Abstract
Whereas the treatment outcome research literature for adolescent alcohol and other drug abuse has shown recent advances (R. J. Williams, S. Y. Chang, & Addiction Centre Adolescent Research Group, 2000), significant knowledge gaps remain. A. E. Kazdin (2001) recently observed that one of the key questions for the field is to identify if client characteristics meaningfully mediate or moderate treatment outcome. There is support from the adolescent clinical literature that internalizing and externalizing personality subtypes are related to the onset and course of youth substance use disorders (D. B. Clark & O. G. Bukstein, 1998). The study extends this literature by examining the association of drug use behaviors outcome and subtyped adolescents (internalizers and externalizers; n = 141) who sought treatment at a 12-Step program. The analysis also includes a community-based control group (n = 94). Specifically, we examined the association of subtype and treatment retention and short-term (Year 1) and long-term (Year 4 and Year 5.5) drug involvement outcomes. Externalizers consistently showed poorer outcomes, including poorer treatment retention and greater drug use and drug disorder symptoms at each follow-up point. The treatment implications of the study are discussed.
Keywords: Adolescent drug abuse, Personality traits, Long-term outcome
1. Introduction
Relative to the adult addictions literature, there is a paucity of research examining adolescent drug abuse treatment outcome (Williams, Chang, & Addiction Centre Adolescent Research Group, 2000). The significance of this gap in the addictions literature is highlighted by recent studies suggesting that 7% to 17% of school-based youth require treatment for psychoactive substance use disorders (SUDs; Harrison, Fulkerson, & Beebe, 1998; Hartwell, Ungemack, & Babor, 1996). Studies suggest that a range of treatment approaches, including 12-Step, cognitive–behavioral, and family-based interventions, work for drug-abusing youth (Kaminer, Burleson, Blitz, Sussman, & Rounsaville, 1998; Latimer, Newcomb, Winters, & Stinchfield, 2000; Surgeon General, 1988; Winters, Latimer, & Stinchfield, 1999). However, sample size limitations characterizing extant studies have generally precluded a thorough examination of factors that explain why treatments work for some but not for others (Catalano, Hawkins, Wells, & Miller, 1991; Winters, 1999).
Kazdin (2001) recently outlined a series of key questions that need to be addressed for the adolescent addictions field to expand beyond its current boundaries. Several questions center around an elucidation of client characteristics that mediate or moderate treatment outcomes for drug-abusing youth. Out of the many possible client characteristics that might be examined as outcome predictors, a focus on psychiatric symptoms or comorbidity issues is supported on empirical and clinical grounds. Firstly, although studies examining relationships between comorbidity patterns and outcome are few, there is a fairly broad base of research documenting high rates of both internalizing (e.g., anxiety and mood disorders) and externalizing (e.g., attention deficit, oppositional defiant, and conduct disorders) disorders among drug-abusing youth (Clark et al., 1995; DeMilio, 1989; Horner & Scheibe, 1997). Secondly, in the event that treatment outcomes are found to vary as a function of psychiatric symptoms or comorbidity patterns among drug-abusing youth, such information could be used by treatment intake workers to inform decisions regarding treatment modality, length, and intensity (Clark & Bukstein, 1998; Clark & Neighbors, 1996).
Not surprisingly, most comorbidity studies of drug-abusing youth in treatment have used categorical measures of psychiatric status given the range of treatment and reimbursement decisions made based on the presence or absence of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)-defined disorders. Generally, these studies suggest that comorbidity patterns affect treatment outcomes. For example, one study with 60 adolescents in residential drug abuse treatment found that a comorbid diagnosis of attention deficit/hyperactivity disorder (ADHD) was associated with shorter length of stay (Adams & Wallace, 1994). Moss, Kirisci, and Mezzich (1994) examined the impact of single and comorbid disorders, including drug use and ADHD, on levels of confidence to resist heavy alcohol drinking in specific situations among 239 youth from drug abuse treatment and community programs. Adolescents with ADHD were significantly less confident than control youth to resist heavy drinking when exposed to physical discomfort, social tension, or emotional states.
A separate study found that probable ADHD status among adolescents in drug treatment resulted in elevated rates of alcohol relapse at 6 months follow-up (Latimer, Ernst, Hennessey, Stinchfield, & Winters, 2004). In the same study, conduct disturbance, not probable ADHD status, was found to predispose youth to relapse on drugs other than alcohol or marijuana during the same follow-up period. Similarly, conduct disorder and preadolescent conduct disturbance have been associated with elevated adolescent drug use following treatment (Mott, Myers, Tammariello, & Brown, 1992; Myers, Brown, & Mott, 1995). Grella, Hser, Joshi, and Rounds-Bryant (2001) found that drug-abusing youth with psychiatric comorbidity exhibited higher rates of problem behavior, marijuana use, and hallucinogen use at 12 months posttreatment when compared with control youth.
Randall, Henggeler, Pickrel, and Brondino (1999) examined the influences of psychiatric comorbidity on outcomes of drug-abusing juvenile offenders. Juvenile offenders with externalizing disorders exhibited higher rates of antisocial behavior at 16 months follow-up when compared with juvenile offenders with either drug abuse alone or with comorbid internalizing disorders. Furthermore, the presence of internalizing disorders protected against criminal activity and drug use at follow-up among a subgroup of juvenile offenders who also exhibited drug abuse and externalizing disorders.
Although most drug abuse comorbidity studies have focused on categorical predictor variables, continuous variables capturing dimensions that distinguish between classes of disorders (e.g., internalizing vs. externalizing disorders) have been shown to provide critical information as outcome predictors that are not captured by the categorical disorders they underlie (Fergusson, Horwood, & Jensen, 1995). One study examined patterns of internalizing and externalizing symptoms among 236 drug-abusing adolescents (Rowe, Liddle, & Dakof, 2001). The three subgroups of drug-abusing youth that emerged were labeled exclusive drug abusers, externalizing drug abusers, and mixed internalizing–externalizing drug abusers. Notably, an internalizing drug abuser group did not characterize the sample. Overall, adolescent drug abusers characterized by either the externalizing or mixed symptom profiles exhibited elevated pretreatment levels of individual and familial psychopathology when compared with the exclusive drug abuse subgroup.
