Abstract
OBJECTIVES
Traumatic brain injury is a leading cause of death in children. On the basis of evidence of better outcomes, the American College of Surgery Committee on Trauma recommends that children with severe traumatic brain injury receive care at high-level trauma centers. We assessed rates of adherence to these recommendations and factors associated with adherence.
METHODS
We studied population and hospital discharge data from 2001 from all of the health care referral regions (n = 68) in 6 US states (Florida, Massachusetts, New Jersey, New York, Texas, and Virginia). We identified children with severe traumatic brain injury by using International Classification of Diseases, Ninth Revision, Clinical Modification, codes and American College of Surgery Committee on Trauma criteria. We defined “high-level centers” as either level I or pediatric trauma centers. We considered an area to be well regionalized if ≥90% of severe traumatic brain injury hospitalizations were in high-level centers. We also explored how use of level II trauma centers affected rates of care at high-level centers.
RESULTS
Of 2117 admissions for severe pediatric traumatic brain injury, 67.3% were in high-level centers, and 87.3% were in either high-level or level II centers. Among states, 56.4% to 93.6% of severe traumatic brain injury admissions were in high-level centers. Only 2 states, Massachusetts and Virginia, were well regionalized. Across health care referral regions, 0% to 100% of severe traumatic brain injury admissions were in high-level centers, and only 19.1% of health care referral regions were well regionalized. Only a weak relationship existed between the distance to the nearest high-level center and regionalization. The age of statewide trauma systems had no relationship to the extent of regionalization.
CONCLUSIONS
Despite evidence for improved outcomes of severely injured children admitted to high-level trauma centers, we found that almost one third of the children with severe traumatic brain injury failed to receive care in such centers. Only 2 of 6 states and less than one fifth of 68 health care referral regions were well regionalized. This study highlights problems with current pediatric trauma care that can serve as a basis for additional research and health care policy.
Keywords: trauma, triage, brain injury, regionalization, pediatric
PEDIATRIC TRAUMATIC BRAIN injury (TBI) results in >400 000 emergency department visits, 37 000 hospitalizations, and ∼2700 deaths each year in the United States.1 Survival from severe traumatic injury in general and severe TBI in particular is improved by prompt, coordinated, specialized care.2-14 Over the past 40 years, US public health policy has supported coordinated, expert trauma care through the implementation of statewide regionalized trauma systems.15 More than three quarters of US states now have these systems.16
There are 2 essential components of a regionalized trauma system.17 First, hospitals must be categorized on the basis of the complexity of trauma care they provide, with expensive resources and expertise needed for the highest level of care concentrated in select centers.12,18 Second, patients must be triaged and transported to a facility appropriate to the nature and severity of their injury. The American College of Surgeons Committee on Trauma (ACS COT) issues criteria for categorizing hospitals and guidelines for triage to these hospitals.18 Specifically, ACS COT recommends that ≥90% of children with severe TBI be treated at either level I or pediatric trauma centers; the recommendation was based on studies that have demonstrated improved outcomes at these centers.10,11,18-21
Unfortunately, there are few data on adherence to ACS COT triage guidelines, and no study has focused on severe pediatric TBI. The objectives of this study were to identify the extent to which children with severe TBI received care at high-level centers and to explore factors associated with admission to these centers.
PATIENTS AND METHODS
Definitions
We defined “high-level center” as either a level I or pediatric trauma center. In our primary analysis, we calculated the proportion of all of the hospitalizations for severe pediatric TBI that occurred at high-level centers in 6 states and the health care referral regions (HRRs) within the states. We classified states and HRRs by the extent to which children received high-level trauma care. States or HRRs with ≥90% of hospitalizations for severe TBI at high-level centers were “well regionalized,” those with 80% to 89% of hospitalizations at high-level centers were “moderately regionalized,” and those with <80% were “poorly regionalized.” We computed straight-line distances between the centers of the home zip code of each patient and the zip codes of the nearest hospital, the admitting hospital, and the closest high-level center using a standard geometric formula (www.mathworld.wolfram.com).
Data Sources
Hospitalization data were obtained from 2001 state hospital discharge databases from Florida,22 Massachusetts,23 New Jersey,24 New York,25 Texas,26 and Virginia,27 representing 25.2% of the US population. The databases included all of the admissions to all of the nonfederal hospitals in the 6 states. We selected these states on the basis of the robustness of their data and their range of trauma system maturity. We extracted patient age, race, gender, insurance status, and hospital mortality. We generated injury severity scores from each patient's International Classification of Diseases, Ninth Revision (ICD-9), codes using ICD MAP-90 software (Trianalytics, Inc, Baltimore, MD).
HRRs for each state were identified by zip code from the Dartmouth Atlas of Healthcare. Each patient's residence and each hospital were assigned to HRRs on the basis of zip codes (www.dartmouthatlas.org). We selected HRRs as a unit of analysis because they are discrete regions with a standardized pattern of referral for expert medical care and are widely used to understand patterns of care. We categorized HRRs by the presence of ≥1 high-level center, no high-level centers but ≥1 level II center, and absence of both high-level and level II centers.
