Abstract
The informed consent process is a cornerstone of modern medical research. This study was conducted to explore the process in the context of neurooncology clinical trials. Qualitative methodology and analysis were used on open-ended, face-to-face interviews conducted with 21 patients. Six comprehensive themes emerged: (1) general understanding of the objectives and purpose of clinical trials was good, (2) recall of risks was low, (3) patients did not believe that their care would be compromised by forgoing the clinical trial, (4) patients felt participation was voluntary and free of coercion, (5) patients would not have withdrawn from the trial in the event of complications, and (6) patients were satisfied with the informed consent process. Informed consent is a dynamic process; when appropriately executed, it can be a powerful safeguard protecting patient autonomy. If sufficient time is allowed to deliberate participation and ample opportunity is provided for information sharing and disclosure, researchers can be confident that participants are knowledgeable about the trial and aware of their rights.
Keywords: brain tumor, clinical trials, informed consent, neurooncology
The informed consent process emerged out of the Nuremburg Trials to protect human research subjects.1 In the ensuing 60 years, it has become the ethical cornerstone of medical practice.2–4 Modern informed consent consists of five tenets: voluntariness, disclosure, understanding, competence, and consent.5 Voluntariness refers to patients giving their agreement free of any coercion or pressure. Disclosure is largely the burden of the researcher to inform the patient of all reasonable information pertaining to the research, but particularly to the risks of the trial. Understanding refers to the patients’ comprehension of the information provided them. Competence is the ability of the patient to understand all the important information available. Finally, consent is the event whereby patients agree to the proposed medical treatment. For the most part, consent is obtained in written form, but for some, especially noninvasive and relatively risk-free research, consent may be obtained verbally.6,7
Research on this topic has shown that although the principles of informed consent are well cemented in medical practice, patients do not always benefit from these principles. Obstacles to informed consent include patients’ lack of understanding of the material presented.8 This may be due to the consent forms’ being laden with unfamiliar terminology. Other reasons include inherent biases, cultural differences, diverse levels of education, and personal expectations.5,9
The issue of informed consent acquires a new dimension when discussed in the context of clinical trials.9,10 Such trials are required for the continued progress of modern medicine and to help determine clinical guidelines and treatment standards. As with any medical intervention, however, clinical trials require a delicate balance between risks and benefits. The benefits of further progress and knowledge acquisition inherent in a clinical trial need to be weighed against the risks, direct or indirect, to the participants. The goal of any clinical trial, therefore—and the principle that underlies its theoretical basis—remains a utilitarian one of maximal benefit to the most number of people.11 The physician-researcher thus must carefully navigate the line between individual risk and community benefit.
Although sound ethical practice demands that all risks and potential benefits be expressed to the patient, this disclosure must be accomplished without creating an overt sense of doom or false hope.12 Such a balance has been sought in the informed consent form for clinical trials. Unfortunately, research has shown that the same obstacles that hinder therapeutic informed consent are especially prominent in the informed consent for clinical trials. For example, one study has found that patients are confused or unclear about the concept of randomization, a feature that is an essential part of many clinical trials.13 Others have found that therapeutic misconception, which is the belief that investigation is an extension of treatment and that it is especially likely to be effective, is fairly widespread.14 It has become clear that despite the prevalence of clinical trials, patients still have difficulty understanding the differences between research and treatment. This so-called therapeutic misconception is further heightened by the participants’ trust in the physician- patient relationship, and the impression that their physician will always have their best interests in mind. The implications of these beliefs on voluntariness are clear, as one has to carefully examine whether patients are being indirectly influenced to enroll in trials. Given all these obstacles and misconceptions, one hypothesis that has emerged is that, in the context of modern medicine, fully informed consent may well be impossible.2
Some researchers have found that patients prefer an active decision-making process wherein they interact with their physicians and research team.8,15 In such a context, informed consent becomes more than a signature on a form—it becomes a dynamic process.16–18
The present study examines the informed consent process in the context of neurooncology clinical trials. In this setting, given their grave diagnoses, patients were presumed to be under significant stress. Their views on the informed consent process were examined, as were their sentiments during the process and their recollection of it.