Similar studies have also focused on the degree to which pretreatment client characteristics along psychiatric dimensions predict treatment outcome. For example, the Pittsburgh group classified adolescents with alcohol use disorders into subgroups based on an internalizing–externalizing behavior dimension (Mezzich et al., 1993). Adolescent alcohol abusers characterized primarily by negative affect exhibited more severe problem behaviors related to drug use yet lower rates of anxiety disorders than did alcohol abusers characterized by behavioral dyscontrol and hypophoria. Crowley, Mikulich, Macdonald, Young, and Zerbe (1998) examined treatment outcomes among drug-abusing male adolescents diagnosed with comorbid attention deficit/hyperactivity, conduct, and mood disorders. The study found that continuous measures of conduct disorder severity and drug involvement at intake predicted worse outcomes across a 2-year follow-up period. Another study of adolescents in drug treatment revealed that heightened externalizing problems, indicated by continuous measures of aggression, alienation, and social maladaptation, were associated with treatment noncompletion (Dobkin, Chabot, Maliantovitch, & Craig, 1998). Among treatment completers, internalizing symptoms on continuous measures for anxiety and depression were associated with worse follow-up outcomes, although this association between internalizing symptoms among completers has not always held up (Whitmore, Mikulich, Ehlers, & Crowley, 2000).
A current gap in the adolescent addictions literature is that there is an insufficient understanding of relationships between posttreatment outcomes and psychiatric problems that are common among adolescent drug abusers. General treatment outcome findings, although useful, can be more informed if client characteristics have a meaningful and reliable relationship with outcome.
This study extends our prior work that described short-and long-term outcome among adolescents with a substance dependence disorder and who received 12-Step treatment (Winters, Stinchfield, Opland, Weller, & Latimer, 2000; Winters, Stinchfield, Latimer, & Lee, 2007). The present analysis will extend our outcome descriptive studies by examining the relationship between internalizing and externalizing symptoms among this group of substance-dependent adolescents. Specifically, we describe the association of treatment outcome (treatment completion and posttreatment drug use behaviors at Year 1, Year 4, and Year 5.5) as a function of subtyped adolescents (internalizers and externalizers; n = 141) who sought treatment at a 12-Step program. A community, non-drug-abusing sample (control group; n = 94) is included in the long-term outcome analysis. Based on the extant literature, we hypothesize the following predictions: (a) internalizers will show a higher rate of treatment completion compared to the externalizers, (b) internalizers will reveal less drug involvement at the follow-up periods compared with externalizers, and (c) both internalizers and externalizers will reveal elevated posttreatment drug involvement compared with the control group.
2. Method
2.1. Participants
A summary of participant characteristics for the two treatment groups (defined below; externalizers, n = 76; internalizers, n = 65) and the control (n = 94) group is provided in Table 1.
Table 1.
Participant characteristics at intake as a function of the two study groups
| Variable | Externalizers | Internalizers | Controls |
|---|---|---|---|
| n | 76 | 65 | 94 |
| % male | 75 | 44 | 59 |
| % White a | 86 | 88 | 83 |
| Mean age a | 15.7 | 15.8 | 16.1 |
| Socioeconomic status a, b | 48 | 49 | 50 |
| % previous drug treatment | 25 | 26 | <1 |
| % at least one dependence diagnosis | 100 | 100 | 0 |
| % 2+ dependence diagnosis | 84 | 79 | 0 |
| % past year, monthly substance use | 100 | 100 | 19 |
The three groups do not differ on these variables.
Socioeconomic status based on Hollingshead et al. (1975); range = 17–66; higher scores are better.
2.1.1. Treatment
Consecutive admissions at an adolescent 12-Step, Minnesota model-based program were approached during an 8-month period during treatment intake to determine interest in participating in the study. Inclusion criteria included the following: the adolescent and his or her family lived in the seven-county metropolitan area, the adolescent was 12 to 18 years old, and the adolescent showed these clinical characteristics (which were determined by research staff): met DSM-IV criteria for at least one current psychoactive substance dependence disorder and showed no evidence of acute psychotic disorder, developmental disability, acute intoxication, and withdrawal symptoms. One hundred seventy-nine admissions initially agreed to participate (71% of those eligible). The mean number of substance dependence diagnosis was 2.4, with alcohol and cannabis dependence being the most common (72% and 86%, respectively), and all reported at least monthly use of at least one drug during the prior year.
Participants in the treatment group differed as to whether treatment was completed or not. Treatment completers (n = 124; 78%) received the full course of primary drug treatment, defined by an approved discharge by the client’s primary physician. All treatment completers participated in therapy for at least the full course of either residential based (approximately 30 days) or outpatient based (approximately 35 sessions), and a few participated for even longer. Treatment noncompleters (n = 35; 22%) left the program prior to staff approval; circumstances included elopement, discharge against staff advice, and expulsion due to violation of program rules.
2.1.2. Controls
The community-recruited control group (n = 99) was recruited from a large public school that was geographically located in the same seven-county metropolitan area where the treatment participants lived. These youth were randomly selected to provide a close approximation on age, ethnicity, and gender to the treatment group; their distribution of gender and ethnicity and their mean age were very close to those of the treatment sample (59% men; 83% White; mean age = 16.1). Inclusion criteria for controls were absence of a current or lifetime substance dependence disorder at baseline. Due to resource limitations, the controls did not receive a Year 1 assessment; but this group had complete data for intake, Year 4 and Year 5.5.
2.2. Typology
Assignment of the treatment cases (n = 159) to either the externalizing or internalizing group was based on the client’s pattern of scale scores obtained at intake from these scales that are part of the self-report Personal Experience Inventory (PEI; Henly & Winters, 1989; Winters & Henly, 1988): negative self-image (10 items, α =.84); psychological disturbance (10 items, α =.82); social isolation (8 items, α =.73); uncontrolled (12 items, α =.87); rejecting convention (11 items, α =.76); and deviant behavior (10 items, α =.81). Typology for an individual was determined based on the following procedures: Each individual was assigned both an internalizing and an externalizing score, which was computed as the average (nonweighted sum) T score across the three respective scales assigned to each subtype (internalizing = negative self-image, psychological disturbance, and social isolation; externalizing = uncontrolled, rejecting convention, and deviance); clients were then assigned to one of the following mutually exclusive groups based on their pattern of internalizing and externalizing scores.