Population data were obtained from the year 2000 US Census (www.uscensus.gov) and the National Center for Health Statistics natality report.28 We obtained hospital information from the American Hospital Association and the National Association of Children's Hospitals and Related Institutions (www.childrenshospitals.net/nachri).29 We identified trauma centers from lists obtained from each state's department of health (New York, Texas, and Virginia) or emergency medical services (Florida, Massachusetts, and New Jersey).30-35
Patient Cohort
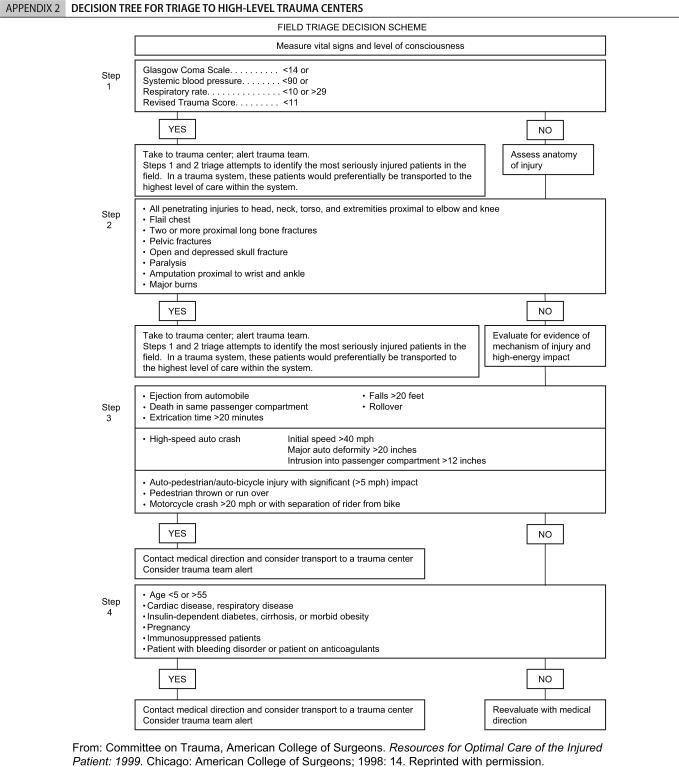
We selected all of the hospital discharges of patients <20 years old with TBI using previously published ICD-9 Clinical Modification–based methodology,12,36-41 and identified severe TBI using the ASC COT field triage decision scheme, mapping the anatomic and physiologic indications to ICD-9 Clinical Modification codes (Appendices 1 and 2). We limited analysis to those HRRs in each state where the central city for the HRR was in 1 of the 6 states. This approach yielded 68 HRRs, of which 18 were in Florida, 3 were in Massachusetts, 7 were in New Jersey, 10 were in New York, 22 were in Texas, and 8 were in Virginia.
Sensitivity Analysis
The ACS COT recognizes that level II trauma centers can serve as the lead trauma facility in a region where no level I center is readily available. To explore how admission to a level II center might impact regionalization, we repeated our primary analysis using an expanded definition of “high-level center” that included level II trauma centers.
Data Analysis
We tested differences in proportions using binomial and χ2 tests. To assess whether rates of care at high-level centers were associated with the maturity of statewide trauma systems, we examined the correlation between state rates and the age (in years) of their trauma systems. To explore the independent contribution of potential predictors of admission to a high-level center, we performed multivariate analyses using generalized estimating equations exploring patient-level characteristics (age, race, gender, injury severity, insurance status, and distance of home to the nearest high-level center) and HRR characteristics (population density, income, and education levels of inhabitants). We considered statistical significance as a P value of <.05, managed data using Foxpro (Microsoft Corp, Richmond, WA), and conducted analyses by using Stata 7.0 (Stata Corp, College Station, TX). We mapped HRR regionalization by using ArcMap 9.0 (ESRI, Inc, Redlands, CA).
RESULTS
In 2001, there were 2117 hospitalizations for severe pediatric TBI (9.8 hospitalizations per 100 000 children per year) in 204 hospitals in the study area (Table 1). Children with severe TBI had a mean (median) injury severity score of 22.7 (21.0) and a hospital mortality of 18.8%. Children <1 year old had the lowest incidence of severe TBI (7.4 per 100 000 children per year) but the highest mortality (27.1%). Teenagers 15 to 19 years old had the highest incidence of severe TBI (20.3 hospitalizations per 100 000 children per year) and the highest absolute number of cases; there were more cases of severe TBI in this group than all of the other age groups combined. More than half (53.4%) of the children with severe TBI were white, and 68.2% were boys (Table 1).
TABLE 1.