Materials and Methods
Design
Qualitative methodology was used. Open-ended, face-to-face interviews were conducted with patients diagnosed with terminal brain cancer who were enrolled in various neurooncology clinical trials.
Setting/Participants
Participants were patients who had been referred to the ambulatory neurooncology clinic at a large urban teaching hospital and enrolled in one of the ongoing neurooncology clinical trials. Our study was concerned with randomized trials in phase I–III involving glioblastoma multiforme (GBM). The patient’s partner was welcome to participate in the interview along with the patient. Exclusion criteria included patients who (1) did not speak English well, (2) had cognitive or speech difficulties, (3) were deemed psychologically unable to participate in the interview, and (4) had signed consent for the clinical trial more than 1 month prior to the interview date.
Sample Size
Thirty (30) interviews were sought, but because of logistical difficulties, 21 were conducted during the study time period. We do not believe this diminished the integrity of the study because we deemed the sample sufficient to reach saturation (a term used in qualitative research to indicate a point beyond which no new information or ideas can arise).19
Data Collection
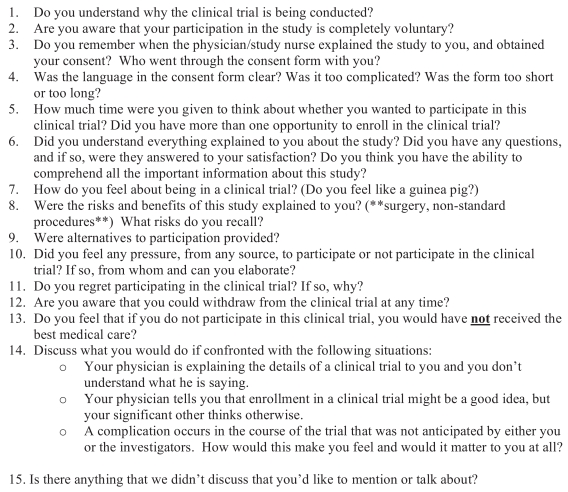
Open-ended, face-to-face interviews were conducted with participants within 1 month of their signing the consent form for a clinical trial. This time frame was chosen to ensure that patients still recalled the informed consent process that they had undergone and to avoid any biasing effect of the outcomes of the trial. The interview questions were based on a guide containing questions about the informed consent form, the process, and explicit scenarios (Fig. 1). Themes were explored as patients brought them to light. All interviews were audiotaped and transcribed. Demographic data were collected for all patients.
Fig. 1.
Interview guide used in the study.
Data Analysis
Modified thematic analysis was conducted by four reviewers. The interview transcripts were read and overarching themes extracted and analyzed.
Research Ethics
The study was approved by the Research Ethics Board at the University Health Network, and written, informed consent was obtained from each participant. Transcripts were anonymized.
Results
Patient Information
Twenty-one patients were interviewed between June 2006 and August 2007 (Table 1). During this 13-month period, 30 patients were enrolled in neurooncology clinical trials. Therefore, 21 of 30 (70%) of eligible neurooncology patients participated. Of those who did not participate, three patients had declined to participate, and five were not interviewed owing to scheduling conflicts.
Table 1.
Patient demographic data
| Characteristic | Study Group |
|---|---|
| Age (years) | |
| Mean | 49 |
| Median | 52 |
| Range | 26–65 |
| Sex (n) | |
| Male | 14 |
| Female | 7 |
| Marital status (n) | |
| Married | 14 |
| Single | 1 |
| Widowed | 1 |
| Divorced | 2 |
| Separated | 1 |
| Common law | 2 |
| Education (n) | |
| Postsecondary | 12 |
| Secondary | 9 |
| Employment (n) | |
| Employed | 19 |
| Unemployed | 1 |
| Retired | 1 |
| Days in trial (n) | |
| Mean | 8 |
| Median | 1 |
| Range | 1–30 |
All interviews were conducted by the first author (E.K.), who had no therapeutic relationship with the patients.
Thematic Analysis
Analysis of the interviews yielded six overarching themes, described below and illustrated with verbatim quotes from patients.
(1) General understanding of the clinical trial was good. All patients expressed an adequate and largely correct general understanding of the purpose of the clinical trial they were enrolled in:
They’re investigating the reaction of a new chemical agent or biological agent in terms of treating the progression or advancement or recurrence of brain tumors.
