SUMMARY
Atherosclerosis is a chronic inflammatory disease of large arteries in which lesion development preferentially occurs at vessel sites exposed to rapid changes in flow. We have previously shown that platelet endothelial cell adhesion molecule (PECAM-1), a surface receptor of the immunoglobulin superfamily, is involved in mechanosensing of rapid changes in flow. We wondered whether apolipoprotein E deficient (ApoE−/−) mice, predisposed to development of atheromas, would be protected from atherosclerosis by deficiency in PECAM-1. Using double knockout (DKO) mice for both PECAM-1 and ApoE (ApoE−/−/PECAM-1−/−) we found a significant reduction of sudanophilic lesions in their aortae compared to single knockout (SKO) (ApoE−/−/PECAM-1+/+) mice maintained on a high-fat Western diet. Immunostaining of aortic sinus cross sections demonstrated significantly lower ICAM-1 expression in DKO lesions compared with SKO lesions, and en face preparations of vessel regions subjected to disturbed and laminar flow showed less disruption of junctional connexin 43 in DKO than in SKO mice. Thus, PECAM-1 deficiency reduced the extent of lesions at the aortic arch and the aortic sinus, and lowered atherogenic indices. These results suggest that PECAM-1 is an important factor in the atherogenic changes seen in the ApoE-deficient mouse model and thus should be considered as a potential target for protection against atherosclerosis.
INTRODUCTION
Atherosclerotic lesions form at specific sites on blood vessels subject to disturbed blood flow, such as in the vicinity of branch points, the outer wall of bifurcations, and the inner wall of curvatures (DeBakey et al., 1985; Glagov et al., 1988; Ku et al., 1985; Chatzizisis et al., 2007). Endothelial cells play a critical role in sensing shear stress, the dragging frictional force created by flow, being ideally situated on the blood vessel lumen, and dysfunction of their mechanosensors is suggested to play a central role in the pathogenesis of atherosclerosis (Ross, 1993; Chatzizisis et al., 2007).
There is growing clinical evidence to suggest that the platelet endothelial cell adhesion molecule (PECAM-1/CD31), a 130kD glycoprotein expressed on the cell surface of monocytes, neutrophils, platelets, subsets of T cells and endothelial cells, plays a role in atherogenesis. A link has been established between certain PECAM-1 polymorphisms and increased risk for severe coronary heart disease and myocardial infarction (Wenzel et al., 1999; Sasaoka et al., 2001). Using knockout (KO) mice, we have previously shown that PECAM-1, localized to the cell-cell junction in vessel endothelium, is necessary for endothelial cells to sense increases in fluid shear stress and couple them with reactive dilatation of the vessel wall (Bagi et al., 2005). In addition, we have demonstrated that PECAM-1 is also complexed with nitric oxide synthase 3 (NOS 3/eNOS) and that this complex abruptly dissociates in response to changes in shear stress (Dusserre et al., 2004). In addition, PECAM-1 also undergoes phosphorylation in response to changes in shear stress (Fujiwara, 2006; Harada et al., 1995). These changes in shear stress are known to upregulate proinflammatory transcriptional activators such as nuclear factor-kappaB (NF-κB) and early growth response 1 (Egr-1) (Bao et al., 1999). In contrast, PECAM-1 deficient cells are reported to have impaired activation of NF-κB and specific kinases involved in cell signaling (Fleming et al., 2005; Tzima et al., 2005). Taken together, these studies suggest that PECAM-1 is important in the detection of mechanoreception (mechanical shear force) and mechanotransduction (conversion into chemical signals) by the endothelium, although the nature of its role is yet to be fully elucidated.
Atherosclerotic lesion development occurs at sites of the vessel that are subject to disturbed flow, i.e. areas where there are significant temporal changes in shear stress or flow [temporal gradients in shear stress (TGS)], and under conditions of low shear stress (DeBakey et al., 1985; Glagov et al., 1988; Ku et al., 1985). We wondered whether PECAM-1’s ability to detect these rapid changes in shear stress could translate disturbed flow stimuli into initiation of lesion development in the apolipoprotein E-deficient mouse model of atherosclerosis (ApoE−/−). Hence we tested whether PECAM-1 functioned as a proatherogenic, mechanoresponsive molecule in this model.
PECAM-1 is known to be involved in many different signaling pathways and may functionally couple with other cell junction molecules such as connexin 43 (Cx43). We have previously shown that unsteady or disturbed shear stress leads to enhanced and sustained expression of Cx43 (Bao et al., 2000). Cx43 trafficking appears to be an important proatherosclerotic event at sites of disturbed flow that are predisposed to lesions (DePaola et al., 1999). Since TGSs induce phosphorylation of mitogen-activated protein kinases (MAPK), and phosphorylation of Cx43 by MAPK is sufficient to disrupt communication at gap junctions (Bao et al., 2000; Warn-Cramer et al., 1998), we wondered if Cx43 expression, in areas of disturbed flow, would be altered by the absence of PECAM-1.
We investigated this hypothesis using single and double KO (SKO, DKO) mice combining the ApoE −/− mouse model of atherosclerosis, with and without the presence of the PECAM-1 gene. We found that DKO mice developed fewer lesions than SKO mice expressing PECAM-1. DKO mice demonstrated a decrease in lesion area at the aortic sinus and reduced endothelial expression of the intercellular adhesion molecule-1 (ICAM-1). Cx43 junctional staining was conserved in DKO mice. Thus, deficiency of PECAM-1 results in an atheroprotective effect and targeting PECAM-1 may represent a new targeting pathway to limit progression of atherosclerosis.