Internalizers: Internalizing score > by at least one half SD than externalizing score;
Externalizers: Externalizing score > by at least one half SD than internalizing score;
Other-mixed: Internalizing and externalizing scores were within one half SD of each other; and
Other-nonclinical: Both internalizing and externalizing scores were < 36 T score, which is considered a score in a nonclinical range (Winters & Henly, 1988).
This strategy yielded the following breakdowns: externalizers (n = 76; 48%); internalizers (n = 65; 41%); other-mixed (n = 11; 7%); and other-nonclinical (n = 7; 3%).
2.3. Treatment
2.3.1. Program description
The treatment group was drawn from an adolescent drug program that consisted of residential and nonresidential units that was fully staffed by administrators, psychiatrists, psychologists, nurses, chemical dependency counselors, school teachers, and additional support staff. This Minnesota model program combines the principles of the Twelve Steps of Alcoholics Anonymous (AA) and basic principles of psychotherapy, and the goal of treatment is abstinence. The program is adjusted for adolescents in that the assessment process uses only adolescent instruments; family involvement in therapy is a high priority; several hours a day include in-program schooling (for residential); and group therapy and recreational activities are mainstays of therapeutic activities.
Clients are involved in a range of treatment components that typically span 4 consecutive weeks for residential clients and 30 sessions during 6 consecutive weeks for outpatient clients. Treatment components include group therapy and individual counseling, family therapy, lectures about the Twelve Steps of AA, a series of AA-based reading and writing assignments, school study sessions, and occupational and recreational therapy. Step work focuses on the first five steps of recovery: (a) admitting to the power of drugs to make one’s life unmanageable, (b) believing there is hope for change if you let yourself be helped, (c) learning from the advice of others as you explore making different decisions about your life, (d) taking an in-depth moral inventory of one’s life, and (e) discussing your past wrongs with a peer, counselor, or significant other. These steps are intended to increase the youth’s recognition that his or her drug involvement is causing problems in his or her life, that a significant lifestyle change is needed to reverse the current escalation of problems, and that support for change can be drawn from several sources in one’s home and community.
2.3.2. Treatment retention
Treatment completers received the full course of primary drug treatment, which is defined by an approved discharge by the client’s primary physician. All treatment completers (78%) participated in therapy for at least the full course of either residential based (approximately 30 days) or out-patient based (approximately 35 sessions). Treatment incompleters (22%) left the program prior to staff approval; circumstances included elopement, discharge against staff advice, and expulsion due to violation of program rules. Most of these noncompleters (81%) left treatment within the first week (residential) or by the fifth session (outpatient), and none of the other noncompleters participated in more than 50% of expected treatment length. (Some residential participants received outpatient treatment and vice versa.)
2.4. Drug involvement measures
For treatment participants, each of these measures was administered at baseline, Year 1, Year 4, and Year 5.5; for controls, they were administered at baseline, Year 4, and Year 5.5.
2.4.1. Drug use frequency
Drug use frequency (DUF) during the prior year was assessed for 12 major drug categories using a 5-point scale (5 = about daily; 4 = about weekly; 3 = about monthly; 2 = about less than monthly; 1 = abstinence). The descriptions of the drugs are identical to the items from the national senior high school surveys (Johnston, Bachman, & O’Malley, 1985). These DUF items have shown high internal consistency (α =.82–.93) and favorable 1-week test–retest stability (r =.86–.91) in drug clinic-referred samples (Winters, Stinchfield, & Henly, 2001). The dependent variable for the analysis was based on a “high-water response” across items; the highest frequency rating, regardless for which drug or drugs, was identified as the individual’s level of frequency of aggregate drug use for that respective period. This score was then used to further categorize individuals. Participants were categorized as improved if their high-water mark score was either abstinent or at the “about monthly” level. Participants were categorized as not improved if their high-water mark score was either “about weekly” or “about daily.” These categorizations are justified within the context that all treatment participants reported at intake either about weekly or about daily use of at least one drug.
2.4.2. SUD diagnoses
Prior year DSM-IV (American Psychiatric Association, 1994) SUDs were measured with the Adolescent Diagnostic Interview, a highly structured interview with favorable psychometric properties (Winters & Henly, 1993). Again a high-water decision rule was used; clients with any dependence diagnosis received the dependence descriptor; an abuse descriptor meant that the client had at least one abuse diagnosis but no dependence diagnosis; no diagnosis meant no abuse or dependence diagnosis was met. SUD was used to establish another set of outcome groups at each follow-up point, defined as follows: improved = no SUD or only one substance abuse diagnosis; not improved = presence of one or more substance dependence disorder or two or more substance abuse disorders, or both. These categorizations are justified given that all treatment participants reported at intake a dependence diagnosis for at least one substance.
2.5. Trajectory groups
Group analyses are not sensitive to individual patterns of change. Thus, we organized the data to permit a trajectory analysis. Given that controls had one less assessment (3) than the treatment group (4), we did not include controls in this analysis. To analyze trajectory patterns for the two treatment groups (externalizers and internalizers), we parsimoniously focused upon change in the diagnostic data from intake. Diagnostic status (1 = improved; 2 = not improved) was coded for each participant at each follow-up point (Year 1, Year 4, and Year 5.5). Given two possible codes across three time points, 8 (23) possible code types can be identified. The frequency distribution of all obtained code types was then inspected. Because most individuals revealed conceptually interesting patterns, we decided to rationally categorize code types rather than use statistical trajectory procedures. Three patterns that characterized most cases were identified and labeled as such: persistors, desistors, and resistors. Persistors (n = 68, 48%) were participants who showed no improved status for all three time points, or improvement once but not at Year 5.5 (pattern code type of 222, 122, or 212). Desistors (n = 54, 38%) were assigned to participants who showed improved status at both Year 4 and Year 5.5, or only at Year 5.5 (pattern code type of 211 or 221). Finally, we labeled as resistors (n = 17, 12%) those who showed improved status for all three follow-up points or showed lack of improvement at only Year 4 (pattern code type of 111 or 121). One possible code type, 112, was eliminated from consideration given that it did not conceptually fit into any of the three groups, and only a very small number cases revealed this pattern (n = 2).
2.6. Procedure
Adolescent clients and their parent or guardian were told during recruitment that the study was aimed at examining youth functioning as a result of prior drug abuse and that participation was independent of referral and treatment decisions by the facility. All testing was conducted by trained research staff. Intake measures were administered as part of the evaluation appointment. Participant follow-up measures were administered either in person or over the telephone for long-distance clients (n = 13 cases with at least one follow-up by telephone). Treatment participants were assessed at baseline and at three follow-up points (Year 1, Year 4, and Year 5.5); a limit on research funds required that control participants only be assessed at baseline and at two follow-up points (Year 4 and Year 5.5).