Characteristics of Admissions for Children With Severe TBI in the 6-State Cohort (N = 2117)
| Characteristic | Severe TBI, % of Cohort | Hospital Mortality, % | Admitted to High-Level Centers, % |
|---|---|---|---|
| Age, y | |||
| <1 | 6.6 | 27.1 | 76.4 |
| 1−4 | 11.8 | 23.2 | 80.8 |
| 5−9 | 13.4 | 14.8 | 78.1 |
| 10−14 | 16.7 | 17.8 | 71.6 |
| 15−19 | 51.5 | 18.1 | 58.8 |
| Total | 100.0 | 18.8 | 67.3 |
| Gender | |||
| Male | 68.2 | 19.1 | 67.6 |
| Female | 31.8 | 18.3 | 66.8 |
| Race | |||
| White, non-Hispanic | 53.4 | 18.2 | 64.5 |
| Hispanic | 18.3 | 19.0 | 59.5 |
| Black, non-Hispanic | 17.8 | 18.9 | 78.2 |
| Others/unknown | 17.0 | 21.2 | 76.6 |
| Injury severity score | |||
| 0−5 | 7.9 | 3.6 | 66.7 |
| 5−15 | 10.7 | 1.3 | 72.6 |
| >15 | 81.4 | 22.6 | 66.7 |
| Insurance coverage | |||
| Medicaid | 19.1 | 17.2 | 72.0 |
| Commercial | 56.7 | 15.8 | 69.1 |
| Uninsured | 10.5 | 32.7 | 59.6 |
| Other/unknown | 13.8 | 22.3 | 58.8 |
Overall, only two thirds (67.3%) of severe pediatric TBI hospitalizations were in high-level centers (1128 admissions to level I trauma centers plus 297 admissions to pediatric trauma centers). Young children were admitted to high-level centers more frequently than adolescents, as were blacks compared with whites or Hispanics (Table 1). Multivariate analyses showed that care at a high-level center was significantly and independently associated with younger age, black race, and having insurance (P < .01; data not shown).
Regionalization Among the 6 States
Among states, the percentage of severe pediatric TBI cases admitted to high-level centers ranged from 56.4% in Texas to 93.6% in Massachusetts (Table 2). Massachusetts and Virginia were the only well-regionalized states. The remaining 4 states were unevenly and poorly regionalized overall. Ready availability of high-level trauma care within states did not ensure adequate regionalization. For example, Massachusetts and New York had the highest number of high-level centers per capita and the lowest number of HRRs without high-level centers, and >80% of children with severe TBI in those states lived within 40 miles of a high-level center (Table 2). However, >93% of severe pediatric TBI admissions were in high-level centers in Massachusetts, whereas <80% were in high-level centers in New York. In addition, the proportion of children with severe TBI living in proximity to high-level centers (<40 miles) was greater than the proportion admitted to high-level centers in all 4 of the poorly regionalized states.
TABLE 2.
State and HRR Characteristics
| Variable | Florida | Massachusetts | New Jersey | New York | Texas | Virginia |
|---|---|---|---|---|---|---|
| Population | ||||||
| Total, millions, n | 16.0 | 6.3 | 8.4 | 19.0 | 20.9 | 7.1 |
| <20 years old, % | 25.3 | 26.4 | 27.1 | 27.5 | 31.4 | 27.4 |
| State size (square miles) | 55 815 | 8173 | 7508 | 48 562 | 264 436 | 39 820 |
| Population density, n per square mile | 286 | 777 | 1121 | 391 | 79 | 178 |
| High-level centers | ||||||
| No. | 15 | 8 | 3 | 24 | 14 | 6 |
| No. per 1 000 000 population | 0.94 | 1.26 | 0.36 | 1.26 | 0.67 | 0.85 |
| Admissions for severe pediatric TBI, n | 518 | 140 | 199 | 408 | 675 | 177 |
| Children with severe TBI residing within 40 miles of high-level center, % | 82.1 | 81.7 | 87.7 | 84.3 | 67.5 | 62.1 |
| HRRs, n | ||||||
| Total | 18 | 3 | 7 | 10 | 22 | 8 |
| Without a high-level center | 11 | 0 | 4 | 2 | 14 | 3 |
| Admissions for severe pediatric TBI, mean (range) | 29 (4−95) | 47 (20−86) | 28 (1−98) | 41 (1−98) | 31 (4−146) | 22 (1−55) |
| Distance from patient residence, mean (median), miles | ||||||
| To nearest hospital | 6.0 (4.0) | 6.3 (4.8) | 4.1 (2.9) | 5.5 (2.7) | 10.9 (5.1) | 9.8 (6.1) |
| To nearest high-level center | 25.4 (15.1) | 20.4 (12.2) | 20.4 (13.7) | 20.4 (8.1) | 64.9 (35.1) | 25.6 (19.2) |
| To admitting hospital | 31.3 (15.7) | 29.9 (11.9) | 17.3 (11.0) | 22.4 (10.4) | 62.0 (23.0) | 26.7 (18.1) |
| Severe pediatric TBI admissions, % | ||||||
| To high-level centers | 61.6 | 93.6 | 57.3 | 78.2 | 56.4 | 91.0 |
| To high-level or level II centers | 93.2 | 93.6 | 96.0 | 86.0 | 77.0 | 96.6 |
Age of the statewide trauma system also had no relationship to regionalization (r2 = 0.012; P = .84). The 6 statewide trauma systems had been in place from 0 (Massachusetts coalesced its 6 regional systems into a statewide system the following year) to 21 years (New Jersey and Virginia). Massachusetts, the “youngest” system, was the best regionalized state overall and was the only state in which all of the HRRs were well regionalized (Table 2). One of the oldest systems was in New Jersey, the second most poorly regionalized state.
