Abstract
Objective
To analyse the process of end of life decisions in a neurosurgical environment.
Methods
All 113 neurosurgical patients, who were subject to so called end of life decisions within a one year period were prospectively enrolled in a computerised data bank. Decision pathways according to patient and physician related parameters were assessed.
Results
Leading primary diagnoses of the patients were traumatic brain injury and intracranial haemorrhage. Forty‐five patients had undergone an emergency neurosurgical operation prior to end of life decision, N = 69 were conservatively treated, which included intracranial pressure recording, or they were not offered neurosurgical care because of futile prognosis. N = 111 died after a median of two (zero to nine) days. Two, in whom the end of life decisions were revised, survived. Clear decisions to terminate further treatment were made by a senior staff member on call being informed by the senior resident on call (27.4%), difficult decisions on the basis of extensive round discussions (71.7%), and very difficult decision by an interdisciplinary ethical consult (0.9%). Decisions were further substantiated by electrophysiological examinations in N = 59.
Conclusion
End of life decisions are to be considered standard situations for neurosurgeons. These decisions may reach a high rate of “positive” prediction, if substantiated by electrophysiological examinations as well as on the grounds of clinical experience and respect for the assumed will of the patient. The fact that patients may survive following revision of an end of life decision underlines the necessity for repeated reassessment of these decisions. Ethical training for neurosurgeons is to be encouraged.
Keywords: end of life decision, neurosurgical intensive care, terminal illness
Death does not occur in a controlled and organised manner—neither do the situations associated with it. In one large study among neurological and neurosurgical patients the decisions to withdraw mechanical ventilation proved not to be based on the characteristics of the healthcare delivery system itself—for example, whether it was academic, private or insurance based.1 Thus, neurosurgeons on call may be confronted with dying and death at any time and place during their routine work—independent of the environment in which they work. The decision process with regard to the action to be taken or not to be taken, and even the decision to postpone this decision involves vigorous assessment of the actual situation, clinical status and sociocultural background of the patient, including his or her presumptive will with regard to life sustaining measures.2,3 Occasionally, these decisions are made on the basis of electronically transmitted computed tomography (CT) images and telephone conferences with physicians who are alone at community hospitals. Thus, there is a chance that the most decisive moment in a human beings life—the decision to start or to abandon/withhold possible further life saving treatment—is being made in a potentially error prone situation. We have prospectively studied the frequency and the basis of so called “end of life decisions” over a one year period at a busy academic neurosurgical centre, in order to analyse how such situations are handled on a daily basis.
Patients and methods
Patient recruitment started in 09/2002 and ended in 08/2003. All patients, in whom a so called end of life decision was being made at the department of neurosurgery at the University of Bonn Medical Center, were included in the study.
Inclusion criteria were:
Refusal of neurosurgical treatment because of suspected futile prognosis at the time of emergency admission. A prognosis was considered futile, if, according to the recent body of knowledge, surgical therapy would not improve the patient's prognosis—for example, in cases of brainstem haemorrhage, or bilaterally fixed and dilated pupils for > two hours in adult patients with traumatic brain injury.
Reduction or withdrawal of continuing life support in patients on the neurosurgical intensive care unit (NICU)—for example, in cases of withdrawal of vasopressor agents.
Do not resuscitate order (applied by the neurointensivists together with the consultant in charge and with the permission of the patient's relatives). These decisions were further augmented if the conjectural will of the patient could be retrieved from so called “patient testaments”, which were signed by the patient prior to his/her disease, and by electrophysiological tests (see below).
The patients' biodata; diagnoses; diagnostic tests for the functional integrity of nervous system conductivity such as somatosensory evoked potentials (SSEPs) or electroencephalography (EEG); means of treatment, and clinical course were prospectively collected and stored on a computerised database (MS EXCEL®).