The study samples in this report (externalizers, n = 76; internalizers, n = 65; controls, n = 94) represent participants for whom complete follow-up data were obtained (i.e., baseline, Year 1, Year 4, and Year 5 for the treatment sample; baseline, Year 1, Year 4, and Year 5 for the control group).
We did examine attrition effects for cases for whom we did not obtain full follow-up data. A total of 19 eligible treatment (9%) participants and 5 eligible control (5%) participants (i.e., met initial study inclusion criteria) were not included in the analysis because of missing data for at least one follow-up data point (due to refusal or could not be located). A comparison between the follow-up attrition and nonattrition for the treatment cases on intake data indicated that the two groups significantly differed only on the PEI deviant behavior scale score, with the former group reporting a higher mean scale score (p <.01). These results suggest that our estimates of treatment outcome are not biased as a result of the follow-up data favoring the less severe cases.
3. Results
3.1. Validity of self-report
Urine drug screens were collected at each follow-up to test for the presence of alcohol, tetrahydrocannabinol at 20 mg/ml, amphetamines, opiates, barbiturates, cocaine, and benzodiazepines. The laboratory used a two-step process in which any positive finding by immunoassay (or gas chromatography for alcohol) is verified by a second testing of gas chromatography/mass spectrometry. As a means of validating the self-report, at each follow-up, all participants completed a revised DUF that asked if use had occurred during a period corresponding to the time frame of the urinalysis (e.g., use of alcohol during the prior 10 hours, any use of cannabis as recent as 2 days ago, daily use of cannabis within the prior 6 weeks). We performed analyses of correspondence between self-reports and urine testing across all follow-up assessments. We found unadjusted percent-exact agreements of 92% between urinalysis and adjusted DUF score. We also calculated kappa coefficients to adjust for prevalence rates, and the result was quite encouraging (κ =.80). In two cases, the self-report did not disclose cannabis use when the urinalysis was positive, and in one instance, the self-report disclosed cannabis use in the presence of a negative urine test.
3.2. Treatment group (externalizers vs. internalizers)
3.2.1. Treatment completion
Treatment completers were more likely to be internalizers compared to externalizers (odds ratio [OR] = 2.6, p <.01).
3.2.2. Drug use frequency
An improved status on DUF was more likely to be associated with internalizers compared with externalizers at all three data points (Year 1, Year 4, and Year 5.5). The ORs were 2.5, 2.3, and 3.9, respectively, all p <.01.
3.2.3. Substance use disorder
The pattern of results for the SUD data was similar to the DUF results. Internalizers were significantly more likely to report an improved SUD status than externalizers at Year 4 (OR = 2.0, p <.05) and Year 5.5 (OR = 6.0, p <.01). The OR at Year 1 was not significant (OR = 1.4, p >.05), but the results were in the expected direction (internalizers had higher improvement rate than externalizers, 49% and 41%, respectively; Table 2).
Table 2.
ORs of outcome measures as a function of subject group
| EXT
|
INT
|
CON
|
EXT vs. INT
|
EXT vs. CON
|
INT vs. CON
|
|
|---|---|---|---|---|---|---|
| Outcome Variables | % | % | % | OR | OR | OR |
| Treatment Completers | 66 | 85 | 2.6 | |||
| Drug use improved | ||||||
| Year 1 | 39 | 62 | 2.5 | |||
| Year 4 | 26 | 45 | 64 | 2.3 | 5.0 | 2.2 |
| Year 5.5 | 14 | 40 | 57 | 3.9 | 8.4 | 2.6 |
| SUD improved | ||||||
| Year 1 | 41 | 49 | 1.4 a | |||
| Year 4 | 34 | 61 | 84 | 2.0 | 10.1 | 5.1 |
| Year 5.5 | 16 | 57 | 80 | 6.0 | 18.5 | 3.1 |
Note. Except when indicated, all ORs are significant (p <.05). EXT = externalizers; INT = internalizers; CON = controls.
Not significant.
3.3. Treatment group (internalizers vs. externalizers): Survival analysis
The survival (improved status) analysis for DUF and SUD showed significant group differences in the rates of improvement across all data points (Year 1, Year 4, and Year 5.5). Internalizers showed significantly higher improvement rates compared with externalizers (Breslow test: 9.5 [DUF], p <.01; 6.1 [SUD], p <.01). The survival patterns for DUF indicated that internalizers had an improvement rate of 62% at Year 1, dropping to 40% at Year 5.5. For externalizers, their improvement rate at Year 1 was 39% and dropped to 14% at Year 5.5. The SUD survival rates showed a similar pattern. However, at Year 1, the two groups had relatively comparable improvement rates (49% for internalizers and 41% for externalizers), but the survival rate of improvement showed a greater significant decline for externalizers compared with internalizers after Year 1. At Year 5.5, 57% of internalizers reported improvement whereas only 18% of externalizers reported improvement (Figs. 1 and 2).
Fig. 1.
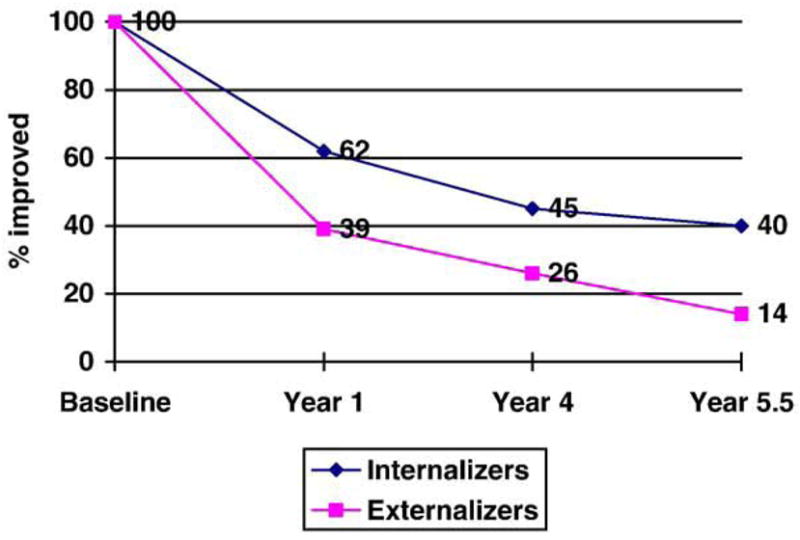
Survival rates of DUF: internalizers vs. externalizers. Note. Breslow test = 9.5, p <.01. DUF variable at each data point refers to those who “improved” their drug use level by virtue of reporting that their prior year aggregate DUF fell below either daily or weekly use (see text for description).
