Abstract
The cardiofaciocutaneous (CFC) syndrome is a condition of sporadic occurrence, with patients showing multiple congenital anomalies and mental retardation. It is characterised by failure to thrive, relative macrocephaly, a distinctive face with prominent forehead, bitemporal constriction, absence of eyebrows, hypertelorism, downward‐slanting palpebral fissures often with epicanthic folds, depressed nasal root and a bulbous tip of the nose. The cutaneous involvement consists of dry, hyperkeratotic, scaly skin, sparse and curly hair, and cavernous haemangiomata. Most patients have a congenital heart defect, most commonly pulmonic stenosis and hypertrophic cardiomyopathy. The developmental delay usually is moderate to severe. The syndrome is caused by gain‐of‐function mutations in four different genes BRAF, KRAS, mitogen‐activated protein/extracellular signal‐regulated kinase MEK1 and MEK2, all belonging to the same RAS–extracellular signal‐regulated kinase (ERK) pathway that regulates cell differentiation, proliferation and apoptosis. The CFC syndrome is a member of a family of syndromes that includes the Noonan and Costello syndromes, presenting with phenotypic similarities. Noonan syndrome is caused by mutations in the protein tyrosine phosphatase SHP‐2 gene (PTPN11), with a few people having a mutation in KRAS. Costello syndrome is caused by mutations in HRAS. The protein products of these genes also belong to the RAS–ERK pathway. Thus, the clinical overlap of these three conditions, which often poses a problem of differential diagnosis, is explained by their pathogenetic relatedness.
The cardiofaciocutaneous (CFC) syndrome (OMIM 115150) is a syndrome where patients have multiple congenital anomalies or mental retardation, failure to thrive, psychomotor delay, a characteristic face, congenital heart defects, and abnormalities of the skin, eyes, gastrointestinal tract and central nervous system. Occurrence is sporadic, with men and women equally affected. The syndrome was first described 20 years ago by Reynolds et al1 in eight children. Additional reports soon followed and, according to a recent review,2 about 59 patients have been reported, providing the basis for an accurate delineation of the phenotypic spectrum of the syndrome. Nevertheless, a question has lingered for many years whether CFC is a unique and separate condition, or a variant of the Noonan syndrome (OMIM 163950)3,4,5,6,7,8,9 or of the Costello syndrome (OMIM 218040).10 These three conditions share several manifestations (table 1)11,12,13 and “borderline” cases do exist, usually in infants, which defy a clear‐cut diagnosis. A useful diagnostic approach was provided with the creation of a CFC index based on 82 clinical traits and their frequencies in the population with the CFC syndrome.14 However, matters changed radically only with the discovery of different genes whose mutations cause each one of these syndromes: the protein tyrosine phosphatase SHP‐2 gene PTPN11 for Noonan syndrome,15HRAS for Costello syndrome,16 and KRAS, BRAF, mitogen‐activated protein/extracellular signal‐regulated kinase MEK1 and MEK2 for CFC.17,18 These discoveries are doubly interesting for (a) finally allowing clarification of the nosology of these three syndromes and (b) explaining their similarities, given that the protein products of the causative genes interact in a common pathway.18 Therefore, it seems timely and appropriate to review the status of the CFC syndrome, providing a thorough clinical and molecular description and a nosological discussion with respect to the Noonan and Costello syndromes (table 1).
Table 1 Phenotypic overlap of the cardiofaciocutaneous, Noonan and Costello syndromes.
| CFC | Noonan syndrome11 | Costello syndrome12,13 | |
|---|---|---|---|
| Head | Relative macrocephaly | Yes | Yes |
| Dolichocephaly | Yes | No | |
| Hair | Sparse, curly, friable | Curly | Fine, sparse, curly, kinky |
| Absent eyebrows | No | No | |
| Face | Tall forehead | Yes | No |
| Narrowed temples | No | No | |
| Small chin | Yes | No | |
| Eye | Palpebral ptosis | Yes | Yes |
| Hypertelorism | Yes | No | |
| Downward‐slanting palpebral fissures | Yes | Yes | |
| Epicanthal folds | Yes | Yes | |
| Exotropia | Strabismus | Strabismus | |
| Ear | Earlobe creases | No | Fleshy lobes |
| Nose | Short | No | Yes |
| Broad nasal base | No | Yes | |
| Mouth | Deep philtrum | Yes | No |
| Cupid's bow lip | No | No |
Prevalence and heritability
No existing neonatal screening or epidemiological studies provide an accurate estimate of the population prevalence of the CFC syndrome. As noted above, about 60 cases are published, most likely representing the tip of an iceberg. More than 100 unpublished cases are known to CFC International, a family‐support group operating worldwide (http://www.cfcsyndrome.org). Even this number must be an underestimate, excluding most of the mildest cases. Molecular confirmation of clinically suspected cases will soon add valuable data to the prevalence issue. All cases described so far are sporadic, most likely due to new dominant mutations, as suggested by the observation of a paternal age effect.19
The phenotype
Growth and longevity
Reynolds et al1 reported that pregnancies of affected women may be complicated by polyhydramnios, although measurements at birth tend to be normal. Postnatally, there is failure to thrive, psychomotor delay and generalised hypotonia.
Short stature is found in 78% of patients.20 Weight is also below the normal growth curve, but there is relative macrocephaly. Bone age is considerably delayed and osteopenia is occasionally observed.21 The typical progression is that a child is born of average weight but then there is failure to thrive, often due to feeding problems.
On the basis of prolonged follow‐up of several affected individuals, it is our impression that the phenotype changes over the years—for example, the face becoming less typical and the hair becoming thicker and more normal. Little is known about the fertility of people with the CFC syndrome. No cases are known of children born to a bona fide parent with the CFC syndrome. Life expectancy is probably shortened on average, due to the early death of those with severe cardiac involvement.
Development and the neurological system
Neurological involvement in the CFC syndrome is extensive, and can involve functions of the cortex, brain stem and ventricular system. Mental retardation and global developmental delay are found in most (81%) cases.20 The less drastically affected children are probably not diagnosed as having the CFC syndrome. As molecular genetic testing is completed on more children, the developmental phenotype may broaden to include children with less severe, or little, developmental delay or mental retardation. When children are serially examined, there is a moderate to marked psychomotor delay in infancy and early childhood, which becomes less obvious with age.5 All cases describe delayed language acquisition. There is one case published of a 25‐year‐old woman with the CFC syndrome without mental retardation. She attended school up to age 19 years, with good results. No specific learning disabilities were reported and she was employed as an administrative assistant.22 Multiple structural brain abnormalities have been reported including cerebral atrophy,23,24,25,26 frontal lobe hypoplasia,1 absence or hypoplasia of the corpus callosum,10 increased ventricular size or hydrocephalus,1,24 non‐specific leucodystrophy of the right frontal region,26 brain stem atrophy,10,27 widening of the cerebral sulci and the basal cisternae,28 and hypoplasia of the cerebellar vermis.10 Hyperactive deep‐tendon reflexes have also been reported.1 Considerable hypotonia leads to marked motor delay. Some children have characteristic recurrent episodes of eyelid fluttering brought on by minimal stimulus.24 Seizures are reported but more often abnormalities can be found on an electroencephalogram, including decreased anterior voltage, spike‐wave or polyspike pattern, sharp and slow waves, generalised dysrhythmia grade I or II, irritative waves, or generalised disorganisation, even when clinically apparent seizures are absent.1,25,26 One child was considered to have Lennox–Gastaux syndrome.29
The face
Children with the CFC syndrome have a relatively large head, a tall forehead with narrowing at the temples, palpebral ptosis and a short nose with a relatively broad nasal base. The philtrum has a deep groove with cupid's bow lip and a small chin. The eyes are wide spaced and the palpebral fissures are often downward slanting, with epicanthic folds (fig 1). These findings are similar to those seen in children with Noonan syndrome, particularly those under 5 or 6 years of age. However, even in this age range, the face tends to be more “coarse” than that seen in case of the Noonan syndrome, and dolichocephaly is more likely to be present. The typical ear shape and placement in the Noonan syndrome, oval with an over‐folded helix, low set and posteriorly angulated, is uncommon in the CFC syndrome. Earlobe creases appear quite frequent. At older ages, the face is broad and coarse, and lacks the inverted triangular shape seen in the Noonan syndrome. Iris colour is rarely the characteristic blue or blue–green as seen in the Noonan syndrome. There is a high likelihood of absent eyebrows with hyperkeratosis (ulerythema ophryogenes). The scalp hair is usually sparse, curly and friable.
