Abstract
Aim
To improve clinical and ethical understanding of patient preferences for information and involvement in decision making.
Objectives
To develop and evaluate a clinical tool to elicit these preferences and to consider the ethical issues raised.
Design
A before and after study.
Setting
Three UK hospices.
Participants
Patients with advanced life‐threatening illnesses and their doctors.
Intervention
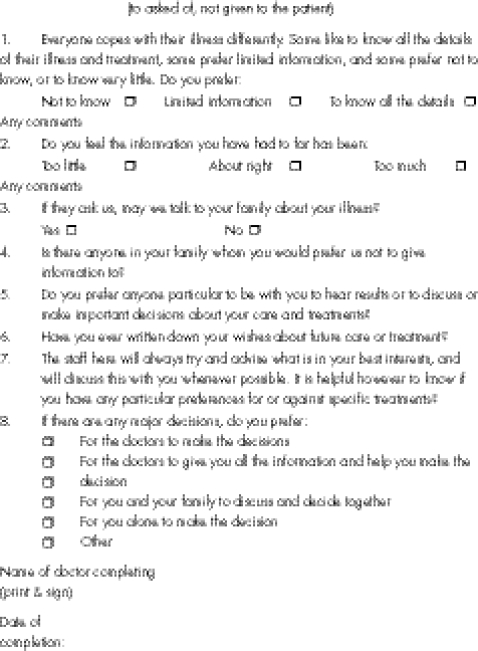
Questionnaire on information and decision‐making preferences.
Main outcome measures
Patient‐based outcome measures were satisfaction with the amount of information given, with the way information was given, with family or carer information, and confidence about future decision making. Doctor‐based outcome measures were confidence in matching information to patient preference, matching family or carer communication to patient preference, knowing patient preferences and matching future decision making with patient preference.
Results
Of 336 admissions, 101 patients (mean age 67.3 years, 47.5% men) completed the study (control, n = 40; intervention, n = 61). Patient satisfaction with the way information was given (χ2 = 6.38, df = 2, p = 0.041) and family communication (χ2 = 14.65, df = 2, p<0.001) improved after introduction of the tool. Doctor confidence improved across all outcome measures (all p values<0.001).
Conclusions
Patient satisfaction and doctor confidence were improved by administering the questionnaire, but complex ethical issues were raised by implementing and applying this research. The balance of ethical considerations were changed by advanced life‐threatening illness, because there is increased risk of harm through delivery of information discordant with the patient's own preferences. The importance of truly understanding patient preferences towards the end of life is highlighted by this study.
Increasing patient autonomy and promoting patient choice is currently high on the social and political agenda in the UK, countering the more “paternalistic” approach to healthcare in the past. Many patients with cancer want wider, more detailed information about their illness and its management options than they currently receive;1,2,3 they also expect greater participation in decisions about their care.4 In palliative care, this raises particularly complex ethical issues. It cannot be assumed that more information will result in increased autonomy and greater choice without associated costs. Information and decision making, especially on treatment and future planning, may well include “bad news” and so be harmful if the amount of information or speed of delivery goes beyond what is acceptable to the patient at that time.
We believe an essential step in the process of giving information and facilitating decisions is to discover a patient's current preferences for information and for involvement in decisions. The literature supports this approach, showing that information poorly matched to preferences is more likely to be unhelpful or even positively harmful.3,5,6 Without this step of eliciting preferences, judgements on the balance of benefit and harm and on facilitating autonomy are limited.
Eliciting preferences in clinical practice is difficult. Considerable evidence exists of inadequate communication between healthcare professionals and patients or carers7,8 and inadequate understanding of preferences.9 Limitations of time, skill and confidence in communication, and lack of prior knowledge of the patient, are all obstacles to this process.4 Ways of enhancing information giving to patients with cancer have been explored.3,5,7,10 Several tools exploring patient preferences have been developed for use in research,11,12 but there are few clinical tools.13 This paper reports the development and evaluation of a clinical questionnaire to facilitate the process of eliciting patient preferences on information and decisions, and explores the ethical issues that arise in formulating, conducting and applying this research.
Methods
Questionnaire development
The questionnaire was adapted from that used by Sayers and colleagues13 (see appendix).
