Abstract
Objective
The goal of this study was to investigate the emergence of dietary restraint, disinhibited eating, weight concerns, and body dissatisfaction among girls from 5 to 9 years old, and to assess whether girls at risk for overweight at age 5 were at greater risk for the emergence of restraint, disinhibited overeating, weight concerns, and body dissatisfaction.
Design
Longitudinal data were used to assess the relationship between weight status and the development of dietary restraint, aspects of disinhibited overeating, weight concern, and body dissatisfaction at ages 5, 7, and 9 years.
Subjects
Participants were 153 girls from predominately middle class and exclusively non-Hispanic white families living in central Pennsylvania.
Statistical Analyses
Differences in weight status, dietary restraint, disinhibition, weight concern, and body dissatisfaction between girls at risk (>85th percentile body mass index) or not at risk for overweight at age 5 were assessed using repeated measures analysis of variance at ages 5, 7, and 9 years.
Results
Girls who were at risk for overweight at age 5 reported significantly higher levels of restraint, disinhibition, weight concern, and body dissatisfaction by age 9. Girls at risk for overweight at age 5 also showed greater increases in weight status from 5 to 9 years of age.
Conclusions
Higher levels of dietary restraint, weight concern, and body dissatisfaction among young girls at risk for overweight were accompanied by greater weight gain from 5 to 9 years of age, consistent with other recent findings suggesting that youths’ attempts at weight control may promote weight gain. Positive alternatives to attempts at dietary restriction are essential to promoting healthful weight status among children, and should include encouraging physical activity, promoting children’s acceptance of a variety of low–energy-density foods, and providing guides to appropriate portion sizes.
The construct of dietary restraint was originally defined as the cognitive tendency to restrict intake as a means of maintaining or losing body weight (1) and tends to be highly related to dieting behavior, body dissatisfaction, and weight concerns (2,3). Initially, dietary restraint was believed to emerge during adolescence as a consequence of the normative weight gain associated with puberty (4). This weight gain was hypothesized to promote body dissatisfaction and more frequent and extreme weight control measures (5,6). However, recent evidence suggests that dietary restraint and the accompanying breakdown of restraint, referred to as disinhibition, may be emerging before puberty, along with other maladaptive eating attitudes and behaviors during childhood (7,8).
Understanding the developmental precursors of restraint, weight concern, and body dissatisfaction is critical because they can elevate the risk for subsequent disordered eating (9–11). It is possible that the recent reports of the emergence of dietary restraint, weight concern, and body dissatisfaction among children are linked to the current epidemic of childhood overweight and obesity (12). Consistent with the data on adolescents (13), higher weight status may place children at increased risk for the onset of dietary restraint, weight concerns and body dissatisfaction, and disinhibited overeating.
Disinhibited overeating, which involves loss of cognitive control over eating, is thought to occur as a result of the breakdown of prior restraint. For example, among adults, many highly restrained individuals are likely to overeat after a high-calorie preload, which is in contrast to what would be considered a normal regulatory response. This experimentally induced dietary disinhibition has also been observed in 9- to 12-year-olds (14,15), and most recently, in a study by Fisher and Birch (16), girls as young as 5 years old were found to overeat when exposed to palatable foods, immediately after a meal and in the absence of hunger. Girls who were overweight and whose mothers reported restricting daughters’ intakes of snack foods were most susceptible to overeating in the absence of hunger (17). Girls as young as age 5 also reported concerns about their weight, which were positively correlated with their weight status (18). During adolescence, elevated weight status is associated with higher weight concerns, dietary restraint, disinhibited overeating, and greater body dissatisfaction (13). This suggests that elevated weight status may also promote the development of weight concern, body dissatisfaction, and disinhibited overeating during childhood.
The goal of this study was to investigate the emergence of dietary restraint, disinhibited eating, weight concerns, and body dissatisfaction among girls from 5 to 9 years old, and to assess whether girls at risk for overweight at age 5 were at greater risk for the emergence of restraint, disinhibited overeating, weight concerns, and body dissatisfaction. We also assessed whether body mass index (BMI) trajectories differed across middle childhood for girls who were either at risk or not at risk for overweight at age 5.
SUBJECTS AND METHODS
Participants
Families were recruited from central Pennsylvania for participation in a longitudinal study of the “health and development of young girls from age 5 to 9 years” using flyers and newspaper advertisements. Families with age-eligible female children within a five-county radius also received letters inviting them to participate in the study. At entry into the study, participants included 197 5-year-old girls (mean age=5.4±0.3) and their parents, of whom 192 families were reassessed 2 years later, when the girls were 7 years old (mean age=7.3±0.3). A third assessment with 183 families was conducted 2 years later, 4 years after the initial assessment, when the girls were 9 years old (mean age=9.34±0.3).