RESULTS
PECAM-1 deficient mice showed reduced atherosclerotic lesions
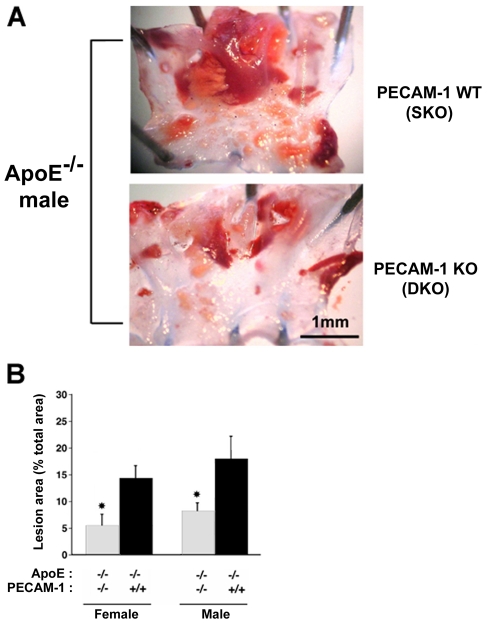
To examine the effect of genotype on development of atherosclerotic lesions in mouse aorta, perfusion-fixed aortic arches were stained with Sudan IV and the lesion area measured as a percentage of the total area of the aortic arch using Image J software. In all animals, at the aortic arch, the major lesion was observed on the lesser curvature, with minor lesions at the branches. However, average lesion area as a percentage of total arch area was significantly reduced (males, 54% reduction; females, 61% reduction) in DKO mice compared with SKO genotypes [male DKO: 8.27±1.30% (s.e.m.), n=16; male SKO: 18.07±4.21%, n=6; P<0.05; and female DKO: 5.55±1.79%, n=10; female SKO: 14.41±2.43%, n=9; P<0.05] (Fig. 1). At harvest, cholesterol analysis revealed no significant difference between the two genotypes maintained on a Western diet [DKO: 1747±872 mg/dL; SKO: 2131±679 mg/dL, data are mean of n=3 ± standard deviation (s.d.)]. DKO mice maintained on a normal chow diet for 11 months showed similar protection from aortic lesion development [DKO: 14.0±2.73% (s.e.m.), n=5; SKO: 22.3±2.14%, n=3; P<0.05, one tailed; data not shown].
Fig. 1. In male and female mice maintained on a Western diet, sudanophilic lesions are significantly reduced in DKO (ApoE−/−/PECAM-1−/−) compared with SKO (ApoE−/−/PECAM-1+/+) mice.
(A) Sudan IV staining of SKO (top) and DKO (bottom) male aortae. (B) Mean values of lesion area for male and female mice (+ s.e.m.), as a percentage of total aortic arch area, is significantly lower in the absence of PECAM-1 (DKO, grey bars) than in SKO mice (black bars) (*P<0.05).
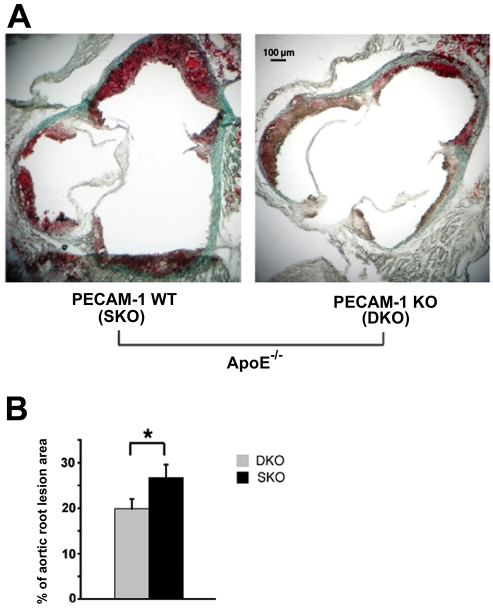
In order to more accurately assess a predisposition to form atherosclerotic lesions, we also investigated cross sections of the aortic sinus at the level of the aortic valve leaflets (Fig. 2). Total lesion areas, as a percentage of total aortal area, in Oil Red O stained aortal sections of DKO male mice were significantly lower than those of SKO male mice [DKO: 19.9±1.19% (s.e.m.), n=5; SKO: 26.7±1.92%, n=5; P<0.05].
Fig. 2. Oil Red O staining of aortal sections.
(A) In mice maintained on a Western diet, there is a significant reduction in aortic root lesion areas in DKO mice (ApoE−/− /PECAM-1−/−, right) compared with SKO mice (ApoE−/− /PECAM-1+/+, left). (B) Mean values of lesion areas (+ s.e.m.) in DKO (grey bars) and SKO (black bars) mice (*P<0.05; n=5 in each group).