Participants and setting
The study population included all patients admitted to three hospices (total 56 beds) in southeast England over 4 months. (The duration of the study was set to recruit adequate numbers based on a sample size calculation, known admission rates and estimated 50% attrition.) Exclusion criteria were the following: Abbreviated Mental Test Score <7,14 inability to sustain a conversation for more than 10 min, extreme psychological distress or previous participation. Ethical approval was obtained before the study began.
Data collection
This prospective study adopted a “before and after” design. Administration of the questionnaire constituted the intervention, introduced halfway through the study period, giving rise to a control group (before introduction of the questionnaire) and an intervention group (after introduction of the questionnaire). Randomisation and concurrent control or intervention groups were not feasible, given the small size of the hospice inpatient units, and the problems with contamination that this raised. Consent was obtained from all participants. Evaluation was carried out by patient–doctor interviews 3–14 days after each admission. Patient‐based outcomes were measured using simple categorical “yes”, “no” or “don't know” answers as many of the patients were too ill for more complex inquiry:
Satisfaction with the amount of information
Satisfaction with the way information had been given
Satisfaction with information given to the family or carer
Confidence about future decision making, matching their preferences.
Doctor‐based outcome measures were measured using 10‐cm unmarked visual analogue scales:
Confidence in matching information to patient preference for information
Confidence in matching communication with family or carer patient preference
Confidence in knowing patient preference for involvement in decision making
Confidence in matching future decision making with patient preference.
Analysis
Data were statistically analysed by using χ2 and Mann–Whitney U tests, as appropriate to data type. Care was taken to establish whether distress was caused by the tool (through direct questions within the doctor interviews).
Results
Recruitment and attrition
Table 1 shows the recruitment of and attrition in patients admitted during the study period. Few patients refused consent. Attrition was high, with 64 patients (37% of those fulfilling the inclusion criteria) unable to complete the study because of deterioration or death. Attrition was similar in the control and intervention groups (29 and 35 patients, respectively, unable to complete the study) and the overall response rate was 55.5%. The required sample size was exceeded.
Table 1 Recruitment of and attrition in patients admitted during the study period.
| Patients admitted to hospices during study period, n = 336 | |||
|---|---|---|---|
| Admitted during “before” phase | Admitted during “after” phase | ||
| 159 | 177 | ||
| Fulfilling inclusion criteria | Excluded | Fulfilling inclusion criteria | Excluded |
| 99 | 60 | 83 | 94 |
| Entered study | Declined consent | Entered study | Declined consent |
| 90 | 9 | 81 | 2 |
| Completed study | Too ill, died or discharged before completion | Completed study | Too ill, died or discharged before completion |
| 61 | 29 | 46 | 35 |
| Final data | Missing data | Final data | Missing data |
| 61 | 0 | 40 | 6 |
Demographic data
We found no statistically significant differences in age, sex or diagnoses between the control and intervention groups, or between the study and denominator populations. Only one patient (1% of the study population) with non‐malignant disease was included.
Findings and analysis of outcome measures.
Tables 2 and 3 show the findings and analysis of outcome measures.
Table 2 Patient outcome measures in control and intervention groups.
| Outcome measure | Control group, n = 61 (% of control group) | Intervention group, n = 40 (% of intervention group) | Statistical analysis (the answers “No” and “Don't know” were combined for analysis) |
|---|---|---|---|
| Has the amount of information been as you wanted? | |||
| Yes | 45 (73.8) | 35 (87.5) | χ2 = 2.898 df = 2 p = 0.235 |
| No | 14 (22.9) | 4 (10.0) | |
| Don't know | 2 (3.3) | 1 (2.5) | |
| Has the information been given in the way you wanted? | |||
| Yes | 49 (80.3) | 39 (97.5) | χ2 = 6.379 df = 2 p = 0.041 (Fisher's exact text used because of small numbers) |
| No | 11 (18.0) | 1 (2.5) | |
| Don't know | 1 (1.6) | 0 (0.0) | |
| Do you feel your family or carer has been kept informed as you wished? | |||
| Yes | 37 (60.7) | 37 (92.5) | χ2 = 14.649 df = 2 p<0.001 |
| No | 21 (34.4) | 1 (2.5) | |
| Don't know | 3 (4.9) | 2 (5.0) | |
| Are you confident that future decisions about your care will be made in the way you wish? | |||
| Yes | 44 (72.1) | 35 (87.5) | χ2 = 4.591 df = 2 p = 0.101 |
| No | 9 (14.8) | 1 (2.5) | |
| Don't know | 8 (13.1) | 4 (10.0) | |
Table 3 Doctor outcome measures in control and intervention groups.
