Abstract
Objective
To classify poisoning deaths of undetermined intent as either suicide or unintentional and to estimate the extent of underreported poisoning suicides.
Methods
Based on 2002 statewide death certificate and medical examiner data in Utah, the authors randomly selected one half of undetermined and unintentional poisoning deaths for data abstraction and included all suicides. Bivariate analyses assessed differences in demographics, death characteristics, forensic toxicology results, mental health history, and other potentially contributing factors. Classification and regression tree (CART) analysis used information from unintentional and suicide poisoning deaths to create a classification tree that was applied to undetermined poisoning deaths.
Results
The authors analyzed 41 unintentional, 87 suicide, and 84 undetermined poisonings. Undetermined and unintentional decedents were similar in the presence of opiates, physical health problems, and drug abuse. Although none of the undetermined decedents left a suicide note, previous attempt or intent to commit suicide was reported for 11 (13%) of these cases. CART analysis identified suicidal behavior, drug abuse, physical health problems, depressed mood, and age as discriminating between suicide and unintentional poisoning. It is estimated that suicide rates related to poisoning are underreported by approximately 30% and overall suicide rates by 10%. Unintentional poisoning death rates were underreported by 61%.
Conclusions
This study suggests that manner of death determination relies on circumstance dependent variables that may not be consistently captured by medical examiners. Underreporting of suicide rates has important implications in policy development, research funding, and evaluation of prevention programs.
Keywords: suicide surveillance, poisoning, undetermined deaths, classification, coroners and medical examiners
Official suicide rates are used to monitor trends, compare suicide rates across regions, and assess risk factors.1,2 However, these statistics are not valid if any proportion of deaths for which intent cannot be determined (referred to as “undetermined deaths”) are in fact self‐inflicted (suicide). Several studies have shown that a proportion of undetermined deaths are likely unreported suicides, and suggest that reported suicide rates underestimate the true rate by 10–30%.1,3,4,5,6,7 Determination of intent is especially difficult in the case of ingested poisoning deaths.3,5,8,9,10 Poisoning deaths account for over two thirds of all undetermined deaths nationally.11
According to 2002 National Vital Record data, Utah has the fourth highest rate of undetermined deaths (7.3 per 100 000 person‐years), over four times the national rate.11 Nearly all (95%) of undetermined deaths in Utah are the result of poisoning. The objective of this study was to classify poisoning deaths of undetermined intent as either suicide or unintentional and to estimate the extent of underreported suicides from poisoning. As a related objective, we sought to characterize undetermined poisoning deaths in Utah and descriptively compare them to suicide and unintentional poisoning deaths.
Methods
Data sources
The National Violent Death Reporting System (NVDRS) was developed by the Centers for Disease Control and Prevention and launched in 2003 to collect and analyze data from violence related deaths.12 The Harvard School of Public Health and collaborating institutions in 11 states and metropolitan areas launched the pilot study for this program in 2000, the National Violent Injury Statistics System (NVISS).13 As part of Utah's participation in NVISS, we abstracted data for all poisoning deaths certified as suicide in Utah during 2002 (n = 87). We then randomly selected approximately one half of the 85 unintentional and 168 undetermined poisoning deaths occurring in 2002 for data abstraction and inclusion in the study. Poisoning deaths of all intents were identified based on International Classification of Disease (10th Revision) codes reported in Utah death certificate data. The ranges used were as follows: suicide poisoning, X60 to X69; unintentional poisoning, X40 to X49; and undetermined poisoning, Y10 to Y19. All unintentional and undetermined death records were abstracted in the same manner as suicide records using standard NVISS definitions and methods. Death certificates provided decedents' demographic data. Medical examiner reports provided more detailed information on circumstances, toxicology, and mental health history. Because Utah has a centralized medical examiner system, these reports were easily accessed from a central location for death investigations occurring anywhere in the state.