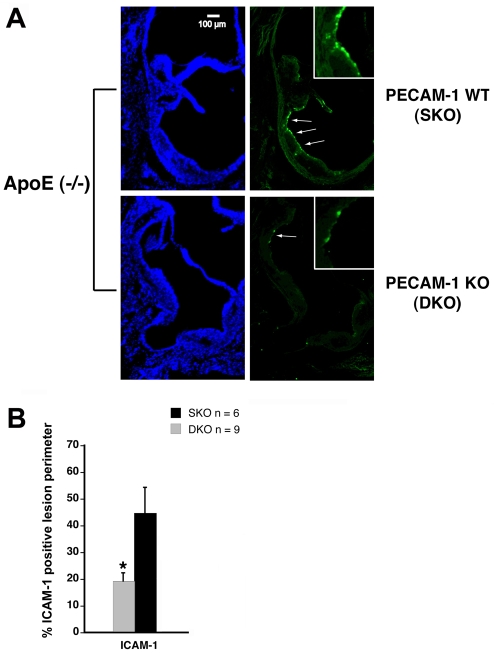
ICAM-1 immunostaining decreased in aortic sinus of PECAM-1 deficient mice
To investigate the expression of an endothelial marker associated with formation and progression of lesion sites (Bourdillon et al., 2000), the immunofluorescent localization of ICAM-1 was quantified at the aortic sinus of male mice, because the large and numerous aortic arch lesions degraded tissue quality and prevented accurate assessment. The extent of the lesion perimeter that was positive for ICAM-1 was significantly lower in DKO mice than in SKO mice [DKO: 19.3±3.53% (s.e.m.), n=9; SKO: 44.8±9.78%, n=6; P<0.05] (Fig. 3). Therefore, the absence of PECAM-1 in this atheroprone region led to the downregulation of ICAM-1.
Fig. 3. In mice maintained on a Western diet, peripheral lesion immunostaining for ICAM-1 in the aortic sinus of DKO mice (ApoE−/−, PECAM-1−/−) is significantly reduced compared with staining in SKO mice (ApoE−/−, PECAM-1+/+).
(A) Cell nuclei counterstain with DAPI (blue, left). Arrows indicate ICAM-1 immunolocalization along the lesion periphery (green; right). Insets are magnification of the staining noted by arrows. (B) The percentage of lesion perimeter positive for ICAM-1 is significantly lower in DKO mice than in SKO mice [DKO: 19.3±3.53% (s.e.m.), n=9; SKO: 44.8±9.78%, n=6; *P<0.05].
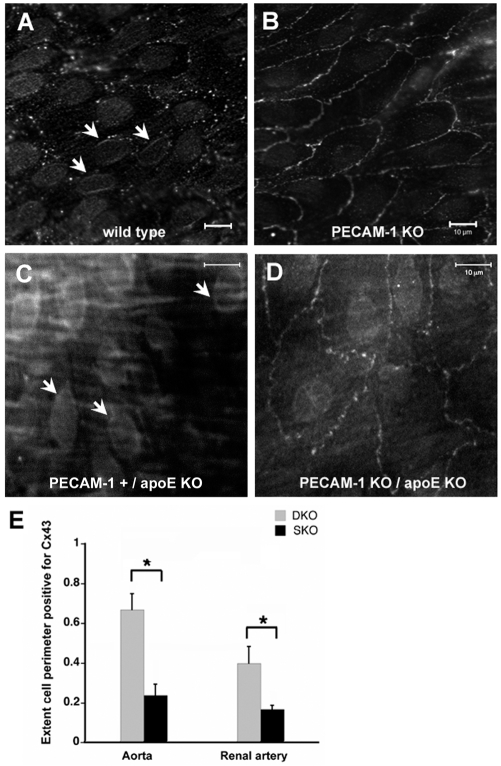
Increase of junctional Cx43 immunostaining in the descending aorta and at branched arteries of PECAM-1 KO mice
Cx43 trafficking appears to be an important proatherosclerotic event at sites of disturbed flow predisposed to lesion formation. To investigate endothelial Cx43 distribution, immunofluorescent localization of Cx43 was performed on sections of the descending aorta (assumed to be atheroprotective) and renal artery branch points (disturbed flow) of wild-type, PECAM-1 KO, ApoE-deficient (SKO) and DKO mice (Fig. 4). The first two groups of mice were maintained on a normal chow diet as opposed to the Western diet of SKO and DKO mice. In the aortae of PECAM-1 deficient mice, punctate staining for Cx43 was apparent at the cell-cell junctions, with occasional perinuclear staining (Fig. 4B). In the aorta of chowfed wild-type animals, Cx43 staining was found in the perinuclear area, with relatively fewer patches of junctional Cx43 staining (Fig. 4A). Similar results were observed in ApoE-deficient mice, with reduced disruption to Cx43 distribution at the cell-cell junction in DKO mice compared with SKO mice (Fig. 4C,D). The extent of the cell perimeter that was positive for Cx43 was significantly higher in the descending aorta (area of laminar shear stress) of DKO mice than in SKO mice [DKO: 0.67±0.09 (s.e.m.), n=3; SKO: 0.24±0.17, n=4; P<0.05] (Fig. 4E). In addition, in the renal artery branches (area of TGS), where smaller lesions permitted staining, junctional Cx43 was also significantly higher in the renal artery of DKO mice compared with SKO mice [DKO: 0.40±0.08 (s.e.m.), n=4; SKO: 0.17±0.02, n=4; P<0.05, one-tailed t-test].
Fig. 4. Cx43 is primarily found on the endothelial plasma membrane of wild-type, chow-fed PECAM-1 KO mice.
