Abstract
Affibody molecules are a new class of small targeting proteins based on a common threehelix bundle structure. Affibody molecules binding a desired target may be selected using phage-display technology. An Affibody molecule ZHER2:342 binding with subnanomolar affinity to the tumor antigen HER2 has recently been developed for radionuclide imaging in vivo. Introduction of a single cysteine into the cysteine-free Affibody scaffold provides a unique thiol group for site-specific labeling of recombinant Affibody molecules. The recently developed maleimido-CHX-A” DTPA was site-specifically conjugated at the C-terminal cysteine of ZHER2:2395-C, a variant of ZHER2:342, providing a homogenous conjugate with a dissociation constant of 56 pM. The yield of labeling with 111In was > 99% after 10 min at room temperature. In vitro cell tests demonstrated specific binding of 111In-CHX-A” DTPAZ2395-C to HER2-expressing cell-line SKOV-3 and good cellular retention of radioactivity. In normal mice, the conjugate demonstrated rapid clearance from all non-specific organs except kidney. In mice bearing SKOV-3 xenografts, the tumor uptake of 111In-CHX-A” DTPAZ2395-C was 17.3 ± 4.8 % IA/g and the tumor-to-blood ratio 86 ± 46 (4 h post-injection). HER2-exprssing xenografts were clearly visualized 1 h post-injection. In conclusion, coupling of maleimido-CHX-A” DTPA to cysteine-containing Affibody molecules provides welldefined uniform conjugate, which can be rapidly labeled at room temperature and provides high-contrast imaging of molecular targets in vivo.
Introduction
Progress in molecular tumor biology is a foundation for increasing specificity of cancer therapy by targeting of molecular structures, which are uniquely expressed or over-expressed on surface of cancer cells. Since such over-expression occurs only in a fraction of tumors, specific therapy has to be personalized, i.e. patients should be carefully stratified to optimize targeted therapy while avoiding over-or undertreatment. The use of radionuclide molecular imaging can be an important tool for detection of expression of a particular molecular target in the primary tumor and metastases of a patient. Successful molecular imaging depends on the availability of imaging agents that are capable of providing a specific and high contrast imaging of cancer-associated targets in vivo.
Three years ago, a pre-clinical evaluation of a new class of targeting proteins, Affibody molecules, was initiated (1-3). Affibody molecules are three helix bundle proteins, derived from staphylococcal protein A. Phage display enables selection of Affibody molecules with a low picomolar affinity (4). A small size, about 7 kDa, enables rapid tumor localization of Affibody molecules and their fast clearance from non-specific compartments. For example, the ZHER2:342 Affibody molecule, which binds HER21 antigen with an affinity of 22 pM (4), demonstrated clear visualization of murine xenografts at 1 h post-injection (pi) (5). Recently, Affibody molecules were developed against another tumor-associated target, EGFR2 (6–8).
Successful molecular imaging depends both on a targeting protein providing specific accumulation of radionuclide in the tumor, and on a label, i.e. a combination of a particular radionuclide and a linker that provides stable attachment to the targeting protein. The use of different labeling methods influences not only the stability of the attachment of the radionuclide to the targeting proteins, but also the charge and the lipophilicity of the conjugate, which may influence uptake in healthy tissues and the excretion route. Alternative labeling of Affibody molecules have previously been demonstrated to result in different biodistribution of the radioactivity (9-16). Different macrocyclic and acyclic chelators have been evaluated for labeling of Affibody molecules with the radionuclide 111In (T ½ = 2.8 days). Initial evaluation was done using isothiocyanate derivatives of DTPA3 (17), DOTA4 (15) and CHX-A” DTPA5 (18). Though all these conjugates demonstrated good targeting properties, isothiocyanate-mediated coupling to amino groups is not site-specific, and the labeled product presented as a distribution of conjugates with chelators at different positions and therefore potentially with different targeting properties. The use of peptide synthesis enabled production of a homogenous conjugate of the anti-HER2 Affibody molecule ZHER2:342 with DOTA attached site-specifically to the N-terminal amine (5). After labeling with 111In, this conjugate demonstrated excellent targeting of HER2-expressing xenografts in mice (5). However, a site-specific method for labeling of Affibody molecules made by recombinant production would be attractive.
One approach to site-specific labeling of recombinant Affibody molecules is based on the fact that is the protein lacks cysteines. Therefore, introduction of a single cysteine into the Affibody molecule provides unique thiol group, which can be use for site-specific labeling. Previously, this approach has been used for labeling of Affibody molecules with radiohalogens for in vivo imaging (9), and Oregon Green and horseradish peroxidase (HRP) for in vitro detection of HER2 (19). Recently, we reported the use of this approach for labeling of the anti-HER2 Affibody molecule ZHER2:2395-Cys (a variant of anti-HER2 Affibody molecule ZHER2:342, which contains a cysteine at C terminus) with 111In using a maleimidoderivative of DOTA (20). The resulting conjugate, 111In-DOTA-ZHER2:2395-C demonstrated a tumor-to-blood ratio similar to the ratio observed with the synthetic 111In-DOTA-ZHER2:342 conjugate in a murine xenograft model (5).
The semi-rigid acyclic chelator CHX-A” DTPA, which forms stable complexes with a number of radiometals of interest for radionuclide imaging, might be an alternative to DOTA for labeling of Affibody molecules. Amino-reactive derivatives of CHX-A” DTPA demonstrated suitability for labeling of proteins and peptides with 111In (21, 22). Of particular importance, the isothiocyanate derivative of CHX-A” DTPA provided the best tumor-toblood ratio among all non-site-specifically 111In-labeled Affibody conjugates (18). A thiolreactive derivative of CHX-A” DTPA, maleimido CHX-A” DTPA6, has recently been reported (23) and is now evaluated here for the site-specific conjugation and radiolabeling of Affibody molecules.
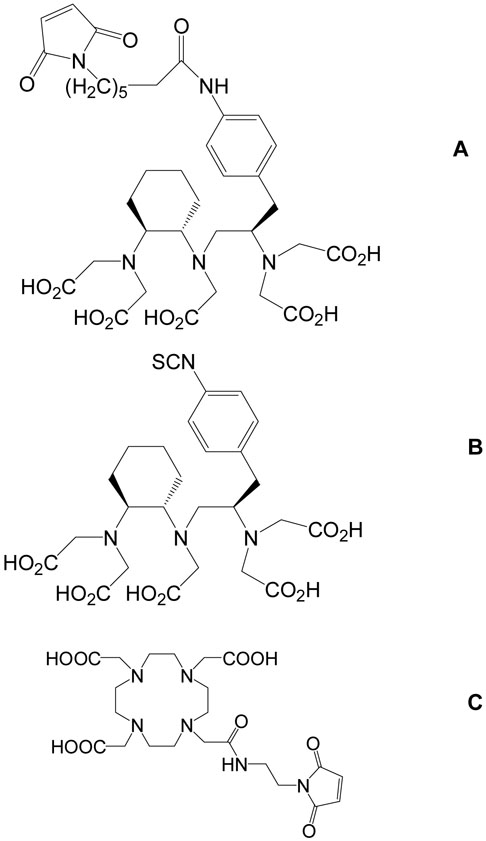
The goals of the study were a) to prepare a maleimido CHX-A” DTPA conjugate of anti-HER2 Affibody molecule ZHER2:2395-Cys; b) to evaluate targeting properties of the Affibody molecule ZHER2:2395 site-specifically labeled with 111In using maleimido CHX-A” DTPA (111In-CHX-A” DTPA-Z2395-C); and c) compare this product with ZHER2:2395 site-specifically labeled with DOTA (111In-DOTA-Z2395-C) and with ZHER2:342 non-specifically labeled using the isothiocyanate derivative of CHX-A” DTPA (111In-CHX-A” DTPA-Z342). The chelators used in this study are presented in Figure 1.
Figure 1.
Structures of maleimido-CHX-A” DTPA (A), CHX-A” DTPA (B), and maleimido-monoamine-DOTA (C).