The NVISS data collection form was designed to capture data for violence related deaths based primarily on information from toxicology reports, narratives, and other evidence collected through the medical examiner or coroner's investigation. Abstractors were trained using standard forms and definitions. Toxicology reports provided data on drugs tested. Information on mental health history and potentially contributing circumstances were captured through the medical examiner's narrative. These narratives are unstructured and rarely include information regarding circumstances not present—for example, if the investigation determined that the decedent had no known history of mental health problems. As a result, circumstances were coded as present or not present/unknown.
This study was approved by the University of Utah Institutional Review Board in Salt Lake City, Utah.
Study variables
As described above, manner or intent of death was classified as either suicide (self‐inflicted), unintentional, or undetermined. For convenience, we refer to decedents who died from self‐inflicted poisoning as suicide decedents, those who died from unintentional poisoning as unintentional decedents, and those who died from poisoning of undetermined intent as undetermined decedents.
The variables included in the analysis were: age, sex, race, education (<high school (HS), HS, >HS), currently employed, injury occurred at residence, any medical contact in the interval between administration of the poison and death (emergency medical services, emergency department, or inpatient admission), primary poisoning agent(s) resulting in death, the presence or absence (based on toxicology results) of alcohol, antidepressants, street drugs (cocaine, amphetamines, and marijuana), opiates, and other drugs, depressed mood at the time of the incident, any mental health problem or diagnosis, mental health treatment (current or past), alcohol or other substance abuse problem, alcohol or drug abuse treatment, suicidal behavior (considered positive if decedent left a suicide note, declared intent to commit suicide, or had previously attempted suicide), same day or recent crisis in decedent's life, physical health problem, and the presence of one or more other contributing factors. Examining the presence of a suicide note separately from declared intent or previous attempt to commit suicide did not add to the analysis, and these behaviors were combined.
Statistical analysis
Counts and percentages were tabulated by medical examiner's assessment of intent for demographic information, circumstances related to the death, forensic toxicology results, mental health and drug abuse history, and other potentially contributing factors. We used χ2 tests to assess differences in categorical variables and analysis of variance to assess differences in mean age. The primary poisoning agent was only summarized descriptively due to small sample sizes across groups and was classified as pharmacy prescription versus other for the classification tree analysis. Drugs tested were reported as present, not present, or not tested. Mental health history and potentially contributing circumstances were classified as either present or not present/unknown.
Classification and regression tree (CART) analysis used the available information to create a classification rule, or decision tree, to determine whether a poisoning death was unintentional or suicide. In this method, predictor variables are partitioned recursively into the two subgroups that are most different with respect to the outcome.14 The final result is a decision tree that accurately classifies as many cases as possible without overfitting the data. When the goal is to correctly classify an outcome, CART is preferable to traditional statistical methods, such as logistic regression, because it deals well with a large number of predictor variables, allows missing data, and requires no assumptions regarding the underlying distribution of the predictor variables.14,15 Our primary reasons for using CART were to identify key predictors in determining intent of death and to obtain an estimate of the number of undetermined deaths that could be classified as suicide. Due to a limited sample size, our application of this technique was not intended to provide a decision rule that can be widely applied to other datasets.
We applied CART analysis to all cases for which the intent of poisoning was known (unintentional and suicide). We then applied the resulting classification algorithm to the undetermined poisoning deaths. Because our sample size was relatively small, we used an additional classification method—random forests—to evaluate the stability of the CART results. This method is an extension of CART that provides accurate and robust classification of an outcome.16,17
Descriptive and bivariate analyses were conducted in SAS version 9 (SAS Institute Inc, NC, USA). CART and random forests analyses were conducted in R version 2.1.
Results
There were 41 unintentional injury poisonings, 87 suicide poisonings, and 84 undetermined poisonings included in this study. Table 1 presents the demographic characteristics and table 2 provides information on the primary poisoning agent(s) used. The average age among decedents whose deaths were coded as undetermined was 38 years, slightly younger than both the unintentional and suicide decedents. Undetermined and unintentional decedents were also more likely than suicide decedents to be male. Medical contact subsequent to poisoning and before death was less likely for suicide decedents than for others. General poisoning characteristics were similar for all three groups, with over three fourths of all deaths occurring at the decedents' homes, and most deaths involving prescription medications. However, the poisoning agent for non‐prescription poisoning deaths was primarily illicit drugs for unintentional and undetermined deaths and primarily carbon monoxide for suicides.