The decision pathways were assessed and ranked daily but after the fact, according to the information provided by the involved physicians—for example, the definition of clear emergency situations with only limited time for discussion among staff members, that is, arrival of comatose poly‐traumatized patient, vs. situations which left more time for the decision process to take place during daily staff conferences—for example, repeated septic shock in an ICU patient in persistent vegetative state. Thus, we conducted a prospective study in the sense that a daily census was performed, but the decisions by the staff members were neither preplanned nor affected by the ongoing study.
Results
A total of N = 137 patients were enrolled. Twenty four patients were rejected for further neurosurgical treatment upon admission on the basis of futile prognosis and transferred to regional community hospitals. In those patients, it was not possible to obtain complete information about their concomitant diseases and further course and they were excluded from the key study. Thus, in N = 113 (51 females, 62 males) patients, follow up information and the database could be completed (see Table 1). Their mean age was 65 years (ranging from 4–94 years). Traumatic brain injury (TBI), intracerebral haemorrhage (ICH), and subarachnoid haemorrhage (SAH) were the leading diagnoses in the patient collective studied. Our annual number of admissions to the neurosurgical ICU (emergency admissions plus postoperative patients) were N = 997 in 2002 and 979 in 2003. Thus the N = 113 patients of this study make up 11.4% of the average annual admission rate during the study time.
Table 1 Overview of diagnoses and diagnostic measures in 113 neurosurgical patients, in whom an end of life decision was being made.
| Number (percentage) of patients (out of N = 113) | |
|---|---|
| Diagnosis | |
| TBI | 30 (26.5%) |
| ICH | 27 (23.0%) |
| SAH | 21 (18.6%) |
| Infarction | 10 (8.8%) |
| Other | 26 (23.0%) |
| Prior neurosurgical operation | |
| Yes | 44 (38.9%) |
| No | 69 (61.1%) |
| Stable cardiac status | |
| Yes | 82 (72.6%) |
| No | 31 (27.4%) |
| Uni‐/bilaterally fixed dilated pupils | |
| Yes | 82 (72.6%) |
| No | 31 (27.4%) |
| Concomitant disease(s) | |
| Yes | 49 (43.4%) |
| No | 64 (56.6%) |
| Supplementary electrophysiology | |
| Yes | 58 (51.3%) |
| No | 55 (48.7%) |
| Attempted resuscitation | |
| Yes | 14 (12.4%) |
| No | 99 (87.6%) |
| Enrolled in organ donor programme | |
| Yes | 15 (13.3%) |
| No | 99 (87.6%) |
| Insurance status | |
| Regular | 81 (76.1%) |
| Private | 15 (13.3%) |
| Social welfare/unclear | 12 (10.6%) |
| Time to death in N = 111 patients | 0–9 (median: 2) days |
| Number of survivors | 2 (1.8%) |
N = 44 (38.9%) patients had undergone a neurosurgical operation prior to the end of life decision (mainly haematoma evacuation), and N = 69 (61.1%) were conservatively treated on the NICU—including monitoring of intracranial pressure (ICP).
At the time of decision making N = 82 (72.6%) were in a stable cardiovascular state, and N = 31 (27.4%) were not. N = 82 (72.6%) had uni‐/bilaterally fixed/dilated pupils as signs of “brain herniation”. In N = 14 (12.4%), cardiopulmonary resuscitation was attempted/performed prior to the end of life decision.
Known concomitant disease status at time of decision making was as follows: none in N = 64 patients (56.6%); heart disease in N = 15 (13.3%); severe pulmonary disease in N = 2 (1.8%); systemic cancer in N = 6 (5.3%); diabetes in N = 1 (0.9%); renal insufficiency in N = 3 (2.7%); hepatic disease or coagulation disorder in N = 6 (5.3%); polymorbidity in N = 8, and (7.1%), polytrauma in N = 6 (5.3%).
Fifteen patients (13.3%) were enrolled in the organ donor programme of the University of Bonn Medical Center.
