Abstract
Backgound
Patients with acute coronary syndrome (ACS) are at high risk of further cardiac events and benefit from early intervention, as reflected by international guidelines recommending early transfer to interventional centres. The current average waiting time of up to 21 days contravenes evidence based early intervention, creates geographical inequity of access, wastes bed days, and is unsatisfactory for patients.
Methods
A regional transfer unit (RTU) was created to expatiate access of ACS patients referred from other centres to the revascularisation service. By redesigning the care pathway patients arriving on the RTU undergo angiography within 24 hours, and then leave the RTU the following day, allowing other ACS patients to be treated.
Results
During the first six months of the RTU, the mean waiting time from referral to procedure decreased from 20 (SD 15) days (range 0–51) to 8 (SD 3) days (range 0–21) for 365 patients transferred from a distict general hopsital. Ninety seven per cent of patients underwent angiography within 24 hours, 61% having undergone percutaneous coronary intervention at the same sitting, and 78% were discharged home within 24 hours.
Conclusions
Delivering standards laid out in the National Service Framework, reducing inequalities of care across the region, and facilitating evidence based strategies of care represents a challenging and complex issue. For high risk patients suffering ACS who need early invasive investigation, a coordinated network wide approach together with the creation of an RTU resulted in a 62% reduction in waiting times for no extra resources. Further improvements can be expected through increased capacity of this verified strategy.
Keywords: acute coronary syndrome, revascularisation, waiting times
Acute coronary syndromes (ACS) represent the most common cause of death in the western world,1 and account for 120 000 admissions to UK hospitals a year.2 Recent improvements in the understanding of ACS and the associated prognosis has lead to evidence based changes in clinical practice and subsequent outcomes.3 The PRAIS‐UK registry of 1046 patients with ACS without ST elevation, found the rate of death and non‐fatal MI at six months after admission was 12.2%, and of death, new myocardial infarction, refractory angina, or readmission for unstable angina was 30%.4 Similarly, the OASIS registry of nearly 8000 patients with unstable angina and NSTEMI found rates of 10.1% and 22% respectively.5 Furthermore, these high risk patients have been shown to gain prognostic benefit from early revascularisation (FRISC‐II and TACTICS‐TIMI 18).6,7 As a result, national and international guidelines recommend referral for inpatient coronary angiography with a view to revascularisation. The routine use of troponin measurements to identify patients at “high risk” has, in particular, increased the proportion of such patients referred for angiography and revascularisation.8
These recommendations have a significant impact on coronary intervention resources and consequent waiting times. Furthermore, it has created a disproportionate waiting time for patients admitted to district general hospitals (DGHs) when compared with those admitted to a hospital with invasive facilities.9 In addition, there is an increasing awareness of the large number of bed days wasted, particularly in DGHs, by patients waiting for inter‐hospital transfer.10 For example, over a six month period in Manchester 212 non‐emergency ACS patients occupied 1755 bed days in DGHs waiting transfer to the interventional centre.10
The massive burden of patients awaiting inpatient coronary intervention for ACS was recently highlighted in the National Transfer Audit conducted as part of the Coronary Heart Disease Collaborative.11 In this audit of 141 UK NHS trusts and a total of 1708 ACS patients, the average time from admission to intervention was 15 days, and up to 21 days in some regions of the country. The average wait was 13 days with 1708 patients transferred during a four week period. This equates to 22 204 occupied bed days.
Such waiting times are unacceptable for a number of reasons. Firstly, they contravene the fifth report on the provision of services for patients with heart disease that suggests patients' “care must be easily accessible with no delay if the need is urgent.” Secondly, the wait represents inefficient use of resources, and is frustrating and upsetting for patients and their relatives. Thirdly, the length of the wait is so far outside the time achieved in the papers upon which the practice is based that it raises the questions as to whether we are actually delivering evidence based care.
This represents an observational prospective study of a novel change in clinical practice designed specifically to provide a rapid solution to long waiting times for DGHs patients by the development of a dedicated regional transfer unit (RTU). The aim of this unit was to admit and treat more ACS patients from referring centres by keeping them at the revascularisation centre for only 24 hours. During that time the patients would undergo angiography and either percutaneous coronary intervention (PCI) followed by discharge or surgical opinion for coronary artery bypass graft (CABG) and then transfer back to the referring centre to await CABG surgery.