Materials and methods
Material
A cysteine-containing variant of ZHER2:342, ZHER2:2395-C, and its derivatives DOTAZ2395-C and 111In-DOTA-Z2395-C were produced according to (20). MMA-DOTA and isothiocyanante-CHX-A”DTPA were purchased from Macrocyclics (Dallas, TX, USA). The maleimido CHX-A” DTPA was prepared as previously reported (23). A 111In-CHXA” DTPA-Z342 was produced and labeled according to (18). Purity and identity of all macromolecules and their conjugates was confirmed using high performance liquid chromatography with on line mass spectrometric detection, as described in the Instrumentation subsection. All purified proteins demonstrated a single peak with a mass, coinciding with the theoretically calculated with an accuracy of ± 1.5 Da, which is within the accuracy of the instrument. Buffers, such as 0.1 M phosphate buffered saline (PBS), pH 7.5, and 0.2 M ammonium acetate, pH 5.5, were prepared using common methods from chemicals supplied by Merck (Darmstadt, Germany). High-quality Milli-Q © water (resistance higher than 18 MΩ cm) was used for preparing solutions. Buffers, which were used for conjugation and labeling, were purified from metal contamination using Chelex 100 resin (Bio-Rad Laboratories, Richmond, CA, USA). NAP-5 size exclusion columns were from Amersham Biosciences, Uppsala, Sweden. [111In]indium chloride was purchased from Tyco. Silica gel impregnated glass fiber sheets for instant thin layer chromatography (ITLC™ SG) were from Gelman Sciences Inc. For cell studies, the HER2-expressing ovarian carcinoma cell line SKOV-3 (ATCC, purchased via LGC Promochem, Borås, Sweden), displaying approximately 1.2×106 HER2 receptors per cell (24) was used. The cell line was cultured in McCoy's medium (Flow Irvine, UK). The medium was supplemented with 10% fetal calf serum (Sigma, USA), 2 mM L-glutamine and PEST (penicillin 100 IU/mL and 100 μg/mL streptomycin), all from Biokrom Kg, Germany. Ketalar [ketamine] (50 mg/mL, Pfizer, NY, USA), Rompun [xylazin] (20 mg/mL, Bayer, Leverkusen, Germany), Heparin (5000 IE/mL, Leo Pharma, Copenhagen, Denmark) were obtained commercially. Data on cellular uptake and biodistribution were analyzed by unpaired, two-tailed t-test using GraphPad Prism (version 4.00 for Windows GraphPad Software, San Diego California USA) in order to determine any significant differences (P<0.05).
Instrumentation
The radioactivity was measured using an automated gamma-counter with 3-inch NaI(Tl) detector (1480 WIZARD, Wallac Oy, Turku, Finland). 111In was measured with the use of both photopeaks and summation peak (energy setting from 140 to 507 keV). SDS-PAGE analysis was performed using NuPAGE 4-12 % Bis-Tris Gel (Invitrogen) in MES buffer (200 V constant). Distribution of radioactivity along the ITLC strips and SDS-PAGE gels was measured on a Cyclone™ Storage Phosphor System (further referred to as PhosphorImager) and analyzed using the OptiQuant™ image analysis software. Cells were counted using electronic cell counter (Beckman Coulter). Affibody samples were analyzed by high performance liquid chromatography with on line mass spectrometric detection (Agilent 1100 HPLC/MSD). The mass spectrometer consisted of a single quadropole mass analyzer with an electrospray ionization (ESI) interface used in positive ion mode. The software used for analysis and evaluation was Chemstation Rev. B.02.01. (Agilent Technologies). For HPLC-MS analysis, 10 μL sample (1:1 dilution with solution A: 0.1% TFA in Milli-Q © water) was loaded onto a Zorbax 300SB-C8 (2.1×150 mm, 3.5 μm) RPC-column equilibrated with solution A with 10% solution B (0.1% TFA in acetonitrile) at a flow-rate of 0.5 mL/min. After 2 min, the proteins were eluted using a linear gradient, 10-70% solution B in 15 min. For purification, a semi-preparative column Zorbax 300SB-C8, 9.4×250 mm, 5 μm) was used. The flow rate was 5 mL/min and fractions were collected according to the peak detect settings specified in the chromatographic method.
Preparation and characterization of 111In-CHX-A” DTPA-Z2395-C
Conjugation of maleimido CHX-A” DTPA to ZHER2:2395 was performed with calculated chelator to protein ratios of 1:1, 2:1 and 3:1. To reduce any spontaneously forming disulfide bonds, 0.5 mL of ZHER2:2395 (stock solution, 3.91 mg/mL) was incubated during 2 h in 30 mM DTT at 37±);C. After incubation, the reduced ZHER2:2395 was purified using NAP-5 column pre-equilibrated and eluted with degassed 0.02 M ascorbic acid. Three aliquots of eluant (concentration 2 mg/mL), 200 μL each, were used for coupling. Aliquots were mixed with a pre-calculated amount of 1 M NH4OAc, pH 5.5, (degassed by sonication) and with freshly prepared solution of maleimido CHX-A” DTPA (1 mg/mL in degassed Milli-Q water). The vial was filled with argon gas, and the mixture was incubated at 37°C for 18 h (overnight). After the end of incubation, the reaction mixture was analyzed using HPLC-MS, as described in instrumentation. Purification of conjugates was performed using semi-preparative HPLC, and buffer was changed to 0.2 M NH4OAc, pH 5.5, using NAP-5 column. Exact concentration of protein was determined by amino acid analysis (Amniosyraanalyscentralen, Uppsala, Sweden). Affinity of conjugate to HER2 was measured using a Biacore 2000 instrument (Biacore, Uppsala, Sweden) according to the method described earlier (Orlova et al., 2007 CR).
For a labeling, 180 μL of conjugate solution (containing 20 μg of conjugate in 0.2 MNH4OAc, pH 5.5) was mixed with 25 μL of 111In in 0.05 M HCl (18 MBq). The mixture was incubated at room temperature. At 10, 20 and 30 min after the start of incubation, a small (0.8 μL) aliquot was taken from reaction mixture and analyzed using ITLC SG eluted with 0.2 M citric acid. To confirm stable chelation, an aliquot of solution was incubated in 500-fold molar excess of EDTA for 4 h, and then analyzed using ITLC. This stability test was repeated twice.
Binding and processing of 111In-CHX-A” DTPA-Z2395-C by HER2-expressing SKOV-3 cell line in vitro
To evaluate cellular processing of 111In-CHX-A” DTPA-Z2395-C, the labeled conjugate was added in 1 mL complete medium to a series of Petri dishes containing 250000 cells at an equimolar ratio of Affibody molecules to HER2 receptors. Dishes were incubated for 1 h at 4°C, and the incubation medium was removed. Cells were washed 3 times with ice-cold serum-free medium and, after addition of 1 mL complete medium, cell dishes were incubated further at 37°C. At designed times of incubation (0, 0.5, 1, 1.5, 2, 3, 4, 8 and 24 h), one set of 3 dishes was analyzed for cell-associated radioactivity. Medium was collected, the cells were washed 3 times with ice-cold serum-free medium and treated with 0.5 mL 4 M urea solution in 0.2 M glycine buffer, pH 2.0, with 0.15 M NaCl for 5 min at 4°C (according to method described in (25)). Solution was collected and cells were additionally rinsed with 0.5 mL of the same buffer. The radioactivity, which was removed by acid wash, was considered as membrane bound fraction. After addition of 0.5 mL 1 M NaOH solution, the cells were incubated for 1 h at 37°C and the solution was collected. Cell dishes were subsequently rinsed with 0.5 mL of alkaline solution. Pooled alkaline fractions represented internalized conjugate. The radioactivity content of the samples was measured using the automated gamma-camera.
To confirm that binding of conjugate was receptor-specific, a 100-fold excess of non-labeled Affibody molecules was added 5 min before the labeled ones to 3 culture dishes and cell-bound radioactivity was measured after treatment with trypsin-EDTA solution (0.25% trypsin, 0.02% EDTA in buffer, Biochrom AG, Berlin, Germany).
To assess the fraction of the conjugate that dissociated intact from the cells, the media was collected after 1, 4, 8 and 24 h of incubation at 37°C and analyzed using disposable NAP-5 size-exclusion columns (cut-of size 5 kDa) pre-equilibrated with 2.5 % bovine serum albumin solution in PBS. Separation on high and low molecular weight fractions was done according to the manufacture descriptions. Radioactivity in a high molecular weight fraction was considered intact dissociated conjugate.