(A) In the descending aorta, Cx43 can be found both in the perinuclear areas (white arrows) and in a punctate distribution on the plasma membrane of endothelial cells. (B) In chow-fed PECAM-1 KO mice, Cx43 staining is uniformly expressed on the plasma membrane. (C–D) Likewise, in the ApoE KO model with mice maintained on a Western diet, less disruption to the punctate distribution of Cx43 at the cell-cell junction is found when comparing renal artery branches from PECAM-1 deficient mice (ApoE−/− /PECAM-1−/−, D) with those from SKO mice (ApoE−/− /PECAM-1+/+, C). Loss of junctional staining in PECAM KO mice was usually accompanied by an increase in perinuclear staining (white arrows). (E) The extent of Cx43-positive cell periphery in both aortae and renal artery branches from DKO and SKO mice (*P<0.05). Bars, 10 μm (A–D).
DISCUSSION
PECAM-1 was shown to be important in the development of lesions at aortic sites susceptible to atherosclerosis in the ApoE-deficient mouse. The downregulation of ICAM-1 in endothelial cells at the lesion periphery, and reduced disruption of Cx43 junctional staining at arterial branch points and in the descending aorta in PECAM-1 deficient mice, further suggest a role of PECAM-1 in atherogenesis.
In mammals, although risk factors such as a high-fat diet affect the whole circulation, the development of atherosclerotic plaques is highly focal and correlates with the type of local hemodynamic forces (DeBakey et al., 1985; Frangos et al., 1999; Chatzizisis et al., 2007). For instance, long-term exposure to laminar shear stress profiles is anti-atherogenic (Resnick et al., 1997; Topper et al., 1996). In contrast, pulsatile or oscillatory shear stresses acting on endothelium modulate pro-inflammatory gene expression (Bao et al., 1999; Garcia-Cardena et al., 2001). It follows that the rapid changes in shear stress (TGS) and low mean shear stress occurring at curves and bifurcations of the aorta, and at the branch points to smaller arteries, are considered to be proatherogenic flow profiles and these areas develop neointimas (early lesions) over time (Cornhill et al., 1990; Dewey et al., 1981; Friedman et al., 1975; Zarins et al., 1983). In the mouse aortic arch, the variations in wall shear stress using computational fluid dynamics are as much as 600 dynes per square centimeter in 50 milliseconds – a temporal gradient that is 150-fold higher than in human aortae (Suo et al., 2007; Weinberg and Ethier, 2007). Higher temporal gradients in the mouse aortic arch may explain our observation of lesions in the inner curvature, which is relatively lesion-free in the human (DeBakey et al., 1985). Since PECAM-1 is known to mediate mechanoreception and mechanotransduction of temporal gradients in shear stress (Bagi et al., 2005; Dusserre et al., 2004), the absence of PECAM-1 in DKO mice may render these areas less sensitive to shear stress, and thus reduce the pro-inflammatory phenotype.
As atherosclerosis is now widely recognized as a chronic inflammatory disease (Hope and Meredith, 2003), we cannot rule out the possibility that the absence of PECAM-1 on leukocytes contributes to the atheroprotective effect in PECAM-1 KO mice. The lack of PECAM-1 definitely impairs leukocyte transendothelial migration, yet another explanation could be the lack of survival signals on PECAM-1 deficient T cells (Gao et al., 2003). However, it is unlikely to be the major reason for the atheroprotective effects we observed here, since leukocyte transmigration in response to various inflammatory stimuli is largely unaffected in PECAM-1 KO mice generated on the C57BL/6 background (Schenkel et al., 2004). In addition, the downregulation of ICAM-1 at the aortic sinus in PECAM-1 deficient mice is not readily explained by the absence of leukocyte transmigration.
ICAM-1 upregulation is often linked to sites of unsteady flow (Endres et al., 1997; Nakashima et al., 1998). Studies on endothelial monolayers show that TGS, such as oscillatory flow, upregulates ICAM-1 expression (Chappell et al., 1998). Since TGS upregulates the pro-inflammatory transcription factor NF-κB in endothelial cells (Bao et al., 1999), and NF-κB transcriptionally regulates ICAM-1 (Chen et al., 1995; Fakler et al., 2000; Read et al., 1995; Voraberger et al., 1991) then PECAM-1 may mediate TGS-induced ICAM-1 upregulation via NF-κB activation. This is consistent with the causal link between PECAM-1 and NF-κB, which revealed the absence of NF-κB activation near bifurcations of PECAM-1 KO aortae (Tzima et al., 2005).
Aortal tissue has been demonstrated to show positive staining for Cx43 at cell-cell junctions (Yeh et al., 2003), and mechanical strain and fluid shear stress are known modulators of Cx43 expression (Cowan et al., 1998; DePaola et al., 1999; Thi et al., 2003). An upregulation of Cx43 gene expression has also been demonstrated in endothelial cells exposed to TGS (Bao et al., 2000). However, the upregulated Cx43 protein appeared to be redistributed to perinuclear and cytoplasmic compartments and did not result in an increased concentration of gap junctional protein (Li et al., 2002). The disruption of Cx43 junctional communication (via translocation from cell borders to the cytosol) appears to be an important pro-atherosclerotic event at sites of unsteady flow that are predisposed to develop lesions (DePaola et al., 1999). In this study we found that PECAM-1 KO mice demonstrated greater conservation of Cx43 junctional staining compared to SKO or wild-type tissue. Therefore, the presence of PECAM-1 appears to aid translocation of Cx43 from the cell-cell junction to intracellular sites. By disruption of Cx43, a protein known to assist the cell junctional movement of small molecules and ions, gradients in shear stress will likely disrupt cell-cell communication. Together, the decreased levels of cytosolic Cx43 and increased amount of junctional Cx43 suggest that PECAM-1 KO mice may be insensitive to TGS. Thus, the present data would support the role of PECAM-1 in mediating TGS-induced atherogenesis.