| Outcome measure confidence in: | Mean (SD) VAS (in control group n = 75*) | Mean (SD) VAS (in intervention group n = 52*) | Mann–Whitney U test† |
|---|---|---|---|
| Matching information to patient preference | 7.24 (2.18) | 8.56 (1.79) | 1198.50 |
| p<0.001 | |||
| Matching family communication to patient preference | 7.14 (2.76) | 9.06 (1.11) | 1109.00 |
| p<0.001 | |||
| Knowing patient preference for involvement in decisions | 7.28 (2.34) | 8.31 (SD 2.07) | 1438.00 |
| p = 0.014 | |||
| Matching future decisions to patient preference | 6.65 (2.68) | 8.00 (2.31) | 1305.00 |
| p = 0.004 |
VAS, Visual Analogue Scores 1–10, 0, not at all confident; 10, very confident.
*Numbers larger than for patient outcome measures because doctor interviews were completed even when patients had become too ill to complete the study.
†This compares difference between VAS of the control and intervention groups and not just difference between mean VAS, although mean VAS are reported here for reasons of space.
Patient satisfaction with the way information was given, and with giving information to the family, both showed significant improvement after introduction of the questionnaire, achieving significance at the 5% level. All of the doctor‐based outcome measures showed highly significant improvement after introduction of the questionnaire. Doctors reported that only two patients were distressed during the questions of the history tool; this was related to hospice admission and questions of disease progression, rather than to the questionnaire itself.
Preferences elicited using the questionnaire
Table 4 shows the preferences elicited using the questionnaire.
Table 4 Preferences elicited using the tool (intervention group only; n = 75).
| Response | n (%) | |
|---|---|---|
| Preferences for information about the illness and treatment | Preferred not to know | 2 (2.7) |
| Preferred limited information | 21 (28.0) | |
| Preferred to know all the details | 52 (69.3) | |
| Previous experience of information about the illness | Too little | 14 (18.7) |
| About right | 61 (81.3) | |
| Too much | 0 (0.0) | |
| Preference for family/carer information | Yes, may discuss | 71 (94.7) |
| No, prefer not | 4 (5.3) | |
| Specific family members not to be given information | Named | 12 (16.0) |
| None named | 63 (84.0) | |
| Specific family members to be present for information | Named | 46 (61.3) |
| None named | 29 (38.7) | |
| Advance directive or living will | Already made | 7 (9.3) |
| Wanted to make | 1 (1.3) | |
| Not wanted | 43 (57.4) | |
| Not asked | 24 (32.0) | |
| Decision‐making preferences | Doctors to decide | 13 (17.3) |
| Combined decision | 27 (36.0) | |
| Self or family to decide | 9 (12.0) | |
| Other preference | 11 (14.7) | |
| Not asked | 15 (20.0) |
*Numbers are larger than for the intervention group (where n = 40) because 35 patients had the tool administered but subsequently became too ill to complete the study.
Much of the value of the tool arose from the discussions on the preferences it initiated rather than just the specific answers produced. In all 61 (81.3%) patients were satisfied with information already received, 2 (2.7%) preferred not to know future details, 52 (69.3%) expressed a preference for full information and 21 (28.0%) chose more limited information. Of the 75 patients, 46 (61.3%) named specific family members they wished to be present during future information giving and 12 (16.0%) identified family members to whom they preferred information not to be given. Although only 1 (1.3%) patient stated a preference to make an advance directive, 12 (16.0%) patients did go on to give clear statements about their future preferences, which were then documented. Two advance directives were newly uncovered.
Discussion
The tool made a clear contribution to recognising the limits of patient confidentiality and ensuring that discussions with relatives or friends matched patient preferences. It also facilitated identification of pre‐existing advance statements. It highlighted preferences for information and decision making and appeared to improve patient satisfaction, but the clinical and ethical relevance of these findings needs further consideration.
