Abstract
Injury is a major public health problem generating substantial morbidity, mortality, and economic burden on society. The majority of seriously injured persons are initially evaluated and cared for by prehospital providers, however the effect of emergency medical services (EMS) systems, EMS clinical care, and EMS interventions on trauma patient outcomes is largely unknown. Outcome-based information to guide future EMS care has been hampered by the lack of comprehensive, standardized, multicenter prehospital data resources that include meaningful patient outcomes. In this paper, we describe the background, design, development, implementation, content, and potential uses of the first North American comprehensive epidemiologic prehospital data registry for injured persons. This data registry samples patients from 264 EMS agencies transporting to 287 acute care hospitals in both the United States and Canada.
Keywords: emergency medical services, prehospital, outcome, trauma, injury, registry
BACKGROUND
Injury is a major international public health problem1–6 and is responsible for a substantial portion of health care expenditures and societal costs.7–10 Despite broad implementation of trauma systems and the growing body of injury-related literature, many trauma questions remain unanswered, particularly regarding the prehospital care of injured patients. Population-based studies measuring the incidence and outcome of major injury are sparse and the effect of prehospital care on the health outcomes of injured persons remains largely undefined.11,12 The lack of multi-site, population-based, comprehensive prehospital data resources for injury has contributed to the persistence of these questions and has slowed further assessment of prehospital practices on outcomes.
While trauma registries have been used to quantify the impact, processes, and patient care provided in organized trauma systems, such data sources generally identify patients using hospital-based criteria (e.g., injury severity, hospital admission), which can introduce significant selection bias. Such registries often have inconsistent inclusion criteria,13 generally contain limited prehospital information, and frequently exclude patients at the extremes of the injury spectrum (e.g., those who die in the field, expire after a failed resuscitation in a non-trauma center, and/or patients treated and released). Such limitations preclude detailed, outcome-based assessments of emergency medical services (EMS) system factors and evaluation of the composition, timing, and sequence of prehospital resuscitation care that are necessary to define best practices.
Recognizing these needs, we sought to design, develop, and implement a multi-site, population-based, North American prehospital epidemiologic data registry of injured persons matched to hospital-based outcomes among a group of diverse sites participating in a prehospital clinical research consortium (the Resuscitation Outcomes Consortium [ROC]). This effort is termed the “ROC Epistry-Trauma” (i.e., an epidemiologic data registry for trauma). In this paper, we describe the background, design and development of the ROC Epistry-Trauma database, including: patient population and sampling, development and description of data elements, case identification, linkage of data sources, data management, quality assurance, regulatory issues, projected sample size, and potential uses of these data. A companion prehospital data registry (“ROC Epistry-Cardiac Arrest”) was developed in parallel to evaluate and improve prehospital emergency care among persons suffering out-of-hospital cardiac arrest and is described in a separate paper.14
EPISTRY METHODS
Design
The ROC Epistry-Trauma is a prospective, consecutive patient, cohort study.
Setting
ROC is a North American consortium of 11 sites, each with multiple EMS agencies and hospitals that was created to perform prehospital interventional trials among patients suffering major injury or (separately) out-of-hospital cardiac arrest. The consortium includes 11 regional coordinating centers, with 8 in the U.S. (Birmingham, AL; Dallas, TX; Iowa City, Iowa; Milwaukee, WI; Pittsburgh, PA; Portland, OR; San Diego, CA; and King County, WA), 3 in Canada (Ottawa, Toronto, and Vancouver), plus a Data Coordinating Center (Seattle, WA) (Figure 1). The ROC Epistry-Trauma consists of consecutive injured patients from these sites, which vary in size (e.g., cities, counties, portions of states and Canadian provinces), each with a defined geographic land mass (Table 1). The more than 36,000 EMS providers within these sites have varying certification levels and serve a combined population of 23.7 million persons from diverse urban, suburban, rural, and frontier regions. There are 264 ground and air medical EMS agencies and 287 hospitals that contribute data to the ROC Epistry-Trauma.15
Figure 1.
Geographic location of the 11 Regional Coordinating sites and Data Coordinating Center contributing to the ROC Epistry-Trauma database.
Table 1.
Description of the 11 Resuscitation Outcomes Consortium (ROC) sites contributing to the ROC Epistry-Trauma database.15
| ROC Site | Service area population* | Geographic Area (sq miles)* | Number of EMS agencies | Number of Hospitals |
|---|---|---|---|---|
| Birmingham, AL | 644,701 | 1,328 | 13 | 14 |
| British Columbia | 2,779,373 | 1,733 | 39 | 33 |
| Dallas, TX | 1,989,357 | 627 | 11 | 22 |
| Iowa | 1,015,347 | 2,614 | 19 | 19 |
| Milwaukee, WI | 940,164 | 242 | 16 | 16 |
| Ottawa | 4,030,696 | 13,213 | 39 | 37 |
| Pittsburgh, PA | 935,967 | 2,362 | 6 | 38 |
| Portland, OR | 1,751,119 | 4,059 | 15 | 16 |
| San Diego, CA | 2,297,334 | 2,059 | 39 | 19 |
| Seattle, WA | 1,666,978 | 1,060 | 35 | 18 |
| Toronto | 5,627,021 | 6,180 | 32 | 55 |
| Total | 23,678,057 | 35,477 | 264 | 287 |
If an agency's service area followed the geographic boundaries of a town, city, or county, population figures were obtained from the 2000 U.S. Census and the 2001 Canadian Census. The areas served by some of the U.S. agencies did not follow the geographic boundaries of a specific town, city, or county. Population figures for those agencies were based on the census tracts within the service area.