Animal studies
The animal experiments were planned and performed in accordance with the national regulation on laboratory animals' protection. The animal study plans have been approved by the local Ethics Committee for Animal Research in Uppsala. Biodistribution studies in non-tumor bearing mice were performed in female immunocompetent Naval Medical Research Institute (NMRI) mice. In all experiments on tumor bearing mice, female outbreed BALB/c nu/nu mice were used. The mice were kept using standard diet, bedding and environment with free access to food and water. All mice were acclimatized for one week at the Rudbeck Laboratory animal facility before any experimental procedures. Xenografts of HER2-expressing SKOV-3 ovarian carcinoma cell line, 107 SKOV-3 cells per animal, were subcutaneously implanted in right hind leg.
In each biodistribution experiment, mice were randomized into groups of four. Animals were injected intravenously (tail vein) with 1 μg conjugate (50 kBq) in 100 μL PBS. At the predetermined time point, a mixture of Ketalar-Rompun (20 μL of solution per gram body weight; Ketalar: 10 mg/mL; Rompun: 1mg/mL) was intraperitonealy injected and the mice were euthanized by a heart puncture using a 1 mL syringe, pre-washed with diluted heparin (5000 IE/mL). Blood as well as lung, liver, spleen, kidneys, tumor (from xenografted mice), samples of muscle and bone, gastrointestinal tract (with its content) and remaining carcass were collected in pre-weighed plastic vials. Organs and tissue samples were weighed and measured for radioactivity using an automatic gamma counter. The tissue uptake values were calculated as percent injected activity per gram tissue (% IA/g), except for the gastrointestinal tract and the carcass, which were calculated as % IA per whole sample. The radioactivity in the gastrointestinal tract with its content was used as a measure of hepatobiliary excretion.
Biodistributions of the three differentially labeled constructs (two site-specifically labeled at C-terminal, 111In-CHX-A” DTPA-Z2395-C and 111In-DOTA-Z2395-C, and one labeled using amino-directed chemistry, 111In-CHX-A” DTPA-Z342) were determined in NMRI mice at 4 h and 24 h p.i.
Tumor targeting and biodistribution of 111In-CHX-A” DTPA-Z2395-Cat 1, 4 and 24 h p.i. were studied in immunodeficient mice bearing SKOV-3 xenografts. To confirm that xenograft accumulation of 111In-CHX-A”DTPA-Z2395-C was HER2-specific, receptors in one additional group of mice were pre-saturated by subcutaneous injection of 520 μg of unlabelled ZHER2:342 45 min prior to injection of radiolabelled Affibody molecule. Mice in this group were sacrificed 4 h after injection. For comparison, biodistributions of 111In-DOTA-Z2395-C and 111In-CHX-A” DTPA-Z342 were studied in the same batch of SKOV-3-grafted mice, 4 h p.i.
For gamma camera imaging, four SKOV-3 xenograft bearing mice were injected with 2.7 MBq 111In-CHX-A” DTPA-Z2395-C (amount of protein 3 μg). One and four hours post injection, two animals were sacrificed by overdosing Ketalar/Rompun followed by cervical dislocation. After euthanasia, the urine bladders were excised and cadavers were stored on ice until imaging. Imaging was performed at the department of Nuclear Medicine at Uppsala University Hospital using a Millennium GE gamma camera equipped with a medium energy general purpose (MEGP) collimator. Static images (10 min), obtained with a zoom factor of 2, were digitally stored in a 256×256 matrix. The evaluation of the images was performed using a Hermes system (Hermes Medical Solutions, Stockholm). In each animal, a region of interest (ROI) was drawn around the tumor. The same region was copied to a contralateral thigh. Tumor-to-contralateral thigh ratios were calculated based on total counts in the ROIs.
Results
Preparation and characterization of 111In-CHX-A” DTPA-Z2395-C
HPLC-MS analysis demonstrated that 83% of the ZHER2:2395 Affibody molecules were conjugated with chelator, when coupling of maleimido-CHX-A” DTPA was performed using equimolar amount of chelator and protein. When maleimido-CHX-A” DTPA was used in a 2- or 3-fold molar excess, no unconjugated Affibody molecules were detected after incubation during 18 h at 37°C, demonstrating that a uniform 1:1 product was produced. Semi – preparative HPLC using Zorbax 300SB-C8 column provided complete separation from non-conjugated chelator.
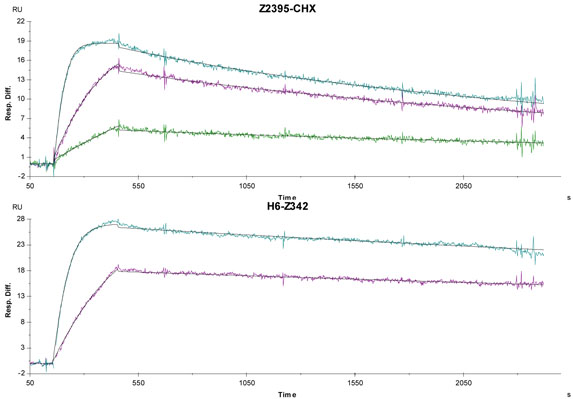
Measurement of the binding kinetics of CHX-A” DTPA-Z2395-C to extracellular domain of HER2 (Figure 2) suggested that the association rate (ka) was 7.4 ± 0.5 × 106 M−1s−1 (an average of two measurements ± maximum error of measurement), and dissociation rate 4.1 ± 0.2 & 10− 4 s−1, resulting in an equilibrium dissociation constant of 56 ± 6.5 pM. Affinity measurement of His6-ZHER2:342 gave a value of 29 pM, which is in a good agreement with previously published data (22 pM (4)). Apparently, coupling of maleimido-CHX-A” DTPA had no major negative effect on the affinity of the conjugate towards HER2.
Figure 2.
Biosensor binding study using surface plasmon resonance. Sensorgrams obtained after injection of the CHX-A” DTPA-Z2395-C conjugate (upper panel) and parental His6-ZHER2:342 (lower panel) over a sensor chip flow-cell surface containing amine-coupled HER2-Fc fusion protein. CHX-A” DTPA-Z2395-C was injected at concentrations of 5 nM, 1.2 nM and 0.31 nM. His6-ZHER2:342 was injected at concentrations of 6 nM and 1.5 nM. Experimental curves were fitted to a 1:1 (Langmuir) binding model with correction for mass transfer effects.
Labeling performed at specific radioactivity of 0.9 MBq/μg (6.3 GBq/μmol) provided nearly quantitative yield (99.7 ± 0.3 %) after 10 min. Extension of the labeling time to 30 min did not increase the labeling yield. Incubation with 500-fold molar excess of EDTA during 4 h did not decrease conjugate-associated radioactivity, indicating that the labeling was fully mediated by CHX-A” DTPA, not by any weak chelating pocket that might be formed by amino acid residues.
Binding and processing of 111In-CHX-A” DTPA-Z2395-C by HER2-expressing SKOV-3 cell line in vitro
Binding of 111In-CHX-A” DTPA-Z2395-C to HER2-expressing SKOV-3 cells was specific, since pre-saturation of receptors with a 100-fold excess of non-labeled Affibody molecules prevented binding nearly completely, from 35 ± 0.5 to 0.06 ± 0.01 % of added radioactivity (p<0.0001).
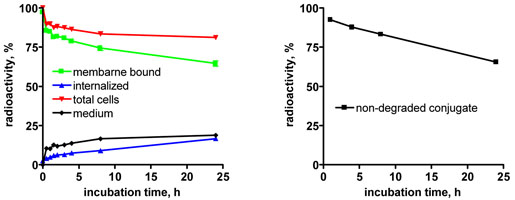
The results of cellular processing experiments indicated that retention of the conjugate was good, 81 ± 0.5% of radioactivity was still associated with cells 24 h after change of the media (Figure 3, left panel). Interestingly, internalization was rather slow as only 16.6 ± 1.4 % of the radioactivity initially associated with cells was internalized at 24 h. Excretion of degraded conjugate was also slow and at early time points the majority of non-cell-bound radioactivity was presented by intact conjugates that dissociated from cells. This observation is in agreement with known good intracellular retention of radiometal labels (26). Excreted radiocatabolites could be detected in the 24 hours media change, but amounted to only 6.5 % of the initial radioactivity. Thus, the favorable cellular retention was mainly due to strong binding (very slow off-rate) to cell membrane target.
Figure 3.