This study includes 153 non-Hispanic white girls with complete data on all measures pertaining to this study. The 153 families did not differ from the dropped cases in terms of family income (F=0.87, P=.35), mothers’ education levels (F=0.09, P=.76), fathers’ education levels (F=1.75, P=.19), or mean BMI (F=2.11, P=.14). All procedures were reviewed and approved by The Pennsylvania State University Human Subjects Institutional Review Board.
MEASURES
Girls’ Dietary Restraint
Children’s restrained eating was measured using the original Dutch Eating Behavior Questionnaire created by Van Strien and colleagues (19). The measure consists of 33 items, and measures three factors: restraint, emotional eating, and external eating. For the purposes of this research, only the 10-item restraint scale was used and the response set was reduced from a five-point scale (ranging from seldom to very often) to a three-point scale (yes, sometimes, no). Some modifications in wording were made for use with children. For example, “Do you deliberately eat less in order not to become heavier?” was changed to read, “Do you try to only eat a little bit on purpose so that you won’t get fat?” In this sample, Cronbach α were 0.64, 0.78, and 0.87 for the restraint scale at ages 5, 7, and 9 years, respectively.
Girls’ Disinhibited Eating
The Eating in the Absence of Hunger Protocol (EAH) provided a behavioral measure of aspects of girls’ disinhibited eating, or eating palatable foods in the absence of hunger. After a self-selected lunch, girls first indicated the extent to which they were hungry using three cartoon figures depicting an empty stomach, half-empty stomach, and full stomach. To minimize the influence of hunger on the assessment of snack food intake, cases in which girls indicated that they were still hungry after lunch were not included in these analyses. Next, a rank-order food preference assessment was performed to ensure that each girl had an opportunity to taste each snack food. After the preference assessment, each girl was shown various toys that were available for a play session. Generous portions of 10 sweet and savory snack foods varying in fat content were presented during the procedure: popcorn (6 g), potato chips (58 g), pretzels (39 g), nuts (44 g), fig bars (51 g), chocolate chip cookies (66 g), fruit-chew candy (66 g), chocolate bars (66 g), ice cream (168 g), and frozen yogurt (168 g). Manufacturers’ information was used to convert the gram weight of each food into energy intakes. Girls were told that they could play with available toys or eat any of the foods while the experimenter did some work in the adjacent room. The experimenter then left the room for 10 minutes. A measure of disinhibited overeating in the absence of hunger was obtained by summing the energy intake of all of the snack foods eaten during this period. In pilot testing by Fisher and Birch (20), girls’ free-access energy intake showed stability across the 4-year period between the ages of 5 and 9 years (r=0.29, P<.001).
Girls’ Weight Concerns
Weight concern was measured using the Weight Concern Scale developed by Killen and colleagues (21). At age 5 years, the measure was amended slightly; terminology was simplified and the response set was reduced from a five-point to a three-point scale. The original scale was used for the remaining waves. Higher scores indicate higher weight concern.
Girls’ Body Dissatisfaction
Children’s self-reported body dissatisfaction was measured using the Body Esteem Scale developed by Mendelson and White (22). For use in this research the response set was increased from yes/no to yes, sometimes, and no, to increase variability of responses. The Cronbach α reported in this sample at each time point was 0.75 at age 5, 0.84 at age 7, and 0.87 at age 9 years.
Girls’ Weight Status: BMI Percentiles
Girls’ heights and weights were measured in triplicate at 5, 7, and 9 years by a trained research assistant to calculate girls’ BMIs (calculated as kg/m2). Because BMI during childhood is age- and sex-specific, BMI percentiles and BMI z-scores were also calculated using the most recent National Center for Health Statistics growth charts from the Centers for Disease Control and Prevention (CDC) (23).
Statistical Analysis
To investigate whether girls who were at risk for overweight at the age of 5 showed differences in patterns of change in weight status or had higher levels of restraint, weight concern, body dissatisfaction, and disinhibited overeating than normal-weight girls at ages 5, 7, and 9 years, girls were classified into two groups: at risk for overweight (≥85th percentile) or not at risk for overweight, based on age- and sex-specific BMI percentile scores at age 5. Of the 153 girls in the sample, 32 were at or above the 85th percentile, the CDC definition for “at risk for overweight.” Repeated measures analysis of variance (ANOVA), with weight status as the between-subjects factor and age as the repeated factor, investigated risk group differences from 5 to 9 years, weight for BMI and BMI z-scores, dietary restraint, EAH, weight concern, and body dissatisfaction. For children, BMIs are age- and sex-specific, but because all of our participating girls’ BMIs were measured at the same ages (5, 7, and 9 years), we were able to use the girls’ BMI scores to illustrate the normative increases in BMI that occur across middle childhood, and to assess whether there were different BMI trajectories over time for girls who were and were not at risk for overweight at age 5. The mean BMI percentile of the at-risk group was consistently above the 92nd percentile, revealing a problem with ceiling effects with the use of BMI percentiles among the at-risk-for-overweight group. To eliminate the ceiling effects, analyses were conducted using BMI z-scores in repeated measures ANOVAs with age as a repeated factor and risk group as the between-subjects factors to assess whether change over time in BMI differed by risk group. However, rather than presenting the standardized z-score measures, which remove the mean differences across age, the results present the BMI data graphically, to illustrate the general increase in BMI for girls that occurs across middle childhood, and to illustrate the difference in the patterns of change in the slopes of the weight status trajectories for the at-risk and not-at-risk groups from ages 5 to 9. All data were analyzed using the Statistical Analysis System (version 8.0, 1999–2001, SAS Institute Inc, Cary, NC).