Regarding the conceptual understanding of trials themselves, many patients acknowledged that, although the treatment may not help them, they hoped it would benefit others in the future. For a few, this altruistic notion was a major factor in their decision to enroll in the clinical trial:
You know it may not help me but it will somebody.
One-third of patients explicitly mentioned that they had enrolled in the trial in hopes that it would treat their condition:
I feel like I’ve been given an opportunity for treatment.
and
I was actually keen to participate because if it’s something that’s gonna help me, then I have an invested interest in that.
Some patients acknowledged that they may not have understood all the important information when it was initially presented to them in clinic, but they stated that taking the consent papers home and having unlimited time to think about them made them feel confident that they did understand the trial:
Q: Do you feel that in your state at the time you had the ability to understand all the important information in the clinical trial?
A: I think so and the fact that I could take it home and investigate things that I wasn’t sure about.
(2) Recall of the risks associated with the clinical trial was low. Nearly one-third of patients (6/21; 29%) admitted to not recalling any risks of the trial drug, although they did assert that it had been mentioned to them and was present on the consent form:
Q: What risks do you recall?
A: Um . . . all the, uh, negative things. Ah, I don’t remember now because I have to have the papers in front of me.
The rest of the patients only recalled general risks such as gastrointestinal upset. At most they mentioned up to four specific risks or side effects:
Just like any other drug, um, nausea, diarrhea, like just your basic and they list 50 of them [risks] because they’re not really sure . . . it’s more overboard.
The range of risks with all the ongoing clinical trials at the clinic was 30 to 48 specific risks listed on the informed consent forms for the various trials.
(3) Patients believed refusal to enroll would not impact treatment. Eighteen of 21 patients (86%) felt that their care would not be compromised or be suboptimal if they decided not to participate in a clinical trial:
I think I’m getting excellent care regardless of being in the study or not.
The other three patients reported that they felt they got better care in the trial because they were given the opportunity to try a treatment that they felt might be more effective. Of note, traditional treatment for many patients had failed, and their illness had progressed:
I think that this is a really viable treatment and will buy me months and years potentially. Yeah, I think I probably wouldn’t have received the best medical care otherwise.
(4) Decision to participate in the study was voluntary and free of coercion. When faced with a scenario in which a family member disagreed with the advice of the doctor to participate in a clinical trial, the majority of patients (14/21; 67%) indicated that they would not necessarily make the decision based solely on the doctor’s directions. They indicated a variety of factors such as listening to their loved one(s), doing further research, or simply making up their own minds:
I would listen to my significant other and the physician and then do further research.
The remaining one-third who said they would follow the doctor’s advice made the following comments indicating faith in the doctor’s expertise:
I would go with the doctor. I mean you would . . . I don’t know . . . unless my better half was a doctor but if I mean that’d be like if you’re shopping for cars you go to find somebody that sells vacuum cleaners.
and
Doctor says, “Hey, we’d like to do these tests on you because it will help other people with cancer.” Go ahead and do it. That’s, you know, . . . I have infinite faith in the doctors. All I’m trying to do is save my life.
The vast majority of patients (19/21; 90%) also stated that they did not feel any pressure from any source to participate or not to participate in the clinical trial. The two patients who did feel pressure stated that it was from themselves:
Q: Did you feel any pressure from any source to participate or not to participate in the clinical trial?
A: Not at all. Not at all. Just from myself because I wanted to . . . ehh . . . I want to explore every option for myself.
(5) Complication did not cause dropout from study. If faced with a complication in the trial, the majority of patients (14/21; 67%) indicated that they would not consider withdrawing from the study, although some did mention that they might be upset:
I’d probably be upset but not upset that I’d decided to take part in the trial because I know that those risks come with that.
Two patients were unsure how they would react to complications, and five explicitly stated that they would consider withdrawing from the trial depending on how severe the complication was and how much it interfered with their lives:
If it happened that I was going back to work and it was really affecting the work, then that might persuade me to think about not continuing. But it all depends on, you know, how tolerable it was.