Table 1 Demographic and death characteristics of poisoning decedents by intent in Utah, 2002.
| Unintentional (n = 41) | Suicide (n = 87) | Undetermined (n = 84) | p Value§ | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Age | 41 years | 10.0 | 43 years | 14.4 | 38 years | 10.1 | 0.03 |
| n | % | n | % | n | % | p Value§ | |
| Male | 28 | 68% | 41 | 47% | 56 | 67% | 0.01 |
| White* | 41 | 100% | 87 | 100% | 83 | 100% | NA |
| Married† | 18 | 45% | 32 | 37% | 31 | 37% | 0.65 |
| Education* | |||||||
| <High school | 11 | 27% | 11 | 13% | 13 | 15% | |
| High school | 15 | 37% | 41 | 48% | 45 | 54% | |
| >High school | 15 | 37% | 34 | 40% | 26 | 31% | 0.20 |
| Employed | 17 | 41% | 33 | 38% | 28 | 33% | 0.65 |
| Injured at residence | 34 | 83% | 68 | 78% | 67 | 80% | 0.82 |
| Medical contact‡ | 29 | 71% | 42 | 48% | 53 | 63% | 0.03 |
*Sample size reduced to n = 211 due to missing information.
†Sample size reduced to n = 210 due to missing information.
‡Defined as any medical contact in the interval between administration of the poison and death (emergency medical services, emergency department, or inpatient admission).
§Reflects analysis of variance for age and χ2 test for all other variables.
Table 2 Primary poisoning agent(s) by intent of death in Utah, 2002 (up to two identified per death).
| Primary poisoning agent | Unintentional (n = 41) | Suicide (n = 87) | Undetermined (n = 84) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Street/recreational drugs | 17 | 41% | 2 | 2% | 33 | 39% |
| Alcohol | 7 | 17% | 6 | 7% | 10 | 12% |
| Pharmacy—prescription | 21 | 51% | 54 | 62% | 52 | 62% |
| Pharmacy—over the counter | 2 | 5% | 8 | 9% | 1 | 1% |
| Carbon monoxide or other gas | 0 | 0% | 29 | 33% | 2 | 2% |
| Other poison or unspecified | 1 | 2% | 2 | 2% | 1 | 1% |
Table 3 presents a summary of substances tested for and identified in toxicological testing after death. This includes, but is not limited to, drugs and other substances directly involved in the death. Opiates were found in 83% of tested cases for both unintentional and undetermined cases compared to only 50% of suicide cases. The presence of other drugs (for example, diazepam, acetaminophen, cyanide) was highest for suicide cases, and suicide cases had a relatively low percentage of street drugs.
Table 3 Substances tested and present by intent in forensic toxicological testing following poisoning deaths in Utah, 2002.
| Unintentional (n = 41) | Suicide (n = 87) | Undetermined (n = 84) | p Value* | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tested | Present | Tested | Present | Tested | Present | |||||
| n | n | % | n | n | % | n | n | % | ||
| Alcohol | 41 | 10 | 24% | 81 | 27 | 33% | 81 | 15 | 19% | 0.10 |
| Antidepressants | 41 | 8 | 20% | 83 | 33 | 40% | 80 | 26 | 33% | 0.08 |
| Street drugs† | 41 | 12 | 29% | 60 | 8 | 13% | 80 | 30 | 38% | 0.007 |
| Opiates | 41 | 34 | 83% | 62 | 31 | 50% | 81 | 67 | 83% | <0.001 |
| Other drugs | 41 | 16 | 39% | 83 | 69 | 83% | 79 | 45 | 57% | <0.001 |
*Reflects χ2 test for association between each variable and intent of death.