RESULTS
The 153 girls with complete data were classified on the basis of BMI percentile scores at age 5; girls above the 85th percentile on the National Center for Health Statistics/CDC BMI percentile standardized growth charts (24) were classified as at risk for overweight, and the remaining girls were classified as not at risk for overweight. None of the girls were classified as underweight (<5th percentile for BMI). Of the 153 girls, 32 were at risk for overweight at age 5. Figure 1 presents mean BMI scores from ages 5 to 9 for girls at risk and not at risk for overweight. Mean BMI at 5, 7, and 9 years increases for both groups, reflecting growth during the period from 5 to 9 years of age. The mean BMI percentile for the at-risk-for-overweight group remained above the 92nd percentile at 5, 7, and 9 years, whereas the mean BMI percentile for girls not at risk for overweight remained between the 50th and 60th BMI percentile at ages 5, 7, and 9 years. Repeated measures ANOVAs were conducted on the BMI data and on BMI z-scores to determine whether patterns of weight gain from ages 5 to 9 differed for girls who were and were not at risk for overweight at age 5; the results of these analyses were very similar and the patterns of changes for the BMI data are presented in Figure 1. In addition to the expected main effect of age on increasing BMI, the BMI results showed a significant interaction of age by risk group (F=17.08, P<.0001), reflecting greater increases in BMI among girls who were at risk for overweight at age 5; this interaction was also significant for the BMI z-scores, P<.05. Girls at risk for overweight at age 5 also had significantly higher BMIs at ages 7 and 9 than girls not at risk, reflecting the fact that the at-risk and not-at-risk groups remained distinct across time. (F=162.27, 120.86, and 73.63 at ages 5, 7, and 9, respectively, P<.0001 at all time points.)
Figure 1.
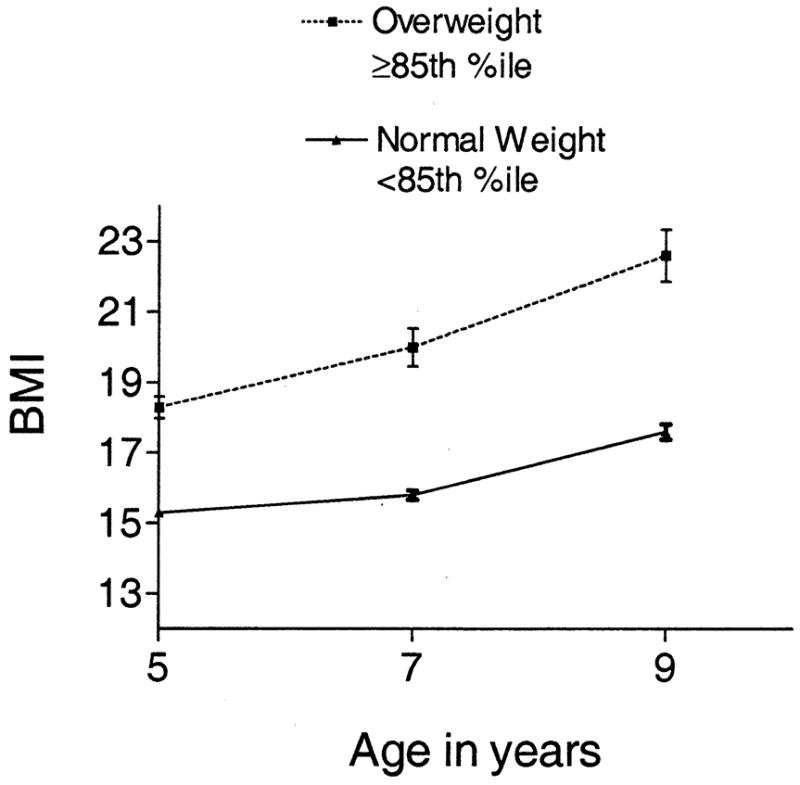
Mean body mass index of overweight and normal-weight girls at the ages of 5, 7, and 9 years.