Left panel: cellular retention and internalization of 111In-CHX-A” DTPA-Z2395-C by HER2-expressing SKOV-3 ovarian carcinoma cell line after inrerrupted incubation. Right panel: percentage of non-degraded conjugate in cell culture media (high-molecular-weight fraction in size-exclusion chromatography using NAP-5 columns) as a function of time after interrupted incubation and media change. Data presented as an average from three cell culture dishes ± SD. Error bars may be not seen since they are smaller than point symbols.
Animal studies
To evaluate influence of maleimido-CHX-A” DTPA conjugation on the biodistribution of the HER2-binding Affibody molecule, the biodistribution of 111In-CHX-A” DTPA-Z2395-C was compared with 111In-DOTA-Z2395-C (site-specifically labeled at the Cterminal using DOTA) and with 111In-CHX-A”DTPA-Z342 (labeled via CHX-A” DTPA coupled using isothiocyanate) in NMRI mice, at 4 h and 24 h p.i. The results of the biodistribution experiments are presented in Table 1. All conjugates demonstrated rapid clearance from blood and the majority of normal organs and tissues. The renal excretion was dominating, which resulted in a low radioactivity accumulation in the gastrointestinal tract, but high uptake in kidneys. There were, however, some differences. Though radioactivity accumulation in bone was low, the use of DOTA provided lower bone uptake than CHX-A” DTPA. At the same time, blood-born radioactivity was higher at both time points for 111In-DOTA-Z2395-C than for both CHX-A” DTPA-containing conjugates. Hepatic accumulation of the radioactivity was also higher for 111In-DOTA-Z2395-C at 24 h pi. Interestingly, the overall clearance of 111In-CHX-A” DTPA-Z342 from blood and tissues was more rapid than clearance of both site-specifically labeled conjugates.
Table 1.
Biodistribution of different anti-HER2 Affibody conjugates after iv injection in NMRI mice.
| Uptake, % IA/g a |
||||||
|---|---|---|---|---|---|---|
| 4 h pi |
24 h pi |
|||||
| 111In-CHX-A” | 111In-DOTA- | 111In-CHX-A” | 111In-CHX-A” | 111In-DOTA- | 111In-CHX-A” | |
| DTPA-Z2395-C | Z2395-C | DTPA-Z342 | DTPA-Z2395-C | Z2395-C | DTPA-Z342 | |
| blood | 0.069 ± 0.003 c, d | 0.18 ± 0.07 | 0.04 ± 0.01 c | 0.023 ± 0.003 c, d | 0.05 ± 0.01 | 0.011 ± 0.002 c |
| lung | 0.34 ± 0.04 | 0.27 ± 0.04 | 0.24 ± 0.06 | 0.158 ± 0.009 d | 0.14 ± 0.03 | 0.107 ± 0.008 |
| liver | 1.1 ± 0.1 d | 1.01 ± 0.05 | 0.32 ± 0.07 c | 0.65 ± 0.05 c, d | 0.85 ± 0.01 | 0.17 ± 0.03 c |
| spleen | 0.30 ± 0.04 | 0.32 ± 0.03 | 0.2 ± 0.1 | 0.21 ± 0.02 d | 0.23 ± 0.02 | 0.13 ± 0.02 c |
| kidney | 234 ± 20 c | 183 ± 12 | 217 ± 21 | 135 ± 9 d | 126 ± 12 | 109 ± 8 |
| muscle | 0.08 ± 0.01 c | 0.055 ± 0.006 | 0.06 ± 0.04 | 0.05 ± 0.01 d | 0.035 ± 0.003 | 0.029 ± 0.009 |
| bone | 0.38 ± 0.08 c | 0.15 ± 0.03 | 0.4 ± 0.3 | 0.245 ± 0.03 c | 0.099 ± 0.008 | 0.17 ± 0.05 c |
| intestineb | 2.0 ± 0.4 | 2.3 ± 0.7 | 1.9 ± 0.6 | 0.87 ± 0.02 | 0.8 ± 0.2 | 0.6 ± 0.2 |
| carcassb | 3.8 ± 0.4 | 3.4 ± 0.6 | 2.6 ± 1.0 | 2.3 ± 0.4 d | 1.9 ± 0.2 | 1.2 ± 0.1 c |
data presented as average ± SD (n = 4) of per cent of injected activity per gram (% IA/g);
for intestine (together with content) and carcass, data presented as per cent of injected activity per whole sample (% IA);
significant difference (p < 0.05) with 111In-DOTA-Z2395-C at the same time point;
significant difference (p < 0.05) with 111In-CHX-A” DTPA-Z342 at the same time point;
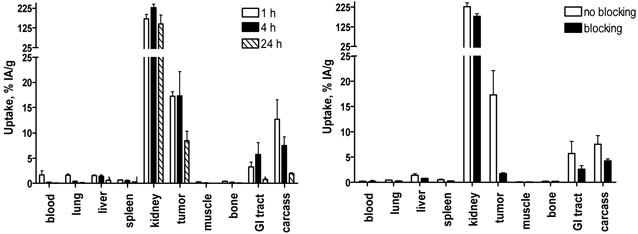
Targeting of HER2 in vivo using 111In-CHX-A” DTPA-Z2395-C was evaluated in BALB/C nu/nu mice bearing SKOV-3 xenografts (Figure 4 and Tables 2 and 3). The average tumor size was 0.57 ± 0.39 g at the time for the experiment. In agreement with biodistribution data for NMRI mice, 111In-CHX-A” DTPA-Z2395-C cleared rapidly from normal tissue and blood, with a rather high degree of renal re-absorption. Tumor targeting was also rapid, and already at 1 h pi, the tumor uptake was higher than uptake in any other organ or tissue, except kidney. At 4 h pi, the tumor uptake was not changed significantly in comparison with 1 h pi, but tumor-to-organ ratios increased significantly for blood, lung, muscle and bone due clearance from normal tissues. Only tumor-to-lung and tumor-to-muscle increased by 24 h pi in comparison with the 4 h pi time point. In order to verify the specificity of 111In-CHX-A” DTPA-Z2395-C accumulation in HER2-expressing xenografts, its biodistribution (4 h pi) was studied after saturating the binding epitope of HER2 by pre-injection of 520-fold molar excess of non-labeled ZHER2:342. The tumor uptake was reduced from 17.3 ± 4.8 to 1.7 ± 0.2 % IA/g (p < 0.001), demonstrating specific HER2-binding of 111In-CHX-A” DTPA-Z2395-C in the xenografts.
Figure 4.
Targeting of HER2-expressing xenografts in vivo. Left panel: Biodistribution of 111In-CHX-A” DTPA-Z2395-C 1, 4 and 24 h pi. Right panel: Specificity of 111In-CHX-A” DTPA-Z2395-C tumor uptake in SKOV-3 xenografts, 4 h p.i. In order to saturate HER2 receptors in tumors, one group of animals was preinjected with 520 μg nonlabeled ZHER2:342 45 min before injection of radiolabeled conjugate (designated as blocking). All animals were injected with 1 μg of labeled Affibody molecules.
Data are expressed as % IA/g (percent of injected radioactivity per gram tissue) and presented as an average from four animals ± SD.
*Data for the gastrointestinal tract (with its content) and for carcass are presented as % IA per whole sample.
Table 2.
Biodistribution of 111In-CHX-A” DTPA-Z2395-C, 111In-DOTA-Z2395-C and 111In-CHX-A” DTPA-Z342 Affibody conjugates 4 h after iv injection in BALB/C nu/nu mice bearing SKOV-3 xenografts
| Uptake, % IA/g a |
|||
|---|---|---|---|
| 111In-CHX-A” | 111In-DOTA- | 111In-CHX-A” | |
| DTPA-Z2395-C | Z2395-C | DTPA-Z342 | |
| blood | 0.22 ± 0.05 d | 0.25 ± 0.09 | 0.04 ± 0.01 c |
| lung | 0.42 ± 0.03 c, d | 0.31 ± 0.06 | 0.15 ± 0.05 c |
| liver | 1.4 ± 0.3 d | 1.6 ± 0.6 | 0.63 ± 0.08 c |
| spleen | 0.5 ± 0.1 d | 0.5 ± 0.2 | 0.16 ± 0.02 c |
| kidney | 227 ± 18 c, d | 169 ± 36 | 184 ± 17 |
| tumor | 17 ± 5 d | 8 ± 2 | 8 ± 2 |
| muscle | 0.12 ± 0.03 c, d | 0.07 ± 0.02 | 0.03 ± 0.01 c |
| bone | 0.21 ± 0.05 d | 0.2 ± 0.2 | 0.09 ± 0.03 |
| GI tract b | 6 ± 2 c | 0.9 ± 0.2 | 4.6 ± 0.3 c |
| carcass b | 8 ± 2 c, d | 2.9 ± 0.3 | 1.9 ± 0.4 c |
data presented as average ± SD (n = 4) of per cent of injected activity per gram (% IA/g);
for intestine (together with content) and carcass, data presented as per cent of injected activity per whole sample (% IA);
significant difference (p < 0.05) with 111In-DOTA-Z2395-C at the same time point;
significant difference (p < 0.05) with 111In-CHX-A” DTPA-Z342 at the same time point;
Table 3.