Patient Population
The ROC Epistry-Trauma database consists of consecutively enrolled injured infants, children, and adults requiring activation of the emergency 9-1-1 system within the predefined geographic regions at each ROC site, receiving EMS provider evaluation (whether transported or not), and meeting specific field-based physiologic inclusion criteria for “major trauma” (Table 2). The inclusion criteria are based on standard field trauma triage guidelines that have previously demonstrated high specificity for serious injury and need for specialized trauma resources among both adults and children.16–33 “Injury” is broadly defined as any blunt, penetrating, or burn mechanism where the EMS provider(s) believes trauma to be the primary clinical insult. Use of a prospective, EMS provider-based definition for trauma/injury does introduce variability to patient sampling (e.g., a person “found down” with altered mental status that may or may not be considered a trauma patient by different prehospital providers). However, employing such an approach for case identification allows for the sampling of patients from the EMS provider perspective and a truly representative EMS sample. While exclusion of patients with normal field vital signs following a significant injury mechanism will exclude some patients with serious injuries,17,19,21–26,29,30 these physiologic criteria were selected for their high predictive value in identifying patients most likely to require prehospital resuscitation and clinical interventions (either as part of standing practice or for prehospital clinical trials), while also balancing the desire for high quality data using available site resources.
Table 2.
Prehospital inclusion criteria for the ROC Epistry-Trauma cohort*
| Systolic blood pressure ≤ 90 mmHg or |
| Glasgow Coma Scale score ≤ 12 or |
| Respiratory rate < 10 or > 29 breaths per minute or |
| Field intubation/advanced airway procedure† or |
| Traumatic death in the field |
Inclusion criteria are based on prehospital provider assessment and management. The criteria are applied regardless of age.
Advanced airway procedures include any of the following: supraglottic airway (e.g., Combitube or King airway), cricothyrotomy, or nasopharyngeal intubation.
Additional inclusion criteria, such as hospital admission or the Injury Severity Score34 (ISS), were intentionally omitted to avoid potential selection bias and to increase the generalizability of the ROC Epistry-Trauma data to other EMS systems, as such factors cannot reliably be determined in the field. Inclusion of all patients who meet standardized prehospital criteria rather than those admitted to a trauma center or having an ISS over a certain value allows for a true EMS-based sample. This sample design is unique to the ROC Epistry-Trauma and is a significant distinction from existing trauma registry data sources.
Further, the ROC Epistry-Trauma does not incorporate age-adjusted inclusion criteria. Previous studies suggest that pediatric and adult physiologic criteria possess comparable accuracy in identifying seriously injured pediatric patients.27,30,35 Uniform entry criteria were selected to provide a simple and straightforward approach to broadly surveying injured adult and pediatric patients. Pregnant women and prisoners are included, where permitted by local institutional review boards (IRBs) and research ethics boards (REBs), as they represent populations perceived to be at increased risk for poor outcomes related to injury, yet have rarely been included in previous trauma studies.
Sampling Framework
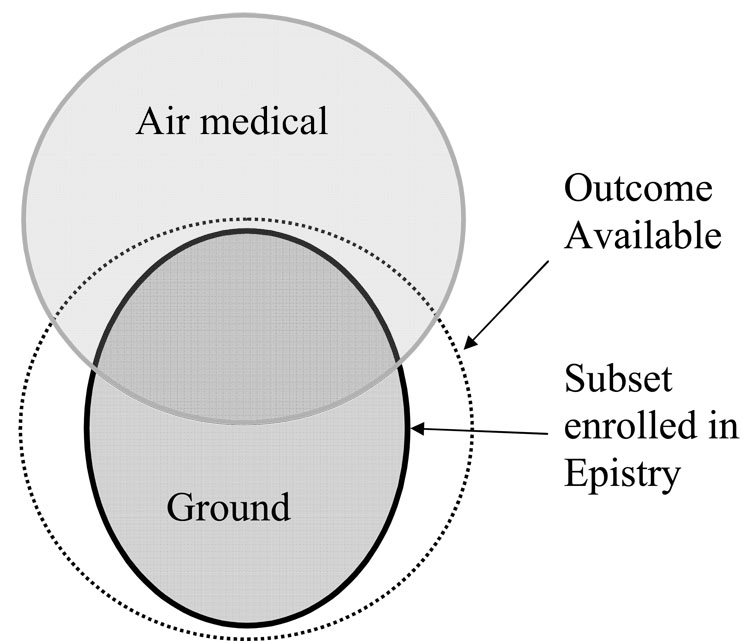
EMS coverage for a given region can be complex and varied between different EMS systems. To further reduce selection bias, the Epistry samples consecutive patients from the majority of EMS agencies providing coverage for a defined geographic “footprint” at each site (Figure 2), rather than sampling by hospital. Each site defined their “footprint” based on participating ground EMS agency coverage territory. Eligible patients originating within the defined regions and ultimately transported by air medical services are also captured in Epistry, though air medical patients originating outside of the footprint are excluded. This geographic approach to sampling allows for a population-based sample in the ROC Epistry-Trauma.