In summary, the decrease in lesion areas observed in PECAM-1 deficient mice support the hypothesis that changes in shear stress, which occur in atheroprone regions of the arterial circulation, are sensed by PECAM-1 and that PECAM-1 promotes atherosclerotic lesions and increases atherogenic indices. We suggest, based on the present data, that absence of PECAM-1 delays onset of atheroma development, but does not prevent its induction. In this manner, PECAM-1 dependent mechanisms are critical to full lesion progression and so PECAM-1 has considerable potential as a candidate target to limit the course of the disease.
METHODS
Animals
The animal use protocols for these studies were pre-approved by the Institutional Animal Care and Use Committee (IACUC) at the La Jolla Bioengineering Institute. All mice (mus musculus), except for those fasted overnight, had access to food and water ad libitum. ApoE-deficient mice with a B6.129 background (B6.129P2ApoEtm1Unc) obtained from Jackson Laboratory (Bar Harbor, USA) were backcrossed 10 times onto C57BL/6J mice. Similarly, PECAM-1 homozygotes (B6.129SPecam1Gt(VICTR20)12Lex and B6.129SF2/J cross; Jackson Laboratory) were backcrossed onto C57BL/6 mice for six generations. ApoE−/− and PECAM-1−/−C57BL/6 mice were then bred to obtain the F2 generation (ApoE−/−PECAM-1−/+), which were then bred together to generate the SKO and DKO littermates used in this study. Genotypes were determined by PCR. At weaning, littermates were placed on a cholate-free high cholesterol Western diet (Teklad adjusted calories diet TD 88137: 21.2% fat wt/wt, 0.2% cholesterol wt/wt) for 12 weeks. Cholesterol analysis of heparinized plasma from terminal bleeds of SKO and DKO fasted male mice was performed by Esoterix (Labcorp, NC). A separate group of littermates were maintained on a normal chow diet from weaning until 11 months of age. A total of 80 mice (including breeders) were used in this study. Terminal weight measurements did not differ significantly by genotype for either male or female groups (male: SKO 38.9±1.13 [standard error of mean (s.e.m.)], n=10; DKO 38.1±1.04, n=23; female: SKO 23.7±0.98, n=12; DKO 23.7±1.36, n=14).
PECAM-1 and ApoE genotyping by PCR
Tail genomic DNA was prepared for PCR using REDExtract-N-Amp Tissue PCR kit (Sigma, St Louis, MO). For the PECAM-1 wild-type (WT) allele, a forward primer (5′-CAGCCACTGTGTGAGACACAAAGGCAAG-3′) and reverse primer (5′-ACCACACACCCAGCAACCCTTTCAGAC-3′) were used. For the KO allele, the forward primer was based on the long terminal repeat (LTR) region of the insertion vector (5′-AAATGGCGTTACTTAAGCTAGCTTGC-3′) and the reverse primer was the same as for the WT allele. These primers amplify a <350 base pair (bp) DNA fragment from the WT allele and a <230 bp fragment from the KO allele. For ApoE, a forward primer (5′-GCCTAGCCGAGGGAGAGCCG-3′) corresponding to the exon 3 genomic sequence was used for PCR with a reverse primer from exon 3 (5′-TGTGACTTGGGAGCTCTGCAGC-3′) to identify the WT allele (155 bp PCR product). To identify the KO allele, a forward primer was used for PCR, together with a reverse primer (5′-GCCGCCCCGACTGCATCT-3′) corresponding to a region within the vector that was used to disrupt the ApoE gene (245 bp PCR product). This strategy was used since both KOs have the neomycin gene.
Sudan IV staining of aortic arch
Mice were anesthetized with ketamine (90 mg/kg)/xylazine (10 mg/kg), intraperitoneally (IP), and monitored until negative to toe pinch. After injection of heparin (1 ml) into the ventricle, mice were perfused with ice-cold Stefanini buffer for 5 minutes (2% paraformaldehyde and 15% picric acid in 0.1 M phosphate buffer, pH 7.6). Aortas were carefully collected from heart to iliac bifurcation and stored in buffer at 4°C. Aortic arches were cleaned, opened longitudinally along the outer curvature, and stained with Sudan IV (0.5% w/v in 1:1 mix of 70% ethanol: 100% acetone) to reveal lipids. The aortic arch is the site of the most significant atherosclerotic lesions in the Apo-E deficient C57BL/6 mouse on a Western diet (Nakashima et al., 1998). Briefly, the aortas were washed in 70% ethanol for 10 minutes, stained in Sudan IV for 60 minutes at room temperature (RT) and rinsed in 70% ethanol for 10 minutes. Stained arches were stored in 4% formaldehyde solution in PBS at 4°C until imaged. The arch was pinned to the gel of a dissecting dish and photographed under a stereomicroscope. Sudanophilic lesions and total arch areas were quantified using Image J software (Rasband, W.S., ImageJ, US National Institutes of Health, Bethesda, MD, http://rsb.info.nih.gov/ij/, 1997–2006).