Figure 2 presents mean levels of restraint at ages 5, 7, and 9 years for girls at risk and not at risk for overweight at age 5. The results of the repeated measures ANOVA showed a significant age-by-weight status interaction (F=3.52, P<.034). At age 5, there were no differences in restraint between girls at risk and not at risk for overweight (F=2.00, P=.16), but at age 7, the difference in restraint between the girls at risk and not at risk for overweight was marginally significant (F=3.59, P<.06), and by age 9 this difference was highly significant (F=27.41, P<.0001), with the at-risk-for-overweight group showing higher levels of restraint. Differences in risk for overweight at age 5 predicted the emergence of differences in restraint at age 9.
Figure 2.
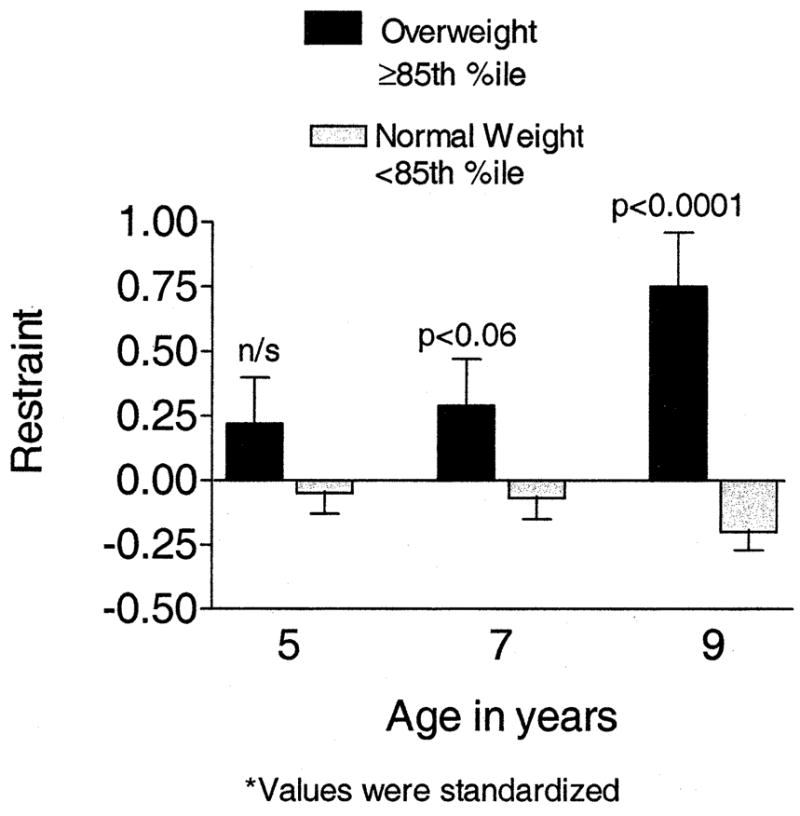
Mean dietary restraint* of overweight and normal-weight girls at the ages of 5, 7, and 9 years.
Figure 3 presents differences in girls’ energy intakes during the EAH laboratory protocol, which was used as a behavioral index of disinhibited overeating. A repeated measures ANOVA showed a significant interaction of risk group and age (F=37.02, P<.05), indicating that from 5 to 9 years, increases in overeating were greater among girls at risk for overweight at age 5 than among the not-at-risk group. Although the risk groups did not differ in the measures of disinhibited overeating at age 5 (F=2.67, P=.11), at the age of 7, girls at risk for overweight were consuming significantly more energy than girls not at risk (F=8.29, P<.005). The difference between the risk groups increased further by age 9 (F=11.26, P<.001), as shown in Figure 3. Consistent with the restraint data, girls at risk for overweight also showed greater increases in overeating in the laboratory.
Figure 3.
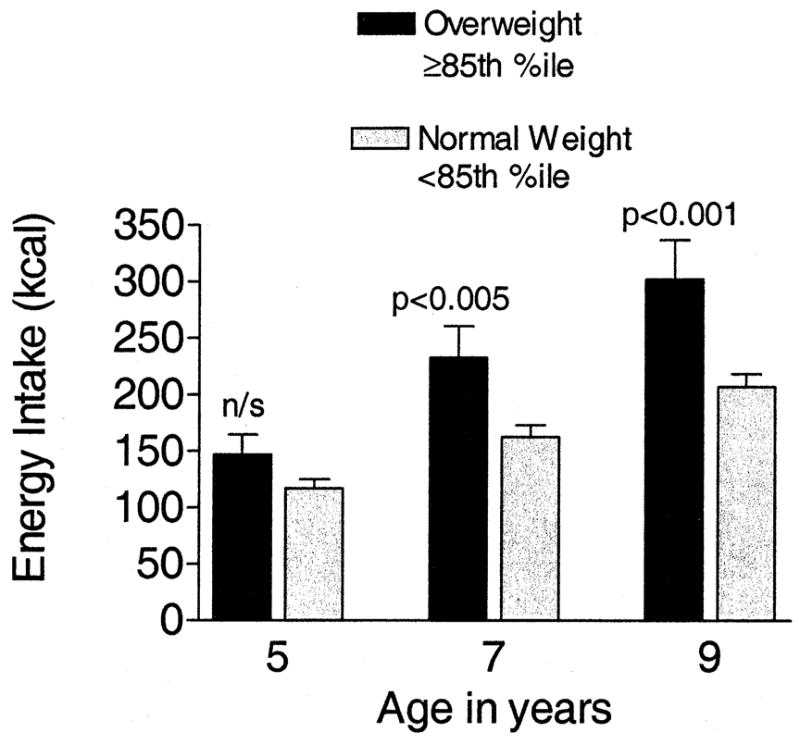
Mean energy intakes of overweight and normal-weight girls during the Eating in the Absence of Hunger protocol.