Figure 1 Three patients of various ages with the cardiofaciocutaneous syndrome. The face is typical, with a broad forehead, bulbous tip of the nose, low‐set ears, sparse scalp hair and absent eyebrows with ulerythema ophryogenes. The upper panel shows the same child at 10 months (left) and 6 years (right), describing the evolution of the phenotype. All of these children carry a BRAF mutation. Parents of patients gave written consent to publish these images.
Allanson et al30 carried out a detailed examination and measurement of 35 children with the CFC syndrome. Anthropometric assessment showed increased facial widths with facial depths and circumferences closer to normal, a broad nose and mouth, and wide‐spaced eyes. In comparison with the Noonan syndrome, the face is both broader and longer.
Skin and adnexa
Cutaneous or adnexal abnormalities are seen in the CFC syndrome and in the phenotypically similar Noonan and Costello syndromes. Our observation of patients with the CFC and Costello syndromes (about 150), who attended family‐support group conferences for both syndromes, has shown that skin or adnexal abnormalities are present in 100% of people affected. However, the clinical presentation is different and in some cases suggests the diagnosis.
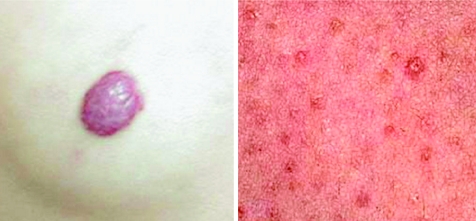
Those with the CFC syndrome present with follicular hyperkeratosis of the arms, legs and face as the most common cutaneous abnormality (table 2; fig 2). Sparse, slow‐growing, curly hair is another hallmark of the CFC syndrome, and is present in 85% of those affected (table 2). On the other hand, patients with the Costello syndrome show palmoplantar hyperkeratosis, skin tags and warts, and nail dystrophy as the most common skin and adnexal anomalies. The presentation of palmoplantar hyperkeratosis also differs from that seen in the CFC syndrome. In people with the Costello syndrome, it is found outside the pressure zones, whereas in those with the CFC syndrome, it is mainly present in the pressure zones.
Table 2 Skin and adnexa findings in people with the cardiofaciocutaneous syndrome.
| Skin | Frequency (%) | Adnexa | Frequency (%) |
|---|---|---|---|
| Keratosis pilaris | 37 | Hair | |
| Ichthyosis | 33 | Sparse | 85 |
| Non‐seborrhoeic eczema | 26 | Curly Fine | 7246 |
| Haemangioma | 24 | Low posterior hairline | 26 |
| Hyperelastic skin | 22 | Light colour | 20 |
| Palmoplantar hyperkeratosis | 13 | Brittle Slow growth | 1817 |
| Seborrhoeic eczema | 9 | Dry | 15 |
| “Café au lait” spots | 9 | Eyebrows | |
| Hyperpigmentation | 5 | Sparse | 43 |
| Keratosis pilaris atrophicans (face) | 5 | AbsentEyelashes | 24 |
| Pigmented naevi | 2 | Sparse | 52 |
| Cutis marmorata | 2 | Absent | 13 |
| Lymphoedema | 2 | Nails | |
| Dystrophy | 15 | ||
| Slow growth | 04 |
Figure 2 Examples of cavernous haemangioma and ulerythema ophryogenes.
Only a few publications have dealt in depth with the cutaneous findings in the CFC syndrome. Histological findings31,32,33 were relatively non‐specific, showing ichthyosis and hyperkeratosis of sweat glands and hair follicles.
Almost two decades of follow‐up of some people with the CFC syndrome has shown that, with age, the dryness of the skin and the follicular hyperkeratosis tend to improve, allowing the hair to grow on the scalp and face. However, palmoplantar hyperkeratosis and lymphoedema may become more severe. Lymphoedema and its complications may have been the cause of death of a teenage boy (personal observation). Therefore, careful follow‐up of patients presenting with lymphoedema and treatment of skin and nail infections is highly recommended.
We have seen no complications related to the pigmented naevi. Periodic evaluation of the pigmented lesions, as well as excision of these lesions in traumatised areas, is recommended, although we have not seen malignant transformations of such lesions.
The heart
Data on cardiac evaluations are available on 53 individuals (published and unpublished) with the CFC syndrome, including three with autopsy (table 3).34,35,36,37,38,39 Cardiac ultrasonography showed no evidence of abnormality in 13 (24.5%) people. The remaining 75.5% had one or more abnormality. Atrial septal defect (ASD), either isolated or associated with pulmonary valve stenosis (PVS), was noted in 9 (22.5%) of those with a cardiac abnormality. Five of these also had mild pulmonary stenosis, two had mild hypertrophic cardiomyopathy and one had severe hypertrophic cardiomyopathy. Surgical repair of the ASD was successful in three patients. One patient required mitral valve replacement because of prolapse with severe insufficiency. Another person underwent closure of an ASD with an Amplatz device. In 13 patients, PVS was the predominant lesion, and in five others it was associated with an ASD. Thus, 18 (45%) had PVS. It was mild or trivial in 15 patients. Two had a surgical pulmonary valvotomy and one had a balloon valvuloplasty. One patient, in addition to PVS, had mitral valve prolapse and another had mild hypertrophic cardiomyopathy. Other cardiac lesions included small ventricular septal defects in two patients and a partial atrioventricular canal in another two patients, one of whom has had successful repair. Another patient had a thickened mitral valve and another mitral valve prolapse. Twelve people had some form of myocardial disease as the primary diagnosis, which was associated with another defect in four others. Thus, 16 (40%) had some form of myocardial disease. Eight had mild hypertrophic cardiomyopathy, two had a localised bulge in the subaortic area and one child had moderate diastolic dysfunction. Two patients were receiving treatment because of major hypertrophic cardiomyopathy with obstruction. Another two patients with severe hypertrophic cardiomyopathy died suddenly at ages 21 and 22 years.
Table 3 Overlapping heart involvement in cardiofaciocutaneous, Noonan and Costello syndromes.
| CFC (this paper) | NS (PTPN11)34,36,37,38,39 | CS35 | |
|---|---|---|---|
| Patients (n) | 53 | 237 | 94 |
| Cardiac abnormality, n (%) | 40 (75.7) | 197 (80) | 60 (63) |
| Type of cardiac abnormality (%) | |||
| Pulmonary valve stenosis | 45 | 71 | 46 |
| Atrial septal defect | 23 | 22 | 7 |
| Hypertrophic cardiomyopathy | 40 | 7 | 44 |
| Other* | 15 | 6 | 8 |
| Cardiac arrhythmias | NA | NA | 30 |
CS, Costello syndrome; NS, Noonan syndrome; NA, figure not available; PTPN11, protein tyrosine phosphatase SHP‐2 gene.