Oil Red O staining and ICAM-1 immunostaining of aortic root
After harvesting aortas, the heart and aortic root were embedded in O.C.T. cryoembedding media (Sakura Finetek, Torrance, CA) and snap frozen in a hexane-chilling bath. Sections (8 μm) were generated of the aortic sinus at the level of the aortic valve leaflets. Oil Red O solution (0.5% w/v in 1:1 mix of 70% ethanol: 100% acetone) was used to stain sections for 5 minutes at RT, before differentiating in 70% ethanol and washing in phosphate buffer saline (PBS). Image J software was used to measure total lesion area relative to total aortal area to adjust for oblique sectioning. For immunostaining, sections were washed in PBS, blocked in Triton/PBS block (5% donkey serum in 0.01% Triton in PBS) and incubated in rat anti-ICAM-1 (Santa Cruz Biotechnology, Santa Cruz, CA), diluted 1/25 in Triton/PBS block, for 1 hour at RT in a humidified chamber. After washing in PBS, slides were incubated in donkey anti-rat or anti-goat Alexa 488 antibodies from Molecular Probes (Invitrogen, Carlsbad, CA), diluted 1/50 in Triton/PBS block, for 1 hour at RT. Sections were counterstained with DAPI (1/1000) for 2 minutes. Slides were mounted in Fluoromount (EMS, Hatfield, PA). Negative controls without primary antibody are shown in the supplementary material (supplementary material Fig. S1).
En face, high-power fluorescence microscopy of Cx43 immunostaining of the luminal surface of aortas and renal artery branches
Aortas from male mice, perfused as above, were carefully dissected; cross-sectional segments were cut and opened longitudinally. Branches (renal artery bifurcation) and blood flow direction were recorded. Permeabilization and staining steps were similar to those for ICAM-1 immunolocalization on aortic root sections, apart from a pre-incubation step in 2% sodium borohydride in PBS for 30 minutes to reduce autofluorescence. For immunostaining, tissues were incubated in rabbit anti-Cx43 (Abcam, Cambridge, MA) in Triton/PBS block for 1 hour at RT. A negative control (without primary antibody) was included (supplementary material Fig. S2). Preparations were mounted, luminal side up, in Gelvatol.
Confocal microscopy analysis
Slides were examined under a confocal fluorescent microscope (Zeiss Pascal LSM 5, Carl Zeiss, Jena, Germany) equipped with Plan-NEOFLUAR 100/1.3 objective and images were analyzed using the Zeiss LSM Image Browser. The extent of cell perimeter that was positive for Cx43, as a proportion of the total cell periphery, was measured for aortal and renal artery DKO and SKO tissues. Areas containing disorganized condensed nuclei signified plaque formation (Nakashima et al., 1998) and were avoided in the assessment of junctional staining.
Data analysis
Data are presented as means ± s.e.m. of the indicated number of observations. Statistical comparisons between groups were performed using two-tailed t-tests, unless otherwise stated, with a significance level of P<0.05.
Supplementary Material
ACKNOWLEDGEMENTS
This work was supported by a grant from NIH HL40696 (to J.A.F.).
Footnotes
AUTHOR CONTRIBUTIONS
H.Y.S., B.M., K.S.B., S.Y. and J.-C.Y. performed the experiments, H.Y.S., B.M. and J.A.F. prepared the manuscript, and J.A.F. designed the experiments and secured the funding.
COMPETING INTERESTS
The authors declare no competing financial interests.
SUPPLEMENTARY MATERIAL
Supplementary material for this article is available at http://dmm.biologists.org/content/1/2-3/175/suppl/DC1
REFERENCES
- Bagi Z, Frangos JA, Yeh JC, White CR, Kaley G, Koller A. (2005). PECAM-1 mediates NO-dependent dilation of arterioles to high temporal gradients of shear stress. Arterioscler. Thromb. Vasc. Biol. 25, 1590–1595 [DOI] [PubMed] [Google Scholar]
- Bao X, Lu C, Frangos JA. (1999). Temporal gradient in shear but not steady shear stress induces PDGF-A and MCP-1 expression in endothelial cells: role of NO, NF kappa B, and egr-1. Arterioscler. Thromb. Vasc. Biol. 19, 996–1003 [DOI] [PubMed] [Google Scholar]
- Bao X, Clark CB, Frangos JA. (2000). Temporal gradient in shear-induced signaling pathway: involvement of MAP kinase, c-fos, and connexin43. Am. J. Physiol. Heart Circ. Physiol. 278, H1598–H1605 [DOI] [PubMed] [Google Scholar]
- Bourdillon MC, Poston RN, Covacho C, Chignier E, Bricca G, McGregor JL. (2000). ICAM-1 deficiency reduces atherosclerotic lesions in double-knockout mice (ApoE(–/–)/ICAM-1(–/–)) fed a fat or a chow diet. Arterioscler. Thromb. Vasc. Biol. 20, 2630–2635 [DOI] [PubMed] [Google Scholar]