Regionalization Among HRRs
The percentage of severe pediatric TBI admissions to high-level centers varied widely among the HRRs, from 0% in 3 HRRs to 100% in another 3 (Fig 1). Only 19.1% (n = 13) of the 68 HRRs were well regionalized, 11.8% were moderately regionalized, and the remaining 69.1% were poorly regionalized. Massachusetts was the only state in which all of the HRRs were well regionalized. In many cases, poorly regionalized HRRs were adjacent to well-regionalized HRRs and had similar size, population density, and number of high-level centers. In the moderately and poorly regionalized HRRs, 25.8% of severe TBI admissions were to level II centers.
FIGURE 1.
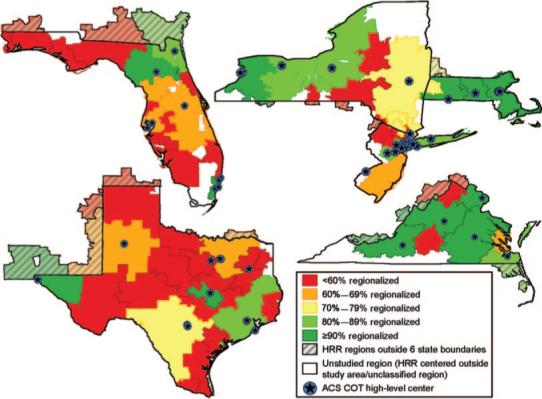
Proportions of children with severe TBI receiving care at high-level centers according to state and HRR. The percentage of severe pediatric TBI admissions to high-level centers varied widely among the HRRs, ranging from 0% in 3 HRRs to 100% in another 3 HRRs.
The presence of a high-level center within the boundaries of an HRR only marginally increased the likelihood that it would be well regionalized. Half of the HRRs contained ≥1 high-level center (n = 34). In these HRRs, 76.7% of severe pediatric TBI admissions were in high-level centers, and only 41.2% (n = 14) of these HRRs were well regionalized (Table 3). Excluding the 14 well-regionalized HRRs containing ≥1 high-level center, only 70% of severe pediatric TBI admissions were in high-level centers. In HRRs with no high-level center (n = 34), only 31.3% of severe TBI admissions were in high-level centers, and all 34 of these HRRs were poorly regionalized.
TABLE 3.
Regionalization of Severe Pediatric TBI According to Presence of High-Level or Level II Centers in HRRs
| Variable | ≥1 High-Level Center in HRR | No High-Level Center but ≥1 Level II Center in HRR | Neither High-Level Nor Level II Center in HRR |
|---|---|---|---|
| Severe pediatric TBI, n (%) | 1677 (79.2) | 210 (9.9) | 230 (10.9) |
| No. of HRRs | 34 | 14 | 20 |
| Population, millions, n (%) | |||
| Total | 58.6 (80.5) | 7.9 (10.8) | 6.5 (8.9) |
| <20 y old | 15.0 (80.6) | 1.9 (10.2) | 1.7 (9.1) |
| Population density, n per square mile | 266 | 198 | 49 |
| Distance from patient residence, mean (median), miles | |||
| To nearest hospital | 7.2 (4.1) | 7.4 (4.4) | 11.2 (4.9) |
| To nearest high-level center | 22.6 (12.7) | 45.6 (41.2) | 131.5 (118.9) |
| To admitting hospital | 33.7 (14.5) | 33.1 (15.5) | 66.3 (40.7) |
| Admitted to type of center, % | |||
| To a high-level center | 76.7 | 31.0 | 31.7 |
| To a high-level or level II center | 92.6 | 87.1 | 48.3 |
| HRRs with ≥90% admitted, n (%) | |||
| To a high-level center | 14 (41.2) | 0 (0.0) | 0 (0.0) |
| To a high-level or level II center | 30 (88.2) | 13 (92.9) | 5 (25.0) |
Regionalization and Distance to High-Level Centers
Distance to admitting hospitals averaged 37.1 miles (range: 0.1−636.9 miles), and distance to the nearest high-level center averaged 36.5 miles (range: 0.1−312.0 miles). However, in some HRRs, high-level centers were remote. For example, 11 HRRs without a high-level center had a mean distance from the patient's home zip code to the nearest high-level center of >100 miles. In 3 of these HRRs, children were admitted to hospitals at a mean distance of 33.2 miles. In the other 8 HRRs, children were admitted to 28 separate hospitals a mean of 97.4 miles from the patient's home zip codes. Despite this considerable distance, 70.3% of these hospitals were level III or lower. These 11 HRRs highlight an important difference between HRRs with and without high-level centers: the mean (median) distance to the nearest high-level center in HRRs with a high-level center was only 22.6 miles (12.7 miles), whereas the mean (median) distance in those without a high-level center was 90.5 miles (62.8 miles).
Distance to the nearest high-level center was not the only factor influencing where children with severe TBI were admitted. The 10 most population-dense HRRs in the sample (>1000 people per square mile) contained 26 high-level centers with a mean distance of only 6.9 miles to the nearest high-level center. In these HRRs, only 77.8% of children with severe TBI were admitted to high-level centers, and only 1 of these HRRs was well regionalized. Just as proximity to high-level centers did not ensure high-level care in population-dense HRRs, remoteness of high-level centers in well-regionalized HRRs did not seem to hinder high-level care (Fig 2A). In moderately and poorly regionalized HRRs, greater distance lowered the likelihood of admission to a high-level center, down to ≤60% for children living 80 to 100 miles from a high-level center (Fig 2B). However, the percentage of subjects with severe TBI admitted to high-level centers was never >80%, even for children residing <10 miles from those centers.