*Other includes ventricular septal defect, ostium primum defect, mitral valve prolapse and aortic stenosis.
Autopsy findings were available in three affected patients. A 4‐year‐old girl died after a brief course of high fever, diarrhoea and a blue, painful right foot. Bacterial endocarditis due to Staphylococcus aureus was documented. Autopsy showed a pulmonary valvectomy carried out at 2 years and an ASD, 8 mm in diameter. All four valves were dysplastic. Extensive vegetations were present on the mitral and aortic valves, with multiple infarcts throughout the body. A 21‐year‐old man died suddenly. A murmur heard in early childhood was attributed to mild PVS. Hypertrophic cardiomyopathy was not recognised until shortly before his death. Autopsy documented biventricular and septal hypertrophy. The pulmonary valve was normal, but the mitral valve was thickened, and the aortic valve was dysplastic with irregular malformed leaflets. Microscopical examination showed the expected focal myofibril disarray, and the intramural coronary arteries showed intimal thickening and early fibrosis, consistent with hypertrophic cardiomyopathy. An unexpected finding was noted in the lungs. The pulmonary artery showed marked intimal thickening, with a narrow lumen consistent with grade 3 pulmonary hypertension. A 22‐year‐old man died shortly after the sudden onset of ventricular fibrillation. A diagnosis of the CFC syndrome had been made in childhood, and an ASD and a PVS had been successfully surgically repaired. At age 20 years, tachycardia and arrhythmia became untreatable problems. At age 22 years, he developed congestive cardiac failure. At autopsy, marked cardiomegaly with microscopic disarray of myocardial fibres, characteristic of hypertrophic cardiomyopathy, was observed.
Cardiac findings in the CFC syndrome are remarkably similar to those noted in the Noonan and Costello syndromes (table 3). Patients with the Noonan syndrome with a PTPN11 mutation have a considerably higher incidence of PVS but a lower incidence of hypertrophic cardiomyopathy.34 Unlike in the Noonan or CFC syndromes, atrial tachycardias or other arrhythmias occur in >30% of patients with the Costello syndrome, particularly in infancy.35,40 The incidence of PVS and hypertrophic cardiomyopathy are similar in CFC and Costello syndromes, whereas Noonan syndrome has a considerably higher incidence of PVS and a much lower incidence of hypertrophic cardiomyopathy. The LEOPARD syndrome, an allelic variant of the Noonan syndrome, has a high incidence of hypertrophic cardiomyopathy.36 The overall incidence of heart disease in the LEOPARD syndrome is 65%, and 80% of those with a cardiac abnormality have hypertrophic cardiomyopathy.41
The congenital defects in all three syndromes can be managed as in any child. However, little is known about the natural history of hypertrophic cardiomyopathy, whose course and prognosis are variable and not well understood. From the experience in the Noonan syndrome and from the limited reports on the CFC and Costello syndromes, marked variability is apparent in the natural history of hypertrophic cardiomyopathy. This condition may be rapidly progressive in infancy42 or may remain stable for many years.43 It may develop late in childhood, and it may resolve, remain stable or progress. Symptomatic hypertrophic cardiomyopathy in infancy is associated with considerable mortality. Although the risk of sudden death in the Noonan syndrome in asymptomatic patients is not well known, sudden unexpected death has been reported.44 The treatment for hypertrophic cardiomyopathy is similar to that in children without the syndrome. Some may improve with high‐dose β blockers.45 Surgical relief of the symptomatic person with obstructive cardiomyopathy may be successful and an occasional patient has undergone cardiac transplantation.
Non‐syndromic hypertrophic cardiomyopathy, often familial, is attributed to mutations in several genes, including the α‐tropomyosin and cardiac troponin T genes.46 It is a heterogeneous disease of sarcomeric proteins and is an important cause of sudden unexpected death in young adults. The myocardial findings in patients with the CFC syndrome and related disorders are similarly characterised by myocardial disarray and thick‐walled intramural coronary arteries.44,47 However, unlike the non‐syndromic form, the right and the left ventricles are often involved.48
In conclusion, our knowledge about the long‐term prognosis of the congenital heart defects in the CFC syndrome is still limited. It is clearly necessary to continue monitoring the cardiovascular system with increasing age. The finding of primary pulmonary hypertension is of interest. This condition has also been reported in several patients with the Noonan syndrome.
Bleeding disorders
Unlike the Noonan syndrome,49 easy bruising and bleeding problems have not been recognised as major problems in the CFC syndrome. Among the patients we have seen, one had transient thrombocytopenia as a newborn and another had frequent nosebleeds that improved with cautery. Easy bruising was not reported by any individual. Haematological data are not available.
The eye
Ocular manifestations are common in the CFC syndrome. Most of them show supraorbital ridge hypoplasia, hypertelorism, downward‐slanting palpebral fissures, ptosis, nystagmus, strabismus or other abnormalities of the eye that require careful management by an ophthalmologist. To date, there is little information in the literature describing the ocular phenotype of this condition. To our knowledge, Young's50 summary of the ocular findings of 12 patients with the CFC syndrome attending the CFC conference in Rockville, Maryland, USA, in 2003, and the report by Young et al51 describing the findings in the eye of 3 children with the CFC syndrome are the only published descriptions of ophthalmic findings in this condition. These results can now be confirmed by the observation of 13 additional individuals. Table 4 summarises the demographic characteristics and ophthalmic findings this group. Of the 13, six were male and seven were female. The ages ranged from birth to 26 years (mean 6.8 (standard deviation 6.6) years).
Table 4 Demographics and data of people with the cardiofaciocutaneous syndrome undergoing an ophthalmological examination.
