Translation requires individuals who are fluent in two languages, and this is equally true of translational medicine, for which clinician-scientists are the essential conduit between laboratory and clinic. Without individuals who lead active laboratory research programmes and possess an understanding of the needs and practical realities of clinical medicine, our hopes of exploiting our burgeoning understanding of disease models and mechanisms to develop new approaches to diagnosis and therapy will founder. The pressure on these professionals is immense as they cope with the demands of literally two jobs in one, and throughout the developed world it is becoming increasingly recognised that they must be more carefully nurtured if the increasing popularity of translational medicine is to generate genuine advances in health care. The landscape in the UK reflects that of other nations with established clinical academic cultures, and highlights the challenges and opportunities that those with both clinical and academic aspirations face.
It is evident that clinician-scientists are high-fliers, but also increasingly obvious that they are rare and endangered
Clinician-scientist programmes were established in the UK in the mid-1980s with a similar aim to the US NIH K08 funding stream, which provides mentored early career awards to support clinically orientated individuals performing basic or translational research. A major initiative was launched to allow clinicians to develop postdoctoral research programmes under the wing of established investigators while simultaneously engaged in clinical practice to complete their higher specialist training. Key agencies that had the vision to see the potential of such schemes to deliver their mission and were early investors were the Medical Research Council, the Wellcome Trust and Cancer Research UK (I declare an interest here – I received funding from the latter as their first such appointment; whether their investment returned a dividend is for others to judge…). Analysis of their impact is complicated as tracking of career progression was neglected until recently, but an analysis of the individuals appointed by the MRC in the first phase (1988–1993) revealed that over 95% of the awardees headed a research group 20 years later; the awardees spent typically over 50% of their time on research; and the majority of those who had been clinician-scientists now generated over £500,000 per annum research funding, compared with between £100,000 and £500,000 for the majority of non-clinical scientists appointed to the parallel career development awards in the same period. It was found that 80% of the clinician-scientists had gone on to hold full Professorships, compared with just 35% of their non-clinical peers of the same period. It is evident that clinician-scientists are high-fliers, but also increasingly obvious that they are rare and endangered.
As in other countries (Ley and Rosenberg, 2005), there has been a dawning realisation that the cadre of clinician-scientists is smaller and older than it was when the programmes were initiated. A tiny minority of individuals has had the opportunity to gain a PhD integrated with their undergraduate medical course, as such programmes exist at only three institutions in the UK (Cambridge with 131 students since 1990, University College London with 62 since 1994 and a much smaller programme at Leicester). By contrast, US programmes are comparatively well funded, with several hundred new entrants annually and a majority of students supported centrally via the National Institutes of Health (NIH) Medical Scientist Training Program (supporting 45 degree-granting institutions). The subsequent US training pathways are well designed to accommodate and fast-track the supply of MD PhD graduates, and tracking of these individuals shows that they are extremely successful in pursuing research careers and obtaining research funding.
There have been diminishing incentives for clinicians to pursue an academic route after qualification. The lack of a clear career structure in clinical academic medicine, with resulting uncertainties in the prospects of ultimately obtaining a tenured senior post, contrasts strongly with the clear career structure for a doctor in a formal specialist training programme who, typically, is qualified for an National Health Service consultant post after five years of training. The debacle following the rushed introduction by the UK Department of Health of a new system for selection of trainees for specialist training was probably the final straw as it appeared actively to discriminate against those with academic credentials in favour of individuals skilled in ‘creative writing’ (Tooke et al., 2007; House of Commons Health Committee, 2008). There is a major financial disadvantage in choosing to be an academic, and the intellectual rewards may not balance the financial imperatives that clinical professionals face from the moment they qualify from medical school. The British Medical Association’s annual medical student finance survey in 2007 reported that the average final year medical student in the UK will graduate with debts of over £20,000 (British Medical Association, 2007), while in the US those graduating from public medical schools in 2004 had a median educational debt of more than $100,000 (Morrison, 2005). Setting out on an academic path at qualification with a cloud of debt overhead is a brave move, and one that a diminishing proportion of graduates have been prepared to make.
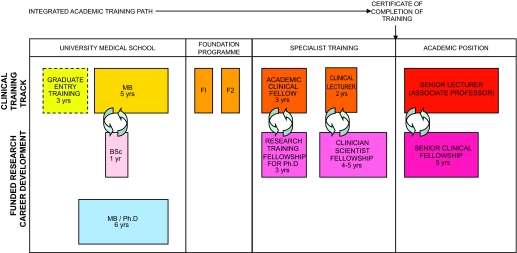
However, as a result of the Savill Report (Academy of Medical Sciences, 2000), a new integrated clinical academic training pathway (Fig. 1) has been established in the UK to address the key stages of a clinician’s career, namely: medical school; early phase of general medical training (Foundation programmes); specialist training; and consultant grade. At each of these stages there are opportunities for those training in medicine to conduct research in parallel supported by the National Institute of Health Research, the Higher Education Funding Committees that support the university sector, as well as the Medical Research Council and a host of charities (notably Wellcome Trust, Cancer Research UK and the British Heart Foundation). Not only has this injected new funding into the system for several hundred new entrants each year, but it gives confidence to trainees that they will no longer be a ‘lost tribe’ but instead a properly recognised cohort of clinician-scientists and research-oriented physicians. Crucially, mentorship is integral to the pathway and, following the lead of the Academy of Medical Sciences, the sponsoring organisations are developing networks that will look after the interests of individuals and ensure quality of both the research and training elements of their programmes.
Fig. 1.
Integrated clinical academic training pathway.
After a prolonged period during which the interests of clinician-scientists were neglected, the culture of both the health service and the academic sector has shifted in a more translational direction. The UK Government’s strategy for funding and management now aims for the NHS to be recognised for taking an international lead in supporting a research-led culture for health (Department of Health, 2006), with health and healthcare improved by research evidence. That evidence can only come from translational research in experimental medicine, and clinician-scientists are natural leaders in this area.
Universities are increasingly interested in providing leadership in health care in the UK, with new Academic Health Sciences Centres following the lead of London’s Imperial College Healthcare NHS Trust, which in 2007 brought together a network of hospitals under the leadership of a leading academic institution. Clinician-scientists are central to the ethos of these enterprises and their futures are intertwined; individual success will fuel advances in public health and the delivery of health care, and it is in all our interests to ensure that every effort is made to encourage and protect their welfare as they move disease research towards a better future.
References
- Academy of Medical Sciences (2000. The tenure-track clinician-scientist: a new career pathway to promote recruitment in clinical academic medicine. http://www.acmedsci.ac.uk/Clinic.pdf
- British Medical Association (2007). Medical Student Committee Newsletter. http://www.bma.org.uk/ap.nsf/Content/mscupdateoctober2007
- Department of Health (2006). Best Research for Best Health: A new national health research strategy. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/Browsable/DH_4127225
- House of Commons Health Committee (2008). http://www.publications.parliament.uk/pa/cm200708/cmselect/cmhealth/25/2502.htm
- Ley T. J., Rosenberg L. E. (2005). The physician-scientist career pipeline in 2005. JAMA 294, 1343–1351 [DOI] [PubMed] [Google Scholar]
- Morrison G. (2005). Mortgaging our future – the cost of medical education. New Engl. J. Med. 352, 117–119 [DOI] [PubMed] [Google Scholar]
- Tooke J., Ashtiany S., Carter D., Cole A., Michael J., Rashid A., Smith P. C., Tomlinson S., Petty-Saphon K. (2007). Aspiring to Excellence. http://www.mmcinquiry.org.uk/MMC_FINAL_REPORT_REVD_4jan.pdf