Fig. 2.
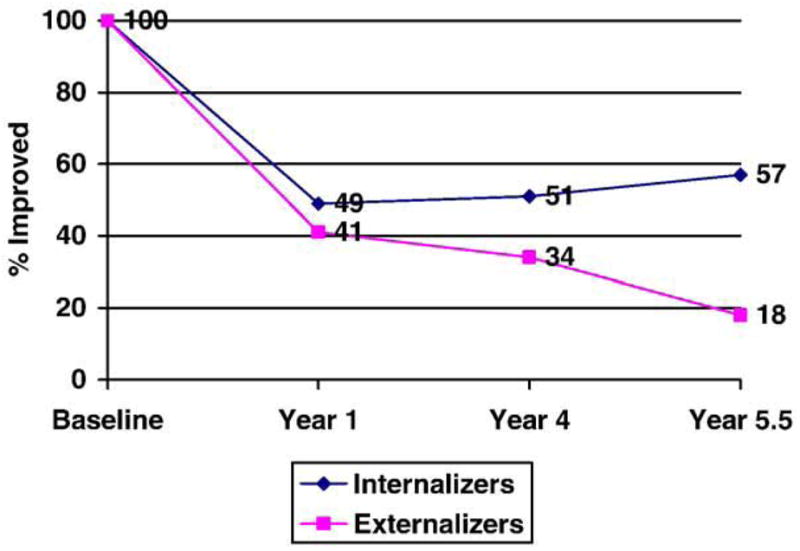
Survival rates of SUD variable: internalizers vs. externalizers. Note. Breslow test = 6.3, p <.01. SUD variables at each data point refer to those who improved their SUD profile by virtue of reporting either no SUD or only an SUD (see text for description).
3.4. Internalizers versus internalizers: Trajectory findings
Given sample size considerations, the comparison of internalizers and externalizers as a function of trajectory status was structured such that we compared the combined group of desistors and resistors (general “positive” outcomes) versus the group of persistors (a “negative” outcome). An OR analysis indicated that internalizers, compared with externalizers, were seven times more likely to be desistors/resistors as opposed to persistors (OR = 7.1, p <.01). Thus, the individual-level analysis confirmed that the between-group analysis, that is, internalizers showed a more favorable outcome as compared with externalizers (Table 3).
Table 3.
OR of trajectory group as a function of subtype
| EXT
|
INT
|
||
|---|---|---|---|
| Trajectory group | % | % | OR (persistor vs. desistor/resistor) |
| Persistors | 76 | 30 | |
| Desistors/Resistors | 24 | 70 | 7.1 |
3.5. Treatment group (internalizers vs. externalizers) versus control group
We next conducted an analysis that compared our treatment subgroups (internalizers and externalizers) against the control group. We computed pairwise comparisons at Year 4 and Year 5.5 (the matched follow-up data points for the treatment and control participants) on the DUF and SUD outcomes (improved and nonimproved). The results indicated that the controls were significantly more likely to be assigned an improved status for DUF and SUD compared with both the internalizers and externalizers (range of ORs = 2.2–18.5, all p <.01). As would be expected given our prior analysis, the comparison of externalizers versus controls produced higher ORs (5.0–18.5) than the ORs for the comparison of internalizers versus controls (2.2–5.2).
4. Discussion
This study provides support for our three main predictions. The findings indicated that externalizers, as compared with internalizers, revealed poorer outcomes on all measures, which included treatment retention and the short-term and long-term drug behavior outcomes. With respect to the pattern of results pertaining to the DUF and SUD drug outcomes, the rate of decline for the two treatment groups was relatively steep from baseline to Year 1, followed by a continued but less dramatic decline thereafter. However, the outcome gap between externalizers and internalizers was the widest at Year 5.5. When all three participant groups were compared at Year 4 and Year 5.5, externalizers and internalizers had worse outcomes than controls.
The pattern of outcome data associated with the treatment group is comparable to outcome findings observed in other adolescent drug treatment studies, including those that have investigated general 12-Step approaches (Harrison & Hoffman, 1989; Winters et al., 2000) and other treatment approaches (Deas & Thomas, 2001; Williams et al., 2000). However, when the separate treatment groups defined by typology are examined, a different outcome picture emerges. The long-term benefits of treatment seem to be significant for internalizers compared with externalizers. At Year 5.5, 40% of internalizers reported improvement in terms of their extent of drug use involvement, and 57% showed improvement in terms of their drug use symptomatology. This level of treatment improvement for the internalizers exceeds the more traditional outcome findings reported in the literature. However, treatment outcome for externalizers reveals a more negative pattern. The improvement rates at Year 5.5 for externalizers were nearly 35% less for DUF and 32% less for SUD. Given that externalizers were more likely to not complete treatment compared with internalizers, it is tempting to consider the impact of treatment retention on outcome. The treatment completion rate among externalizers was much lower (66%) compared with internalizers (84%). However, we conducted a post hoc analysis by comparing treatment completers and treatment noncompleters as a function of typology, and externalizers still revealed poorer outcome on DUF and SUD at all three time points as compared with internalizers (range of χ2 = 6.7–12.2; all p <.05).
Given that a large population of externalizers were boys and that a large proportion of internalizers were girls, we conducted a post hoc analysis to see if gender and typology were associated with outcome. None of the outcome findings (treatment retention and all drug involvement measures) were related to gender. We also examined drugs commonly used by relapsers. In our earlier reports (Winters et al., 2000; Winters, Stinchfield, 2007), we observed that relapsers typically used either alcohol or marijuana at follow-up. In this study, we found that regardless of typology, alcohol and marijuana were clearly the drugs used most often at Year 4 and Year 5.5. This tendency for relapsers to fall back to these drugs suggests a continuity of between drug of choice prior to receiving treatment and at relapse, a pattern that ought to be emphasized as part of relapse prevention.