FIGURE 2.
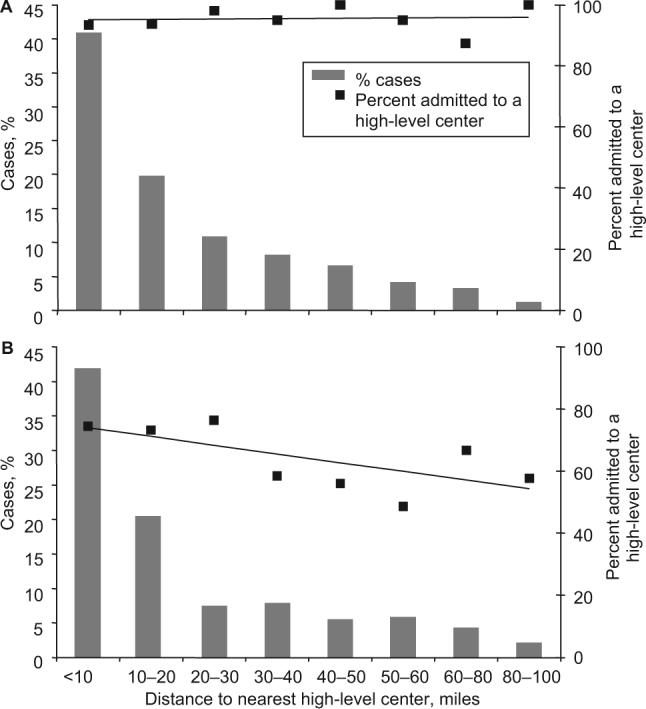
Case distribution and percentage of patients admitted to a high-level center as a function of distance to the nearest high-level center for HRRs with ≥1 high-level center. A, Well-regionalized HRRs. B, Poorly regionalized HRRs. In well-regionalized HRRs, ≥90% of patients with severe TBI were admitted to high-level centers regardless of the distance to the centers (A). In moderately and poorly regionalized HRRs, the percentage was never >80%, even for children residing <10 miles from high-level centers (B).
Sensitivity Analysis
Overall, 19.9% of severe TBI admissions were in level II centers. Level II centers had less than half the caseload of high-level centers (mean of 9.3 severe TBI admissions per level II center compared with 21.9 admissions per high-level center). When we modified the definition of “high-level center” to include level II trauma centers, the percentage of subjects with severe TBI admitted to high-level centers increased to 87.3%. Using this definition, 4 of the 6 states became well regionalized, New York became moderately regionalized, and Texas remained poorly regionalized (Table 2). The definition change made only very small differences in the percentage of subjects with severe TBI admitted to high-level centers in Massachusetts and Virginia, reflecting the very small percentage of cases (<4% overall) admitted to level II centers in these states.
Including level II centers in the definition of “high-level center,” 17 of the 68 HRRs remained poorly regionalized, 13 were moderately regionalized, and only 38 (55.9% of the 68 HRRs) were well regionalized. For the 34 HRRs without a level I or pediatric trauma center, including level II centers in the definition of “high-level center” more than doubled the percentage of subjects with severe TBI admitted to high-level centers, from 31.4% to 66.8%. For the HRRs with ≥1 level I or pediatric trauma center, the proportion of subjects with severe TBI admitted to high-level centers also increased from 76.7% to 92.6%.
DISCUSSION
Despite evidence that severely injured children have better outcomes when they receive care at high-level trauma centers, we found that almost one third of children with severe TBI in 6 US states failed to receive care in such centers. Only 2 of the states and less than one fifth of the 68 HRRs provided high-level trauma care to ≥90% of children with severe TBI. Poor regionalization was attributed in part to the lack of proximity to high-level centers. However, the presence of a nearby high-level center did not ensure adequate regionalization. The majority of HRRs with ≥1 high-level center were poorly or moderately regionalized. In many of these HRRs, the distance to the admitting hospital was longer than the distance to the nearest high-level center.
When we expanded the definition of “high-level center” to include level II centers, regionalization improved overall, especially in HRRs without level I or pediatric trauma centers. Care providers in these HRRs seem to be following ACS COT guidelines by using level II centers as lead trauma facilities in regions without a level I or pediatric trauma center. However, the ability of level II centers to serve as leading centers for severe pediatric TBI is debatable, particularly given that these centers admitted <1 subject with severe TBI per month on average. Including level II centers in the definition of “high-level center” also increased the proportion of severe TBI admissions in high-level centers in HRRs that already contained ≥1 level I or pediatric trauma center. In these HRRs, frequent use of level II centers may not have been appropriate given the presence of local level I centers.