Standardized weight concern and body dissatisfaction scores at 5, 7, and 9 years are presented for the at-risk and not-at-risk groups in Figures 4 and 5, respectively. By age 9, girls at risk for overweight at age 5 had significantly higher weight concern and body dissatisfaction than girls who were not at risk for overweight. In both cases, the age by risk status interaction was significant, reflecting the differing patterns of change, with the girls at risk for overweight showing greater increases in weight concerns and body dissatisfaction across time; the differences in weight concern and body dissatisfaction between the groups was not significant at age 5, approached significance at age 7, and was highly significant at age 9 for weight concern (F=17.03, P<.0001) and body dissatisfaction (F=13.27, P<.001).
Figure 4.
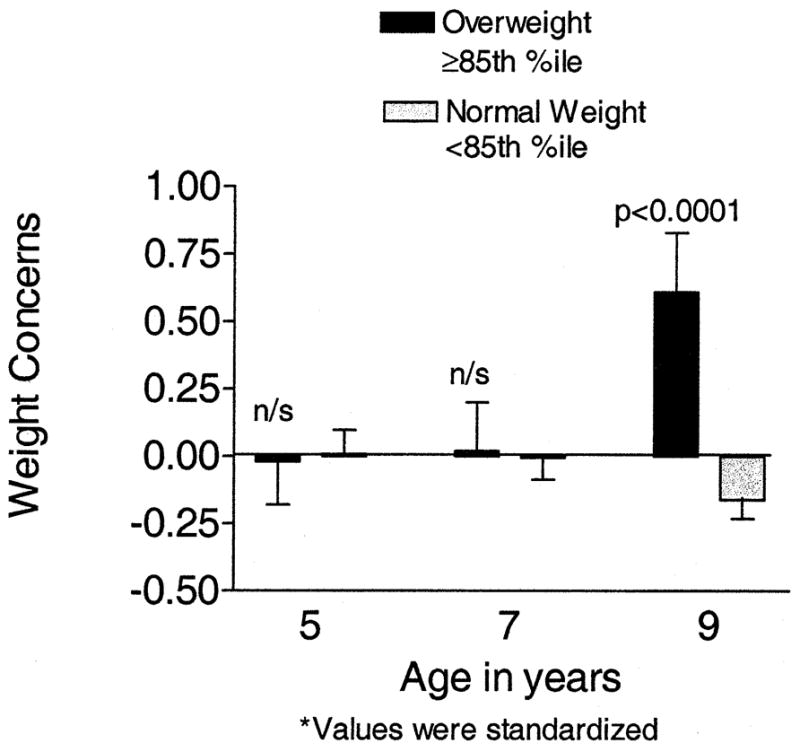
Mean weight concern* of overweight and normal-weight girls at the ages of 5, 7, and 9 years.
Figure 5.
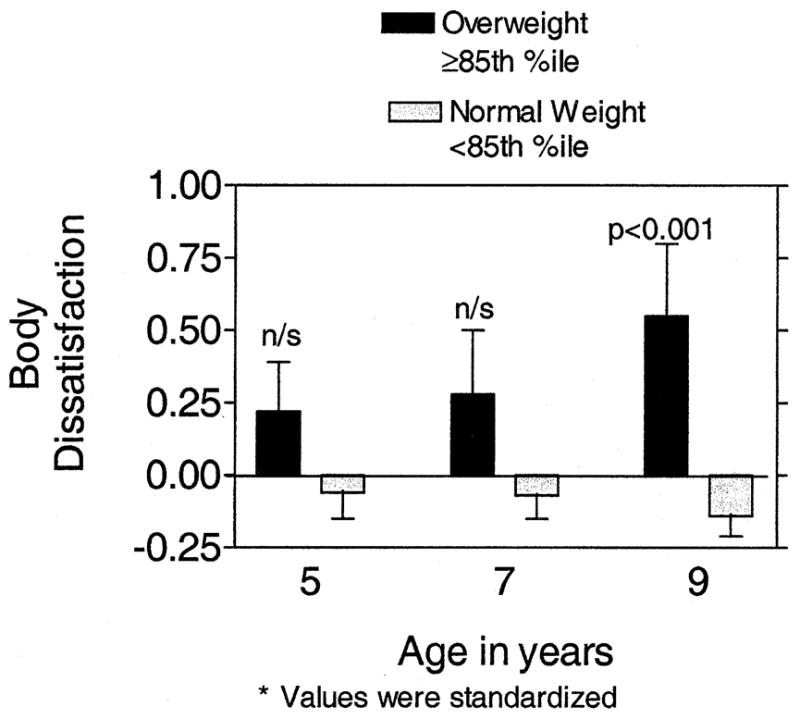
Mean body dissatisfaction of overweight and normal-weight girls at the ages of 5, 7, and 9 years.