| Case number, sex | Age at eye exam | Documented CNS symptoms | Strabismus type (PD) | Ocular surgery | Best corrected VA | Refractive error | Astigmatism >1 D | Ocular refraction | Spectacle correction | Amblyopia | Nystagmus | Optic nerve findings | Other |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1, F | 8 years, 4 months | + | RHT; XT | Strabismus surgery (3 years) | 20/60 OU | – | − | – | − | − | + | – | DVD; IOOA; NLDO; Brown syndrome |
| 2, M | 6 years, 6 months | − | 30 XT | Strabismus surgery (at 4 years, 2 months) | 20/160 OU | Myopia | + | OD: −3.00 +0.50 ×12; OS: −2.50 +1.50 ×167 | + | − | + | ON hypoplasia | inferior visual field deficit; decreased contrast sensitivity; light sensititivity |
| 3, F | 3 years, 3 months | + | – | – | 20/90 OU | Mild hyperopia | − | OD: +3.00 +0.50 ×93; OS: +3.50 sphere | + | − | − | – | – |
| 4, F | 4 years, 11 months | − | Accommodative ET | − | – | Mild hyperopia | − | OU: +3.50 sphere | + | + | − | – | – |
| 5, M | 3 years | − | 10 X(T) | − | – | Hyperopia | − | OD: +5.50 sphere; OS: +4.50 sphere | − | + | − | – | – |
| 6, F | 9 years, 11 months | − | XT | − | F&F | Myopia | + | – | − | − | − | ON hypoplasia | – |
| 7, F | 2 years | − | – | − | F&F | – | − | – | − | − | + | – | – |
| 8, M | 6 years, 4 months | + | XT | – | LP | – | − | – | − | − | + | – | Cortical vision loss |
| 9, M | 4 years, 3 months | + | 35 X(T) | – | F&F | Myopia | + | OD: −2.50 +2.00 ×90; OS: −1.50 +2.00 ×90 | + | − | − | ON atrophy | Ptosis bilaterally |
| 10, F | 1 years, 6 months | + | XT | – | F&F | Mild hyperopia | + | – | + | − | − | – | – |
| 11, F | 1 year | − | 10 RHT; 30 XT | – | – | Mild hyperopia | − | OU: +1.25 sphere | − | + | + | Small optic nerves | – |
| 12, M | 12 years, 2 months | − | XT | Strabismus surgery | 20/100 OD; 20/50 OS | Myopia | − | – | − | + | + | ON hypoplasia | Lamellar cataracts bilaterally |
| 13, M | 26 years | + | – | – | 20/400 OU | – | − | – | − | − | + | – | Dense visual opacity; keratoconus |
| Total | 6 (46%) | 10 (77%) | 3 (23%) | 9 (69%) | 4 (31%) | 5 (38%) | 4 (31%) | 7 (54%) | 5 (38%) |
+, present, ‐, absent; CNS, central nervous system; D, dioptres; DVD, dissociated vertical deviation; ET, esotropia; F, female; F&F, fix and follows; IOOA, inferior oblique overaction; LP, light perception; M, male; NLDO, nasolacrimal duct obstruction; OD, right eye; ON, optic nerve; OS, left eye; OU, both eyes; PD, prism diopters; RHT, right hypertropia; VA, visual acuity; XT, exotropia; X(T), intermittent exotropia.
One of the most notable findings in the previous and present studies was the considerable range of visual function among people with the CFC syndrome. Loss of vision to the level of light perception was rare, whereas decrease in visual acuity was more common. Strabismus was also common, affecting about one third of patients. An exotropic deviation was more common than esotropia. A higher percentage of children in the present group had nystagmus (7/13; 54%) than that described by Young et al51 (2/12; 17%). This study also shows a higher prevalence of myopia (4/13; 31%) compared with that in Young's50 summary (1/12; 8%), although only two of four patients with myopia were prescribed spectacle correction.
The only optic nerve finding that occurred in more than one patient was optic nerve hypoplasia. One person had optic atrophy, suggesting a possible increase in intracranial pressure. There were only isolated cases of cataracts, vertical strabismus, dissociated vertical deviation and inferior oblique muscle overaction, nasolacrimal duct obstruction, ptosis and keratoconus. Ocular coloboma, lens dislocation or other structural changes in the eye were not observed. Most children evaluated had difficulty with depth perception and binocular function. Although this may be due to visual‐processing challenges, an overlying strabismus or nystagmus can also contribute to fixation and tracking abnormalities. Studies on a larger number of patients are needed to confirm the ocular phenotype of the CFC syndrome.
In conclusion, it is important that children with the CFC syndrome undergo a comprehensive ophthalmological evaluation as early as possible in the newborn period to assess visual disturbances, including strabismus and refractive error, which may ultimately lead to amblyopia.
Gastrointestinal tract
Feeding problems are seen in the neonatal period, characterised by poor suck, aspiration, gastro‐oesophageal reflux, oral aversion, hyperemesis and gastrointestinal dysmotility. These problems are important enough to often require nasogastric tube feeding, gastrostomy tube placement and/or Nissen fundoplication. Structural abnormalities have also been reported. There have been two cases with malrotation and antral foveolar hyperplasia.21 Antral foveolar hyperplasia is often an acquired abnormality caused by an inflammatory infiltrate, but cultures and stains were negative in the reported case and the cause remains uncertain.21 McDaniel and Fujimoto52 reported a child admitted for inadequate weight gain and frequent postprandial vomiting. Gastrointestinal evaluation showed malrotation of the small intestine, which was surgically corrected. Severe constipation (with normal ganglion cells) requiring disimpaction has also been reported.21 Nanda et al53 reported an unusual case of a 17‐year‐old young woman with the CFC syndrome, with a history of recurrent intermittent abdominal pain and fatty changes in the liver. Liver biopsy showed non‐specific fatty changes (mixed macrovesicular and microvesicular steatosis). Ion et al27 reported one child with Crohn's disease. The case of a toddler with food intolerance, especially to milk, fish and egg, with episodes of asthma, diarrhoea and vomiting was also reported.28 Additional digestive system findings include hepatomegaly, umbilical hernia, inguinal hernia, anal stenosis and intestinal malrotation.52
Molecular aspects
Since the original description in 1986, it has taken 20 years to discover genes whose mutations cause the CFC syndrome and to indisputably establish this condition as a distinct genetic entity, with autosomal dominant heritability. The nosological tangle involving the CFC, Noonan and Costello syndromes was partly solved by the discovery in 2001 of PTPN11 as a gene responsible for a large proportion of patients with the Noonan syndrome.15 Reports soon followed, showing that PTPN11 mutations are not found in those with a firm clinical diagnosis of the CFC syndrome.20,27 Further clarifying evidence was provided by the report in 2005 that the Costello syndrome is caused by HRAS mutations.16 These mutations were also shown not to be involved in the CFC syndrome.54
The final evidence came with the recent discovery that yet other genes cause the CFC syndrome. Rodriguez‐Viciana et al,17 studying 23 individuals with the CFC syndrome, found 11 different mutations of BRAF in 18 of them, mutations of MEK1 in two and of MEK2 in one person. All of these were de novo mis‐sense mutations, suggesting a gain‐of‐function effect. Likewise, Niihori et al,18 studying a non‐overlapping group of 43 patients with the CFC syndrome, found eight different de novo mis‐sense mutations in BRAF in 16 and also de novo mis‐sense mutations in KRAS in three of them. All patients from Niihori et al's18 group testing positive for any one of the reported mutations had a typical CFC phenotype (growth failure, mental retardation, relative macrocephaly, characteristic face, curly and sparse hair, heart defects). On the other hand, not all typical cases of the CFC syndrome have one of the known mutations. Out of 10 bona fide cases described by Kavamura et al,20 only five tested positive for a mutation (Dr Aoki, personal communication, 2006). With respect to genotype–phenotype correlations, Niihori et al18 found that skin abnormalities were present in BRAF‐positive patients, but not in KRAS‐positive ones. No other major differences were noted. By pooling data from the two reports (table 5), there are 13 different BRAF mutations, Q257R being the most common (n = 8).
Table 5 Genes involved in the causation of the cardiofaciocutaneous, Noonan and Costello syndromes.
| Gene | First author, year | CFC syndrome | Noonan syndrome | Costello syndrome |
|---|---|---|---|---|
| BRAF | Niihori,18 2006 | 16/43 | ||
| Rodriguez‐Viciana,17 2006 | 18/23 | |||
| KRAS | Niihori,18 2006 | 3/43 | ||
| Schubbert, 57 2006 | 1/12 | 5/175 | ||
| MEK1 | Rodriguez‐Viciana,17 2006 | 2/23 | ||
| MEK2 | Rodriguez‐Viciana,17 2006 | 1/23 | ||
| HRAS | Aoki,16 2005 | 12/13 | ||
| Kerr,58 2006 | 37/43 | |||
| Estep,54 2006 | 0/8 | 33/36 (20 patients overlap) | ||
| Gripp,59 2006 | 33/40 | |||
| Niihori,18 2006 | 0/43 | |||
| PTPN11 | Ion,27 2002 | 0/28 | ||
| Jongmans,60 2005 | 76/170 | |||
| Kavamura,20 2003 | 0/10 | |||
| Musante,61 2003 | 0/5 | 15/32 | ||
| Tartaglia,15 2001 | 54/119 | |||
| Tartaglia,55 2003 | 0/27 | |||
| Troger,56 2003 | 0/18 | |||
| Zenker,39 2004 | 34/57 |
CFC,cardiofaciocutaneous; MEK, mitogen‐activated protein/extracellular signal‐regulated kinase; PTPN11, protein tyrosine phosphatase SHP‐2 gene.