Figure 2.
Schematic of the ROC Epistry-Trauma geographic “footprint” for sampling patients relative to emergency medical services ground and air medical agency coverage areas.
Development of Data Elements
A comprehensive review of the trauma literature was initially conducted to search for all relevant English language publications. Following the literature review, an interdisciplinary working group of ROC investigators from all 11 sites, ROC site research and EMS personnel, and Data Coordinating Center (DCC) investigators met weekly by conference call over 15 months (September 15, 2004 through November 30, 2005) to develop the ROC Epistry concept, vision, protocol, and detailed database components by consensus. Definitions and response options for each variable were reviewed and related literature (e.g., National Emergency Medical Services Information System [NEMSIS],36 Utstein style uniform reporting for trauma37) was used and cited wherever possible. Where there was controversy, small groups of experts were assembled to reach consensus based on site pilot data and thorough review of the literature, subsequently providing a recommendation and justification to the larger group. The intent of the ROC Epistry development process was not to reinvent previously developed terms, but rather to use existing EMS data elements where available, to develop definitions for terms not previously defined, and to assure that all variables met the needs for scientific investigation and trauma resuscitation research. A manual of operations was developed to guide the selection and use of common terms in NEMSIS, the Utstein trauma template, and Epistry so that EMS agencies could readily map these fields into the ROC Epistry-Trauma database.
The database is divided into two general phases of care: prehospital and in-hospital. The prehospital data points collected for all enrolled subjects include (as recorded by prehospital providers): episode-specific factors, demographic, mechanism, clinical, procedural, geospatial measures (census tract, latitude/longitude coordinates, or Universal Transverse Mercator Grid), and field disposition information. Hospital-based data elements include date, receiving hospital, interhospital transfer information, and emergency department/hospital disposition (i.e., survival).
Because of the large number of EMS agencies and hospitals participating in this project, we sought to restrict “mandatory” data elements to those representing the most essential field elements and easily obtainable outcomes. A summary list of mandatory prehospital and hospital variables is provided in Table 3. All ROC Epistry-Trauma data elements, data definitions, and mapped NEMSIS and Utstein data elements are listed in Appendix 2 (on-line http site XXXX). Accompanying images of web-based ROC Epistry data forms (for both the trauma and cardiac arrest cohorts) are listed in Appendix 3 (online http site XXXX). Appendices 2 and 3 represent the most recent version of the ROC Epistry-Trauma components, although we acknowledge that further refining and improving the ROC Epistry-Trauma is a continuing process and these forms are likely to be modified with future versions.
Table 3.
Mandatory variables included in the ROC Epistry-Trauma database.*
| Prehospital | |
|---|---|
| Episode-specific factors: | Time call received at dispatch† |
| Responding EMS agencies and vehicles | |
| Time of arrival for each vehicle | |
| Number of EMS providers | |
| Highest EMS provider service levels | |
| Criteria for Epistry enrollment | |
| Concomitant clinical trial participation | |
| Date of service | |
| Prehospital times (9) | |
| Geospatial location of event | |
| Public versus private location of event | |
| Demographics: | Age |
| Gender | |
| Race/ethnicity | |
| Clinical information: | Systolic blood pressure (mmHg)‡ |
| Glasgow Coma Scale score (eye, motor, verbal)‡ | |
| Respiratory rate (breaths/minute)‡ | |
| Pulse rate (beats/minute)‡ | |
| Pulse oximetry (% oxygen saturation)‡ | |
| Traumatic arrest | |
| Injury type | |
| Injury mechanism | |
| Use of safety equipment | |
| Prehospital interventions: | Intravenous/intraosseus line placement |
| Fluid therapy | |
| Airway interventions | |
| Cardiopulmonary resuscitation | |
| Hemorrhage control | |
| Prehospital disposition: | Died at scene or en route (noted with or without EMS treatment) |
| Reason not treated or why treatment halted | |
| Alive and not transported by EMS | |
| Transport to hospital/mode of transport | |
| Patient status at ED arrival | |
| Hospital | |
| Hospital information: | Date of ED arrival |
| Name of hospital, trauma level | |
| Interhospital transfer to another acute care hospital, date | |
| Outcome: | Date of final ED/hospital disposition |
| Hospital discharge survival status | |
Detailed descriptions of both mandatory and optional ROC Epistry-Trauma variables are included in Appendix 1. EMS = emergency medical service; ED = emergency department.
Although time call received at the initial 9-1-1 dispatch is available at some sites, many other sites have layered dispatch systems where initial calls are relayed from a primary safety access point (i.e., first ring at 9-1-1) to a dedicated EMS dispatch center. Based on uniform availability at all sites, EMS “time zero” in ROC Epistry-Trauma represents the time of call to the EMS dispatch center.