DISCUSSION
Longitudinal data were used to investigate the relationship between girls’ risks for overweight at age 5 and the development of dietary restraint, disinhibited overeating, weight concern, and body dissatisfaction during middle childhood. Findings showed that girls who were at risk for overweight at age 5 had higher levels of dietary restraint, disinhibited overeating, weight concern, and body dissatisfaction by age 9. At age 5, there were no differences between the weight status groups in dietary restraint; at age 7, there was a trend for dietary restraint to be higher among overweight girls. By age 9, the at-risk-for-overweight girls had significantly higher levels of dietary restraint than their normal-weight peers. This pattern of findings shows that girls who were categorized as at risk for overweight at age 5 remained at risk for overweight at age 9, and that risk status at age 5 moderated increases in BMI from ages 5 to 9, with girls at risk showing greater increases in BMI and BMI z-scores from ages 5 to 9 years. Relative to girls not at risk for overweight at age 5, girls at risk for overweight were also at greater risk for the development of restrained eating, aspects of disinhibited eating, higher weight concerns, and greater body dissatisfaction.
This research, in addition to showing the importance of weight status in the development of dietary restraint, also investigated associations between weight status and the emergence of aspects of disinhibited eating in girls. Our findings provide evidence linking elevated weight status to both dietary restraint and the development of disinhibited overeating eating behaviors. For example, by age 7, overweight girls ate significantly more palatable food in the absence of hunger, providing evidence that their higher weight status was associated with some aspects of disinhibited eating. Among adults and adolescents, self-initiated attempts at dietary restraint tend to fail, placing individuals at increased risk for disinhibited overeating (10). Our findings show that a similar pattern of relationships might exist among young girls; it is possible that early attempts at restraint lead to disinhibited overeating. However, it is also possible that during development, disinhibited overeating precedes and triggers attempts at restraint, and other research in our laboratory suggests that eating in the absence of hunger is fostered by mothers’ uses of restrictive feeding practices, especially among overweight girls (25).
Although our research indicates that differences in weight status temporally precede the development of differences in both restraint and disinhibition, the causal direction of relationships remains a question, especially in light of recent findings providing evidence for a genetic influence on eating in the absence of hunger, our measure of disinhibited overeating, which was also involved in the expression of obesity among Hispanic children (26). Even during the preschool period, before any evidence for the emergence of dietary restraint, maternal feeding practices that restrict children’s access to palatable foods can promote children’s overeating (16,27). The use of restrictive feeding practices may occur in middle-class families in response to parental concerns about children’s risk for overweight, which is seen as a threat to children’s healthy development (28). However, rather than promoting moderation, these feeding practices can promote disregulated overeating in children (25). The bidirectional influence inherent in relationships between parents and children will probably preclude establishing clear causal relationships among children’s weight status, restrictive parental feeding practices, children’s overeating, and the emergence of restraint. However, it is clear that among our sample, girls who were at early risk for overweight were also at risk for developing higher levels of dietary restraint, disinhibited overeating, and elevated weight concerns and body dissatisfaction during middle childhood.
The contemporary cultural obsession with thinness and the overwhelming aversion to obesity has been observed in both adults and children (18,29), and stigmatization and failure of self-initiated weight control attempts among the obese have been linked to low self-esteem and poor self-image among obese individuals (30). Consistent with previous reports for older children and adolescents, the present findings show that by age 9, girls who were at risk for overweight at age 5 have already begun to experience higher levels of weight concern and body dissatisfaction than their normal-weight counterparts. Although these attributes are linked to restraint between the ages of 5 and 9, when controlling for weight status at age 9, the associations between body dissatisfaction and restraint and between weight concern and restraint disappeared. This pattern of findings suggests that by age 9, these relationships were primarily attributable to girls’ weight status. Consistent with the work of Braet and Wydhooge (31), this pattern also provides evidence that elevated weight status is a predictor of dietary restraint.