Tumor-to-organ ratios in BALB/C nu/nu mice bearing SKOV-3 xenograftsa
| 111In-CHX-A” | 111In-DOTA- | 111In-CHX-A” | |||
|---|---|---|---|---|---|
| DTPA-Z2395-C |
Z2395-C |
DTPA-Z342 |
|||
| 1 h | 4 h | 24 h | 4 h | 4 h | |
| blood | 12 ± 5 b | 86 ± 46 | 157 ± 49 | 36 ± 10 | 195 ± 13e, f |
| lung | 11 ± 2 b | 42 ± 14 c | 67 ± 9 | 27 ± 8 | 61 ± 16 f |
| liver | 11.5 ± 0.7 | 12 ± 3 | 14 ± 3 | 6 ± 2 d | 13 ± 3 f |
| spleen | 28 ± 4 | 35 ± 9 | 32 ± 7 | 18 ± 4 d | 53 ± 10e, f |
| kidney | 0.10 ± 0.01 | 0.08 ± 0.02 | 0.06 ± 0.01 | 0.05 ± 0.01 | 0.05 ± 0.01e |
| muscle | 61 ± 13 b | 157 ± 64 c | 246 ± 29 | 125 ± 26 | 325 ± 89 e, f |
| bone | 42 ± 8 b | 83 ± 9 | 109 ± 35 | 53 ± 25 | 103 ± 23 f |
Data are presented as an average for four animals ± SD.
Significant difference (p < 0.05) between tumor-to-organ ratios at 1 and 4 h p.i. for 111In-CHX-A” DTPA-Z2395-C
Significant difference (p < 0.05) between tumor-to-organ ratios at 4 and 24 h p.i. for 111In-CHX-A” DTPA-Z2395-C
Significant difference (p < 0.05) between tumor-to-organ ratios 4 h p.i. for 111In-CHX-A” DTPA-Z2395-C and 111In-DOTA-Z2395-C;
Significant difference (p < 0.05) between tumor-to-organ ratios 4 h p.i. for 111In-CHX-A” DTPA-Z2395-C and 111In-CHX-A” DTPA-Z342
Significant difference (p < 0.05) between tumor-to-organ ratios 4 h p.i. for 111In-DOTA-Z2395-C and 111In-CHX-A” DTPA-Z342
The targeting properties were assessed at 4 h pi to compare 111In-CHX-A” DTPA-Z2395-C with the two most favorable HER2-targeting Affibody conjugates, 111In-DOTA-Z2395-C (sitespecifically labeled at C-terminal using DOTA (20)) and 111In-CHX-A” DTPA-Z342 (labeled via CHX-A” DTPA coupled using isothiocyanate (18)). The results of this comparison are presented in Tables 2 and 3.
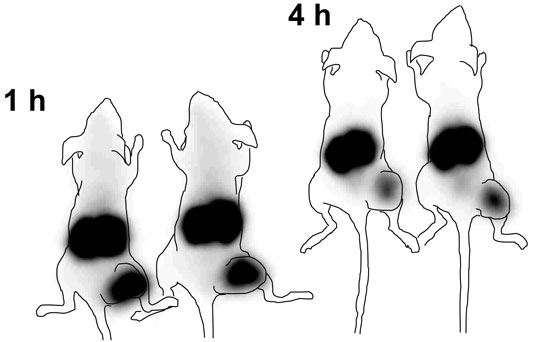
Images acquired after the i.v. injection of the 111In-CHX-A” DTPA-Z2395-C into mice bearing SKOV-3 xenografts confirmed the capacity of this conjugate to visualize HER2-expression (Figure 5). In agreement with the biodistribution data, tumors were clearly visualized already at 1 h pi (tumor-to-contralateral thigh ratio 20 ± 6). By 4 h pi, the contrast of imaging increased due to decrease of the background radioactivity (tumor-to-contralateral thigh ratio 37 ± 8). Due to the renal excretion, high radioactivity was accumulated also in kidneys.
Figure 5.
Anterior gamma-camera images of nude mice bearing HER2-expressing SKOV-3 xenografts 1 h (left) and 4 h (right) after injection of 111In-CHX-A” DTPA-Z2395-C. Contours derived from a digital photographs were superimposed over gamma-camera images to facilitate interpretation. Besides tumors (right hind legs) only kidneys are visualized.
Discussion
Personalizing cancer treatment requires methods for detection of a variety of tumor-specific cell-surface antigens for patient stratification. The Affibody technology of small robust highaffinity binders may be a convenient platform for development of molecular imaging agents to be used for non-invasive assessment of responsiveness to patient-specific therapy (1-3). The rapid tumor localization of Affibody-based targeting conjugates and their rapid clearance from blood and healthy tissues (except kidneys) result in high-contrast in vivo imaging of tumor biomarkers shortly after injection. However, careful studies on structure-properties relationship are required for design of optimal Affibody-based conjugates. Selection of suitable chelators for labeling with radiometals is one important direction of such studies. Thiol-directed chemistry is of particular interest, since it can provide exquisite site-specific coupling of chelators to both chemically and recombinantly produced Affibody molecules having a unique cystein, thereby increasing the flexibility of manufacturing.
HER2 is a transmembrane tyrosine kinase receptor, which is over-expressed in a fraction of breast, ovary and urinary bladder carcinomas (27–29). Blocking of HER2 signaling in breast carcinomas using the monoclonal antibody trastuzumab (Herceptin®) results in increase of survival and is approved for clinical use both in Europe and North America for patients with HER2 overexpressing tumors. Besides, targeted therapy of HER2-expressing tumors using radionuclides (30-33) and drugs (34) is under development. Both the American Association of Clinical Oncology (35) and the European Group on Tumour Markers (36) recommend detecting HER2 expression in each new breast tumor or recurrence in order to select patients who would benefit from trastuzumab therapy. Presently, the assessment of HER2 expression is done based on histopathological examination. Unfortunately, the results of such tests may be affected by sampling errors, discordance in HER2 expression in primary tumors and metastasis, and experience of a laboratory performing analysis (37). In contrast, molecular imaging would allow an assessment of the global HER2 expression. An example of clinical utility of radionuclide imaging of HER2 expression in breast cancer patients has been presented by Behr and co-workers (38). It was shown that the use of 111In-DTPA-trastuzumab identify not only of patients responding to trastuzumab treatment (alone or in combination with chemotherapy) but also patients, who may suffer from cardiac toxicity associated with such treatment.