(6) Overall satisfaction with the process was good. The majority of patients (18/21; 86%) seemed satisfied overall with the informed consent process. Some indicated that they were initially somewhat confused about certain aspects of the trial but that their concerns were clarified by the staff. A few patients felt that the whole process was too rushed, but they also realized the urgency of their situation, so they were more satisfied than upset by the swiftness of the process. Patients appreciated the time to think their decisions over:
I think having the delay in time when you could go away and think about it and give it some consideration is really useful . . . I think that makes a difference for the informed consent because it gives you a chance to mull it over and, for me anyway, I find that that’s important.
The two patients who expressed some dissatisfaction with the process indicated that they wished there had been more information available to them regarding the study and that taking the informed consent papers home to read was not enough:
After all of it, the only thing that I would say is that they should sit with you when you’re reviewing it because there are questions that you have, or if not at the moment, send you home and then you come back and say you have 15 minutes to discuss this.
Overall, none of the patients regretted participating in the clinical trial.
Discussion
The present study explores the views of patients enrolled in neurooncology clinical trials regarding the informed consent process. Although this process has been investigated, few studies, if any, have examined it in a high-stakes setting such as a neurooncology clinical trial. Given the grave diagnosis of malignant brain tumor, an effective and ethically sound informed consent process for a clinical research trial becomes that much more important.
The present study is unique in that (1) it employed open-ended interviews to allow patients to elaborate on their thoughts, (2) it recruited patients within 1 month of having signed the informed consent to avoid the bias of early study outcomes, (3) it explored the informed consent process in the unique context of clinical trials on patients with brain cancer, and (4) the focus was on patients’ feelings about the informed consent process, the factors that influenced their decision to participate, and their general knowledge of the clinical trial.
Our study showed that the requirements of informed consent were fulfilled in the setting studied herein. The patients were all aware that they had voluntarily agreed to participate in the trial, without any coercion or pressure, and that the option to withdraw was available to them at any time. They all showed a good understanding of the general principles of the study; they could describe it to the interviewer. Most also felt that they had been provided with sufficient information before participating and further appreciated the time they were given to consider participation prior to formal enrollment.
As with previous studies, our study found that participants in clinical research recall very few specific risks related to their trials.20–22 Krupp asked patients to write down all risks they recalled 2 h after a consent interview.21 On average, participants recalled 4 risks out of a possible 32 for cranial surgery and 25 for spinal surgery. Of six “typical major risks,” 65% of participants did not recall more than two. In Fortney’s study, only 23% of women correctly recalled the risk of pregnancy on the trial contraceptive.20 The present study agrees with both these findings. Patients seem to recall only general risks and at most can name four examples. Several reasons may account for this recall failure. One possibility is that patients simply do not care to know or remember the risks involved, although this is highly unlikely since most acknowledged that their life and health were important factors in the clinical trial. Other patients may feel that they are somehow less vulnerable to the risks than the “typical” patient, or perhaps they may be protecting themselves psychologically by blocking out the most salient risks, such as seizure or coma. Also, patients may feel that their illness poses a greater and more immediate threat to morbidity and mortality than the risks inherent in a clinical trial. These and other factors affect people’s perceptions of risk, which could ultimately account for the low recall of risks.22
Contrary to other studies, the present investigation revealed that patients do have a good understanding of the purpose of the clinical trial they are undergoing.5,20,23 In Fortney’s study, some women actually failed to mention the research aspect of it, and many thought the purpose was to help them avoid getting pregnant.20 Agard et al. similarly found that patients in a myocardial infarction study understood very little about the study before they signed up.23 However, the patients in that study were given the informed consent form soon after having a heart attack, while they were still heavily medicated. Both these factors may account for their lack of understanding.
In our study, some patients did admit to less than full comprehension when information was initially provided about the study. However, they reported a significant improvement in their understanding following a review of the consent package at home, taking the opportunity to explore the package at their convenience and to independently research and seek assistance in understanding the details of the trial. Most participants benefited from and valued the time between being presented with the information and returning to the hospital to sign the consent form. This time period gave them a unique advantage over previously studied clinical trial participants and most likely explains their higher knowledge levels. Furthermore, none of the patients had any cognitive deficits—an exclusion criterion of the study—which would, of course, increase their capacity to comprehend the information about the trial.