Results from this study identify weight status as a key predictor of emerging dietary restraint and disinhibition among young girls. With the prevalence of obesity continuing to increase in young children, weight loss efforts may be advisable for these children; however, this study presents evidence that higher levels of dietary restraint do not promote effective weight control among girls at risk for overweight; girls at risk for overweight had greater increases in restraint from ages 5 to 9 years, but increasing levels of restraint among at-risk girls were accompanied by greater increases in weight status during middle childhood. The present findings are consistent with recent research indicating that self-initiated dieting attempts by children and adolescents tend to lead to additional weight gain, not weight loss (13,32), and may also heighten weight concern and body dissatisfaction.
CONCLUSIONS
Evidence supporting the role of girls’ weight status at age 5 as a risk factor for the emergence of dietary restraint, disinhibited overeating, weight concern, and body dissatisfaction during middle childhood emphasizes the need for developing programs focused on the prevention and early treatment of childhood overweight. Girls at risk for overweight at age 5 tended to remain overweight across middle childhood, and self-initiated attempts at dietary restraint fail to attenuate increases in weight status, suggesting that programs designed to prevent and treat childhood overweight should begin early, during the preschool period. To be successful in creating eating and activity environments that promote healthful weight status, interventions to address childhood obesity will have to promote change at multiple levels, addressing activity patterns and the food intake, and will have to include initiatives at the federal policy level, within the food industry, at the neighborhood and community level, and within families (33). With respect to supporting healthful weight control within families, parents and children need positive alternatives to self-imposed dietary restraint. Early prevention should include an emphasis on structuring the eating environment to promote children’s learning to like foods lower in energy density and higher in nutrient density, such as fruits and vegetables. Because many parents of children at risk for overweight are themselves overweight, primary prevention programs for children should also focus on providing healthful weight control strategies for both overweight parents and their children. Alternative strategies to parents’ self-imposed dietary restraint should include providing clear information regarding both appropriate portion sizes for parents and for children and strategies for choosing foods lower in energy density when selecting foods prepared outside the home, and providing information on preparation techniques that can lower the energy density of foods prepared at home. Finally, information should be included on how to increase physical activity and reduce sedentary activity for all family members. Providing positive strategies for promoting healthful weight control among parents is particularly critical because parents serve as models for young children’s developing eating and activity patterns, and parents also structure children’s eating and activity environments in ways that can either support or undermine the development and maintenance of healthful weight status in children.
Acknowledgments
This research was supported in part by National Institutes of Health Grant RO1 HD32973, The National Dairy Council, and the services provided by the General Clinical Research Center of the Pennsylvania State University are appreciated, supported by National Institutes of Health Grant M01 RR10732.
References
- 1.Herman CP, Polivy J. Anxiety, restraint and eating behavior. J Abnorm Psychol. 1975;84:666–672. [PubMed] [Google Scholar]
- 2.Polivy J, Herman CP. Dieting and binging—A causal analysis. Am Psychol. 1985;40:198–201. doi: 10.1037//0003-066x.40.2.193. [DOI] [PubMed] [Google Scholar]
- 3.Wardle J. Eating style: A validation study of the Dutch Eating Behavior Questionnaire in normal subjects and women with eating disorders. J Psychosom Res. 1987;31:161–169. doi: 10.1016/0022-3999(87)90072-9. [DOI] [PubMed] [Google Scholar]
- 4.Striegel-Moore RH, Silberstein SR, Rodin J. Toward an understanding of risk factors for bulimia. Am Psychol. 1986;41:246–263. doi: 10.1037//0003-066x.41.3.246. [DOI] [PubMed] [Google Scholar]
- 5.Attie I, Brooks-Gunn J. Development of eating problems in adolescent girls: A longitudinal study. Devel Psychol. 1989;25:70–79. [Google Scholar]
- 6.Levine MP. Student Eating Disorders: Anorexia Nervosa and Bulimia. Washington, DC: National Education Association; 1987. [Google Scholar]
- 7.Carper JL, Fisher JO, Birch LL. Young girls’ emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite. 2000;35:121–129. doi: 10.1006/appe.2000.0343. [DOI] [PubMed] [Google Scholar]
- 8.Cutting TM, Fisher JO, Grimm-Thomas K, Birch LL. Like mother, like daughter: Familial patterns of overweight are mediated by mothers’ dietary disinhibition. Am J Clin Nutr. 1999;69:608–613. doi: 10.1093/ajcn/69.4.608. [DOI] [PubMed] [Google Scholar]