†Street drugs refers here to cocaine, amphetamines, and/or marijuana.
Table 4 summarizes the prevalence of factors related to alcohol and drug use, mental and physical health, and personal difficulties such as job loss or relationship problems. Undetermined decedents had the highest percentage of reported current or past mental health treatment. While none of the undetermined decedents left a suicide note, suicidal behavior (previous attempt or intent to commit suicide) was reported for 11 (13%) of these cases. The undetermined decedents were similar to unintentional decedents with respect to recent crisis, physical health problems, and alcohol or drug abuse problems. Of the three groups, suicide decedents were the most likely to be reported as depressed at the time of incident and the most likely to have a diagnosis of mental illness.
Table 4 Mental health history and potentially contributing factors by intent among poisoning deaths in Utah, 2002.
| Unintentional (n = 41) | Suicide (n = 87) | Undetermined (n = 84) | p Value‡ | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Depressed mood | 7 | 17% | 72 | 83% | 27 | 32% | <0.001 |
| Any mental diagnosis | 19 | 46% | 74 | 85% | 58 | 69% | <0.001 |
| Mental health treatment | 21 | 51% | 50 | 57% | 57 | 68% | 0.16 |
| Alcohol/drug abuse | 34 | 83% | 29 | 33% | 63 | 75% | <0.001 |
| Alcohol/drug treatment | 3 | 7% | 2 | 2% | 10 | 12% | 0.05 |
| Suicidal behaviour* | 0 | 0% | 68 | 78% | 11 | 13% | <0.001 |
| Recent crisis | 6 | 15% | 26 | 30% | 12 | 14% | 0.02 |
| Physical health | 26 | 63% | 23 | 26% | 57 | 68% | <0.001 |
| Contributing factor(s)† | 14 | 34% | 47 | 54% | 40 | 48% | 0.11 |
*Suicidal behavior was considered positive if the decedent left a suicide note, declared intent to commit suicide, or had previously attempted suicide.
†Factors included are relationship problems, job, school, and financial problems, recent suicide or death of a friend or family member, criminal or legal problems, perpetrator or victim of interpersonal violence, and other circumstances potentially related to the death.
‡Reflects χ2 test for association between each variable and intent of death.
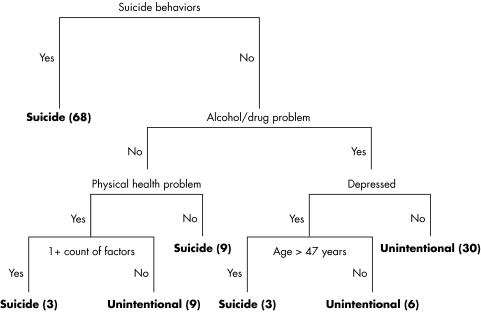
The results of the CART analysis are presented in figure 1. Each split of the tree represents a decision point for classifying a poisoning death record as unintentional or suicide. Using this analytic technique, suicidal behavior was identified as the single most important discriminating factor between unintentional and self‐inflicted poisonings.
Figure 1 Classification of intent (suicide v unintentional) based on CART analysis. Note: this figure highlights suicidal behavior, alcohol or drug abuse/dependence, physical health problems, depression, one or more contributing factors (see table 4 footnotes), and age >47 years as discriminating between suicide and unintentional poisoning. Parenthetical numbers represent the total cases in each terminal node for those having reported manner of death of either suicide or unintentional (n = 128).
To interpret the tree, follow each decision point to a terminal node where the classification of suicide or unintentional death is given. For example, a poisoning death with no history of alcohol or drug abuse and no physical health problems would be classified as suicide. As another example, if an alcohol or drug problem was identified, and there was no indication of a depressed mood at the time of the incident, then the record was classified as unintentional.
The tree misclassified four of the 128 unintentional and suicidal poisonings resulting in an apparent misclassification rate of 3%. No data were available to obtain a true misclassification rate which would be calculated by applying this decision tree to a new dataset with the same variables and known classification.