Field physiologic measures include first, second, and worst recorded values from the field.
Case Identification, Data Capture, and Disparate Data Sources
Site surveillance of EMS-attended field trauma patient evaluation is important to assure a true population-based registry. However, to produce an accurate and sequential picture of prehospital care and heterogeneous nature of emergency response systems, it is necessary to link a variety of disparate data sources (e.g., dispatch centers, EMS ground agencies, air medical services). Some systems generate two or more prehospital records for each patient (e.g., dispatch data from one or more sources, multiple agencies responding to a single incident) that must be matched and discrepancies resolved. In most cases, a variety of methods (e.g., hand sorting, electronic queries, local data managers) with multiple collaborators (e.g., EMS agencies, communication and dispatch centers, medical directors, and state EMS offices) are used within a given site to ensure complete case identification and data capture. The DCC provides monthly reviews of ROC Epistry-Trauma enrollment by site and by agency to further assure complete, consistent, and timely case capture.
Data Management Strategies
A data management system is intended to facilitate data entry and access (e.g., for monitoring and analysis), while maintaining data accuracy, completeness, security, and quality. Central database management for the ROC Epistry-Trauma is overseen and facilitated by the DCC. Once cases are identified, prehospital records captured, and outcomes matched for ROC Epistry-Trauma, sites enter this information into a standardized central database. Two strategies for centralized data submission were designed to allow flexibility, while maintaining data integrity: web-based data entry and batch uploading. Web entry entails manual data entry with real-time error checks to increase the quality of data and to reduce data entry errors. Batch uploading consists of comprehensive coding and mapping of data fields to allow sites with local electronic data systems to upload cleaned data efficiently. Error checks are built into the batch upload process to ensure quality data for ROC Epistry-Trauma. Only de-identified information is submitted to the DCC to ensure compliance with privacy regulations and standards in both the U.S. and Canada.
Quality Assurance
Each site developed specific quality assurance plans for the ROC Epistry-Trauma data. These plans include: initial EMS provider training in data collection, continuing education of EMS providers for certain variables and definitions (e.g., Glasgow Coma Scale score), DCC review of randomly selected site records to confirm accuracy of data entry, and data element range and consistency checks in both the web-based data entry forms and the batch upload process. In addition, the DCC conducts annual site visits to further review a portion of entered records, data capture processes, site progress, and site-specific mechanisms for quality assurance.
Regulatory Issues
In total, 153 IRBs/REBs (127 hospital-based and 26 EMS agency-based) reviewed and approved the ROC Epistry-Trauma protocol. Great efforts were made to assure that the sampling strategy and population-based study design would not be compromised by variability in review board approval.38 As an observational study using existing data sources (i.e., EMS and hospital records), the ROC Epistry-Trauma project met requirements for minimal risk research and a waiver of consent in both the United States39 and Canada.40 However, because protected health information is required by sites to accurately link records from the two phases of patient care, additional protections were instituted to assure stringent patient confidentiality protections, including secure encrypted transfer of information. To further monitor human subject protections and progress in the ROC Epistry-Trauma, a data safety and monitoring board reviewed the initial protocol and provides ongoing semi-annual reviews.
Sample Size
When developing the ROC Epistry-Trauma, each site was asked to derive an estimate for the number of annual trauma patients meeting eligibility criteria for enrollment. These estimates were made using existing data sources (e.g., hospital-based trauma registries, individual EMS agency databases). While a reliable estimate of major trauma based on prehospital measures is not available (and will be one of the epidemiologic questions addressed by the Epistry), we anticipate the ROC Epistry-Trauma to enroll up to 13,000 injured persons per year.
POTENTIAL USES of EPISTRY-TRAUMA DATA
The Epistry will provide the first international, standardized, population-based EMS database of injured persons matched to hospital outcomes. This project will also complement ongoing efforts to standardize EMS data fields36,41,42 and to create and standardize a national hospital-based trauma dataset.43,44 The data definitions, data forms, and data field mapping to existing NEMSIS and Utstein data fields may also provide other EMS systems and investigators a template to utilize in their own EMS research. In the following sections, we highlight three potentially important uses of ROC Epistry-Trauma data.
Need for Outcome-Based Assessment of EMS Care
There is a great need for outcome-based assessment of the EMS care for injured persons. Seriously injured patients often involve complex prehospital medical decision-making and care, yet most prehospital emergency practices lack outcome-based evidence to support or refute their use.11,12,45–51 Some evidence even suggests that certain prehospital practices may be harmful.52 The need for outcome-based evidence to refine EMS practices was a major impetus for development of the National EMS Research Agenda, for recommendations of sound methodological approaches to EMS research, and in producing a conceptual foundation for high quality EMS research.41,42,51,53–56 The ROC Epistry-Trauma will provide meaningful insight into the outcome-based assessment of EMS practices for major trauma patients at system-, agency-, and patient-levels to better define the optimal prehospital care for injured patients and a confidential method to assist local prehospital quality improvement and provider education processes. All of these goals are consistent with the recent Institute of Medicine recommendations for improving the state of EMS care.11
Facilitation of Prehospital Interventional Trials
While randomized controlled trials are widely recognized as the gold standard for informing optimal clinical care, trials evaluating prehospital trauma care are sparse. Although such research has rapidly accelerated the pace of evidence-based practices for other conditions, similar information is lacking for the prehospital care of trauma patients. Because the out-of-hospital setting is dynamic and difficult to adequately capture with existing data infrastructure in most systems, developing a mechanism of regularly capturing such information may assist in the ability to plan and conduct prehospital interventional trials. Such a database will allow critical insight into study design, sample size calculations, implementation barriers, identification of missed cases, biases in patient enrollment, generalizability of trauma trial results, and confounding factors in prehospital trials.