*Values are genes found in number of patients/total number of patients.
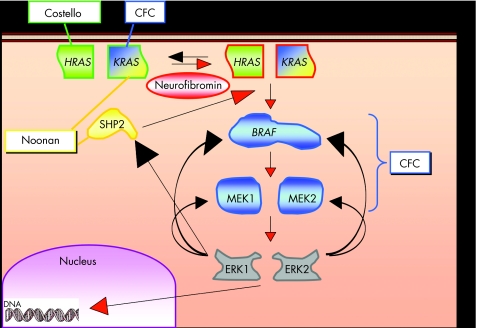
The protein products of the CFC genes and those of HRAS involved in the causation of Costello syndrome,16 and those of PTPN11 in the Noonan syndrome15 (table 5), all have a role in the RAS—extracellular signal‐regulated kinase (ERK) pathway (fig 3). RAS genes encode guanosine triphosphate‐binding proteins that serve as molecular on–off switches that activate or inhibit downstream molecules. It is a signalling pathway that is important for cell proliferation, growth and death. When dysfunctional, it can cause cancer. A major proportion of mutations are gain‐of‐function mutations, as shown by in vitro assays, and stimulate the RAS–ERK pathway. This might explain the increased incidence of solid tumours (rhabdomyosarcoma, ganglioneuroblastoma, bladder carcinoma, etc) in patients with the Costello syndrome and of haematopoietic malignancies in those with the Noonan syndrome.62 Conversely, no increased incidence of tumours has been noted so far in patients with the CFC syndrome. It is not clear whether acute lymphoblastic leukaemia in one patient with a BRAF mutation18 should be considered to be a component manifestation of the syndrome or just a coincidence. However, increased cellular proliferation could explain some of the clinical findings in the CFC syndrome, such as hyperkeratosis and hypertrophic cardiomyopathy. Still, the major effect of all described mutations seems to take place during development, explaining psychomotor retardation and physical anomalies, the common denominator of all three syndromes.
Figure 3 RAS–extracellular signal‐regulated kinase (ERK) signalling pathway connecting pathogenetically the cardiofaciocutaneous (CFC), Costello and Noonan syndromes. Inactive HRAS and KRAS (green outline) are activated (red outline) by neurofibromin and SHP2. Red arrowheads, activation; black arrowheads, inhibition.
Many important details need further clarification through the discovery of additional causative genes. For instance, a good proportion of patients with the Noonan syndrome do not have a PTPN11 mutation and, although a recent report established that KRAS mutations can also cause the Noonan syndrome, mutations were found in only a small proportion of cases. These individuals were described to have more severe features than would be expected in typical Noonan syndrome.57 The complexity of the issue is well considered by Bentires‐Alj et al,63 who dissected the many components of the RAS pathway in relation to the Noonan, CFC, Costello and neurofibromatosis syndromes. At the moment, however, there are more questions than answers in trying to establish why pathogenetically related syndromes display major phenotypic differences.
Yet, we can firmly state that the CFC, Noonan and Costello syndromes are genetically heterogeneous. As they are all caused by mutations in genes whose protein products are part of the RAS–ERK pathway, we also understand, at least partly, why they are phenotypically similar. Further clarification may result from new molecular findings also, but perhaps more likely, and from a more detailed phenotypic description of the various affected patients.
Historical colophon
Virtually every well‐defined condition or syndrome in medical genetics (ever more frequently causally identified) has a classic historical precedent as de Lange had in Brachmann, Étienne‐Louis Arthur Fallot (tetratology) in Niels Stensen and Johann Friedrich Meckel the Younger (the latter fully aware of the resulting defect in oxygenation), Turner (45,X) in Ullrich and George Fraser in the German‐speaking cryptophthalmos pioneers Zehender, Chiari and Fuchs64. The list is endless and the CFC syndrome is no exception.
First published synoptically, after some editorial surgery, upon evaluation of eight patients by Reynolds et al,1 it was preceded by at least one report by Navaratnam and Hodgson,65 who described the entity ulerythema ophryogenes in patients who obviously had what is now known as the CFC syndrome.
In the same year that saw the publication of Reynolds et al,1 Baraitser and Patton66 evidently described the same entity—another one of innumerable recent instances of “when the time is right” discoveries of the same condition or phenomenon, independently in one part of the world or another.
All biological entities have two histories: an ontogeny in a specific individual and a species‐specific phylogeny involving a group of individuals. Again, the CFC syndrome is no exception. The ontogeny of the condition is encapsulated in the eight clinical reports by Reynolds et al1; however, that publication had a phylogeny spanning almost two decades.
The first child with the CFC syndrome studied by JMO was SVH (patient 3 in Reynolds et al1), born on 20 July 1968 and ascertained on 9 December 1968 at the former Wisconsin Orthopedic Hospital for Children of the University of Wisconsin, Wisconsin, Madison, USA after a visit to the cardiology clinic for probable pulmonic stenosis and atrial septal defect. He was followed up for some years, also studied by FR Grosse and Gerhard Neuhäuser, and then lost to follow‐up. An effort has been initiated to determine his subsequent fate.
The second child from Wisconsin was KAS, patient 2 in Reynolds et al,1 born on 11 March 1969 and ascertained on 28 July 1969. She was one of two of the original three children with the CFC syndrome with a cavernous hemangioma. She had a heart failure presumably due to an endocardial cushion defect. Her present condition is unknown. Patient 1 in Reynolds et al1 was the third of the children with the CFC syndrome from Wisconsin, born on 5 July 1967 and ascertained on 19 April 1971, also with a hemangioma. An attempt to interest former Wisconsin coworkers in a collaborative publication at that time was unsuccessful.
About 10 years after the Wisconsin group began collaborating with Dr Philip D Pallister in Montana, we studied KL (patient 6 in Reynolds et al,1 born on 2 September 1974 and first seen by Dr Pallister on 17 December 1976). In west America, especially Montana, families tend to “stay put”; thus, it was no surprise that this young woman's mother called promptly at 08:00 on 1 March 2006 from her original phone of 30 years ago, delighted at the news that no less than four genes had been identified as the cause of the CFC syndrome and to tell us that her daughter was in stable condition, doing well at age 31 years. She had graduated from high school in special education and was now living, self‐sufficiently in an apartment space of her own in the family's original home with her sister, brother‐in‐law and five children. She is able to use her microwave oven, walk up and down stairs, used a lotion for her “rough” skin and glasses for her visual defect—which had remained stable since the first evaluation. She greatly enjoys television and the love and company of her family and considers herself perfectly normal. An incipient menstrual hygiene problem had been solved through a partial hysterectomy; however, her breast hypertrophy still awaits surgical action. Results of her DNA study will be communicated in due time.
