Abstract
Acquired haemophilia is rare and potentially fatal, with a mortality of 20% if left untreated. There is a strong association with other autoimmune diseases. This report describes a patient with rheumatoid arthritis, vitiligo, and bullous pemphigoid where the diagnosis of acquired haemophilia was made after an extensive bleed into a bullous lesion in the buccal mucosa. This case highlights some of the potential complications of acquired haemophilia and its treatment.
Keywords: acquired haemophilia, bullous pemphigoid, buccal haematoma, factor VIII inhibitor concentration, factor eight inhibitor bypassing activity (FEIBA)
Acquired haemophilia is a rare autoimmune disease with an annual incidence of one per million. Anti‐factor VIII IgG is the most commonly detected autoantibody and in most cases its presence is idiopathic. However, in a number of cases it is associated with other autoimmune diseases. In contrast with the low inhibitor levels seen in association with malignancy, pregnancy, or adverse drug reactions, patients with inhibitor attributable to autoimmunity usually have high titre inhibitors that do not recede spontaneously or with corticosteroids alone.1 Further immunosuppressive therapy is often needed. Thus clinicians should maintain a high index of suspicion where there is unusual unexplained bleeding in patients with systemic autoimmune disease.
Case report
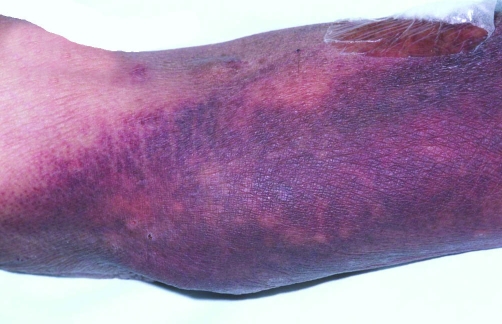
A 78 year old man presented to the accident and emergency department with persistent bleeding from a large left buccal haemorrhagic swelling (fig 1). Examination also showed extensive bruising on both his arms (fig 2).
Figure 1 Bleeding into intraoral bullae.
Figure 2 Extensive ecchymoses on the upper limb.
Four months previously, the patient had presented with widespread cutaneous blistering. A skin biopsy showed an eosinophil‐rich subepidermal blister and direct immunofluorescence showed linear deposition of IgG along the dermoepidermal junction, findings characteristic of bullous pemphigoid. He was treated with prednisolone 40 mg daily, tailing to a maintenance dose of 20 mg. The APTT was normal (29.2 seconds) before the biopsy.
His medical history included rheumatoid arthritis, vitiligo, and ischaemic heart disease. Recent endoscopies for iron deficiency anaemia revealed a hiatus hernia with gastric erosions and a normal lower gastrointestinal tract. He was taking Adcal D3, lansoprazole, digoxin, spironolactone, bumetanide, aspirin, atorvastatin, sulphasalazine, ramipril, carvedilol, and prednisolone.
Investigations showed a microcytic anaemia and prolonged APTT (115.0). Blood film showed polychromasia and rouleaux in keeping with autoimmune disease and recent haemorrhage. A repeat clotting screen confirmed the increased APTT. A 50:50 mix of the patient's plasma with normal plasma showed only partial correction of the APTT consistent with the presence of an inhibitor of coagulation rather than deficiency of an intrinsic clotting factor, in which full correction of the APTT would be expected. Factor VIII was measured at <1% and factor VIII antibodies at 839 Bethesda units (BU)/ml. Liver function tests, chest radiography, and prostate specific antigen were normal and there was no obvious underlying malignancy.
A diagnosis of acquired haemophilia was made. Factor eight inhibitor bypassing activity (FEIBA) 3000 international units (IU) was given twice daily to arrest the acute bleed and he was given 100 mg cyclophosphamide and 100 mg hydrocortisone. Initially treatment was given intravenously in view of the difficulty tolerating oral medication.
He responded promptly to treatment, with a 30% fall in inhibitor titre by day three and undetectable levels at six weeks. He continued on 30 mg prednisolone, but the cyclophosphamide had to be withdrawn in view of severe neutropenia and sepsis that required treatment with antibiotics and GCSF.
He relapsed three months later with a decline in his factor VIII level but responded promptly to 60 mg prednisolone alone and has maintained remission, without further treatment, for 12 months.
Discussion
This is one of the few case reports of acquired haemophilia in association with bullous pemphigoid.2,3,5,6,7,8 Our patient presented with a unique combination of four autoimmune diseases; rheumatoid arthritis, bullous pemphigoid; vitiligo; and acquired haemophilia. The association between bullous pemphigoid and acquired haemophilia is unlikely to be unique and may reflect some underlying immunogenetic susceptibility to autoimmune disease.10 Sequence homology between epitopes on factor VIII and XIII collagen (BP 180) or BP 230 was considered but a search through protein databases did not disclose any obvious homologous sequences.
Sulphonamides are reported to be associated with acquired haemophilia1 and a pathogenic role for sulphasalazine cannot be excluded in this case, although the lack of a temporal relation makes it unlikely.