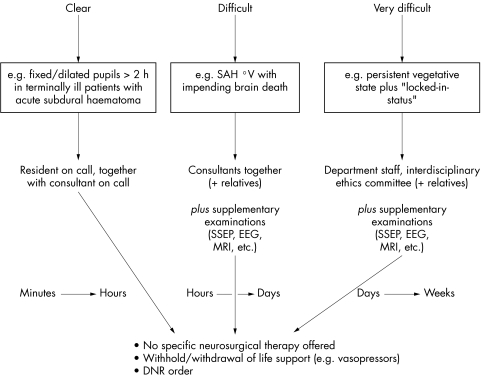
The decisions to withdraw/withhold were grouped as follows (see Fig. 1):
Figure 1 Hierarchy of “end of life decisions” in a total of 113 patients.
In N = 31 patients (27.4%) the decisions were primarily made jointly by the senior staff member and the resident on call. These decisions were considered clear decisions.
In N = 81 patients (71.7%) the decisions were made on the basis of senior staff discussions at rounds and supplementary examinations. These decisions were considered difficult decisions.
In one patient (0.9%), who remained in a persistent vegetative state following palliative removal of a complex cerebral arteriovenous malformation (AVM), which had led to progressive dementia due to chronic intracranial venous hypertension, the decision was made by an interdisciplinary ethical consult. This decision was considered a very difficult decision.
The overall rate of SSEP examinations was 51.3% (N = 58 patients). The standardised “brain death protocol” (two clinical examinations after 12 consecutive hours, performed by two independent and experienced physicians) including EEG was completed in N = 25 patients (22.1%).
One hundred and eleven patients (98.2%) died after a median of two (zero to nine) days following the “end of life decision”. Two patients (1.8%), in whom the end of life decisions were revised, survived (one with cerebellar haemorrhage, one with diffuse traumatic brain injury).
Case 1 (clear decision)
This seventy one year old man was admitted with a large spontaneous cerebellar haemorrhage. He was intubated, unsedated and breathing spontaneously. Pupillary and other brainstem derived reflexes were absent, and he did not show any sign of motor reaction toward painful stimuli. His coagulation status was poor due to long term anticoagulation because of tachyarrhythmia, and he was suffering from diabetes mellitus. The staff member on duty together with the resident on call decided together to withhold any further surgical and/or medical therapy, and the patient died a few hours following admission.
Case 2 (revised end of life decision)
This seven year old girl had had her head squeezed between another person's body and a staircase after that person had fallen on the stairs. Reportedly, she was GCS 7 ( = severe brain injury according to the Glasgow coma scale), and she arrived sedated and intubated at our department. Computerised tomography revealed an extensive skull fracture system, including bilateral optic canal compression and diffuse brain trauma. Initially, a left temporal impression fracture was lifted and a system for intracranial pressure (ICP) measurements was put in place. The ICP and SSEP were normal by day two. Intradural bilateral optic canal decompression was performed in order to avoid future blindness, and her previously unreactive pupils became reactive thereafter. The girl remained comatose, however, and—two days later—developed significant ICP increases with all signs of brain herniation including unreactive pupils and worsened but yet detectable SSEPs. During a first staff discussion we decided against further surgical measures in the sense of an end of life decision, which was further augmented by the fact that she had developed severe inflammatory abdominal problems in addition. This decision was revised a few hours later in another staff discussion, and bilateral hemicraniectomy ( = skull bone removal for pressure relief) was performed the same night, followed by explorative abdominal surgery. After a very delayed recovery over the next four weeks, which included slow weaning from ventilator support and a period during which she would not respond to verbal stimuli, she ultimately did very well, with no visual field deficits, and returned back to school.