Patient 8 of the original report (ARA, born on 23 April 1976) was a patient of Dr James G Coldwell of Tulsa, Oklahoma, USA, where the boy was evaluated in November 1983, as reported in Reynolds et al.1 In 1999, Dr Coldwell informed us that the young man had developed severe, poorly controlled congestive heart failure at age 18 years, followed by a supraventricular tachycardia at 20 years. This “converted poorly” and was interpreted as an ectopic atrial tachycardia with a “tachycardia‐induced cardiomyopathy”. There was successful radio frequency ablation of one atrial ectopic site but inability to ablate the second ectopic site, and poor adherence to the medical regimen was probably the cause of death at 22 years. The report of the medical examiner was instructive. He (the patient) was described as a short man with an extremely short neck and short and stubby toes and fingers. A marked cardiomegaly (1080 g) was observed, with the right and left ventricles and septum measuring 1.5, 3.0 and 2.0 cm in thickness, respectively. Brain weight was 1750 g. Sections of the heart showed considerable fibre disarray. Before death, he had been found unresponsive by a relative and at a local hospital discovered to have ventricular fibrillation unresponsive to resuscitation. Histological sections transmitted to us were so broken that they did not enable further histological analysis.
JP, patient 5 in Reynolds et al,1 is now 30 years old, living in a group home and visiting with parents every weekend. Despite being considered “profoundly” mentally retarded, she is reportedly happy and social. She recently came close to death due to pneumonia and intestinal obstruction.
Had an earlier publication been possible (say in 1972), the CFC syndrome would accordingly have been designated the VHSZ syndrome, much to the annoyance of Victor McKusick. As it turned out, it was not until the opportunity of the 1986 David Smith meeting in Vermont presented itself that Reynolds et al1 finally completed their manuscript, initially including 10 patients. In a thoughtful analysis, one reviewer concluded “that the CFC syndrome is [not] a unique genetic MCA/MR [multiple congenital abnormality/mental retardation] syndrome”, perhaps a form or subgroup of the Noonan syndrome, and a second reported that “the cases are too diverse to be sold as a single entity”. Owing to the conflict of interest, we asked Dr John C Carey to edit the manuscript; he had the good sense to recommend deletion of cases 8 and 10 of the original manuscript (who, in retrospect, clearly did not have the CFC syndrome), leaving it with the eight, now clearly bona fide children with the CFC syndrome. Thus, the “heterogeneity” alluded to above actually refers to the phenomenon of variability (a phenotypic attribute); the heterogeneity (a causal attribute) of the CFC syndrome did not become evident until the recent work by Rodriguez‐Viciana et al17 and Niihori et al.18 The Salt Lake City CFC files include about 78 affected children (and a few adults); many of these are probably not members of the CFC Support Group. Much work remains to be carried out on the CFC syndrome and related conditions.
Acknowledgements
We acknowledge the help and continued support of Brenda Conger, President of CFC International, and the families with members with the CFC syndrome who participated in the studies that form the basis of this review.
Abbreviations
ASD - atrial septal defect
CFC - cardiofaciocutaneous
ERK - extracellular signal‐regulated kinase
PTPN11 - protein‐tyrosine phosphatase nonreceptor type II encoding Tyrosine Phosphate SHP2
PVS - pulmonary valve stenosis
Footnotes
Competing interests: None declared.
References
- 1.Reynolds J F, Neri G, Herrmann J P, Blumberg B, Coldwell J G, Miles P V, Opitz J M. New multiple congenital anomalies/mental retardation syndrome with cardio‐facio‐cutaneous involvement—the CFC syndrome. Am J Med Genet 198628413–427. [DOI] [PubMed] [Google Scholar]
- 2.Weiss G, Confino Y, Shemer A, Trau H. Cutaneous manifestations in the cardiofaciocutaneous syndrome, a variant of the classical Noonan syndrome. Report of a case and review of the literature. J Eur Acad Derm Vener 200418324–327. [DOI] [PubMed] [Google Scholar]
- 3.Fryer A E, Holt P J, Hughes H E. The cardio‐facio‐cutaneous syndrome and Noonan syndrome: are they the same? Am J Med Genet 199138548–551. [DOI] [PubMed] [Google Scholar]
- 4.Neri G, Zollino M, Reynolds J F. The Noonan‐CFC controversy. Am J Med Genet 199139367–370. [DOI] [PubMed] [Google Scholar]
- 5.Ward K A, Moss C, McKeown C. The cardio‐facio‐cutaneous syndrome: a manifestation of the Noonan syndrome? Br J Dermatol 1994131270–274. [DOI] [PubMed] [Google Scholar]
- 6.Leichtman L G. Are cardio‐facio‐cutaneous syndrome and Noonan syndrome distinct? A case of CFC offspring of a mother with Noonan syndrome. Clin Dysmorph 1996561–64. [DOI] [PubMed] [Google Scholar]
- 7.Lorenzetti M E, Fryns J ‐ P. Retinitis pigmentosa in a young man with Noonan syndrome: further evidence that Noonan syndrome (NS) and the cardio‐facio‐cutaneous syndrome (CFC) are variable manifestations of the same entity? Am J Med Genet 19966597–99. [DOI] [PubMed] [Google Scholar]
- 8.Neri G, Zollino M. More on the Noonan‐CFC controversy. Am J Med Genet 199665100. [DOI] [PubMed] [Google Scholar]
- 9.Legius E, Schollen E, Matthijs G, Fryns J P. Fine mapping of Noonan/cardio‐facio cutaneous syndrome in a large family. Eur J Hum Genet 1998632–37. [DOI] [PubMed] [Google Scholar]
- 10.Wieczorek D, Majewski F, Gillessen‐Kaesbach G. Cardio‐facio‐cutaneous (CFC) syndrome—a distinct entity? Report of three patients demonstrating the diagnostic difficulties in delineation of CFC syndrome. Clin Genet 19975237–46. [DOI] [PubMed] [Google Scholar]
- 11.Tartaglia M, Gelb B D. Noonan syndrome and related disorders: genetics and pathogenesis. Annu Rev Genom Hum Genet 2005645–68. [DOI] [PubMed] [Google Scholar]
- 12.Johnson J B, Golabi M, Norton M E, Rosenblatt R M, Feldman G M, Yang S P, Hall B D, Fries M H, Carey J. Costello syndrome: phenotype, natural history, differential diagnosis, and possible cause. J Pediatr 1998133441–448. [DOI] [PubMed] [Google Scholar]