Of the cases of bullous pemphigoid and acquired haemophilia, only two of these presented with similar bleeding into intraoral bullae in the presence of inhibitor.2,3 In one of those, recombinant factor VIIa, human immunoglobulins, prednisolone, and azathioprine were needed to achieve haemostasis, and suppress inhibitor production.2 In another case, acquired haemophilia was associated with anti‐laminin 5 pemphigoid, a rare autoimmune blistering disease.4 Autoantibodies, such as PM‐Scl have also been found to be associated with acquired haemophilia,5 but in this case no such autoantibodies were detected.
Patients with acquired haemophilia are at higher risk of death from haemorrhage than patients with congenital haemophilia who develop inhibitors. A recent meta‐analysis on treatment and prognostic markers in acquired haemophilia concluded that elderly patients with factor VIII autoantibodies have a very high mortality, although often related to comorbidity rather than the presence of inhibitor.1 Our patient had a myocardial infarction three years previously. This posed a particular risk during treatment when there is often an overshoot to supranormal factor VIII levels, increasing the potential for recurrent thrombosis.
Meta‐analysis showed that the level of factor VIII inhibitor has a great influence on patient outcome.1 Eradication is needed to prevent successive bleeds and is associated with a better clinical outcome. The antibody level detected in our patient (840 BU/ml) is higher than other reported cases of acquired haemophilia and bullous pemphigoid. In only one of these was a level greater than 100 BU/ml reported.3
Traditionally immunosuppression has been achieved with a combination of cyclophosphamide and prednisolone but prednisolone may be used alone and indeed there has been recent concern about increased morbidity with the addition of cyclophosphamide.1,9 This is highlighted in this case where cyclophosphamide led to severe neutropenia and there was equally rapid response to prednisolone alone for the treatment of his relapse.
This man had a number of poor prognostic risk factors in association with his acquired haemophilia, including age, comorbidity, and a very high inhibitor titre. Nevertheless, he responded rapidly to treatment and his outcome was favourable.
Learning points
The presentation of acquired haemophilia with bullous pemphigoid is a rare but important one.
Poor prognostic factors associated with acquired haemophilia include old age, comorbidity, and high inhibitor titre.
Lowering of the inhibitor level is the target of successful treatment aiming to reduce the risk of successive bleeds.
The treatment of acquired haemophilia in association with other autoimmune diseases may need additional immunosuppressive agents (for example, cyclophosphamide) but this can be associated with significant adverse effects.
This case highlights the importance of rapid diagnosis and effective treatment to prevent the torrential and sometimes relentless bleeding complications that can occur and to obtain a favourable outcome.
Acknowledgements
Sarah Sutton, Clinical Librarian, Leicester Royal Infirmary, Leicester. Linda Ward, Clinical Librarian, Leicester General Hospital, Leicester.
References
- 1.Delgado J, Jimenez‐Yuste V, Hernandez‐Navarro F.et al Acquired haemophilia: review and meta‐analysis focused on therapy and prognostic factors. Br J Haematol 200312121–35. [DOI] [PubMed] [Google Scholar]
- 2.Lightburn E, Morand J J, Graffin B.et al Pemphigoid and acquired haemophilia. Ann Dermatol Venereol 20011281229–1231. [PubMed] [Google Scholar]
- 3.Vissink A, van Coevorden A M, Spijkervet F K L.et al Spontaneous blood blister formation swellings of the oral mucosa. Ned Tijdschr Tandheelkd 2003110359–361. [PubMed] [Google Scholar]
- 4.Ly A, Roth B, Causeret A S.et al Anti‐laminin 5 pemphigoid and acquired haemophilia. Br J Dermatol 20021461104–1105. [DOI] [PubMed] [Google Scholar]
- 5.Beyne‐Rauzy O, Fortenfant F, Adoue D. Acquired haemophilia and PM‐Scl antibodies. Rheumatology 200039927–928. [DOI] [PubMed] [Google Scholar]
- 6.Maczek C, Thoma‐Uszynski S, Schiler G.et al Simultaneous onset of pemphigoid and factor VIII antibody haemophilia. Hautrarzt 200253412–415. [DOI] [PubMed] [Google Scholar]
- 7.Angchaisuksuri P, Atichartakam V, Pathepchotiwong K.et al Experience with factor VIII:C inihibitors and acquired von Willibrand's disease in an adult at Ramathibodi Hospital. Southeast Asian J Trop Med Public Health 199324(suppl 1)152–158. [PubMed] [Google Scholar]
- 8.Fisher M, Lechner K, Raith W. Inhibitor haemophilia in bullous pemphigoid. Hautarzt 196819459–462. [PubMed] [Google Scholar]
- 9.Collins P, Macartney N, Davies R.et al A population based, unselected, consecutive cohort of patients with acquired haemophilia A. Br J Haematol 200412486–90. [DOI] [PubMed] [Google Scholar]
- 10.Eisenbarth G S, Gottlieb P A. Autoimmune polyendocrine syndromes. NEJM 20043502068–2079. [DOI] [PubMed] [Google Scholar]