- Chappell DC, Varner SE, Nerem RM, Medford RM, Alexander RW. (1998). Oscillatory shear stress stimulates adhesion molecule expression in cultured human endothelium. Circ. Res. 82, 532–539 [DOI] [PubMed] [Google Scholar]
- Chatzizisis YS, Coskun AU, Jonas M, Edelman ER, Feldman CL, Stone PH. (2007). Role of endothelial shear stress in the natural history of coronary atherosclerosis and vascular remodeling. J. Am. Coll. Cardiol. 49, 2379–2393 [DOI] [PubMed] [Google Scholar]
- Chen CC, Rosenbloom CL, Anderson DC, Manning AM. (1995). Selective inhibition of E-selectin, vascular cell adhesion molecule-1, and intercellular adhesion molecule-1 expression by inhibitors of I kappa B-alpha phosphorylation. J. Immunol. 155, 3538–3545 [PubMed] [Google Scholar]
- Cornhill JF, Herderick EE, Stary HC. (1990). Topography of human aortic sudanophilic lesions. Monogr. Atheroscler. 15, 13–19 [PubMed] [Google Scholar]
- Cowan DB, Lye SJ, Langille BL. (1998). Regulation of vascular connexin43 gene expression by mechanical loads. Circ. Res. 82, 786–793 [DOI] [PubMed] [Google Scholar]
- DeBakey ME, Lawrie GM, Glaeser DH. (1985). Patterns of atherosclerosis and their surgical significance. Ann. Surg. 201, 115–131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePaola N, Davies PF, Pritchard WF, Jr, Florez L, Harbeck N, Polacek DC. (1999). Spatial and temporal regulation of gap junction connexin43 in vascular endothelial cells exposed to controlled disturbed flows in vitro. Proc. Natl. Acad. Sci. USA 96, 3154–3159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewey CF, Jr, Bussolari SR, Gimbrone MA, Jr, Davies PF. (1981). The dynamic response of vascular endothelial cells to fluid shear stress. J. Biomech. Eng. 103, 177–185 [DOI] [PubMed] [Google Scholar]
- Dusserre N, L’Heureux N, Bell KS, Stevens HY, Yeh J, Otte LA, Loufrani L, Frangos JA. (2004). PECAM-1 interacts with nitric oxide synthase in human endothelial cells: implication for flow-induced nitric oxide synthase activation. Arterioscler. Thromb. Vasc. Biol. 24, 1796–1802 [DOI] [PubMed] [Google Scholar]
- Endres M, Laufs U, Merz H, Kaps M. (1997). Focal expression of intercellular adhesion molecule-1 in the human carotid bifurcation. Stroke 28, 77–82 [DOI] [PubMed] [Google Scholar]
- Fakler CR, Wu B, McMicken HW, Geske RS, Welty SE. (2000). Molecular mechanisms of lipopolysaccharide induced ICAM-1 expression in A549 cells. Inflamm. Res. 49, 63–72 [DOI] [PubMed] [Google Scholar]
- Fleming I, Fisslthaler B, Dixit M, Busse R. (2005). Role of PECAM-1 in the shear-stress-induced activation of Akt and the endothelial nitric oxide synthase (eNOS) in endothelial cells. J. Cell Sci. 118, 4103–4111 [DOI] [PubMed] [Google Scholar]
- Frangos SG, Gahtan V, Sumpio B. (1999). Localization of atherosclerosis: role of hemodynamics. Arch. Surg. 134, 1142–1149 [DOI] [PubMed] [Google Scholar]
- Friedman MH, O’Brien V, Ehrlich LW. (1975). Calculations of pulsatile flow through a branch: implications for the hemodynamics of atherogenesis. Circ. Res. 36, 277–285 [DOI] [PubMed] [Google Scholar]
- Fujiwara K. (2006). Platelet endothelial cell adhesion molecule-1 and mechanotransduction in vascular endothelial cells. J. Intern. Med. 259, 373–380 [DOI] [PubMed] [Google Scholar]
- Gao C, Sun W, Christofidou-Solomidou M, Sawada M, Newman DK, Bergom C, Albelda SM, Matsuyama S, Newman PJ. (2003). PECAM-1 functions as a specific and potent inhibitor of mitochondrial-dependent apoptosis. Blood 102, 169–179 [DOI] [PubMed] [Google Scholar]
- Garcia-Cardena G, Comander J, Anderson KR, Blackman BR, Gimbrone MA., Jr (2001). Biomechanical activation of vascular endothelium as a determinant of its functional phenotype. Proc. Natl. Acad. Sci. USA 98, 4478–4485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glagov S, Zarins C, Giddens DP, Ku DN. (1988). Hemodynamics and atherosclerosis. Insights and perspectives gained from studies of human arteries. Arch. Pathol. Lab. Med. 112, 1018–1031 [PubMed] [Google Scholar]
- Harada N, Masuda M, Fujiwara K. (1995). Fluid flow and osmotic stress induce tyrosine phosphorylation of an endothelial cell 128 kDa surface glycoprotein. Biochem. Biophys. Res. Commun. 214, 69–74 [DOI] [PubMed] [Google Scholar]
- Hope SA, Meredith IT. (2003). Cellular adhesion molecules and cardiovascular disease. Part I. Their expression and role in atherogenesis. Intern. Med. J. 33, 380–386 [DOI] [PubMed] [Google Scholar]