Defining the Burden of Injury
The true incidence of life threatening injury is elusive. Differences in estimates may reflect the lack of a common definition for trauma, incomplete episode identification, and selection bias inherent in existing data sources, among other reasons. The ROC Epistry-Trauma will provide less biased estimates of the incidence and survival of injured persons with physiologic derangement in the field, plus estimates of the number of traumatic deaths in the field. The societal and EMS burden from trauma is likely to be substantially higher than currently recognized when estimates include deaths at the scene of injury.57 The ROC Epistry-Trauma will provide the first opportunity to quantify the international extent of injury-related field deaths with an EMS response.
LIMITATIONS
Although many potential uses and benefits of the ROC Epistry-Trauma exist, there are limitations. First, the inclusion criteria are limited to injured persons with field-based physiologic derangement or death in the field. Based on previous studies, these inclusion criteria will exclude some patients with serious injuries and/or requiring specialized trauma resources. 17,19,21–26,29,30 However, using measures of physiologic derangement as inclusion criteria assures that a substantial portion of such patients will indeed have serious injury.
The working group also recognized the importance of injury severity measures. However, most commonly used measures of injury severity (e.g., Abbreviated Injury Scores [AIS],58 Injury Severity Score [ISS],34,59,60 International Classification of Disease-based Severity Score [ICISS]61) are based on information obtained during in-hospital evaluation and such hospital records are not consistently available for review (e.g., patients that die at the scene, non-transported patients, missing charts). Capturing such information from a large number of hospitals also requires a large amount of resources. The field inclusion criteria and mandatory variables represent a balance between the site resources required to adequately capture and characterize complex sequential EMS events and outcomes (i.e., feasibility) and the ability to rigorously address scientifically important prehospital injury questions.
For many sites, the geographic “footprint” of ROC Epistry-Trauma provides only a partial representation of air medical care. Although the geographic-based approach allows for population-based sampling, this feature may not be optimal for certain air medical research questions. Though air medical services play an important role in many EMS systems, further evaluating the utility, appropriateness, and indications for air medical transport may be limited using the Epistry data.
Finally, the ROC Epistry-Trauma may still underestimate the true rate of out-of-hospital mortality due to injury, as certain obvious traumatic deaths in the field do not receive an EMS medical response. Such events may include those with only police and/or medical examiner evaluation, the frequency of which likely differs between sites based on differences in local policy and regulations.
CONCLUSIONS
The ROC Epistry-Trauma is a North American, standardized, population-based data collection effort that matches prehospital information to hospital outcomes for injured patients evaluated by EMS providers. The project is intended to complement ongoing efforts to standardize both EMS and national in-hospital trauma registry data. The information collected in ROC Epistry-Trauma will provide important insight into defining prehospital best practices, facilitating public health efforts for injury prevention, and improving EMS quality improvement, education and training efforts. Taken together, the ROC Epistry-Trauma provides an opportunity to address gaps in our understanding of the prehospital care of injured persons and in turn potentially improve the outcomes of such patients.
Supplementary Material
ACKNOWLEDGMENTS
We would like to acknowledge and thank the development committee for ROC Epistry which, in addition to the authors, was comprised of the following individuals: Tom Terndrup and Shannon Stephens (Alabama); Ray Fowler (Dallas); Judy Powell and Graham Nichol (University of Washington); Michael Hartley and Melanie Kenney (Iowa); Chris Von Briesen (Milwaukee); Lisa Nesbit (Ottawa); Lori Kelly (Pittsburgh); Jonathan Larsen (Seattle/King County); Bruce Cameron, Jamie Frank, Jennifer Long, and Jim Lavery (Toronto); Sara Pennington, Dan Bishop and Dug Andrusiek (Vancouver). We also want to thank the many contributing EMS agencies, EMS providers, study coordinators, staff, and other investigators (see Appendix 1) for their willingness to participate in and support this project, and for their continued dedication to improving the EMS care and outcomes for their patients.
FUNDING
This study was supported by a cooperative agreement (5U01 HL077863) with the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, The Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the Heart and Stroke Foundation of Canada, and the American Heart Association.
Appendix 1
ROC Epistry contributors.
Appendix 2
ROC Epistry – Trauma data elements, definitions, and reference codes.
Appendix 3
ROC Epistry web-based data forms (trauma and cardiac arrest).