All healthcare professionals should aim for fully informed patients and maximal respect for autonomy. There is a legal requirement for consent to interventions, no matter how trivial, which requires patient involvement and information giving. On this basis, the rationale for eliciting preferences for information and involvement in decisions could be questioned. Should palliative professionals elicit these preferences at all, or do the requirements of consent imply that patients be fully informed, whatever the patient's preferences for information? This question is highly relevant to palliative care where giving too much information too quickly has great potential for harm. Patients who deal with their advancing illness and poor prognosis by denial of the reality of their situation are not uncommon. But many more patients deal with often heart‐breaking information at a level and pace they can manage, developing limited or gradual realisation of the full implications of their illness. Inflicting open discussions in either of these situations inappropriately can clearly cause harm, and is usually ethically indefensible.
Although it is accepted that competent patients must give consent (certainly for specific interventions) and that they must be informed for that consent to be valid, in clinical practice, interventions vary widely in extent and consequence. Consent is more than the formality of passing on information and responsibility for a decision. Especially at the end of life, consent can be a complex, even ambiguous process, rather than a simple event.15 How much information a patient should be given is unclear. For example, the Bristol Inquiry16,17 found that:
the issue is no longer whether to inform a patient, but how to do so effectively…We believe that healthcare professionals have a duty to empower patients; providing information is one means of empowerment. We accept that each patient is different and may wish for varying amounts of information at various times, with the constant ability to say “enough”. But this fact does not serve as a reason for not setting out on the information journey.
In the palliative context, the need for consent may range from agreement to hospice admission, to provision of daily care, to complex decisions on palliative surgery or chemotherapy. The balance between respecting autonomy and causing harm will vary according to the importance and implications of the decision at hand. In addition, there may be wide variation in the time relationship between decisions on interventions and the consequences of those decisions. Unless issues such as preference for a home death are assessed early, any opportunity for appropriate advanced planning is lost and dying at home becomes impossible.
We would reason that balancing the clinical and ethical demands cannot be achieved without first understanding the patient's preferences. Preferences for full information and involvement indicate openness and readiness to discuss, and harm from discussion is likely to be much reduced. Preferences “not to know” suggest a potentially high risk of harm from imposing too much information on the patient too quickly. This requires skilled and sensitive judgements from professionals, and there is an urgent clinical need for tools to help this difficult process. This research evaluates one way to help explore preferences, so that the health professional better understands what level of informed consent is achievable and how choices may best be facilitated.
Providing full information and involvement to a patient who expresses a preference for an open approach should be straightforward so long as appropriate communication skills are used. A dilemma arises of how a healthcare professional should act when patients prefer limited information. Although good practice requires that patient preferences should be revisited regularly, we would reason that the major ethical defence to denying this preference is where an intervention is being considered that may make a substantial difference to outcome or well‐being. As the patient approaches the end of life, it generally becomes harder to argue for such a substantial difference. In non‐palliative settings, this may not be the case and the balance of ethical considerations will be different.
The patient responses elicited by the tool concur with much research already undertaken in people with cancer, but key differences may prove ethically and clinically important. The proportion of patients satisfied with information given so far is high. The proportion who prefer not to have information is almost identical to the 1.9% noted by Jenkins et al.1 Only 69% of patients, however, preferred as much information as possible, which was less than the 87% described by Jenkins et al1 and the 79% described by Meredith et al,18 both studies on people with cancer. Our study population was at a more advanced stage of illness, and as the illness advances and death approaches, patients may prefer less detailed information. A longitudinal study of patient preferences for information is needed to explore this more fully.