When applied to undetermined poisoning deaths, 18 of the 84 deaths (21%) were classified as suicides. The majority of these (n = 11) received this classification based on the presence of suicidal behaviors. The remainder of undetermined poisoning deaths (n = 66) were classified as unintentional. If we apply this result to all undetermined poisoning deaths reported for 2002 (n = 168), a total of 36 would be classified as suicide. Thus, according to this model, the poisoning suicide rate in Utah for 2002 is underestimated by 29% (36/(87+36)). There were 342 suicides from all causes in 2002, resulting in an overall underreporting due to undetermined poisoning suicides of just under 10% (36/(342+36)). The underreporting for unintentional poisoning deaths is estimated at 61% (132/(85+132)).
Similar to the CART analysis, our random forests analysis identified suicidal behavior, depressed mood, physical health, alcohol/drug problems, and age as key predictors of intent of death. In addition, the primary poisoning agent (pharmacy prescription v other) was also highlighted as a key predictor. The percentage of undetermined poisoning deaths classified as suicide using the random forests technique was 13%, slightly lower than the 21% from our CART analysis.
Discussion
Suicide is a complex phenomenon which often evokes strong opinions in individuals and communities regarding philosophical, cultural, religious, social, and medico‐legal issues.1,2 Without explicit evidence of suicidal intent, these pressures may decrease the likelihood that a death is certified as a suicide. While there has been substantial debate over what portion of undetermined deaths may be attributable to suicide, there is general agreement that at least some undetermined deaths are suicides.1,3,4,5,6,18,19 Poisoning deaths are particularly difficult to classify by intent. Similar to other studies,9,20 our study showed that most undetermined poisoning decedents have alcohol or drug abuse problems, test positive for opiates, and have physical health problems. These characteristics mirror unintentional poisoning deaths in many ways and may only be distinguished by anecdotal information or circumstances that suggest suicidal intent.3,20 For example, we found that depression and suicidal behaviors, known risk factors for suicide, were more prevalent in undetermined than unintentional poisoning cases. Assigning intent is further complicated because many drug users demonstrate an ambivalence or reckless disregard for life that can be difficult to distinguish from suicidal intent, especially if other circumstances, such as relationship problems or recent death of a loved one, are present.20,21
Another obstacle to correctly assessing intent is the lack of routine forensic toxicological examination, physical evidence, and circumstantial data collected by medical examiners and others who investigate poisoning deaths. Most medical examiners and coroners agree on the fundamental premise that manner of death (intent) is circumstance dependent, not autopsy dependent.22 However, risk factors for suicide such as depression and precipitating circumstances in the decedent's life may not be consistently known or reported. Studies have advocated for standardized guidelines for death investigation that would provide information relevant to suicide deaths.10,20,23 Standardized data collection forms that facilitate consistent and detailed medico‐legal investigation into poisoning deaths of all intents would not only strengthen research regarding suicide and undetermined deaths, but also improve understanding of the self‐destructive or risk taking behaviors that play a role in many unintentional poisoning deaths.
Many studies of suicide treat all undetermined deaths as suicide; others exclude this group entirely. Both approaches are flawed and miscount the number and possibly the nature of suicide.2,24 Our classification tree analysis showed that one in five undetermined poisoning deaths is likely self‐inflicted, underestimating the poisoning suicide rate by approximately 30%, and the overall suicide rate by 10%. These findings have implications for surveillance efforts which aid in health planning and are used to track trends in rates, identify new problems, and assess the impact of interventions. Although not the primary focus of this manuscript, our results show an even greater degree of underreporting for unintentional poisoning deaths.