Footnotes
CONFLICT of INTEREST
There are no conflicts of interest between the authors and the content included in this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hoyert DL, Heron MP, Murphy SL, Kung H-C. Deaths: Final data for 2003. National Vital Statistics Reports. 2006;54:1–120. [PubMed] [Google Scholar]
- 2.Mock C, Quanash R, Krishnan R, Arreola-Risa C, Rivara F. Strengthening the prevention and care of injuries worldwide. Lancet. 2004;363:2172–2179. doi: 10.1016/S0140-6736(04)16510-0. [DOI] [PubMed] [Google Scholar]
- 3.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997 May 3;349(9061):1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 4.Anonymous. A league table of child deaths by injury in rich nations. Innocenti report card No. 2. Florence: Unicef Innocenti Research Centre; 2001. [Google Scholar]
- 5.Minino AM, Anderson RN, Fingerhut LA, Boudreault MA, Warner M. Deaths: Injuries, 2002. National Vital Statistics Reports. 2006;54:1–125. [PubMed] [Google Scholar]
- 6.Subramanian R. Research note, traffic safety facts: motor vehicle traffic crashes as a leading cause of death in the United States, 2000. National Center for Statistics and Analysis. 2003 October; DOT HS 809 661. [Google Scholar]
- 7.Rice DP, MacKenzie EJ Associates. Cost of injury in the United States: A report to Congress. San Francisco, CA: Institute for Health & Aging, University of California and Injury Prevention Center, The Johns Hopkins University; 1989. [Google Scholar]
- 8.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. [cited November 1, 2006];Web-based Injury Statistics Query and Reporting System (WISQARS) [online] Available from URL: http://www.cdc.gov/ncipc/wisqars.
- 9.Finkelstein EA, Corso PS, Miller TR, editors. Associates. Incidence and Economic Burden of Injuries in the United States. New York: Oxford University Press; 2006. [Google Scholar]
- 10.Thorpe KE, Florence CS, Joski P. Which medical conditions account for the rise in health care spending? Health Aff. 2004 Jul–Dec; Suppl Web Exclusives:W4-437–W4-445. doi: 10.1377/hlthaff.w4.437. [DOI] [PubMed] [Google Scholar]
- 11.Future of Emergency Care Series: Emergency Medical Services, At the Crossroads. Committee on the Future of Emergency Care in the United States Health System, Board on Health Care Services. Institute of Medicine of the National Academies. Washington, D.C.: The National Academy Press; 2006. [Google Scholar]
- 12.Spaite DW. The future of emergency care in the United States: The Institute of Medicine subcommittee on prehospital emergency medical services. Ann Emerg Med. 2006;48:126–130. doi: 10.1016/j.annemergmed.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 13.Mann NC, Guice K, Cassidy L, Wright D, Koury J. Are statewide trauma registries comparable? Reaching for a national trauma dataset. Acad Emerg Med. 2006;13:946–953. doi: 10.1197/j.aem.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 14.Morrison LJ, Sears GK, Rea TD, et al. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry–Cardiac Arrest. doi: 10.1016/j.resuscitation.2008.02.020. (Submitted - Resuscitation) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis DP, Garberson LA, Andrusiekc D, et al. A descriptive analysis of emergency medical service systems participating in a large, prehospital resuscitation research network. Prehospital Emergency Care. 2007;11:369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 16.Committee on Trauma. Resources for Optimal Care of the Injured Patient. Chicago, Ill: American College of Surgeons; 1999. [Google Scholar]
- 17.Cottington EM, Young JC, Shufflebarger CM, et al. The utility of physiologic status, injury site, and injury mechanism in identifying patients with major trauma. J Trauma. 1988;28:305–311. doi: 10.1097/00005373-198803000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Esposito TJ, Offner PJ, Jurkovich GJ, et al. Do out of hospital trauma center triage criteria identify major trauma victims? Archives of Surgery. 1995;130:171–176. doi: 10.1001/archsurg.1995.01430020061010. [DOI] [PubMed] [Google Scholar]
- 19.Kane G, Engelhardt R, Celentano J, et al. Empirical development and evaluation of out of hospital trauma triage instruments. J Trauma. 1985;25(6):482–489. doi: 10.1097/00005373-198506000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Norcross ED, Ford DW, Cooper ME, Zone-Smith L, Byrne TK, Yarbrough DR. Application of American college of surgeons’ field triage guidelines by pre-hospital personnel. J Am Coll Surg. 1995;181:539–544. [PubMed] [Google Scholar]
- 21.Henry MC, Hollander JE, Alicandro JM, Cassara G, O’Malley S, Thode HC., Jr Incremental benefit of individual American College of Surgeons trauma triage criteria. Acad Emerg Med. 1996 Nov;3(11):992–1000. doi: 10.1111/j.1553-2712.1996.tb03340.x. [DOI] [PubMed] [Google Scholar]