We also found that there was only a weak relationship between regionalization and distance to the nearest high-level center and that the likelihood of admission to a high-level center was associated with patient characteristics such as age, race, and insurance status. The ACS COT guidelines emphasize that younger children should preferentially receive high-level care, and, therefore, the association with age may be considered reassuring. However, if children with traumatic injuries experience disparities in access to health care on the basis of sociodemographic characteristics, then trauma care may not be as protocolized as we believed previously. It is also possible that propensity to admit a patient with severe TBI to a high-level center is more an organizational characteristic of the HRRs themselves. Therefore, regionalization might be improved by making organizational changes within the current systems. For HRRs without local high-level centers, where patients are transported long distances for admission to lower-level centers, a small incremental increase in transport distance might allow admission to a higher-level center. In regions where neither high-level nor level II centers are available, statewide trauma systems may need to develop ultraregionalized systems whereby patients are transported longer distances to optimal centers farther away.
This study highlights inconsistencies in current trauma care that can serve as a basis for both additional research and health care policy. More research is needed to understand why current standards for the regionalization of care are not being met and what could be done to improve these processes. We cannot determine from this study to what extent our findings represent limitations of the ACS COT guidelines themselves (eg, perhaps some patients for whom high-level care is recommended do not benefit from such care), nor can we can determine the extent to which family or physician preferences or logistic limitations interfered with transfer to high-level care. More research is also needed to understand what differentiates the states that are meeting ACS COT guidelines from those that are not and how patient outcome might be affected by this type of variation in practice. From a policy standpoint, this study identifies the gap between quality standards and actual performance. Trauma policy leaders in each state may choose to use this opportunity to re-evaluate their own quality standards and quality improvement processes to ensure that the gap is being narrowed.
There are several limitations to this study related to the use of administrative data. Although these data are essential for broad, population-based analyses, they contain limited clinical information.41,42 We addressed this limitation by using a strict definition of severe TBI based on anatomic and physiologic criteria, an approach used by others.41 Although data limitations also precluded the use of mechanism of injury to identify severe TBI, others have found mechanism of injury to be an unreliable predictor of the need for hospitalization or ICU services.43-45 We could not determine the geographic location of patient injury and had to rely on estimates based on patient home zip codes. However, Ni et al46 found that the vast majority of recreational childhood injuries in the United States in 1997−1998 occurred in close proximity to family homes.
CONCLUSIONS
Pediatric TBI is a serious medical problem in the United States. Although the mechanisms needed to organize care for severe TBI in dedicated, high-level centers are in place in many states, we found that these mechanisms are not sufficient to fully meet the needs of the most severely injured children. This occurs despite the widespread availability of high-level centers and decades of emphasis on trauma system development.
ACKNOWLEDGMENTS
This work was supported by National Institute of Child Health and Human Development/National Institutes of Health grants T32 HD40686 and K23 HD046489.
We thank Kristen Kurland for assistance in working with ArcMap and creating the maps.
Abbreviations
- TBI
traumatic brain injury
- ACS COT
American College of Surgery Committee on Trauma
- HRR
health care referral region
- ICD-9
International Classification of Diseases, Ninth Revision
APPENDIX
APPENDIX 1.
ICD-9 CODES USED FOR IDENTIFICATION OF SUBJECTS
| ICD-9 codes that indicate TBI | |
| 800.0−801.9 | Fracture of vault or base of skull |
| 803.0−804.9 | Other and unqualified and multiple fractures of skull or face with other bones |
| 850.0−854.1 | Intracranial injury, including concussion, contusion, laceration, and hemorrhage |
| ICD-9 codes that indicate anatomically severe head injury | |
| 800.6−800.9 | Open fracture of vault of skull with intracranial injury |
| 801.6−801.9 | Open fracture of base of skull with intracranial injury |
| 803.6−803.9 | Open other and unqualified skull fractures |
| 804.6−804.9 | Open multiple fractures of skull or face with other bones |
| 851.1, 851.3, 851.5, 851.7, 851.9 | Cerebral laceration and contusions with open intracranial wound |
| 852.1, 852.3, 852.5 | Subarachnoid, subdural and extradural hemorrhage with open intracranial wound |
| 853.1 | Other and unspecified intracranial hemorrhage with open intracranial wound |
| 854.1 | Other and unspecified intracranial injury with open intracranial wound |
| Codes that indicate physiologically severe head injury | |
| ICD-9 codes | |
| 850.3, 850.4 | Concussion with prolonged loss of consciousness |
| 958.4 | Traumatic shock |
| Procedure codes | |
| 96.70−96.72 | Mechanical ventilation |
Footnotes
The authors have indicated they have no financial relationships relevant to this article to disclose.
What's Known on This Subject Trauma research in the United States has repeatedly demonstrated that care at specialized trauma centers is associated with better outcomes for severely injured children.
What This Study Adds Relatively little attention has been paid to the extent to which severely injured patients receive care at high-level trauma centers, and no studies have examined children with severe traumatic brain injuries. This study suggests complex deficiencies in functioning of some statewide trauma systems.