Efforts to address surveillance issues must account for regional differences in suicide and undetermined death rates. These rates are affected by variations in legal requirements and definitions, differences in the extent to which cases are investigated, and area specific risk factors.1,6,8 Because there are no standardized guidelines for manner of death classification, it is difficult to compare manner of death statistics across states, regions, or even individual medical examiners and coroners.25 Utah, for example, has unique demographic and cultural influences, a centralized medical examiner system, and as a general policy certifies all recreational drug deaths as undetermined unless there is clear evidence for a more specific manner of death (Todd Grey, MD, Utah Chief Medical Examiner, personal communication, 2005). Utah is one of four states (also Maryland, Massachusetts, and Rhode Island) with an undetermined death rate that is more than four times the national rate.11 As a result, although general conclusions from this study are likely to extend to other localities, specific conclusions related to the extent of underreporting may not be generalizable.
This study has limitations. First, due to funding constraints we were only able to include a relatively small sample size over a one year period. Collection of data over multiple years and inclusion of all cases would allow further investigation into the study hypothesis. Second, we found that documentation was often unavailable for mental health history and other factors in the medical examiner record, especially for unintentional or undetermined poisoning deaths. This makes it difficult to correctly classify undetermined deaths based on these characteristics. The differences we observed in circumstances by manner of death may represent actual differences in prevalence, but could also be due to whether or not these factors were reported. In addition, abstractors were not blinded to the intent of death assigned by the medical examiner. This could have resulted in differential capture or interpretation of information. Finally, our CART analysis assumes that all suicide and unintentional deaths were classified correctly by the medical examiner. A systematic review and reclassification of manner of death by someone other than the medical examiner was not within the scope of this study.
Overall, our results show that while the characteristics of undetermined poisonings do have striking similarities to both unintentional and suicidal poisonings, they are distinct from either group. It may be these distinct characteristics that make it difficult for a medical examiner to classify these deaths as either suicide or unintentional. Using the novel approach of classification tree analysis, we identified suicidal behavior, drug abuse, physical health problems, depressed mood, and age as discriminating between suicide and unintentional poisoning and estimated that suicides rates related to poisoning are underreported by approximately 30% in our state. This underreporting has important implications in suicide surveillance efforts including policy development, funding, and evaluation of prevention programs.
Key points
Poisoning deaths pose a unique difficulty to medical examiners and coroners in determining the intent of death.
Classification tree analysis identified suicidal behavior, drug abuse, physical health problems, depressed mood, and age as discriminating between suicide and unintentional poisoning.
We estimated that the poisoning suicide rate in Utah is underreported by approximately 30% and the overall suicide rate is underreported by 10%.
Standards that promote consistent and detailed medico‐legal investigation into poisoning deaths of all intents would strengthen research regarding suicide and undetermined deaths.
Acknowledgements
We gratefully acknowledge the assistance of Anna Davis, Andrea Genovesi, and Lee Anne Gabor in abstracting and entering data from the medical examiner records. We also acknowledge Dr Todd Grey and Sarah Kay North at the Utah Office of the Medical Examiner for facilitating the data collection process, and Catherine Barber, Todd Grey, and Lisa Hyde for their insightful reviews before submission of the manuscript.
Abbreviations
CART - classification and regression tree
NVDRS - National Violent Death Reporting System
NVISS - National Violent Injury Statistics System
Footnotes
This research was partially supported by Centers for Disease Control and Prevention grant number U49/CCU915983/06 and a grant from the Harvard Injury Control Research Center's National Violent Injury Statistics System project.
Competing interests: none.
Ethics approval: this study was approved by the University of Utah Institutional Review Board.
Partially presented at the American Public Health Association's (APHA) 133rd Annual Meeting, Philadelphia, Pennsylvania, December 2005.