- 22.Knopp R, Yanagi A, Kallsen G, et al. Mechanism of injury and anatomic injury as criteria for out of hospital trauma triage. Ann Emerg Med. 1988;17:895–902. doi: 10.1016/s0196-0644(88)80666-8. [DOI] [PubMed] [Google Scholar]
- 23.Long WB, Bachulis BL, Hynes GD. Accuracy and relationship of mechanisms of injury, trauma score, and injury severity score in identifying major trauma. American Journal of Surgery. 1986;151:581–584. doi: 10.1016/0002-9610(86)90553-2. [DOI] [PubMed] [Google Scholar]
- 24.Bond RJ, Kortbeek JB, Preshaw RM. Field trauma triage: combining mechanism of injury with the prehospital index for an improved trauma triage tool. J Trauma. 1997;43:283–287. doi: 10.1097/00005373-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Lerner EB. Studies evaluating current field triage: 1966–2005. Prehospital Emergency Care. 2006;10:303–306. doi: 10.1080/10903120600723921. [DOI] [PubMed] [Google Scholar]
- 26.Engum SA, Mitchell MK, Scherer LR, et al. Prehospital Triage in the Injured Pediatric Patient. J Pediatr Surg. 2000;35:82–87. doi: 10.1016/s0022-3468(00)80019-6. [DOI] [PubMed] [Google Scholar]
- 27.Eichelberger MR, Gotschall CS, Sacco WJ, et al. A comparison of the trauma score, the revised trauma score, and the pediatric trauma score. Ann Emerg Med. 1989;18:1053–1058. doi: 10.1016/s0196-0644(89)80930-8. [DOI] [PubMed] [Google Scholar]
- 28.Chan BSH, Walker PJ, Cass DT. Urban trauma: An analysis of 1,116 paediatric cases. J Trauma. 1989;29:1540–1547. [PubMed] [Google Scholar]
- 29.Ramenofsky ML, Ramenofsky MB, Jurkovich GJ, Threadgill D, Dierking BH, Powell RW. The predictive validity of the pediatric trauma score. J Trauma. 1988;28:1038–1042. doi: 10.1097/00005373-198807000-00021. [DOI] [PubMed] [Google Scholar]
- 30.Kaufmann CR, Maier RV, Rivara FP, et al. Evaluation of the pediatric trauma score. JAMA. 1990;263:69–72. [PubMed] [Google Scholar]
- 31.Burd RS, Jang TS, Nair TS. Predicting hospital mortality among injured children using a national trauma database. J Trauma. 2006;60:792–801. doi: 10.1097/01.ta.0000214589.02515.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DiRusso SM, Sullivan T, Risucci D, Nealon PM, Slim M. Intubation of pediatric trauma patients in the field: predictor of negative outcome despite risk stratification. J Trauma. 2005;59:84–91. doi: 10.1097/01.ta.0000171462.28379.f3. [DOI] [PubMed] [Google Scholar]
- 33.Edil BH, Tuggle DW, Jones S, et al. Pediatric major resuscitation – respiratory compromise as a criterion for mandatory surgeon presence. J Pediatric Surgery. 2005;40:926–928. doi: 10.1016/j.jpedsurg.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 34.Baker SP, O'Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 35.Nayduch DA, Moylan J, Rutledge R, et al. Comparison of the ability of adult and pediatric trauma scores to predict pediatric outcome following major trauma. J Trauma. 1991;31(4):452–458. doi: 10.1097/00005373-199104000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Dawson DE. National Emergency Medical Services Information System (NEMSIS) Prehosp Emerg Care. 2006;10:314–316. doi: 10.1080/10903120600724200. [DOI] [PubMed] [Google Scholar]
- 37.Dick WF, Baskett PJ. Recommendations for uniform reporting of data following major trauma--the Utstein style. A report of a working party of the International Trauma Anaesthesia and Critical Care Society (ITACCS) Resuscitation. 1999;42(2):81–100. doi: 10.1016/s0300-9572(99)00102-1. [DOI] [PubMed] [Google Scholar]
- 38.Newgard CD, Hui J, Stamps-White P, Lewis RJ. Institutional variability in a minimal risk, population-based study: recognizing policy barriers to health services research. Health Services Research. 2005;40:1247–1258. doi: 10.1111/j.1475-6773.2005.00408.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Federal policy for the protection of human subjects. Final Rule. Federal Register. 1991;56:28003–28018. [PubMed] [Google Scholar]
- 40.Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council Canada, Social Sciences and Humanities Research Council of Canada. Tri-County Policy Statement: Ethical Conduct for Research Involving Humans. 1998. (with 2000, 2002, and 2005 amendments). [Google Scholar]
- 41.Maio RF, Garrison HG, Spaite DW, et al. Emergency medical services outcomes project I (EMSOP I): prioritizing conditions for outcomes research. Ann Emerg Med. 1999;33:423–432. doi: 10.1016/s0196-0644(99)70307-0. [DOI] [PubMed] [Google Scholar]
- 42.Spaite DW, Maio R, Garrison HG, et al. Emergency medical services outcomes project (EMSOP) II: developing the foundation and conceptual models for out-of-hospital outcomes research. Ann Emerg Med. 2001;31:657–663. doi: 10.1067/mem.2001.115215. [DOI] [PubMed] [Google Scholar]