The choice of the chelator moiety contributes to the overall charge and lipophilicity of the conjugate, and could in addition have an effect on the conformation of the tracer. The present study focused on the effects of different labeling methods on ZHER2:2395-C, a cysteinecontaining derivative of anti-HER2 Affibody molecule ZHER2:342 (4). Previous data have shown that coupling with the chelator DOTA followed by labeling with 111In result in a favorable molecular imaging agent, 111In-DOTA-Z2395-C (20), superior to 111In-Bz-DOTAZ342, bearing Bz-DOTA randomly coupled to amino groups (15). In contrast to DOTA, CHXA” DTPA is a semi-rigid chelator that provides stable labeling at ambient temperature with a range of medically useful radionuclides (18, 21, 39, 40). A maleimido derivative of the CHXA” DTPA was developed for use in site-directed maleimide-thiol Michael addition conjugation chemistry (23). Site-specific coupling of the maleimido-CHX-A” DTPA to ZHER2:2395-C had no major effect on affinity, suggesting that no major structural changes resulted from the conjugation. The cellular processing was essentially unchanged in comparison with 111In-DOTA-Z2395-C (20). Although 111In-CHX-A” DTPA-Z2395-C demonstrated strong membrane binding, internalization was as slow as for 111In-DOTA-Z2395-C (Figure 3). In normal mice, 111In-CHX-A” DTPA-Z2395-C, as well as 111In-DOTA-Z2395-C and 111In-CHX-A” DTPA-Z342 were rapidly cleared from the blood and the majority of tissues, accompanied by a high degree of renal re-absorption of radioactivity. Interestingly, the 111In-CHX-A” DTPA-Z342 conjugate (with the chelators conjugated via a thiourea bond) cleared more rapidly than the site-specifically labeled conjugates. The same was observed in tumor-bearing mice. In our previous study (20), an 111In-Bz-DTPA-Z342 conjugate, with an acyclic chelator randomly amine-coupled demonstrated a more rapid clearance than 111In-DOTA-Z2395-C having DOTA site-specifically coupled. One might hypothesize that a decrease in positive charge resulting from reaction of the isothiocyanate with e-amines of the lysine residues or the N-terminus amine facilitates clearance. In tumor-bearing mice, 111In-CHX-A” DTPA-Z2395-C displays rapid tumor localization, enabling high tumor-to-organ ratios as early as 1 h pi (Table 3). These results were confirmed by g-camera imaging (Figure 5). By 4 h pi, the contrast had improved further. Also, the tumor-to-lung and tumor-to-bone ratios were sufficient for imaging at 4 h pi, although these ratios were significantly increased by 24 h. At 4 h pi, the tumor-to-blood ratio of 111In-CHX-A” DTPA-Z2395-C (86:1) greatly exceeded reported values of any non-Affibody based HER2-targeting agent, including the 111In-DOTA(GSG)-KCCYSL peptide (tumor-to-blood ratio of 3:1 (41)) or 111In-CHX-A” DTPA-C6.5K-A diabody (tumor-to-blood ratio of 1.34:1 (21)).
The high kidney uptake of 111In-CHX-A” DTPA-Z2395-C might be of some concern, although the radiation dose to is most likely not a radiation safety issue. The present data are insufficient for a detailed dosimetry evaluation, but a dose estimate has been performed for another Affibody molecule, 111In-DOTA-ZHER2:342, which displayed somewhat higher uptake in kidneys (5). Dosimetry modelling suggested that the renal dose from 111In-DOTA-ZHER2:342 would be 1.8 mSv/MBq, or 200 mSv if 111 MBq is given to the patient. This is comparable with the 124 mSv/185 MBq for 111In-ProstaScint (data from package insert). It should be noted that renal doses as high as 45 Gy (after more than 90 GBq injected radioactivity) did not cause negative effects on the kidneys in clinical trials using 111In-octreotide for therapy (42, 43). The high renal uptake might complicate imaging of metastases close to kidney, however contemporary reconstruction algorithms may minimize this problem. Handling of renal uptake of radiometal-labeled Affibody molecules is discussed in more detail in a recent publication (20).
The chelator CHX-A” DTPA may be used for labeling with a different nuclides. As illustrated here, SPECT studies with 111In are possible. PET imaging is possible after labeling with 86Y, granted that the half-life of only 14.7 h is compatible with the half-life of the tracer (44). The half-life of this nuclide would facilitate distribution of radiolabelled conjugates from a central cyclotron-equipped dispensary to satellite PET centers. The use of PET might improve of sensitivity of imaging, including possibility to visualize smaller metastases or tumors in the vicinity of kidneys or urinary bladder. The chelator may also be used with a number of therapeutic radionuclides, including 90Y (21, 22, 45) 114mIn (18), 177Lu (28, 32), and the α-emitting nuclides 212 Bi and 213Bi (39, 46, 47). High renal uptake would, most likely, prevent systemic therapy using radiolabeled CHX-A” DTPA-Z2395-C. However, locoregional therapy of bladder carcinoma or brain metastases of breast cancer (sing short lived alphaemitters) deserves further investigations. The maleimido-CHX-A” DTPA is of course not limited to the labeling of Affibody molecules, but may be used with any targeting protein containing an unpaired cysteine residue, including Fab' fragments of monoclonal antibodies and scFv with an engineered cysteine. The final choice of tracer to carry the nuclide will depend on several factors. Besides pharmacokinetics and biodistribution discussed in the present report, multiple administrations may require a low immunogenic response to the tracer. Preliminary data suggest that the Affibody molecules display a low immunogenic potential, possibly due to rapid clearance from the body 7.
Conclusion
The use of maleimido-CHX-A” DTPA enables facile and stable site-specific labeling of Affibody molecules with 111In under mild conditions. The conjugate demonstrated preserved binding to HER2-expressing cells and good cellular retention of the radioactivity. In BALB/c nu/nu mice bearing HER2-expressing xenografts, the tumors were clearly visualized 1 and 4 h pi. This suggests that the Affibody molecule-maleimido-CHX-A” DTPA conjugates possess a high potential for in vivo imaging of tumor-associated targets and, possible, for radionuclide therapy. Apparently, the maleimido-CHX-A” DTPA can be a suitable chelator for sitespecific labeling of other targeting proteins, including Fab'-fragments.
Acknowledgement
This research was supported in part by the Intramural Research Program of the NIH, National Cancer Institute, Center for Cancer Research and by grant from Swedish Cancer Society (Cancerfonden).
Footnotes
HER2 - human epidermal growth factor receptor type 2, known also as neu, c-ErbB2, p185.
EGFR – human epidermal growth factor receptor type 1.
DTPA - diethyleneaminepentaacetic acid.
DOTA - 1,4,7,10-tetraazacyclododecane tetraacetic acid.
CHX-A” DTPA - N-[(R)-2-Amino-3-(p-aminophenyl)propyl]-trans-(S,S)-cyclohexane-1,2-diamine-N,N,N,N,N-pentaacetic acid.
Maleimido CHX-A” DTPA – [[2-(Bis-carboxymethyl-amino)-cyclohexyl]-(2-bis-carboxymethyl-amino)-3-{4-[7-(2,5-dioxo-2,5-dihydro-pyrrol-1-ul)-heptanoylamino]-phenyl}-propyl)-amino]-acetic acid.