- 13.van Eeghen A M, van Gelderen I, Hennekam R C M. Costello syndrome: report and review. Am J Med Genet 199982187–193. [DOI] [PubMed] [Google Scholar]
- 14.Kavamura M I, Peres C A, Alchorne M M, Brunoni D. CFC index for the diagnosis of cardiofaciocutaneous syndrome. Am J Med Genet 200211212–16. [DOI] [PubMed] [Google Scholar]
- 15.Tartaglia M, Mehler E L, Goldberg R, Zampino G, Brunner H G, Kremer H, van der Burgt I, Crosby A H, Ion A, Jeffery S, Kalidas K, Patton M A, Kucherlapati R S, Gelb B D. Mutations in PTPN11, encoding the protein tyrosine phosphatase SHP‐2, cause Noonan syndrome. Nat Genet 200129465–468. [DOI] [PubMed] [Google Scholar]
- 16.Aoki Y, Niihori T, Kawame H, Kurosawa K, Ohashi G, Tanaka Y, Filocamo M, Kato K, Suzuki Y, Kure S, Matsubara Y. Germline mutations in HRAS proto‐oncogene cause Costello syndrome. Nat Genet 2005371038–1040. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez‐Viciana P, Tetsu O, Tidyman W E, Estep A L, Conger B A, Santa Cruz M, McCormick F, Rauen K A. Germline mutations in genes within the MAPK pathway cause cardio‐facio‐cutaneous syndrome. Science 20063111287–1290. [DOI] [PubMed] [Google Scholar]
- 18.Niihori T, Aoki Y, Narumi Y, Neri G, Cave H, Verloes A, Okamoto N, Hennekam R C M, G Gillessen‐Kaesbach . Wieczorek D, Kavamura M I, Kurosawa K, Ohashi H, Wilson L, Heron D, Bonneau D, Corona G, Kaname T, Naritomi K, Baumann C, Matsumoto N, Kato K, Kure S, Matsubara Y. Germline KRAS and BRAF mutations in cardio‐facio‐cutaneous syndrome. Nat Genet 200638294–296. [DOI] [PubMed] [Google Scholar]
- 19.Somer M, Peippo M, Aalto‐Korte K, Ritvanen A, Niemi K M. Cardio‐facio‐cutaneous syndrome: three additional cases and review of the literature. Am J Med Genet 199244691–695. [DOI] [PubMed] [Google Scholar]
- 20.Kavamura M I, Pomponi M G, Zollino M, Lecce R, Murdolo M, Brunoni D, Alchorne M M, Opitz J M, Neri G. PTPN11 mutations are not responsible for the cardiofaciocutaneous syndrome. Eur J Hum Genet 20031164–68. [DOI] [PubMed] [Google Scholar]
- 21.Herman T E, McAlister W H. Gastrointestinal and renal abnormalities in cardio‐facio‐cutaneous syndrome. Pediatr Radiol 200535202–205. [DOI] [PubMed] [Google Scholar]
- 22.Manoukian S, Lalatta F, Selicorni A, Tadini G, Cavalli R, Neri G. Cardio‐facio‐cutaneous (CFC) syndrome: report of an adult without mental retardation. Am J Med Genet 199663382–385. [DOI] [PubMed] [Google Scholar]
- 23.Drolet B A, Baselga E, Esterly N B. What syndrome is this? Pediatr Dermatol 200017231–234. [DOI] [PubMed] [Google Scholar]
- 24.Grebe T A, Clericuzio C. Neurological and gastrointestinal dysfunction in cardio‐facio‐cutaneous syndrome: identification of a severe phenotype. Am J Med Genet 200095135–143. [PubMed] [Google Scholar]
- 25.Raymond G, Holmes L B. Cardio‐facio‐cutaneous (CFC) syndrome: neurological features in two children. Dev Med Child Neurol 199335727–741. [DOI] [PubMed] [Google Scholar]
- 26.Sabatino G, Verrotti A, Domizio S, Angelozzi B, Chiarelli F, Neri G. The cardio‐facio‐cutaneous syndrome: a long‐term follow‐up of two patients, with special reference to the neurological features. Child Nerv Syst 199713238–241. [DOI] [PubMed] [Google Scholar]
- 27.Ion A, Tartaglia M, Song X, Kalidas K, van der Burgt I, Shaw A C, Ming J E, Zampino G, Zackai E H, Dean J C, Somer M, Parenti G, Crosby A H, Patton M A, Gelb B D, Jeffery S. Absence of PTPN11 mutations in 28 cases of cardiofaciocutaneous (CFC) syndrome. Hum Genet 2002111421–427. [DOI] [PubMed] [Google Scholar]
- 28.Neri G, Sabatino G, Bertini E, Genuardi M. Brief clinical report: the CFC syndrome—report of the first two cases outside of the United States. Am J Med Genet 198727767–771. [DOI] [PubMed] [Google Scholar]
- 29.Gross‐Tsur V, Gross‐Kieselstein E, Amir N. Cardio‐facio‐cutaneous syndrome: neurological manifestations. Clin Genet 199038382–386. [DOI] [PubMed] [Google Scholar]
- 30.Allanson J, Opitz J M, Carey J C, Viskochil D, Noonan J, Kavamura M I, Neri G. Cardio‐facio‐cutaneous syndrome: a distinct entity. Proc Greenwood Genet Ctr 20022167 [Google Scholar]
- 31.Verloes A, Le Merrer M, Soyeur D, Kaplan J, Pangalos C, Rigo J, Briard M L. CFC syndrome: a syndrome distinct from Noonan syndrome. Ann Genet 198831230–234. [PubMed] [Google Scholar]
- 32.Pierard G E, Soyeur‐Broux M, Estrada J A, Pierard‐Franchimont C, Soyeur D, Verloes A. Cutaneous presentation of the cardio‐facio‐cutaneous syndrome. J Am Acad Dermatol 199022920–922. [DOI] [PubMed] [Google Scholar]
- 33.Borradori L, Blanchet‐Bardon C. Skin manifestations of the cardio‐facio‐cutaneous syndrome. J Am Acad Dermatol 199328815–819. [DOI] [PubMed] [Google Scholar]
- 34.Tartaglia M, Kalidas K, Shaw A, Song X, Musat D L, van der Burgt I, Brunner H G, Bertola D R, Crosby A, Ion A, Kucherlapati R K, Jeffery S, Patton M A, Gelb B D. PTPN11 mutations in Noonan syndrome: molecular spectrum, genotype‐phenotype correlation, and phenotypic heterogeneity. Am J Hum Genet 2002701555–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin A E, Grossfeld P D, Hamilton R M, Smoot L, Gripp K W, Proud V, Weksberg R, Wheeler P, Picker J, Irons M, Zackai E, Marino B, Scott C I, Nicholson L. Further delineation of cardiac abnormalities in Costello syndrome. Am J Med Genet 2002111115–129. [DOI] [PubMed] [Google Scholar]
- 36.Sarkozy A, Conti E, Deripa D, Digilio M C, Grifone M, Tandoi C, Fazio V M, Di Ciommo V, Marino B, Pizzuti A, Dallapiccola B. Correlation between PTPN11 gene mutations and congenital heart defects in Noonan and LEOPARD syndromes. J Med Genet 200340704–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bertola D R, Kim C A, Sugayama S M, Albano L M, Wagenfuhr J, Moyses R L, Gonzalez C H. Cardiac findings in 31 patients with Noonan's syndrome. Arq Bras Cardiol 200075409–412. [DOI] [PubMed] [Google Scholar]
- 38.Marino B, Digilio M C, Toscano A, Gianotti A, Dallapiccola B. Congenital heart disease in children with Noonan syndrome: an expanded cardiac spectrum with high prevalence of atrioventricular canal. J Pediatr 1999135703–706. [DOI] [PubMed] [Google Scholar]
- 39.Zenker M, Buheitel G, Rauch R, Koenig R, Bosse K, Kress W, Tietze H U, Doerr H G, Hofbeck M, Singer H, Reis A, Rauch A. Genotype‐phenotype correlations in Noonan syndrome. J Pediatr 2004144368–374. [DOI] [PubMed] [Google Scholar]