- 43.The Health and Human Services Administration. Maternal Child Health Bureau. Emergency Medical Services for Children Program. National Trauma Registry for Children Planning Grants (Grants 1H72 MC00004 01 and 1H72 MC00002 01) Washington, DC: Emergency Medical Services for Children; 2002. [Google Scholar]
- 44.The Health and Human Services Administration. Health Resources and Services Administration. Trauma-Emergency Medical Services Systems Program. National Trauma Data Bank (NTDB): Data Element Identification. (03-MCHB-93B [DLC]) Washington, DC: Emergency Medical Services for Children; 2003. [Google Scholar]
- 45.Liberman M, Mulder D, Lavoie A, Denis R, Sampalis JS. Multicenter Canadian study of prehospital trauma care.[comment] Annals of Surgery. 2003;237(2):153–160. doi: 10.1097/01.SLA.0000048374.46952.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liberman M, Mulder D, Sampalis J. Advanced or basic life support for trauma: meta-analysis and critical review of the literature. Journal of Trauma-Injury Infection & Critical Care. 2000;49(4):584–599. doi: 10.1097/00005373-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 47.Sampalis JS, Lavoie A, Williams JI, Mulder DS, Kalina M. Impact of on-site care, prehospital time, and level of in-hospital care on survival in severely injured patients. J Trauma. 1993;34(2):252–261. doi: 10.1097/00005373-199302000-00014. [DOI] [PubMed] [Google Scholar]
- 48.Sethi D, Kwan I, Kelly AM, Roberts I, Bunn F. Advanced trauma life support training for ambulance crews. Cochrane Database Syst Rev. 2001;(2):CD003109. doi: 10.1002/14651858.CD003109. [DOI] [PubMed] [Google Scholar]
- 49.Nicholl J, Turner J. Effectiveness of a regional trauma system in reducing mortality from major trauma: before and after study.[comment] Bmj. 1997;315(7119):1349–1354. doi: 10.1136/bmj.315.7119.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rutledge R. 9-1-1 access and trauma deaths: a complex association. Ann Emerg Med. 1993;22:160–161. doi: 10.1016/s0196-0644(05)81332-0. [DOI] [PubMed] [Google Scholar]
- 51.National EMS Research Agenda. National Highway Traffic Safety Administration, Department of Transportation and Maternal and Child Health Bureau, Health Resources Services Administration, Department of Health and Human Services. 2001. Dec, [Google Scholar]
- 52.Wang HE, Yealy DM. Out-of-hospital endotracheal intubation: where are we? Ann Emerg Med. 2006;47:532–541. doi: 10.1016/j.annemergmed.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 53.Keim SM, Spaite DW, Maio RF, et al. Establishing the scope and methodologic approach to out-of-hospital outcomes and effectiveness research. Ann Emerg Med. 2004;11:1067–1073. doi: 10.1197/j.aem.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 54.McLean SA, Maio RF, Spaite DW, Garrison HG. Emergency medical services outcomes research: evaluating the effectiveness of prehospital care. Prehospital Emergency Care. 2002;6(2 Suppl):S52–S56. doi: 10.3109/10903120209102683. [DOI] [PubMed] [Google Scholar]
- 55.Garrison HG, Maio RF, Spaite DW, et al. Emergency medical services outcomes project III (EMSOP III): the role of risk adjustment in out-of-hospital outcomes research. Ann Emerg Med. 2002;40:79–88. doi: 10.1067/mem.2002.124758. [DOI] [PubMed] [Google Scholar]
- 56.Sedgwick ML, Dalziel K, Watson J, Carrington DJ, Cobbe SM. Performance of an established system of first responder out-of-hospital defibrillation. The results of the second year of the Heartstart Scotland Project in the 'Utstein Style'. Resuscitation. 1993;26(1):75–88. doi: 10.1016/0300-9572(93)90166-n. [DOI] [PubMed] [Google Scholar]
- 57.Brown LH, Khanna A, Hunt RC. Rural vs urban motor vehicle crash death rates: 20 years of FARS data. Prehosp Emerg Care. 2000 Jan–Mar;4(1):7–13. doi: 10.1080/10903120090941551. [DOI] [PubMed] [Google Scholar]
- 58.The Abbreviated Injury Scale, 1990 Revision, Update 98. Association for the Advancement of Automotive Medicine. 2001 [Google Scholar]
- 59.Eichelberger MR, Mangubat EA, Sacco WJ, Bowman LM, Lowenstein AD. Outcome analysis of blunt injury in children. J Trauma. 1988;28(8):1109–1117. doi: 10.1097/00005373-198808000-00002. [DOI] [PubMed] [Google Scholar]
- 60.Champion HR, Copes WS, Sacco WJ, et al. The major trauma outcome study: establishing national norms for trauma care. J Trauma. 1990;30:1356–1365. [PubMed] [Google Scholar]
- 61.Hannan EL, Waller CH, Farrell LS, Cayten CG. A comparison among the abilities of various injury severity measures to predict mortality with and without accompanying physiologic information. J Trauma. 2005 Feb;58(2):244–251. doi: 10.1097/01.ta.0000141995.44721.44. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.