Feldwisch J., unpublished results
References
- 1.Tolmachev V, Orlova A, Nilsson FY, Feldwisch J, Wennborg A, Abrahmsén L. Affibody molecules: potential for in vivo imaging of molecular targets for cancer therapy. Expert Opin. Biol. Ther. 2007;7:555–568. doi: 10.1517/14712598.7.4.555. [DOI] [PubMed] [Google Scholar]
- 2.Nilsson FY, Tolmachev V. Affibody molecules: new protein domains for molecular imaging and targeted tumor therapy. Curr. Opin. Drug. Discov. Devel. 2007;10:167–175. [PubMed] [Google Scholar]
- 3.Orlova A, Feldwisch J, Abrahmsén L, Tolmachev V. Update: affibody molecules for molecular imaging and therapy for cancer. Cancer Biother. Radiopharm. 2007;22:573–584. doi: 10.1089/cbr.2006.004-U. [DOI] [PubMed] [Google Scholar]
- 4.Orlova A, Magnusson M, Eriksson TL, Nilsson M, Larsson B, Höidén-Guthenberg I, Widström C, Carlsson J, Tolmachev V, Ståhl S, Nilsson FY. Tumor imaging using a picomolar affinity HER2 binding affibody molecule. Cancer Res. 2000;66:4339–4348. doi: 10.1158/0008-5472.CAN-05-3521. [DOI] [PubMed] [Google Scholar]
- 5.Orlova A, Tolmachev V, Pehrson R, Lindborg M, Tran T, Sandström M, Nilsson FY, Wennborg A, Abrahmsén L, Feldwisch J. Synthetic affibody molecules: a novel class of affinity ligands for molecular imaging of HER2-expressing malignant tumors. Cancer Res. 2007;67:2178–2186. doi: 10.1158/0008-5472.CAN-06-2887. [DOI] [PubMed] [Google Scholar]
- 6.Friedman M, Nordberg E, Höidén-Guthenberg I, Brismar H, Adams GP, Nilsson FY, Carlsson J, Ståhl S. Phage display selection of Affibody molecules with specific binding to the extracellular domain of the epidermal growth factor receptor. Protein Eng. Des. Sel. 2007;20:189–199. doi: 10.1093/protein/gzm011. [DOI] [PubMed] [Google Scholar]
- 7.Nordberg E, Friedman M, Göstring L, Adams GP, Brismar H, Nilsson FY, Ståhl S, Glimelius B, Carlsson J. Cellular studies of binding, internalization and retention of a radiolabeled EGFR-binding affibody molecule. Nucl. Med. Biol. 2007;34:609–618. doi: 10.1016/j.nucmedbio.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Friedman M, Orlova A, Johansson E, Eriksson T, Höidén-Guthenberg I, Tolmachev V, Nilsson FY, Ståhl S. Directed evolution to low nanomolar affinity of an epidermal growth factor receptor 1-binding Affibody molecule. J. Mol. Biol. 2008;376:1388–1402. doi: 10.1016/j.jmb.2007.12.060. [DOI] [PubMed] [Google Scholar]
- 9.Mume E, Orlova A, Larsson B, Nilsson AS, Nilsson FY, Sjöberg S, Tolmachev V. Evaluation of ((4-hydroxyphenyl)ethyl)maleimide for sitespecific radiobromination of anti-HER2 affibody. Bioconjug. Chem. 2005;16:1547–1555. doi: 10.1021/bc050056o. [DOI] [PubMed] [Google Scholar]
- 10.Orlova A, Nilsson FY, Wikman M, Widström C, Ståhl S, Carlsson J, Tolmachev V. Comparative in vivo evaluation of technetium and iodine labels on an anti-HER2 affibody for single-photon imaging of HER2 expression in tumors. J. Nucl. Med. 2006;47:512–519. [PubMed] [Google Scholar]
- 11.Engfeldt T, Orlova A, Tran T, Bruskin A, Widström C, Karlström AE, Tolmachev V. Imaging of HER2-expressing tumours using a synthetic Affibody molecule containing the 99mTc-chelating mercaptoacetyl-glycyl-glycylglycyl (MAG3) sequence. Eur. J. Nucl. Med. Mol. Imaging. 2007;34:722–733. doi: 10.1007/s00259-006-0266-4. [DOI] [PubMed] [Google Scholar]
- 12.Tran T, Orlova A, Sivaev I, Sandström M, Tolmachev V. Comparison of benzoate-and dodecaborate-based linkers for attachment of radioiodine to HER2-targeting Affibody ligand. Int. J. Mol. Med. 2007;19:485–493. [PubMed] [Google Scholar]
- 13.Tran T, Engfeldt T, Orlova A, Widström C, Bruskin A, Tolmachev V, Karlström AE. In vivo evaluation of cysteine-based chelators for attachment of 99mTc to tumor-targeting Affibody molecules. Bioconjug Chem. 2007;18:549–558. doi: 10.1021/bc060291m. [DOI] [PubMed] [Google Scholar]
- 14.Engfeldt T, Tran T, Orlova A, Widström C, Feldwisch J, Abrahmsen L, Wennborg A, Karlström AE, Tolmachev V. 99mTc-chelator engineering to improve tumour targeting properties of a HER2-specific Affibody molecule. Eur. J. Nucl. Med. Mol. Imaging. 2007;34:1843–1853. doi: 10.1007/s00259-007-0474-6. [DOI] [PubMed] [Google Scholar]
- 15.Orlova A, Tran T, Widström C, Engfeldt T, Eriksson Karlström A, Tolmachev V. Pre-clinical evaluation of [111In]-benzyl-DOTA-ZHER2:342, a potential agent for imaging of HER2 expression in malignant tumors. Int. J. Mol. Med. 2007;20:397–404. [PubMed] [Google Scholar]
- 16.Tran T, Engfeldt T, Orlova A, Sandström M, Feldwisch J, Abrahmsén L, Wennborg A, Tolmachev V, Karlström AE. 99mTc-maEEE-ZHER2:342, an Affibody molecule-based tracer for the detection of HER2 expression in malignant tumors. Bioconjug. Chem. 2007;18:1956–1964. doi: 10.1021/bc7002617. [DOI] [PubMed] [Google Scholar]
- 17.Tolmachev V, Nilsson FY, Widström C, Andersson K, Rosik D, Gedda L, Wennborg A, Orlova A. 111In-benzyl-DTPA-ZHER2:342, an affibody-based conjugate for in vivo imaging of HER2 expression in malignant tumors. J. Nucl. Med. 2006;47:846–853. [PubMed] [Google Scholar]
- 18.Orlova A, Rosik D, Sandström M, Lundqvist H, Einarsson L, Tolmachev V. Evaluation of [111/114mIn]CHX-A″-DTPA-ZHER2:342, an Affibody ligand coniugate for targeting of HER2-expressing malignant tumors. Q. J. Nucl. Med. Mol. Imaging. 2007;51:314–323. [PubMed] [Google Scholar]
- 19.Lundberg E, Höidén-Guthenberg I, Larsson B, Uhlén M, Gräslund T. Site-specifically conjugated anti-HER2 Affibody molecules as one-step reagents for target expression analyses on cells and xenograft samples. J Immunol. Methods. 2007;319:53–63. doi: 10.1016/j.jim.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 20.Ahlgren S, Orlova A, Rosik D, Sandström M, Sjöberg A, Baastrup B, Widmark O, Fant G, Feldwisch J, Tolmachev V. Evaluation of maleimide derivative of DOTA for site-specific labeling of recombinant Affibody molecules. Bioconjug. Chem. 2008;19:235–243. doi: 10.1021/bc700307y. [DOI] [PubMed] [Google Scholar]
- 21.Adams GP, Shaller CC, Dadachova E, Simmons HH, Horak EM, Tesfaye A, Klein-Szanto AJ, Marks JD, Brechbiel MW, Weiner LM. A single treatment of yttrium-90-labeled CHX-A″-C6.5 diabody inhibits the growth of established human tumor xenografts in immunodeficient mice. Cancer Res. 2004;64:6200–6206. doi: 10.1158/0008-5472.CAN-03-2382. [DOI] [PubMed] [Google Scholar]
- 22.Parry R, Schneider D, Hudson D, Parkes D, Xuan JA, Newton A, Toy P, Lin R, Harkins R, Alicke B, Biroc S, Kretschmer PJ, Halks-Miller M, Klocker H, Zhu Y, Larsen B, Cobb RR, Bringmann P, Roth G, Lewis JS, Dinter H, Parry G. Identification of a novel prostate tumor target, mindin/RG-1, for antibody-based radiotherapy of prostate cancer. Cancer Res. 2005;65:8397–8405. doi: 10.1158/0008-5472.CAN-05-1203. [DOI] [PubMed] [Google Scholar]
- 23.Xu H, Baidoo KE, Wong KJ, Brechbiel MW. A novel bifunctional maleimido CHX-A″ chelator for conjugation to thiol-containing biomolecules. Bioorg Med Chem Lett. 2008;18:2679–83. doi: 10.1016/j.bmcl.2008.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Persson M, Tolmachev V, Andersson K, Gedda L, Sandstrom M, Carlsson J. [177Lu]pertuzumab: experimental studies on targeting of HER-2 positive tumour cells. Eur. J. Nucl. Med. Mol. Imaging. 2005;32:1457–1462. doi: 10.1007/s00259-005-1902-0. [DOI] [PubMed] [Google Scholar]