REFERENCES
- 1.Langlois JA, Rutland-Brown W, Thomas KE. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Centers for Disease Control; Atlanta, GA: 2004. [Google Scholar]
- 2.Nathens AB, Jurkovich GJ, Maier RV, et al. Relationship between trauma center volume and outcomes. JAMA. 2001;285(9):1164–1171. doi: 10.1001/jama.285.9.1164. [DOI] [PubMed] [Google Scholar]
- 3.Mullins RJ, Mann NC, Hedges JR, Worrall W, Jurkovich GJ. Preferential benefit of implementation of a statewide trauma system in one of two adjacent states. J Trauma. 1998;44(4):609–616. doi: 10.1097/00005373-199804000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000;48(1):25–30. doi: 10.1097/00005373-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Dudley RA, Johansen KL, Brand R, Rennie DJ, Milstein A. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA. 2000;283(9):1159–1166. doi: 10.1001/jama.283.9.1159. [DOI] [PubMed] [Google Scholar]
- 6.Cales RH, Trunkey DD. Preventable trauma deaths: a review of trauma care systems development. JAMA. 1985;254(8):1059–1063. doi: 10.1001/jama.254.8.1059. [DOI] [PubMed] [Google Scholar]
- 7.Kane G, Wheeler NC, Cook S, et al. Impact of the Los Angeles County Trauma System on the survival of seriously injured patients. J Trauma. 1992;32(5):576–583. doi: 10.1097/00005373-199205000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Shackford SR, Hollingworth-Fridlund P, Cooper GF, Eastman AB. The effect of regionalization upon the quality of trauma care as assessed by concurrent audit before and after institution of a trauma system: a preliminary report. J Trauma. 1986;26(9):812–820. doi: 10.1097/00005373-198609000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Nathens AB, Jurkovich GJ. The effect of organized systems of trauma care on motor vehicle crash mortality. JAMA. 2000;283(15):1990–1994. doi: 10.1001/jama.283.15.1990. [DOI] [PubMed] [Google Scholar]
- 10.Hall JR, Reyes HM, Meller JL, Loeff DS, Dembek R. The outcome for children with blunt trauma is best at a pediatric trauma center. J Pediatr Surg. 1996;31(1):72–76. doi: 10.1016/s0022-3468(96)90322-x. [DOI] [PubMed] [Google Scholar]
- 11.Nakayama DK, Copes WS, Sacco W. Differences in trauma care among pediatric and nonpediatric trauma centers. J Pediatr Surg. 1992;27(4):427–431. doi: 10.1016/0022-3468(92)90328-5. [DOI] [PubMed] [Google Scholar]
- 12.Hulka F, Mullins RJ, Man NC, et al. Influence of a statewide trauma system on pediatric hospitalization and outcome. J Trauma. 1997;42(3):514–519. doi: 10.1097/00005373-199703000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Demetriades D, Martin M, Salim A, Rhee P, Brown C, Chan L. The effect of trauma center designation and trauma volume on outcome in specific severe injuries. Ann Surg. 2005;242(4):512–519. doi: 10.1097/01.sla.0000184169.73614.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Potoka DA, Schall LC, Gardner MJ, Stafford PW, Peitzman AB, Ford HR. Impact of pediatric trauma centers on mortality in a statewide system. J Trauma. 2000;49(2):237–245. doi: 10.1097/00005373-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Trunkey DD. History and development of trauma care in the United States. Clin Orthop Relat Res. 2000;374(374):36–46. doi: 10.1097/00003086-200005000-00005. [DOI] [PubMed] [Google Scholar]
- 16.MacKenzie EJ, Hoyt DB, Sacra JC, et al. National inventory of hospital trauma centers. JAMA. 2003;289(12):1515–1522. doi: 10.1001/jama.289.12.1515. [DOI] [PubMed] [Google Scholar]
- 17.Ma MH, MacKenzie EJ, Alcorta R, Kelen GD. Compliance with prehospital triage protocols for major trauma patients. J Trauma. 1999;46(1):168–175. doi: 10.1097/00005373-199901000-00029. [DOI] [PubMed] [Google Scholar]
- 18.American College of Surgeons, Committee on Trauma . Resources for the Optimal Care of the Injured Patient. American College of Surgeons; Chicago, IL: 1990. [Google Scholar]
- 19.Johnson DL, Krishnamurthy S. Send severely head-injured children to a pediatric trauma center. Pediatr Neurosurg. 1996;25(6):309–314. doi: 10.1159/000121145. [DOI] [PubMed] [Google Scholar]
- 20.Santaniello JM, Esposito TJ, Luchette FA, Atkian DK, Davis KA, Gamelli RL. Mechanism of injury does not predict acuity or level of service need: field triage criteria revisited. Surgery. 2003;134(4):698–703. doi: 10.1016/s0039-6060(03)00331-3. [DOI] [PubMed] [Google Scholar]
- 21.Champion HR. Triage. In: Cales RH, Heileg RW, editors. Trauma Care Systems. Aspen Publishers; Rockville, MD: 1986. pp. 79–108. [Google Scholar]
- 22.Agency for Healthcare Administration . Hospital Inpatient Data File, State of Florida. State of Florida, Agency for Healthcare Administration; Tallahassee, FL: 2000. [Google Scholar]
- 23.Department of Public Health . Massachusetts Hospital Inpatient Datafile 1999. State of Massachusetts, Department of Public Health; Boston, MA: 2000. [Google Scholar]