The finding that youth with externalizing disorders relapsed more rapidly and at higher rates than internalizers suggests poorer prognostic outcomes of youth who show core features of delinquency or deviant behavior (e.g., behavior disinhibition, sensation-seeking traits, poor social skills deficits, and cognitive-processing deficits; e.g., Crowley et al., 1998). As noted in the introduction, several studies have shown the prognostic significance of co-occurring conduct disorder for drug-abusing youth (Brown, Gleghorn, Schuckit, Myers, & Mott, 1996; Crowley et al., 1998; Myers et al., 1995; Tomlinson, Brown, & Abrantes, 2004). An additional contribution of this study to this comorbidity literature is that our follow-up period is longer than the more typical shorter term follow-up periods in the literature, and we included a community-based control group. Other recent treatment outcome studies have primarily focused on 1-year outcome and explored course of alcohol use and related problems (Chung, Maisto, Cornelius, & Martin, 2004; Maisto, Pollock, Cornelius, Lynch, & Martin, 2003; Maisto, Pollock, Lynch, Martin, & Ammerman, 2001).
Both the fields of developmental psychopathology and adolescent drug treatment have stressed the importance of identifying dimensional variations in adolescent disorders that may have etiological or clinical relevance (Kazdin & Kagan, 1994). The study supports the point of view that treatment should tailor curriculum by targeting features that distinguish adolescents with important variations. Given the poorer outcomes by externalizers, our study supports the position that adolescents in this group, many of whom are likely to come from families with low level of family cohesion (Henggler, 1993; Loeber, 1989), may need a focused form of treatment aimed at ameliorating these behaviors and the risk factors that promote such behaviors. For externalizing adolescents, poor affiliation with parents, schools, and prosocial institutions may be perennial risk factors contributing to poorer treatment outcome.
The statistical procedures we used for the typology analysis identified very few adolescents who were elevated on both internalizing and externalizing features. Our observation of so few mixed cases is similar to findings by Mezzich et al. (1993) but in contrast to the clinical sample described by Rowe et al. (2001). Our sample of severe drug abusers, all of whom met at least one dependence disorder, is more similar to the study by Mezzich et al. than to the more moderate drug-abusing sample described in the study by Rowe et al. Our findings do not contradict the notion that delinquent adolescents are absent of internalizing problems (Armistead, Wierson, Forehand, & Frame, 1992). Nearly one third of our externalizers had an internalizing factor score above the treatment mean. Thus, our procedure for subtyping the sample should not be viewed as evidence that mixed cases did not exist.
Our finding that girls were overrepresented in the internalizing group and boys were overrepresented in the externalizing group may, on the face of it, appear to be a contradiction to findings from other studies. Rowe et al. (2001) found that girls were overrepresented in their externalizing group and that boys were overrepresented in the exclusive drug-abusing group. Other studies have shown that girls with drug abuse problems may report high levels of conduct problems (Dakof, 2000). Although did not find a proportionally higher rate of girls in the externalizing group, girls in the internalizing group had a mean T score on the externalizing factor (M = 52) that exceeded the mean T score on this factor of the drug clinic standardization sample (M = 50) based on the PEI standardization norms (Winters & Henly, 1988). Another way to look at these data is that 64% of internalizing girls had an externalizing factor score that exceeded the standardized drug clinic mean score, whereas only 32% of boys in the externalizing group had a mean T score on the externalizing factor that equaled or exceeded the standardized drug clinic score for the internalizing factor. Thus, our data do support the notion that drug-abusing girls reported more severe problems than drug-abusing boys.
4.1. Limitations
Because the study did not involve random assignment, caution must be exercised when interpreting the comparisons between groups. In addition, the study described outcomes for youth who received treatment in the mid-to-late 1990s, which may make our results outdated by today’s standards of treatment.
Another important limitation of the study is that we focused our analysis on posttreatment drug use behaviors. This focus does not minimize the importance of understanding mediating and moderating variables that impact treatment outcome, such as aftercare treatment variables and other environmental factors unrelated to treatment (Institute of Medicine, 1990). The adolescent outcome research literature points to the importance of the interrelationships of patient and contextual variables because they pertain to posttreatment outcome (Friedman, Glickman, & Morrissey, 1986; Latimer et al., 2000; Winters, Lee, Stinchfield, & Latimer, in press).
Another limitation of the study is its sampling bias. The sample is largely White, middle class, and suburban, which limits generalizability to other samples. In addition, our study does not generalize to adolescent drug abusers not receiving treatment who may show different patterns of internalizing and externalizing characteristics.
In addition, the study relied primarily on self-report measures. Although there are studies supporting the validity of adolescent drug abuse self-report (Maisto, Connors, & Allen, 1995), one cannot rule out that our self-report data may reflect distrustfulness or inaccuracies. In an effort to validate our self-report data, we did compare client ratings with urinalysis, and favorable overall agreement was observed.
4.2. Summary
Our developmental psychopathology approach to subtyping a drug treatment sample underscores the need to assess core internalizing and externalizing characteristics among adolescent drug-abusing treatment individuals. The study also emphasizes the potential value of tailoring treatment to address the unique and important underlying risk factors of those whose clinical symptomatology shows a dominance of externalizing characteristics. Future studies are needed to evaluate the processes by which psychopathology impairs drug treatment outcome, how this affects the course of outcome over the long term, and the circumstances under which comorbid adolescents are at distinct risk for a return to drug involvement following treatment.
Acknowledgments
This study was supported by the National Institute on Drug Abuse through Grants DA05104 and DA15347.
Footnotes
This article appeared in a journal published by Elsevier. The attached copy is furnished to the author for internal non-commercial research and education use, including for instruction at the authors institution and sharing with colleagues.
Other uses, including reproduction and distribution, or selling or licensing copies, or posting to personal, institutional or third party websites are prohibited.