References
- 1.Institute of Medicine Reducing suicide: a national imperative. Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE (eds). Washington DC: The National Academies Press, 2002 [PubMed]
- 2.Public Health Service National strategy for suicide prevention: goals and objectives for action. Silverman MM, Frankel MJ, Miller AC (eds). Rockville, MD: US Department of Health and Human Services, Public Health Service, 2001
- 3.Ohberg A, Lonnqvist J. Suicides hidden among undetermined deaths. Acta Psychiatr Scand 199898214–218. [DOI] [PubMed] [Google Scholar]
- 4.Phillips D P, Ruth T E. Adequacy of official suicide statistics for scientific research and public policy. Suicide Life Threat Behav 199323307–319. [PubMed] [Google Scholar]
- 5.Speechley M, Stavraky K M. The adequacy of suicide statistics for use in epidemiology and public health. Can J Public Health 19918238–42. [PubMed] [Google Scholar]
- 6.O'Carroll P W. A consideration of the validity and reliability of suicide mortality data. Suicide Life Threat Behav 1989191–16. [DOI] [PubMed] [Google Scholar]
- 7.Kleck G. Miscounting suicides. Suicide Life Threat Behav 198818219–236. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention Unintentional and undetermined poisoning deaths – 11 states, 1990–2001. Morb Mortal Wkly Rep 200453233–238. [PubMed] [Google Scholar]
- 9.Camidge D R, Wood R J, Bateman D N. The epidemiology of self‐poisoning in the UK. Br J Clin Pharmacol 200356613–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lindqvist P, Gustafsson L. Suicide classification—clues and their use. A study of 122 cases of suicide and undetermined manner of death. Forensic Sci Int 2002128136–140. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention National Center for Injury Prevention and Control. Web‐based injury statistics query and reporting system. Available at http://www.cdc.gov/ncipc/dvp/dvp.htm (accessed November 2005)
- 12.Harvard Injury Control Research Center National Violent Injury Statistics System Workgroup. Uniform data elements: National Violent Injury Statistics System, release 2, 0. Available at http://www.hsph.harvard.edu/nviss/documents/Version2UDE3.pdf (accessed May 2005)
- 13.Paulozzi L J, Mercy J, Frazier L., Jret al CDC's National Violent Death Reporting System: background and methodology. Inj Prev 20041047–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewis R J. An introduction to classification and regression tree (CART) analysis. Available at http://www.saem.org/download/lewis1.pdf (accessed May 2005)
- 15.Breiman L, Friedman J H, Olshen R A.et alClassification and regression trees. New York: Chapman and Hall, 1993
- 16.Breiman L. Random forests. Machine learning 2001455–32. [Google Scholar]
- 17.Breiman L, Cutler A. Random forests. Available at http://oz.berkeley.edu/users/breiman/RandomForests/cc_home.htm (accessed March 2006)
- 18.Mohler B, Earls F. Trends in adolescent suicide: misclassification bias? Am J Public Health 200191150–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holding T A, Barraclough B M. Undetermined deaths—suicide or accident? Br J Psychiatry 1978133542–549. [DOI] [PubMed] [Google Scholar]
- 20.Cantor C, McTaggart P, De Leo D. Misclassification of suicide‐the contribution of opiates. Psychopathology 200134140–146. [DOI] [PubMed] [Google Scholar]
- 21.Stanistreet D, Taylor S, Jeffrey V.et al Accident or suicide? Predictors of Coroners' decisions in suicide and accident verdicts. Med Sci Law 200141111–115. [DOI] [PubMed] [Google Scholar]
- 22.Hanzlick R, Hunsaker J C, Davis G J. National Association of Medical Examiners. A guide for manner of death classification. Available at http://www.thename.org/Library/MannerRev.pdf (accessed June 2005)
- 23.Jougla E, Pequignot F, Chappert J.et al Quality of suicide mortality data [in French]. Rev Epidemiol Sante Publique 20025049–62. [PubMed] [Google Scholar]
- 24.Linsley K R, Schapira K, Kelly T P. Open verdict v. suicide—importance to research. Br J Psychiatry 2001178465–468. [DOI] [PubMed] [Google Scholar]
- 25.Hanzlick R, Goodin J. Mind your manners. Part III: Individual scenario results and discussion of the National Association of Medical Examiners Manner of Death Questionnaire, 1995. Am J Forensic Med Pathol 199718228–245. [DOI] [PubMed] [Google Scholar]