- 40.Siwik E, Zahka K, Wiesner G. Cardiac disease in Costello syndrome. Pediatrics 1998101706–709. [DOI] [PubMed] [Google Scholar]
- 41.Sarkozy A, Conti E, Digilio M C, Marino B, Morini E, Pacileo G, Wilson M, Calabro R, Pizzuti A, Dallapiccola B. Clinical and molecular analysis of 30 patients with multiple lentigines LEOPARD syndrome. J Med Genet 200441e68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Takahashi K, Kogaki S, Kuvotobi S, Nasuno S, Ohta M, Okabe H, Wada K, Sakai N, Taniike M, Ozono K. A novel mutation in the PTPN11 gene in a patient with Noonan syndrome and rapidly progressive cardiomyopathy. Eur J Pediatr 2005165497–500. [DOI] [PubMed] [Google Scholar]
- 43.Noonan J. Noonan syndrome and related disorders. Prog Pediatr Cardiol 200520177–185. [Google Scholar]
- 44.Noonan J A, O'Connor W. Noonan syndrome: a clinical description emphasizing the cardiac findings. Acta Paediatr Jpn 19963876–83. [DOI] [PubMed] [Google Scholar]
- 45.Ostman‐Smith I, Wettrell G, Riesenfeld T A. A cohort study of childhood hypertrophic cardiomyopathy. J Am Coll Cardiol 1999341813–1822. [DOI] [PubMed] [Google Scholar]
- 46.Theirfelder L, Watkins H, MacRae C, Lamar R, McKenna W, Vosberg H ‐ P, Seidman J, Seidman C. A tropomyosin and cardiac troponin T mutations cause familial hypertrophic cardiomyopathy: a disease of the sarcomere. Cell 199477701–712. [DOI] [PubMed] [Google Scholar]
- 47.Burch M, Mann J M, Sharland M, Shinebourne E A, Patton M A, McKenna W J. Myocardial disarray in Noonan syndrome. Br Heart J 199268586–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Skinker D M, Cottrill C M, O'Connor W N. Right ventricular biopsy findings of hypertrophic cardiomyopathy in a patient with Noonan syndrome. Cardiol Young 19988256–259. [Google Scholar]
- 49.Sharland M, Patton M A, Talbot S, Chitolie A, Bevan D H. Coagulation‐factor deficiencies and abnormal bleeding in Noonan syndrome. Lancet 199233919–21. [DOI] [PubMed] [Google Scholar]
- 50.Young T L. Cardio‐facio‐cutaneous syndrome conference ophthalmic findings summary, Rockville Maryland—June 2003. http://www.cfcsyndrome.org/conference‐summary.htm
- 51.Young T L, Ziylan S, Schaffer D B. The ophthalmologic manifestations of the cardio‐facio‐cutaneous syndrome. J Pediatr Ophthalmol Strabismus 19933048–52. [DOI] [PubMed] [Google Scholar]
- 52.McDaniel C H, Fujimoto A. Intestinal malrotation in a child with cardio‐facio‐cutaneous syndrome. Am J Med Genet 199770284–286. [DOI] [PubMed] [Google Scholar]
- 53.Nanda S, Rajpal M, Reddy B S N. Cardio‐facio‐cutaneous syndrome: report of a case with a review of thje literature. Int Soc Dermatol 200443447–450. [DOI] [PubMed] [Google Scholar]
- 54.Estep A L, Tidyman W E, Teitell M A, Cotter P D, Rauen K A. HRAS mutations in Costello syndrome: detection of constitutional activating mutations in codon 12 and 13 and loss of wild‐type allele in malignancy. Am J Med Genet A 20061408–16. [DOI] [PubMed] [Google Scholar]
- 55.Tartaglia M, Cotter P D, Zampino G, Gelb B D, Rauen K A. Exclusion of PTPN11 mutations in Costello syndrome: further evidence for distinct genetic etiologies for Noonan, cardio‐facio‐cutaneous and Costello syndromes. Clin Genet 200363423–426. [DOI] [PubMed] [Google Scholar]
- 56.Troger B, Kutsche K, Bolz H, Luttgen S, Gal A, Almassy Z, Caliebe A, Freisinger P, Hobbiebrunken E, Morlot M, Stefanova M, Streubel B, Wieczorek D, Meinecke P. Exclusion of PTPN11 mutations in Costello syndrome: further evidence for distinct genetic etiologies for Noonan, cardio‐facio‐cutaneous and Costello syndromes. Am J Med Genet A 200312182–84. [DOI] [PubMed] [Google Scholar]
- 57.Schubbert S, Zenker M, Rowe S L, Boll S, Klein C, Bollag G, can der Burgt I, Musante L, Kalscheuer V, Wehner L K, Nguyen H, West B, Zhang K Y J, Sistermans E, Rauch A, Niemeyer C M, Shannon K, Kratz C P. Germline KRAS mutations cause Noonan syndrome. Nat Genet 200638331–336. [DOI] [PubMed] [Google Scholar]
- 58.Kerr B, Delrue M A, Sigaudy S, Perveen R, Marche M, Burgelin I, Stef M, Tang B, Eden T, O'Sullivan J, De Sandre‐Giovannoli A, Reardon W, Brewer C, Bennett C, Quarrell O, McCann E, Donnai D, Stewart F, Henekam R, Cave H, Verlos A, Philip N, Lacombe D, Levy N, Arveiler B, Black G. Genotype‐phenotype correlation in Costello syndrome; HRAS mutation analysis in 43 cases. J Med Genet 2006 [DOI] [PMC free article] [PubMed]
- 59.Gripp K W, Lin A E, Stabley D L, Nicholson L, Scott C I, Doyle D, Aoki A, Matsubara Y, Zackai E H, Lapunzina P, Gonzalez‐Meneses A, Holbrook J, Agresta C A, Gonzalez I L, Sol‐Church K. HRAS mutation analysis in Costello syndrome. Am J Med Genet A 20061401–7. [DOI] [PubMed] [Google Scholar]
- 60.Jongmans M, Sistermans E A, Rikken A, Nillsen W M, Tamminga R, Patton M, Maier E M, Tartaglia M, Noordam K, van der Burgt I. Genotypic and phenotypic characterization of Noonan syndrome: new data and review of the literature. Am J Med Genet A 2005134165–170. [DOI] [PubMed] [Google Scholar]
- 61.Musante L, Kehl H G, Majewski F, Meinecke P, Schweiger S, Gillesen‐Kaesbach G, Wieczorek D, Hinkel G K, Tinschert S, Hoeltzenbein M, Ropers H H, Kalscheuer V M. Spectrum of mutations in PTPN11 and genotype‐phenotype correlation in 96 patients with Noonan syndrome and five patients with cardio‐facio‐cutaneous syndrome. Eur J Hum Genet 200211201–206. [DOI] [PubMed] [Google Scholar]
- 62.Tartaglia M, Niemeyer, Fragale A, Song X, Buechner J, Jung A, Hahlen K, Hasle H, Licht J D, Gelb B D. Somatic mutations in PTPN11 in juvenile myelomonocytoc leukaemia, myelodysplastic syndromes and acute myeloid leukaemia. Nat Genet 200334148–150. [DOI] [PubMed] [Google Scholar]
- 63.Bentires‐Alj M, Konmtaridis M I, Neel B G. Stops along the RAS pathway in human genetic disease. Nat Med 200612283–285. [DOI] [PubMed] [Google Scholar]
- 64.Comstock J M, Putnam A R, Opitz J M, Pysher T J, Szakacs J. Prenatal death in Fraser syndrome. Fetal Pediatr Pathol 200524223–238. [DOI] [PubMed] [Google Scholar]
- 65.Navaratnam A E D, Hodgson G A. Ulerythema ophryogenes with mental retardation. Proc R Soc Med 107366233–234. [PMC free article] [PubMed] [Google Scholar]
- 66.Baraitser M, Patton M A. A Noonan‐like short stature syndrome with sparse hair. J Med Genet 198623161–164. [DOI] [PMC free article] [PubMed] [Google Scholar]