“Therapeutic misconception” is a term that refers to patients’ erroneous belief that the main purpose of the trial in question is beneficial treatment rather than investigation. Clearly, the acquisition of informed consent when patients are under the assumption that they are essentially participating in further positive treatment rather than investigation is ethically problematic. Therapeutic misconception was only somewhat prevalent in this study as compared with others.24 In a study of the effect of antibiotics on preterm labor, Kenyon revealed that the women’s primary reason for enrollment in the trial was the possibility of improving the outcome for their babies.24 In our study only a minority of patients explicitly expressed the view that the trial was meant to treat or improve their condition. Most showed an understanding that it was indeed a research endeavor. Furthermore, very few patients believed that their care would be compromised if they did not enroll in the clinical trial, and almost no patients indicated a desire to withdraw should complications occur. In general, the overall attitude of the participants was positive toward research and clinical trials, despite the acknowledged inherent uncertainty of medical research.
As with all studies, the present one has its limitations. Although the objective of qualitative analysis is not necessarily to provide generalizable results, our study was conducted in a teaching hospital within a socialized medical system. Whether findings would be similar in other settings and health care systems remains to be investigated, although we have no reason to believe that results would be different.
Also, owing to the qualitative methodology and use of open-ended interviews, it is possible that certain themes were overlooked. Despite our use of an interview guide (Fig. 1), ideas were explored freely as they were brought up by patients. However, it is possible that important questions were not posed.
The number of patients, although within the acceptable range for qualitative research, was still small. If and when a larger sample size is used, the results might change or new themes arise, but we suspect that saturation was achieved.
Finally, the results of this study were surprisingly positive. Patients in this study may have been slightly more knowledgeable than those enrolled in other studies because they had already spent much time in the medical system and had received a very serious diagnosis. They would have gone through extensive workups to receive their diagnosis, then neurosurgery and standard radiation and chemotherapy. This time would allow them to familiarize themselves with their condition so that by the time they came to the clinical trial, it was easier for them to understand its purpose. Also, most patients were allowed ample time to consider enrollment in the trial, which gave them the opportunity to further research areas of the trial that may have been ambiguous to them initially. All these factors may have contributed to producing the rather positive outcomes.
Conclusions
The informed consent process in the neurooncology clinical trials population studied herein seems to be effective. Based on these results, we can make three suggestions to improve patient autonomy and ethical integrity: (1) the provision of sufficient time between the initial presentation of the clinical trial and the signing of the consent form (this will allow patients to conduct their own investigations and consolidate their knowledge); (2) staff involved in the research should be readily available to answer any questions patients may have pertaining to the clinical trial; and (3) the informed consent forms should suitably emphasize both risks and benefits and should be written in a clear, easy-to-understand language. As much as possible, treatment should be kept separate from research to minimize therapeutic misconception. Clinical, diagnostic, and prognostic information should be disclosed and discussed separately from research and clinical trial information, perhaps in different settings and at different times.
The acquisition of informed consent is a dynamic process. A dialogue that prioritizes patient autonomy and well-being should take place between the research team and the participant, and relevant questions and concerns should be addressed before, rather than after, enrollment.
Acknowledgments
We thank the dedicated neurooncology nurses for help in arranging the patient interviews. This work was partly funded by Canadian Institute of Health Research grant MOP 77670.