Another important point for practice is the numbers of patients expressing specific preferences about family communication. Palliative care gives prominence to the role of families, both providing family support and recognising their care‐giving role.19 Given the potential conflicts that may arise between patients and families, and given that patient capacity often becomes increasingly impaired towards death, we believe it is important for professionals to be informed early about patient preferences. This facilitates the professionals in fulfilling their primary duty of care to the patient, whenever differences between patient and family arise. This is not an infrequent issue; moderate or severe problems in communication between patient and family are reported in 30–40% of patients with cancer at the end of life.20
Further ethical issues arose in the design and implementation of the study. We did not use the more rigorous randomised controlled trial because of anticipated difficulties with contamination and the related ethical challenges of randomising such an intervention. Delivery of the intervention by the admitting doctors would probably contaminate their approach to patients in the control group, thus blurring the distinction between intervention and control. Randomisation raised the possibility of delivering inequitable care to patients directly alongside each other, which, although not ethically different from the “before and after” design (where preference exploration was offered to the “after” group, but not to the “before” group), would have been more clinically challenging for both patients and professionals. Such difficulties have already been well described in palliative care,21,22 although often with stronger arguments for inequity because of the greater importance of the intervention.23 As a result of this, and related issues, randomised controlled trials are infrequent. Alternative designs bring greater possibility of bias. The short duration of this study (4 months) minimised the largest source of bias (due to change over time) expected in a before and after design.
Patient‐based evaluation is limited, partly because of the constraints of research with patients who are very ill, but also because of the use of satisfaction alone as an outcome measure. The value of satisfaction as an outcome measure is controversial. Satisfaction depends on a number of variables, including a patient's expectations, previous experiences and attitude to and openness about the illness, professional skill and experience in communication and factors relating to continuity and subsequent teamwork.4,7,24,25 For example, patients with low expectations are likely to be more readily satisfied whatever the realities of their actual care. We recognise the severe limitations of satisfaction as an outcome measure in this context, but would suggest that other outcome measures, such as the patient's psychological well‐being, the quality of family relations and family well‐being are more onerous for these ill patients and are hard to attribute to single specific interventions, such as this questionnaire.
The best way to assess satisfaction is also debatable.26 In this study, direct questions were used. This approach had the advantage of simplicity and ease of response for a study population of patients who were very ill. This reduced the research burden and attrition, but confined the response to a single aspect of satisfaction predetermined by the researcher rather than exploring indirectly the multidimensional nature, which some reason goes to make up the complexity of satisfaction.26
Respecting autonomy provides a challenge in palliative care because of doubts about capacity, varying degrees of denial and collusion, and the distress of emotionally difficult news for the patient. Establishing preferences enables us to show respect for patient autonomy in a manner that is sensitive and timely for that patient. A demand for full respect for autonomy for all leaves a cost for those who are more vulnerable and do not want this. A relationship of mutual trust is suggested as an improved approach.27 Patients need a sensitive, compassionate and skilled approach, which respects their autonomy, while understanding something of the complex interplay between preferences, reasoning and emotion in the face of advanced disease and imminent death. Capturing such complexity while achieving realistic research goals and working with people who are ill remains a challenge in palliative care research of all types.
Conclusions
Eliciting patient preferences for information and for involvement in decisions towards the end of life is a major clinical challenge and raises important ethical issues. This study introduces a new clinical tool that has the potential to facilitate this process; it does not increase patient distress and improves both patient satisfaction and doctor confidence in the palliative care setting. It may be most valuable as a way of initiating dialogue and as a prompt for documentation and interdisciplinary communication. Eliciting preferences is, however, a dynamic process, and on‐going dialogue and a review of preferences is paramount.
By implementing this research and applying its findings in the palliative care context we raise key ethical issues. The presence of an advanced and life‐threatening illness changes the balance of ethical considerations, as the possibility of harm through delivery of information discordant with the patient's own preferences increases, and this highlights the critical importance of truly understanding patient preferences and working with them towards the end of life.
Acknowledgements
This study was completed towards an MSc in Palliative Care at Kings College London. We thank the patients who willingly contributed and the staff in all three hospices. We also thank Dr Polly Edmonds, Professor Irene Higginson and Jonathan Koffman for their support.