In most cases authors are permitted to post their version of the article (e.g. in Word or Tex form) to their personal website or institutional repository. Authors requiring further information regarding Elsevier’s archiving and manuscript policies are encouraged to visit: http://www.elsevier.com/copyright
References
- Adams L, Wallace JL. Residential treatment for the ADHD adolescent substance abuser. Journal of Child and Adolescent Substance Abuse. 1994;4:35–44. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Armistead L, Wierson M, Forehand R, Frame C. Psychopathology in incarcerated juvenile delinquents: Does it extend beyond externalizing problems? Adolescence. 1992;27:309–314. [PubMed] [Google Scholar]
- Brown SA, Gleghorn A, Schuckit MA, Myers MG, Mott MA. Conduct disorder among adolescent alcohol and drug abusers. Journal of Studies on Alcohol. 1996;57:314–324. doi: 10.15288/jsa.1996.57.314. [DOI] [PubMed] [Google Scholar]
- Catalano RF, Hawkins JD, Wells EA, Miller JM. Evaluation of the effectiveness of adolescent drug abuse treatment, assessment of risks for relapse and promising approaches for relapse prevention. International Journal of the Addictions. 1991;25:1085–1140. doi: 10.3109/10826089109081039. [DOI] [PubMed] [Google Scholar]
- Chung T, Maisto SA, Cornelius JR, Martin CS. Adolescents’ alcohol and drug use trajectories. Journal of Studies on Alcohol. 2004;65:105–114. doi: 10.15288/jsa.2004.65.105. [DOI] [PubMed] [Google Scholar]
- Clark DB, Bukstein OG. Psychopathology in adolescent alcohol abuse and dependence. Alcohol Health and Research World. 1998;22:117–121. [PMC free article] [PubMed] [Google Scholar]
- Clark DB, Bukstein OG, Smith MG, Kaczynski NA, Mezzick AC, Donovan JE. Identifying anxiety disorders in adolescents hospitalized for alcohol abuse or dependence. Psychiatric Services. 1995;46:618–620. doi: 10.1176/ps.46.6.618. [DOI] [PubMed] [Google Scholar]
- Clark DB, Neighbors B. Adolescent substance abuse and internalizing disorders. Child and Adolescent Psychiatric Clinics of North America. 1996;5:45–57. [Google Scholar]
- Crowley TJ, Mikulich SK, Macdonald M, Young SE, Zerbe GO. Substance-dependent, conduct-disordered adolescent males: Severity of diagnosis predicts 2-year outcome. Drug and Alcohol Dependence. 1998;49:225–237. doi: 10.1016/s0376-8716(98)00016-7. [DOI] [PubMed] [Google Scholar]
- Dakof GA. Understanding gender differences in adolescent drug abuse: Issues of comorbidity and family functioning. Journal of Psychoactive Drugs. 2000;32:25–32. doi: 10.1080/02791072.2000.10400209. [DOI] [PubMed] [Google Scholar]
- Deas D, Thomas SE. An overview of controlled studies of adolescent substance abuse treatment. American Journal on Addictions. 2001;10:178–189. doi: 10.1080/105504901750227822. [DOI] [PubMed] [Google Scholar]
- DeMilio L. Psychiatric syndromes in adolescent substance abusers. American Journal of Psychiatry. 1989;146:1212–1214. doi: 10.1176/ajp.146.9.1212. [DOI] [PubMed] [Google Scholar]
- Dobkin PL, Chabot L, Maliantovitch K, Craig W. Predictors of outcome in drug treatment of adolescent inpatients. Psychological Reports. 1998;83:175–186. doi: 10.2466/pr0.1998.83.1.175. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Jensen PS. Predictive validity of categorically and dimensionally scored measures of disruptive childhood behaviors. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:477–485. [PubMed] [Google Scholar]
- Friedman A, Glickman N, Morrissey M. Prediction to successful treatment outcome by client characteristics and retention in treatment in adolescent drug treatment programs: A large-scale cross validation study. Journal of Drug Education. 1986;16:49–165. doi: 10.2190/98EM-3TNT-5066-7QHP. [DOI] [PubMed] [Google Scholar]
- Grella CE, Hser Y, Joshi V, Rounds-Bryant J. Drug treatment outcomes for adolescents with comorbid mental and substance use disorders. Journal of Nervous and Mental Disease. 2001;189:384–392. doi: 10.1097/00005053-200106000-00006. [DOI] [PubMed] [Google Scholar]
- Harrison PA, Fulkerson JA, Beebe TJ. DSM-IV substance use disorder criteria for adolescents: A critical examination based on a statewide school survey. American Journal of Psychiatry. 1998;155:486–492. doi: 10.1176/ajp.155.4.486. [DOI] [PubMed] [Google Scholar]
- Harrison PA, Hoffmann N. CATOR report: Adolescent treatment completers one year later. St. Paul, MN: CATOR; 1989. [Google Scholar]
- Hartwell S, Ungemack J, Babor TF. Adolescent substance abuse treatment needs assessment: The 1995 adolescent alcohol and drug use school survey state of Connecticut. Hartford, CT: Department of Mental Health and Addiction Services; 1996. [Google Scholar]
- Henggler SW. Multisystemic treatment of serious juvenile offenders: Implications for the treatment of substance-abusing youths. In: Onken LS, Blaine JD, Boren JJ, editors. Behavioral treatments for drug abuse and dependence. Rockville, MD: National Institute on Drug Abuse Research Monograph; 1993. pp. 181–200.pp. 137 [PubMed] [Google Scholar]
- Henly GA, Winters KC. Development of psychosocial scales for the assessment of adolescent alcohol and drug involvement. International Journal of the Addictions. 1989;24:973–1001. doi: 10.3109/10826088909047324. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social status. New Haven, CT: Yale University; 1975. [Google Scholar]
- Horner BR, Scheibe KE. Prevalence and implications of attention-deficit hyperactivity disorder among adolescents in treatment for substance abuse. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:30–36. doi: 10.1097/00004583-199701000-00014. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Broadening the base of treatment for alcohol problems. Washington, DC: National Academy Press; 1990. pp. 279–312. [Google Scholar]
- Johnston LD, Bachman JG, O’Malley PM. Monitoring the future: Questionnaire responses from the nation’s high school seniors, 1984. Ann Arbor, MI: Survey Research Center, Institute for Social Research; 1985. [Google Scholar]