- 25.Wållberg H, Orlova A. Slow internalization of anti-HER2 synthetic Affibody monomer 111In-DOTA-ZHER2:342-pep2: implications for development of labeled tracers. Cancer Biother. Radiopharm. 2008. in press. [DOI] [PubMed]
- 26.Shih LB, Thorpe SR, Griffiths GL, Diril H, Ong GL, Hansen HJ, Goldenberg DM, Mattes MJ. The processing and fate of antibodies and their radiolabels bound to the surface of tumor cells in vitro: a comparison of nine radiolabels. J. Nucl. Med. 1994;35:899–908. [PubMed] [Google Scholar]
- 27.Aunoble B, Sanches R, Didier E, Bignon YJ. Major oncogenes and tumor suppressor genes involved in epithelial ovarian cancer (review) Int. J. Oncol. 2000;16:567–576. doi: 10.3892/ijo.16.3.567. [DOI] [PubMed] [Google Scholar]
- 28.Carlsson J, Nordgren H, Sjostrom J, et al. HER2 expression in breast cancer primary tumours and corresponding metastases. Original data and literature review. Br J Cancer. 2004;90:2344. doi: 10.1038/sj.bjc.6601881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gardmark T, Wester K, de la Torre M, Carlsson J, Malmstrom PU. Analysis of HER2 expression in primary urinary bladder carcinoma and corresponding metastases. BJU Int. 2005;95:982–986. doi: 10.1111/j.1464-410X.2005.05452.x. [DOI] [PubMed] [Google Scholar]
- 30.Brechbiel MW, Waldmann TA. Anti-HER2 radioimmunotherapy. Breast Dis. 2000;11:125–132. doi: 10.3233/bd-1999-11111. [DOI] [PubMed] [Google Scholar]
- 31.Milenic DE, Garmestani K, Brady ED, Albert PS, Ma D, Abdulla A, Brechbiel MW. Targeting of HER2 antigen for the treatment of disseminated peritoneal disease. Clin. Cancer Res. 2004;10:7834–7841. doi: 10.1158/1078-0432.CCR-04-1226. [DOI] [PubMed] [Google Scholar]
- 32.Tolmachev V, Orlova A, Pehrson R, Galli J, Baastrup B, Andersson K, Sandström M, Rosik D, Carlsson J, Lundqvist H, Wennborg A, Nilsson FY. Radionuclide therapy of HER2-positive microxenografts using a 177Lu-labeled HER2-specific Affibody molecule. Cancer Res. 2007;67:2773–2782. doi: 10.1158/0008-5472.CAN-06-1630. [DOI] [PubMed] [Google Scholar]
- 33.Milenic DE, Garmestani K, Brady ED, Albert PS, Ma D, Abdulla A, Brechbiel MW. Alpha-particle radioimmunotherapy of disseminated peritoneal disease using a 212Pb-labeled radioimmunoconjugate targeting HER2. Cancer Biother. Radiopharm. 2005;20:557–568. doi: 10.1089/cbr.2005.20.557. [DOI] [PubMed] [Google Scholar]
- 34.Mandler R, Wu C, Sausville EA, Roettinger AJ, Newman DJ, Ho DK, King CR, Yang D, Lippman ME, Landolfi NF, Dadachova E, Brechbiel MW, Waldmann TA. Immunoconjugates of geldanamycin and anti-HER2 monoclonal antibodies: antiproliferative activity on human breast carcinoma cell lines. J. Natl. Cancer. Inst. 2000;92:1573–1581. doi: 10.1093/jnci/92.19.1573. [DOI] [PubMed] [Google Scholar]
- 35.Bast RC, Jr, Ravdin P, Hayes DF, Bates S, Fritsche H, Jr, Jessup JM, Kemeny N, Locker GY, Mennel RG, Somerfield MR, American Society of Clinical Oncology Tumor Markers Expert Panel 2000 update of recommendations for the use of tumor markers in breast and colorectal cancer: clinical practice guidelines of the American Society of Clinical Oncology. J. Clin. Oncol. 2001;19:1865–1878. doi: 10.1200/JCO.2001.19.6.1865. [DOI] [PubMed] [Google Scholar]
- 36.Molina R, Barak V, van Dalen A, Duffy MJ, Einarsson R, Gion M. Tumor markers in breast cancer-European Group on Tumor Markers recommendations. Tumour Biol. 2005;26:281–293. doi: 10.1159/000089260. [DOI] [PubMed] [Google Scholar]
- 37.Perez EA, Suman VJ, Davidson NE, Martino S, Kaufman PA, Lingle WL, Flynn PJ, Ingle JN, Visscher D, Jenkins RB. HER2 testing by local, central, and reference laboratories in specimens from the North Central Cancer Treatment Group N9831 intergroup adjuvant trial. J Clin Oncol. 2006;24:3032–3038. doi: 10.1200/JCO.2005.03.4744. [DOI] [PubMed] [Google Scholar]
- 38.Behr TM, Behe M, Wormann B. Trastuzumab and breast cancer. N Engl J Med. 2001;345:995–996. doi: 10.1056/NEJM200109273451312. [DOI] [PubMed] [Google Scholar]
- 39.Nikula TK, McDevitt MR, Finn RD, Wu C, Kozak RW, Garmestani K, Brechbiel MW, Curcio MJ, Pippin CG, Tiffany-Jones L, Geerlings MW, Sr, Apostolidis C, Molinet R, Geerlings MW, Jr, Gansow. OA, Scheinberg DA. Alpha-emitting bismuth cyclohexylbenzyl DTPA constructs of recombinant humanized anti-CD33 antibodies: pharmacokinetics, bioactivity, toxicity and chemistry. J. Nucl. Med. 1999;40:166–176. [PubMed] [Google Scholar]
- 40.Milenic DE, Garmestani K, Chappell LL, Dadachova E, Yordanov A, Ma D, Schlom J, Brechbiel MW. In vivo comparison of macrocyclic and acyclic ligands for radiolabeling of monoclonal antibodies with 177Lu for radioimmunotherapeutic applications. Nucl. Med. Biol. 2002;29:431–442. doi: 10.1016/s0969-8051(02)00294-9. [DOI] [PubMed] [Google Scholar]
- 41.Kumar SR, Quinn TP, Deutscher SL. Evaluation of an 111In-Radiolabeled Peptide as a Targeting and Imaging Agent for ErbB-2 Receptor – Expressing Breast Carcinomas. Clin. Cancer Res. 2007;13:6070–6079. doi: 10.1158/1078-0432.CCR-07-0160. [DOI] [PubMed] [Google Scholar]
- 42.Valkema R, De Jong M, Bakker WH, Breeman WA, Kooij PP, Lugtenburg PJ, De Jong FH, Christiansen A, Kam BL, De Herder WW, Stridsberg M, Lindemans J, Ensing G, Krenning EP. Phase I study of peptide receptor radionuclide therapy with [In-DTPA]octreotide: the Rotterdam experience. Semin. Nucl. Med. 2002;32:110–122. doi: 10.1053/snuc/2002.31025. [DOI] [PubMed] [Google Scholar]
- 43.Kwekkeboom DJ, Mueller-Brand J, Paganelli G, Anthony LB, Pauwels S, Kvols LK, O'dorisio TM, Valkema R, Bodei L, Chinol M, Maecke HR, Krenning EP. Overview of results of peptide receptor radionuclide therapy with 3 radiolabeled somatostatin analogs. J. Nucl. Med. 2005;46(Suppl 1):62S–66S. [PubMed] [Google Scholar]
- 44.Clifford T, Boswell CA, Biddlecombe GB, Lewis JS, Brechbiel MW. Validation of a novel CHX-A″ derivative suitable for peptide conjugation: small animal PET/CT imaging using yttrium-86-CHX-A″-octreotide. J. Med. Chem. 2006;49:4297–4304. doi: 10.1021/jm060317v. [DOI] [PubMed] [Google Scholar]
- 45.Lee FT, Mountain AJ, Kelly MP, Hall C, Rigopoulos A, Johns TG, Smyth FE, Brechbiel MW, Nice EC, Burgess AW, Scott AM. Enhanced efficacy of radioimmunotherapy with 90Y-CHX-A″-DTPA-hu3S193 by inhibition of epidermal growth factor receptor (EGFR) signaling with EGFR tyrosine kinase inhibitor AG1478. Clin. Cancer Res. 2005;11:7080S–7086S. doi: 10.1158/1078-0432.CCR-1004-0019. [DOI] [PubMed] [Google Scholar]
- 46.McDevitt MR, Barendswaard E, Ma D, Lai L, Curcio MJ, Sgouros G, Ballangrud AM, Yang WH, Finn RD, Pellegrini V, Geerlings MW, Jr., Lee M, Brechbiel MW, Bander NH, Cordon-Cardo C, Scheinberg DA. An alpha-particle emitting antibody ([213>Bi]J591) for radioimmunotherapy of prostate cancer. Cancer Res. 2000;60:6095–6100. [PubMed] [Google Scholar]
- 47.Kelly MP, Lee FT, Tahtis K, Smyth FE, Brechbiel MW, Scott AM. Radioimmunotherapy with alpha-particle emitting 213Bi-C-functionalized transcyclohexyl-diethylenetriaminepentaacetic acid-humanized 3S193 is enhanced by combination with paclitaxel chemotherapy. Clin. Cancer Res. 2007;13:5604S–5612S. doi: 10.1158/1078-0432.CCR-07-1071. [DOI] [PubMed] [Google Scholar]