Appendix
Questionnaire
References
- 1.Jenkins V, Fallowfield L, Saul J. Information needs of patients with cancer: results from a large study in UK cancer centres. Br J Cancer 20018448–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fallowfield L, Ford S, Lewis S. No news is not good news: information preferences of patients with cancer. Psychooncology 19954197–202. [DOI] [PubMed] [Google Scholar]
- 3.NHS Centre for Reviews and Dissemination Informing, communicating and sharing decisions with people who have cancer. Effect Health Care 200061–8. [Google Scholar]
- 4.Say R E, Thomson R. The importance of patient preferences in treatment decisions‐‐challenges for doctors. BMJ 2003327542–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McPherson C J, Higginson I J, Hearn J. Effective methods of giving information in cancer: a systematic literature review of randomized controlled trials. J Public Health Med 200123227–234. [DOI] [PubMed] [Google Scholar]
- 6.Harris K A. The informational needs of patients with cancer and their families. Cancer Pract 1998639–46. [DOI] [PubMed] [Google Scholar]
- 7.National Institute for Clinical Excellence Improving supportive and palliative care for adults with cancer. London: National Institute for Clinical Excellence, 2004
- 8.Baggs J G. End‐of‐life care for older adults in ICUs. Annu Rev Nurs Res 200220181–229. [PubMed] [Google Scholar]
- 9.Greipp M E. SUPPORT study results ‐‐ implications for hospice care. Am J Hospice Palliat Care 19961338–45. [DOI] [PubMed] [Google Scholar]
- 10.Walsh R A, Girgis A, Sanson‐Fisher R W. Breaking bad news. 2: what evidence is available to guide clinicians. Behav Med 19982461–72. [DOI] [PubMed] [Google Scholar]
- 11.Rothenbacher D, Lutz M P, Porzsolt F. Treatment decisions in palliative cancer care: patients' preferences for involvement and doctors' knowledge about it. Eur J Cancer 1997331184–1189. [DOI] [PubMed] [Google Scholar]
- 12.Gauthier D M, Froman R D. Preferences for care near the end of life: scale development and validation. Res Nurs Health 200124298–306. [DOI] [PubMed] [Google Scholar]
- 13.Sayers G M, Barratt D, Gothard C.et al The value of taking an ‘ethics history'. J Med Ethics 200127114–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hodkinson H M. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing 19721233–238. [DOI] [PubMed] [Google Scholar]
- 15.Alderson P, Goodey C. Theories of consent. BMJ 19983171313–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mayberry M K, Mayberry J F.Bristol Royal Infirmary Inquiry: final report. The inquiry into the management of care of children receiving complex heart surgery at the Bristol Royal Infirmary. Bristol: Bristol Royal Infirmary Inquiry, 2001, 287. (Command Paper CM 5207. )
- 17.Mayberry M K, Mayberry J F. Consent with understanding: a movement towards informed decisions. Clin Med 20022523–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meredith C, Symonds P, Webster L.et al Information needs of cancer patients in west Scotland: cross sectional survey of patients' views. BMJ 1996313724–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization Definition of palliative care. 2002. http// www.who.int/cancer/palliative/definition/en (accessed 16 Jun 2005)
- 20.Higginson I J, Constantini M. Communication in end‐of‐life cancer care: a comparison of team assessments in three European countries. J Clin Oncol 2002203674–3682. [DOI] [PubMed] [Google Scholar]
- 21.Kaasa S, De Conno F. Palliative care research. Eur J Cancer 200137(Suppl 8)S153–S159. [DOI] [PubMed] [Google Scholar]
- 22.Jordhoy M S, Kaasa S, Fayers P.et al Challenges in palliative care research; recruitment, attrition and compliance: experience from a randomized controlled trial. Palliat Med 199913299–310. [DOI] [PubMed] [Google Scholar]
- 23.McWhinney I R, Bass M J, Donner A. Evaluation of a palliative care service: problems and pitfalls. BMJ 19943091340–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marwit S J, Datson S L. Disclosure preferences about terminal illness: an examination of decision‐related factors. Death Stud 2002261–20. [DOI] [PubMed] [Google Scholar]
- 25.Murray M, Miller T, Fiset V. Decision support: helping patients and families to find a balance at the end of life. Int J Palliat Nurs 200410270–277. [DOI] [PubMed] [Google Scholar]
- 26.Aspinal F, Addington‐Hall J, Hughes R.et al Using satisfaction to measure the quality of palliative care: a review of the literature. J Adv Nurs 200342324–339. [DOI] [PubMed] [Google Scholar]
- 27.Boyd K. Deciding about resuscitation. J Med Ethics 200127291–294. [DOI] [PMC free article] [PubMed] [Google Scholar]