- Ku DN, Giddens DP, Zarins CK, Glagov S. (1985). Pulsatile flow and atherosclerosis in the human carotid bifurcation. Positive correlation between plaque location and low oscillating shear stress. Arteriosclerosis 5, 293–302 [DOI] [PubMed] [Google Scholar]
- Li H, Brodsky S, Kumari S, Valiunas V, Brink P, Kaide J, Nasjletti A, Goligorsky MS. (2002). Paradoxical overexpression and translocation of connexin43 in homocysteine-treated endothelial cells. Am. J. Physiol. Heart Circ. Physiol. 282, H2124–H2133 [DOI] [PubMed] [Google Scholar]
- Nakashima Y, Raines EW, Plump AS, Breslow JL, Ross R. (1998). Upregulation of VCAM-1 and ICAM-1 at atherosclerosis-prone sites on the endothelium in the ApoE-deficient mouse. Arterioscler. Thromb. Vasc. Biol. 18, 842–851 [DOI] [PubMed] [Google Scholar]
- Read MA, Neish AS, Luscinskas FW, Palombella VJ, Maniatis T, Collins T. (1995). The proteasome pathway is required for cytokine-induced endothelial-leukocyte adhesion molecule expression. Immunity 2, 493–506 [DOI] [PubMed] [Google Scholar]
- Resnick N, Yahav H, Khachigian LM, Collins T, Anderson KR, Dewey FC, Gimbrone MA., Jr (1997). Endothelial gene regulation by laminar shear stress. Adv. Exp. Med. Biol. 430, 155–164 [DOI] [PubMed] [Google Scholar]
- Ross R. (1993). The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 362, 801–809 [DOI] [PubMed] [Google Scholar]
- Sasaoka T, Kimura A, Hohta SA, Fukuda N, Kurosawa T, Izumi T. (2001). Polymorphisms in the platelet-endothelial cell adhesion molecule-1 (PECAM-1) gene, Asn563Ser and Gly670Arg, associated with myocardial infarction in the Japanese. Ann. N. Y. Acad Sci. 947, 259–270 [DOI] [PubMed] [Google Scholar]
- Schenkel AR, Chew TW, Muller WA. (2004). Platelet endothelial cell adhesion molecule deficiency or blockade significantly reduces leukocyte emigration in a majority of mouse strains. J. Immunol. 173, 6403–6408 [DOI] [PubMed] [Google Scholar]
- Suo J, Ferrara DE, Sorescu D, Guldberg RE, Taylor WR, Giddens DP. (2007). Hemodynamic shear stresses in mouse aortas: implications for atherogenesis. Arterioscler. Thromb. Vasc. Biol. 27, 346–351 [DOI] [PubMed] [Google Scholar]
- Thi MM, Kojima T, Cowin SC, Weinbaum S, Spray DC. (2003). Fluid shear stress remodels expression and function of junctional proteins in culture bone cells. Am. J. Physiol. Cell Physiol. 284, C389–C403 [DOI] [PubMed] [Google Scholar]
- Topper JN, Cai J, Falb D, Gimbrone MA., Jr (1996). Identification of vascular endothelial genes differentially responsive to fluid mechanical stimuli: cyclooxygenase-2, manganese superoxide dismutase, and endothelial cell nitric oxide synthase are selectively up-regulated by steady laminar shear stress. Proc. Natl. Acad. Sci. USA 93, 10417–10422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzima E, Irani-Tehrani M, Kiosses WB, Dejana E, Schultz DA, Engelhardt B, Cao G, DeLisser H, Schwartz MA. (2005). A mechanosensory complex that mediates the endothelial cell response to fluid shear stress. Nature 437, 426–431 [DOI] [PubMed] [Google Scholar]
- Voraberger G, Schafer R, Stratowa C. (1991). Cloning of the human gene for intercellular adhesion molecule 1 and analysis of its 5′-regulatory region. Induction by cytokines and phorbol ester. J. Immunol. 147, 2777–2786 [PubMed] [Google Scholar]
- Warn-Cramer BJ, Cottrell GT, Burt JM, Lau AF. (1998). Regulation of connexin-43 gap junctional intercellular communication by mitogen-activated protein kinase. J. Biol. Chem. 273, 9188–9196 [DOI] [PubMed] [Google Scholar]
- Weinberg PD, Ethier CR. (2007). Twenty-fold difference in hemodynamic wall shear stress between murine and human aortas. J. Biomech. 40, 1594–1598 [DOI] [PubMed] [Google Scholar]
- Wenzel K, Baumann G, Felix SB. (1999). The homozygous combination of Leu125Val and Ser563Asn polymorphisms in the PECAM1 (CD31) gene is associated with early severe coronary heart disease. Hum. Mutat. 14, 545. [DOI] [PubMed] [Google Scholar]
- Yeh HI, Lu CS, Wu YJ, Chen CC, Hong RC, Ko YS, Shiao MS, Severs NJ, Tsai CH. (2003). Reduced expression of endothelial connexin37 and connexin40 in hyperlipidemic mice: recovery of connexin37 after 7-day simvastatin treatment. Arterioscler. Thromb. Vasc. Biol. 23, 1391–1397 [DOI] [PubMed] [Google Scholar]
- Zarins CK, Giddens DP, Bharadvaj BK, Sottiurai VS, Mabon RF, Glagov S. (1983). Carotid bifurcation atherosclerosis. Quantitative correlation of plaque localization with flow velocity profiles and wall shear stress. Circ. Res. 53, 502–514 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.