, Benight CC, Muntner P, et al. Psychometric properties of the Hurricane Coping Self-Efficacy Measure following Hurricane Katrina. J Ner Mental Dis. 2008 doi: 10.1097/NMD.0b013e31817d016c. In Press. [DOI] [PubMed] [Google Scholar]
- 8.Morisky DE, Ang A, Krousel-Wood MA, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008 doi: 10.1111/j.1751-7176.2008.07572.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 9.Krousel-Wood MA, Islam T, Morisky DE, et al. Concordance of Self-Reported Medication Adherence by Pharmacy Fill in Patients with Hypertension. Poster presentation at AHA 48th Annual Conference on Cardiovascular Disease Epidemiology and Prevention; Colorado Springs, Colorado. March 14, 2008; abstract in press (Circulation 2008) [Google Scholar]
- 10.Jones JK, Gorkin L, Lian JF, et al. Discontinuation of and changes in treatment after start of new courses of antihypertensive drugs: a study of a United Kingdom population. Bmj. 1995;311(7000):293–5. doi: 10.1136/bmj.311.7000.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conlin PR, Gerth WC, Fox J, et al. Four-Year persistence patterns among patients initiating therapy with the angiotensin II receptor antagonist losartan versus other artihypertensive drug classes. Clin Ther. 2001;23(12):1999–2010. doi: 10.1016/s0149-2918(01)80152-1. [DOI] [PubMed] [Google Scholar]
- 12.McCombs JS, Nichol MB, Newman CM, et al. The costs of interrupting antihypertensive drug therapy in a Medicaid population. Med Care. 1994;32(3):214–26. doi: 10.1097/00005650-199403000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Monane M, Bohn RL, Gurwitz JH, et al. The effects of initial drug choice and comorbidity on antihypertensive therapy compliance: results from a population-based study in the elderly. Am J Hypertens. 1997;10(7 Pt 1):697–704. doi: 10.1016/s0895-7061(97)00056-3. [DOI] [PubMed] [Google Scholar]
- 14.Marentette MA, Gerth WC, Billings DK, et al. Antihypertensive persistence and drug class. Can J Cardiol. 2002;18(6):649–56. [PubMed] [Google Scholar]
- 15.Sharkness CM, Snow DA. The patient’s view of hypertension and compliance. Am J Prev Med. 1992;8(3):141–6. [PubMed] [Google Scholar]
- 16.Wang PS, Bohn RL, Knight E, et al. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17(7):504–11. doi: 10.1046/j.1525-1497.2002.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krousel-Wood M, Hyre A, Muntner P, et al. Methods to improve medication adherence in patients with hypertension: current status and future directions. Curr Opin Cardiol. 2005;20(4):296–300. doi: 10.1097/01.hco.0000166597.52335.23. [DOI] [PubMed] [Google Scholar]