- 9.Stice E. A prospective test of the dual-pathway model of bulimic pathology: Mediating effects of dieting and negative affect. J Abnorm Psychol. 2001;110:124–135. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- 10.Stice E. Risk and maintenance factors for eating pathology: A meta-analytic review. Psychol Bull. 2002;128:825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- 11.Marchi M, Cohen P. Early childhood eating behaviors and adolescent eating disorders. J Am Acad Child Adolesc Psychiatry. 1990;29:112–117. doi: 10.1097/00004583-199001000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Troiano RP, Flegal KM. Overweight children and adolescents: Description, epidemiology, and demographics. Pediatrics. 1998;101:497–504. [PubMed] [Google Scholar]
- 13.Stice E, Mazotti L, Krebs M, Martin S. Predictors of adolescent dieting behaviors: A longitudinal study. Psychol Addict Behav. 1998;12:195–205. [Google Scholar]
- 14.Allison D. Handbook of Assessment Methods for Eating Behaviors and Weight Related Problems. Thousand Oaks, CA: Sage Publications; 1995. [Google Scholar]
- 15.Braet C, Van Strien T. Assessment of emotional, externally induced and restrained eating behaviour in nine to twelve-year-old obese and non-obese children. Behav Res Ther. 1997;35:863–873. doi: 10.1016/s0005-7967(97)00045-4. [DOI] [PubMed] [Google Scholar]
- 16.Fisher JO, Birch LL. Restricting access to a palatable food affects children’s behavioral response, food selection and intake. Am J Clin Nutr. 1999;69:1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- 17.Birch LL, Davison KK, Fisher JO. Learning to overeat: Maternal use of restrictive practices promotes girls’ eating in the absence of hunger. Am J Clin Nutr. 2003;78:215–220. doi: 10.1093/ajcn/78.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davison KK, Birch LL. Weight status, parent reaction, and self-concept in 5-year-old girls. Pediatrics. 2001;107:46–53. doi: 10.1542/peds.107.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Strien T, Fritjers JER, Bergers GPA, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional and external eating behavior. Int J Eat Disord. 1986;5:295–315. [Google Scholar]
- 20.Fisher J, Birch L. Eating in the absence of hunger and overweight in girls at 5 and 7 y of age. Am J Clin Nutr. 2002;76:226–231. doi: 10.1093/ajcn/76.1.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Killen JD, Taylor CB, Hayward C, Wilson DM, Hayde F, Hammer LD, Simmonds B, Robinson TN, Lih I, Varaday A, Kraemer H. Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: A three-year prospective analysis. Int J Eat Disord. 1994;16:227–238. doi: 10.1002/1098-108x(199411)16:3<227::aid-eat2260160303>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 22.Mendelson BK, White DR. Relation between body-esteem and self-esteem of obese and normal children. Percept Mot Skills. 1982;54:899–905. doi: 10.2466/pms.1982.54.3.899. [DOI] [PubMed] [Google Scholar]
- 23.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL. CDC Growth Charts: United States. Advance Data From Vital and Health Statistics. Hyattsville, MD: National Center for Health Statistics; 2000. [PubMed] [Google Scholar]
- 24.Length and Stature for Age, Weight for Age, and Weight for Length and Stature. Washington, DC: US Department of Health and Human Services, Center for Disease Control and Prevention; 2000. Normalized NCHS/CDC Anthropometric References. [Google Scholar]
- 25.Fisher JO, Rolls BJ, Birch LL. Children’s bite size and intake of an entree are greater with large portions than with age-appropriate or self-selected portions. Am J Clin Nutr. 2003;77:1164–1170. doi: 10.1093/ajcn/77.5.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fisher JO, Butte NF, Jaramillo SJ. Eating in the absence of hunger as a behavioral phenotype of overweight Hispanic children. Fort Lauderdale, FL: North American Association for the Study of Obesity (NAASO); 2003. [Google Scholar]
- 27.Fisher JO, Birch LL. Restricting access to foods and children’s eating. Appetite. 1999;32:405–419. doi: 10.1006/appe.1999.0231. [DOI] [PubMed] [Google Scholar]
- 28.Costanzo PR, Woody EZ. Domain specific parenting styles and their impact on the child’s development of particular deviance: The example of obesity proneness. J Soc Clin Psychol. 1985;3:425–445. [Google Scholar]
- 29.Lerner RM, Gellert E. Body build, identity, preference and aversion in children. Dev Psychol. 1969;1:456–462. [Google Scholar]
- 30.Puhl R, Brownell KD. Bias, discrimination and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 31.Braet C, Wydhooge K. Dietary restraint in normal weight and overweight children: A cross-sectional study. Int J Obes Relat Metab Disord. 2000;24:314–318. doi: 10.1038/sj.ijo.0801129. [DOI] [PubMed] [Google Scholar]
- 32.Field AE, Austin S, Taylor CB, Malspeis S, Rosner B, Rockett HR, Gillman MW, Colditz GA. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics. 2003;112:900–906. doi: 10.1542/peds.112.4.900. [DOI] [PubMed] [Google Scholar]
- 33.Davison KK, Birch LL. Childhood overweight: A contextual model and recommendations for future research. Obes Rev. 2001;2:159–171. doi: 10.1046/j.1467-789x.2001.00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