- Kaminer Y, Burleson JA, Blitz C, Sussman J, Rounsaville BJ. Psychotherapies for adolescent substance abusers: A pilot study. Journal of Nervous and Mental Disease. 1998;186:684–690. doi: 10.1097/00005053-199811000-00004. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Progression of therapy research and clinical application of treatment require better understanding of the change process. Clinical Psychology: Science and Practice. 2001;8:43–151. [Google Scholar]
- Kazdin AE, Kagan J. Models of dysfunction in developmental psychopathology. Clinical Psychology: Science and Practice. 1994;1:35–52. [Google Scholar]
- Latimer WW, Ernst J, Hennessey J, Stinchfield RD, Winters KC. Relapse among adolescent drug abusers following treatment: The role of probable ADHD status. Journal of Child and Adolescent Substance Abuse. 2004;13:1–16. [Google Scholar]
- Latimer WW, Newcomb M, Winters KC, Stinchfield RD. Adolescent substance abuse treatment outcome: The role of substance abuse problem severity, psychosocial, and treatment factors. Journal of Consulting and Clinical Psychology. 2000;68:684–696. [PubMed] [Google Scholar]
- Loeber R. Natural histories of conduct problems, delinquency, and associated substance use: Evidence for developmental progressions. In: Lahey BB, Kazdin AE, editors. Advances in clinical child psychopathology. New York: Plenum; 1989. pp. 73–124. [Google Scholar]
- Maisto SA, Connors GJ, Allen JP. Contrasting self-report screens for alcohol problems: A review. Alcoholism: Clinical and Experimental Research. 1995;19:1510–1516. doi: 10.1111/j.1530-0277.1995.tb01015.x. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Pollock NK, Cornelius JR, Lynch KG, Martin CS. Alcohol relapse as a function of relapse definition in a clinical sample of adolescents. Addictive Behaviors. 2003;28:449–459. doi: 10.1016/s0306-4603(01)00267-2. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Pollock NK, Lynch KG, Martin CS, Ammerman R. Course of functioning in adolescents 1 year after alcohol and other drug treatment. Psychology of Addictive Behaviors. 2001;15:68–76. doi: 10.1037/0893-164x.15.1.68. [DOI] [PubMed] [Google Scholar]
- Mezzich AC, Tarter R, Kirisci L, Clark D, et al. Subtypes of early age onset alcoholism. Alcoholism: Clinical and Experimental Research. 1993;17:767–770. doi: 10.1111/j.1530-0277.1993.tb00838.x. [DOI] [PubMed] [Google Scholar]
- Moss HB, Kirisci L, Mezzich AC. Psychiatric comorbidity and self-efficacy to resist heavy drinking in alcoholic and nonalcoholic adolescents. American Journal on Addictions. 1994;3:204–212. [Google Scholar]
- Mott MA, Myers MG, Tammariello CF, Brown SA. Conduct disorder diagnosis is related to long-term adolescent drug treatment outcome. Poster presented at the American Psychological Society Annual Meeting; San Diego. 1992. [Google Scholar]
- Myers MG, Brown SA, Mott MA. Preadolescent conduct disorder behaviors predict relapse and progression of addiction for adolescent alcohol and drug abusers. Alcoholism: Clinical and Experimental Research. 1995;19:528–1536. doi: 10.1111/j.1530-0277.1995.tb01019.x. [DOI] [PubMed] [Google Scholar]
- Randall J, Henggeler SW, Pickrel SG, Brondino MJ. Psychiatric comorbidity and the 16-month trajectory of substance-abusing and substance-dependent juvenile offenders. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1118–1124. doi: 10.1097/00004583-199909000-00015. [DOI] [PubMed] [Google Scholar]
- Rowe CL, Liddle HA, Dakof GA. Classifying clinically referred adolescent substance abusers by level of externalizing and internalizing symptoms. Journal of Drug Education. 2001;11:41–65. [Google Scholar]
- Surgeon General. A report of the Surgeon General, U.S. Department of Health and Human Services. Atlanta, GA: Center for Disease Control and Prevention, Center for Health Promotion and Education; 1988. The health consequences of smoking: Nicotine addiction. [Google Scholar]
- Tomlinson KL, Brown SA, Abrantes A. Psychiatric comorbidity and substance use treatment outcomes of adolescents. Psychology of Addictive Behaviors. 2004;18:160–169. doi: 10.1037/0893-164X.18.2.160. [DOI] [PubMed] [Google Scholar]
- Whitmore EA, Mikulich SK, Ehlers KM, Crowley TJ. One-year outcome of adolescent females referred for conduct disorder and substance abuse/dependence. Drug and Alcohol Dependence. 2000;59:131–141. doi: 10.1016/s0376-8716(99)00112-x. [DOI] [PubMed] [Google Scholar]
- Williams RJ, Chang SY Addiction, Centre Adolescent Research Group. A comprehensive and comparative review of adolescent substance abuse treatment outcome. Clinical Psychology: Science and Practice. 2000;7:138–166. [Google Scholar]
- Winters KC. Treating adolescents with substance use disorders: An overview of practice issues and treatment outcomes. Substance Abuse. 1999;20:203–225. doi: 10.1080/08897079909511407. [DOI] [PubMed] [Google Scholar]
- Winters KC, Henly GA. Personal Experience Inventory and manual. Los Angeles, CA: Western Psychological Services; 1988. [Google Scholar]
- Winters KC, Henly GA. Adolescent Diagnostic Interview and manual. Los Angeles, CA: Western Psychological Services; 1993. [Google Scholar]
- Winters KC, Latimer WW, Stinchfield RD. Adolescent treatment. In: Ott PJ, Tarter RE, Ammerman RT, editors. Sourcebook on substance abuse: Etiology, epidemiology, assessment and treatment. New York: Allyn and Bacon; 1999. [Google Scholar]
- Winters KC, Stinchfield RD, Henly GA. Technical report on the Personal Experience Inventory. Minneapolis, MN: Center for Adolescent Substance Abuse Research, Department of Psychiatry, University of Minnesota; 2001. [Google Scholar]
- Winters KC, Lee S, Stinchfield RD, Latimer WW. Psychosocial factors associated with long-term outcome of drug-abusing youth following 12-Step treatment. Substance Abuse. doi: 10.1016/j.jsat.2006.12.003. in press. [DOI] [PubMed] [Google Scholar]
- Winters KC, Stinchfield RD, Latimer WW, Lee S. Long-term outcome of substance dependent youth following 12-Step treatment. Journal of Substance Abuse Treatment. 2007;33:61–69. doi: 10.1016/j.jsat.2006.12.003. [DOI] [PubMed] [Google Scholar]
- Winters KC, Stinchfield RD, Opland E, Weller C, Latimer WW. The effectiveness of the Minnesota Model for treating adolescent drug abusers. Addiction. 2000;95:601–612. doi: 10.1046/j.1360-0443.2000.95460111.x. [DOI] [PubMed] [Google Scholar]