Case 3 (very difficult decision/interdisciplinary ethical consult)
This patient had undergone partial removal of a cerebellar AVM at another institution fifteen years earlier. Meanwhile he developed progressive dementia due to chronic intracranial venous hypertension. The AVM posed a very high surgical risk, and only after extensive discussions with the patient and his family about the pros and cons of such an undertaking, did he vote for removal of this AVM in order to halt the progressive decline of his mental function. The AVM was removed—but intraoperatively significant bleeding was encountered. Intraoperative SSEP monitoring revealed worsening of nerve tract conductivity. Postoperatively, the patient remained in a persistent vegetative state with bilaterally fixed and dilated pupils and absent corneal reflexes and spontaneous breathing—with recovery of his SSEPs derived from his upper extremities, but persisting loss of SSEPs from his lower extremities. Magnetic resonance imaging revealed isolated brainstem infarction, and EEG showed diffuse alterations. He underwent tracheostomy and was transferred to a normal ward. An interdisciplinary ethical consult of the university medical centre took place, in which the patient's relatives took part, in order to decide upon further therapy. An “end of life decision” was made to withhold active therapy should a life threatening situation occur, and he died several weeks later in septic shock with no specific treatment efforts being made.
Discussion
Circumstances of decision making
Many people are afraid that toward the end of their life they will be at the mercy of the kind of medicine which is solely based on technical devices, without due respect being paid to the overall picture and to the humanitarian aspects of the patient's individual dignity. This raises the question as to whether and when to stop treatment in patients who have a grave prognosis with regard to “useful” living or to survival at all—a question which must be answered by the healthcare team and the surrogates of the patient. Neurosurgeons are confronted with situations which may require sudden and profound decisions to be made about patients whose explicit wishes as to possibly life prolonging decisions they do not know, because of the rapid course of the patients' illnesses.4 On the other hand, the attitude toward death and the decision to withhold specific neurosurgical care or to withdraw life support on intensive care units—for example, by withholding or withdrawing vasopressive agents—may be affected not only by medical judgment and moral factors but also by economic constraints and limitation of manpower. Only a few studies have focused on neurological and neurosurgical patients so far, so there is no much information in the literature about this yet.1,5,6,7
In classical medical ethics the physician's responsibility toward the patient is characterised by two fundamental normative components: first, the obligation to carry out all treatment in conformity with the best available clinical knowledge; and, second, the obligation to pay due respect to the patient's informed consent (thus avoiding a purely paternalistic attitude). The first component implies that decisions have to be based on firm clinical grounds. The second component, however, turns out to be more delicate as in neurosurgical emergency situations the patient's informed consent is frequently not available. Under these conditions, written documents indicating treatment directives or designating surrogate decision makers are to be taken as a basis for decision making. If, however, even these documents are unavailable, then the physician must turn to the patient's relatives in order to try to get the best approximation of what the patient would have wanted to be done.
In the present study two different subsets of parameters were studied: patient related ( = medical and social) parameters, and physician related ( = parameters based on individual expertise and preconceived ideas/values), both of which influenced the decisions that were made.
Two results of the present prospective study of 113 patients, in whom active neurosurgical therapy or further life support was withheld, at first sight seemed surprising: first, the rather high number of situations in which the clinicians were forced to make end of life decisions—that is, at a rate of two or three times per week. Second, the fact that two patients survived following revision of the previously made end of life decision.
As opposed to a war situation, where rapid decisions on the fate of numerous victims must be made under high stress, the conditions in a large academic medical centre should allow for sophisticated and thoughtful judgment as to the prognosis of the patients prior to an end of life decision.8 Even in the most stressful situations, these decisions should not be affected by the circumstances under which the patient is being evaluated (for example, less emergent patients pushing to be seen by doctor on call etc). Furthermore, there is a difference in the nature of decision making in the setting we describe from most of the decision making which takes place in the emergency room right after admission: there decisions are being made quickly and in agreement with the other physicians on duty (anaesthesiologist, consultant neurosurgeon, trauma surgeon etc). In contrast, neurosurgical decisions often ought to be based on prolonged observations because clinical evidence concerning the patient's state may be subject to fast and substantial changes. In these cases, the ethical requirement that the physician's decision is based on firm clinical grounds and that substantiated prognosis can only be made on the basis of observation over an adequate period of time.