References
- 1.Weindling P. The origins of informed consent: the international scientific commission on the medical war crimes, and the Nuremberg code. Bull Hist Med. 2001;75:37–71. doi: 10.1353/bhm.2001.0049. [DOI] [PubMed] [Google Scholar]
- 2.Bernstein M. Fully informed consent is impossible in surgical clinical trials. Can J Surg. 2005;48:271–272. [PMC free article] [PubMed] [Google Scholar]
- 3.Etchells E. Informed consent in surgical trials. World J Surg. 1999;23:1215–1219. doi: 10.1007/s002689900650. [DOI] [PubMed] [Google Scholar]
- 4.Rajput V, Bekes CE. Ethical issues in hospital medicine. Med Clin North Am. 2002;86:869–886. doi: 10.1016/s0025-7125(02)00013-5. [DOI] [PubMed] [Google Scholar]
- 5.Kanerva A, Suominen T, Leino-Kilpi H. Informed consent for short-stay surgery. Nursing Ethics. 1999;6:483–493. doi: 10.1177/096973309900600604. [DOI] [PubMed] [Google Scholar]
- 6.Dandry T, Catalano J. Legal, Ethical and Political Issues in Nursing. Philadelphia: Davis; 1993. [Google Scholar]
- 7.Fisher F, McDonald N-J, Weston R, et al. Medical Ethics Today: Its Practice and Philosophy. Plymouth, UK: Latimer Trend; 1995. [Google Scholar]
- 8.Bernat JL, Peterson LM. Patient-centered informed consent in surgical practice. Arch Surg. 2006;141:86–92. doi: 10.1001/archsurg.141.1.86. [DOI] [PubMed] [Google Scholar]
- 9.Sankar P. Communication and miscommunication in informed consent to research. Med Anthropol Q. 2004;18:429–446. doi: 10.1525/maq.2004.18.4.429. [DOI] [PubMed] [Google Scholar]
- 10.Korn EL, Baumrind S. Randomised clinical trials with clinician- preferred treatment. Lancet. 1991;337:149–152. doi: 10.1016/0140-6736(91)90809-4. [DOI] [PubMed] [Google Scholar]
- 11.Dudley HA. Informed consent in surgical trials. Br Med J (Clin Res Ed) 1984;289:937–938. doi: 10.1136/bmj.289.6450.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daugherty C. Impact of therapeutic research on informed consent and ethics of clinical trials: a medical oncology perspective. J Clin Oncol. 1999;17:1601–1617. doi: 10.1200/JCO.1999.17.5.1601. [DOI] [PubMed] [Google Scholar]
- 13.Featherstone K, Donovan JL. Random allocation or allocation at random? Patients’ perspectives of participation in a randomised controlled trial. BMJ. 1998;317:1177–1180. doi: 10.1136/bmj.317.7167.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kimmelman J, Palmour N. Therapeutic misconception in the consent form of phase I gene transfer trials: an empirical analysis. J Med Ethics. 2005;31:209–214. doi: 10.1136/jme.2003.006247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ruiz-Moral R, Rodriguez EP, de Torres LAP, de la Torre J. Physician-patient communication: a study on the observed behaviours of specialty physicians and the ways their patients perceive them. Patient Educ Couns. 2006;64:242–248. doi: 10.1016/j.pec.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Doyal L. Good clinical practice and informed consent are inseparable. Heart. 2002;87:103–106. doi: 10.1136/heart.87.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mazur DJ, Hickam DH. Patients’ preferences for risk disclosure and role in decision making for invasive medical procedures. J Gen Intern Med. 1997;12:114–117. doi: 10.1046/j.1525-1497.1997.00016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raab EL. The parameters for informed consent. Trans Am Ophthalmol Soc. 2004;102:225–232. [PMC free article] [PubMed] [Google Scholar]
- 19.Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Beverly Hills, CA: Sage; 1990. p. 180. [Google Scholar]
- 20.Fortney JA. Assessing recall and understanding of informed consent in a contraceptive clinical trial. Stud Fam Plann. 1999;30:339–346. doi: 10.1111/j.1728-4465.1999.t01-5-.x. [DOI] [PubMed] [Google Scholar]
- 21.Krupp W, Spanehl O, Laubach W, Seifert V. Informed consent in neurosurgery: patients’ recall of preoperative discussion. Acta Neurochir (Vienna) 2000;142:233–239. doi: 10.1007/s007010050030. [DOI] [PubMed] [Google Scholar]
- 22.Lloyd AJ. The extent of patients’ understanding of the risk of treatments. Qual Health Care. 2001;10(suppl I):i14–i18. doi: 10.1136/qhc.0100014... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agard A, Hermeren G, Herlitz J. Patients’ experience of intervention trials on the treatment of myocardial infections: is it time to adjust the informed consent procedure to the patient’s capacity? . Heart. 2001;86:632–637. doi: 10.1136/heart.86.6.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kenyon A, Dixon-Woods M, Jackson CJ, Winderidge K, Pitchforth E. Participating in a trial in a critical situation: a qualitative study in pregnancy. Qual Saf Health Care. 2006;15:98–101. doi: 10.1136/qshc.2005.015636. [DOI] [PMC free article] [PubMed] [Google Scholar]