- 24.Department of Health and Senior Services . Discharge Data UB-92 YTD Tape File, New Jersey. State of New Jersey, Department of Health and Senior Services; Trenton, NJ: 2000. [Google Scholar]
- 25.New York State Department of Health . New York State Department of Health SPARCS “Expanded Administrative Releasable” Data. State of New York Department of Health; New York, NY: 2000. [Google Scholar]
- 26.Healthcare Information Council . Texas Hospital Inpatient Discharge Public Use Datafile. Texas Healthcare Information Council; Austin, TX: 2002. [Google Scholar]
- 27.Virginia Health Information . Public Use File-PUF1 Patient Level Data, Virginia. Virginia Health Information; Richmond, VA: 2000. [Google Scholar]
- 28.Ventura SJ, Martin JA, Curtin SC, Menacker F, Hamilton BE. Births: final data for 1999. Natl Vital Stat Rep. 2001;49(1):1–100. [PubMed] [Google Scholar]
- 29.American Hospital Association . AHA Guide to the Health Care Field. American Hospital Association; Chicago, IL: 2000. [Google Scholar]
- 30.State Department of Health . State-Approved Trauma Centers. Florida State Department of Health; Tallahassee, FL: 2002. [March 15, 2006]. Available at: www.doh.state.fl.us/demo/Trauma/center.htm. [Google Scholar]
- 31.Washington State Office of Emergency Medical and Trauma Prevention . Washington State Designated Trauma Services. Washington State Office of Emergency Medical and Trauma Prevention; Olympia, WA: 2003. [March 15, 2006]. Available at: www.doh.wa.gov/hsqa/emstrauma/traumadesig.htm. [Google Scholar]
- 32.Massachusetts Trauma Centers . Massachusetts Office of Emergency Medical Services. Massachusetts Trauma Centers; Boston, MA: 2002. [Google Scholar]
- 33.New York State Department of Health . New York State Trauma Centers. New York State Department of Health; Albany, NY: 2002. [March 15, 2006]. Available at: www.health.state.ny.us/nysdoh/ems/trauma2.htm. [Google Scholar]
- 34.New Jersey Department of Health . New Jersey's Trauma Centers. New Jersey Department of Health; Trenton, NJ: 2002. [Google Scholar]
- 35.Virginia Department of Health Office of Emergency Medical Services . Trauma Centers. Virginia Department of Health Office of Emergency Medical Services; Richmond, VA: 2002. [March 15, 2006]. Available at: www.vdh.state.va.us/oems/Files_page/trauma/TraumaCentersMap&List.pdf. [Google Scholar]
- 36.Thurman D, Guerrero J. Trends in hospitalization associated with traumatic brain injury. JAMA. 1999;282(10):954–957. doi: 10.1001/jama.282.10.954. [DOI] [PubMed] [Google Scholar]
- 37.Reid SR, Roesler JS, Gaichas AM, Tsai AK. The epidemiology of pediatric traumatic brain injury in Minnesota. Arch Pediatr Adolesc Med. 2001;155(7):784–789. doi: 10.1001/archpedi.155.7.784. [DOI] [PubMed] [Google Scholar]
- 38.Jager TE, Weiss HB, Coben JH, Pepe PE. Traumatic brain injuries evaluated in U.S. emergency departments, 1992−1994. Acad Emerg Med. 2000;7(2):134–140. doi: 10.1111/j.1553-2712.2000.tb00515.x. [DOI] [PubMed] [Google Scholar]
- 39.Potoka DA, Schall LC, Ford HR. Improved functional outcome for severely injured children treated at pediatric trauma centers. J Trauma. 2001;51(5):824–832. doi: 10.1097/00005373-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Báez AA, Lane PL, Sorondo B. System compliance with out-of-hospital trauma triage criteria. J Trauma. 2003;54(2):344–351. doi: 10.1097/01.TA.0000046258.81127.E1. [DOI] [PubMed] [Google Scholar]
- 41.Iezzoni LI. Using administrative diagnostic data to assess the quality of hospital care. Pitfalls and potential of ICD-9-CM. Int J Technol Assess Health Care. 1990;6(2):272–281. doi: 10.1017/s0266462300000799. [DOI] [PubMed] [Google Scholar]
- 42.Rubenfeld GD, Angus DC, Pinsky MR, et al. Outcomes research in critical care: results of the American Thoracic Society Critical Care Assembly Workshop on Outcomes Research. Am J Respir Crit Care Med. 1999;160(1):358–367. doi: 10.1164/ajrccm.160.1.9807118. [DOI] [PubMed] [Google Scholar]
- 43.Shatney CH, Sensaki K. Trauma team activation for ‘mechanism of injury’ blunt trauma victims: time for a change? J Trauma. 1994;37(2):275–281. [PubMed] [Google Scholar]
- 44.Henry MC, Alicandro JM, Hollander JE, Moldashel JG, Cassara G, Thode HC., Jr Evaluation of American College of Surgeons trauma triage criteria in a suburban and rural setting. Am J Emerg Med. 1996;14(2):124–129. doi: 10.1016/S0735-6757(96)90117-5. [DOI] [PubMed] [Google Scholar]
- 45.Murray JA, Chen D, Velmahos GC, et al. Pediatric falls: is height a predictor of injury and outcome? Am Surg. 2000;66(9):863–865. [PubMed] [Google Scholar]
- 46.Ni H, Barnes P, Hardy AM. Recreational injury and its relation to socioeconomic status among school aged children in the US. Inj Prev. 2002;8(1):60–65. doi: 10.1136/ip.8.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]