The two survivors in our group belonged to the majority of patients in whom the end of life decision was based on prolonged observation of the patient, plus additional objective examinations, such as SSEPs, and on open staff discussions, which are an important factor in the decision process.6,7 Obviously, ambiguity may exist among within this group, which may even lead to a wrong end of life decision, and future events—for example, the unexpected survival of the patient, will reveal the decision to have been wrong. The two survivors among our series underscore the need to refrain from making dogmatic statements which are regarded as being beyond contradiction, and the need to be ready to reconsider decisions which may have been made on grounds which may change over time—although this approach may seem unscientific at first sight. The two survivors ultimately benefited from the fact that the clinical staff who took part in the study re‐initiated the discussion about withdrawal of further therapy.
Decision aids
There are precise criteria for the diagnosis of brain death, which are accepted among most physicians worldwide, despite existing cultural differences. The role of SSEPs for the prediction of outcome in comatose patients has been stressed by others.9,10 There is, however, a twilight zone during the course of illness, which is far more difficult to assess by means of critical medical judgment—even at a senior level. Thus it is not possible to “predict with absolute certainty that a patient will not survive...”.11 The fact that many patients do not or do not yet fulfil the criteria for brain death at the time of decision making, underscores the necessity for grounded judgment. Furthermore, and as illustrated by our AVM patient, recovery of SSEPs alone may not imply a quality of life that would meet many people's ideas of a “life worth living”, and the SSEP results must be seen in the overall clinical and social context of the patient. We agree with Levy that these decisions should not be made by the junior house staff alone in the middle of the night and that only thorough training will help minimize the rate of erroneous decisions and ensure that staff have the necessary communication skills to give the patient's relatives the confidence that the best is being done for the patient.12,13 In addition to that, and whenever possible, the conjectural will of the patient must be respected during the process of decision making. Evidence for the conjectural will of the patient can be derived from written documents stating the patient's preferences concerning certain situations of health, disablement, consciousness etc. It should be mentioned here that such written documents or written wills are not legally binding on the physician and that, moreover, observing the wishes the patient has expressed in them is not always clinically justified. A less reliable source for ascertaining the patient's will are corresponding testimonies provided by the patient's relatives and, finally, some general assumptions on people's wishes and preferences with respect to situations of emergency and the restoration of imperfect health.
Diringer et al have provided the largest study of the withdrawal of ventilator support on a combined neurological/neurosurgical ICU, with 284 patients out of a total of 2109 non‐selective admissions on that ICU over a period of 82 months. They found a clear correlation between the severity of the neurological insult and the decision to withhold further treatment. Furthermore they found older age to make withdrawal more likely as well. As with their study, we did not take into account the religious or cultural background of the patients.
The context of decision making
Clear decisions can and should be made on the basis of straight and thoughtful communication between the senior staff member on call and the residents on duty. It must be ensured that these decisions do not rely solely on telephone communications with primary care hospitals. Costly patient transfer for neurosurgical examination should be avoided only if digital image transmission allows for sufficient analysis and if on site examination by non‐neurosurgeons allows for clear statements regarding pupillary status and Glasgow Coma Status (GCS). Difficult decisions require more extensive discussions among the staff. They should not be dogmatic and should be further augmented by electrophysiological examinations and neuroimaging. Very difficult decisions occur rarely enough to allow time to call together the local ethics committee.
It has to be kept in mind that our experience should be seen in the context of our own legal and societal, and professional framework: The opinion of leading German physicians' associations is against active and legalised “medicide” even in extreme situations, because this might ultimately lead toward active killings in widely differing situations and to societal and personal pressure on the very ill. Indirect medicide—for example, the use of drugs which are known to reduce the remaining lifetime, and passive medicide—for example, refraining from life prolonging measures in terminally ill patients, are legally allowed, if the documented will of the patient is respected. The current legal situation in Germany leaves a twilight zone, where decisions may go in one or the other direction.
Conclusion
As we found neurosurgeons involved in end of life situations almost every second day we think that a small grain of uncertainty will always remain with the resulting decisions. Such decisions are made under pressure of time as well as under increasing constraints in the areas of manpower and budget. The data show that if time is taken for difficult decisions, outcome may be affected positively, which should encourage ethical training for clinicians. Furthermore, thorough clinical training and vigorous performance of neurological examinations in conjunction with electrophysiological testing plus respect for factors which are not derived from sole medical parameters, such as the patient's will and dignity, may help. The decision process should be kept as transparent as possible in these situations, which exert the greatest professional and emotional stress on the physicians as well as on the patient's relatives. It must also be borne in mind that the patient and the relatives may come from a different cultural background from that of the clinical staff, and any implications arising from this must be taken into consideration.3,14,15
Acknowledgements
The authors are indebted to Dietmar Hübner, PhD, and Thomas Heinemann, MD, of the Institute of Science and Ethics, University of Bonn, for very helpful comments.
Abbreviations
AVM - arteriovenous malformation
ICP - intracranial pressure
SSEP - somatosensory evoked potential
TBI - traumatic brain injury
Footnotes
Ethics approval: As this was a sole observational study, we did not apply for a statement by the respective ethics committee initially. We have done that post hoc, however, and presented the study outline and the results to the local ethics committee of the University of Bonn, which found no objections against it (letter 271/04, dated 01/20/05).
References
- 1.Diringer M N, Edwards D F, Aiyagari V.et al Factors associated with withdrawal of mechanical ventilation in a neurology/neurosurgery intensive care unit. Crit Care Med 2001291792–1797. [DOI] [PubMed] [Google Scholar]
- 2.Sittisombut S, Love E J, Sitthi‐Amorn C. Cardiopulmonary resuscitation performed in patients with terminal illness in Chiang Mai University Hospital, Thailand. Int J Epidemiol 200130896–898. [DOI] [PubMed] [Google Scholar]
- 3.Vincent J L. Cultural differences in end of life care. Crit Care Med 200129(2suppl)52–5N. [DOI] [PubMed] [Google Scholar]
- 4.Clusmann H, Schaller C, Schramm J. Fixed and dilated pupils after trauma, stroke, and previous intracranial surgery: management and outcome. J Neurol Neurosurg Psychiatry 200171175–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashkan K, Edwards R J, Bell B A. Crisis in resources: a neurosurgical prospective. Br J Neurosurg 200115342–346. [DOI] [PubMed] [Google Scholar]
- 6.Barlow P, Jennett B. Decisions to limit treatment in a neurosurgical unit: an aspect of audit of mortality. Scott Med J 199136109–111. [DOI] [PubMed] [Google Scholar]
- 7.Fitzpatrick M O, Goyal K, Barlow P. Treatment limiting decisions in a neurosurgical unit. Scott Med J 19994447–48. [DOI] [PubMed] [Google Scholar]
- 8.Kelly P J. Vietnam, 1968–1969: a place and a year like no other. Neurosurgery. 2003;52: 927–39, 939–943, [DOI] [PubMed]
- 9.Zentner J, Rohde V. SEP and MEP in comatose patients. Neurol Res 19941689–92. [DOI] [PubMed] [Google Scholar]
- 10.Christophis P. The prognostic value of somatosensory evoked potentials in traumatic primary and secondary brainstem lesions. Zentralbl Neurochir 20046525–31. [DOI] [PubMed] [Google Scholar]
- 11.Nyman D J, Sprung C L. End of life decision making in the intensive care unit. Intensive Care Med 2000261414–1420. [DOI] [PubMed] [Google Scholar]
- 12.Agich G J, Arroliga A C. Appropriate use of DNR orders: a practical approach. Cleve Clin J Med. 2000;67: 392, 395, 399–400, [DOI] [PubMed]
- 13.Levy M M. End of life care in the intensive care unit: can we do better? Crit Care Med 200129(2 suppl)56–61N. [DOI] [PubMed] [Google Scholar]
- 14.Prendergast T J, Puntillo K A. Withdrawal of life support: intensive caring at the end of life. JAMA 20022882732–2740. [DOI] [PubMed] [Google Scholar]
- 15.Tschann J M, Kaufman S R, Micco G P. Family involvement in end of life hospital care. J Am Geriatr Soc 200351835–840. [DOI] [PubMed] [Google Scholar]