Aims
The aim of this observational prospective study was to monitor a novel change in clinical practice designed specifically to provide a rapid solution to long waiting times for DGH patients by the development of a dedicated RTU.
Methods
An internal audit was initially performed that confirmed a mean time from referral to intervention of 20 (SD 15) days (range 0–51) for patients presenting to district hospitals. At any one time during this audit there were between 40 and 60 patients awaiting transfer to the interventional centre. Furthermore, for the patients transferred into the interventional centre the mean time from arrival to angiography was four (SD six) days.
The RTU was developed in the following way.
A subcommittee of the Central South Coast Cardiac Network was set up with special responsibility for ACS. This committee included representatives from all referring hospitals, Wessex Cardiac Unit as well as Network and CHD collaborative managers. It was agreed that it was a priority to use the revascularisation facilities as efficiently as possible. To minimise the stay for each patient, a form was devised to be filled in at the time of referral that would ensure each patient was ready to undergo an angiogram (± PCI) within 24 hours of arrival. The form mandates investigation of important comorbidities such as anaemia, recent stroke, renal impairment before transfer (the form is available on line http://www.postgradmedj.com/supplemental).
Representatives for Hampshire Ambulance Services were coopted onto the ACS Network Committee and were actively involved in the planning of the transport of patients transferred into RTU. Patients were booked into available slots and the ambulance service was therefore given at least 24 hours notice for most journeys.
A dedicated six bedded bay was created out of existing beds previously occupied by patients awaiting ACS intervention. Minimal additional resources were therefore required. Hospital management agreed to protect RTU for regional transfer ACS patients only.
Patients arriving on the RTU were pre‐booked into designated catheter laboratory slots for “coronary angiography with a view to follow on PCI”. Such slots were either on the day of transfer or the following morning (table 1).
To ensure continuous patient turnover within 24 hours, patients would be required to leave the RTU the day after their interventional slot. The following pathways were used: (a) discharge home if either they had undergone PCI or if they were to be treated medically (b) transfer to the DGH of patients requiring inpatient CABG. To facilitate this patients referred to the surgical team would be assessed, and listed for surgery, on the day of catheterisation. (c) Transferred to an ordinary bed in Southampton if unfit for discharge or requiring very urgent surgery.
Table 1 Referring hospitals and the percentage of patients having local angiography.
| Hospital | Percentage having local angiography |
|---|---|
| 1 | 100 |
| 2 | 15 |
| 3 | 1 |
| 4 | 90 |
| 5 | 0 |
| 6 | 0 |
| 7 | 0 |
| 8 | 0 |
| 9 | 0 |
The primary end point of the study was a reduction in waiting times for patients requiring invasive investigation for an ACS.
Results
During the first six months of the RTU, 365 patients with ACS were referred and transferred for further intervention. The mean (SD) age was 63.8 (11.3) years, and 75% of patients were male.
Time to transfer
The mean (SD) waiting time from DGH referral to angiography decreased from 20 (15) days (range 0–51) to 8 (3) days (range 0–21), (p<0.001). Once in the RTU, 97% all patients received invasive investigation either the same day or within 24 hours.
Outcome of invasive investigation
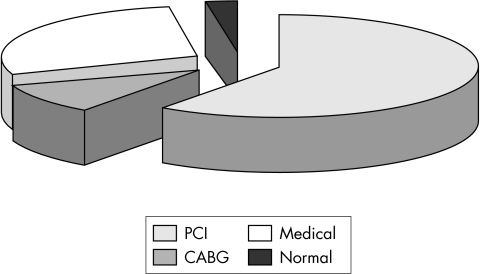
Sixty one per cent of all patients underwent PCI, and 10% were referred for inpatient CABG (none as an emergency). Twenty seven per cent of patients did not receive either PCI or CABG, but had coronary disease requiring ongoing medical therapy. Two per cent of patients had angiographically normal coronary arteries (fig 1).
Figure 1 Outcome of interventional investigation. PCI , percutaneos intervention; CABG, coronary artery bypass graft surgery.
After the procedure, 78% of patients were discharged home within 24 hours. Five per cent were transferred back to the DGH to await inpatient CABG. Fourteen per cent required step down to a cardiology ward bed for further treatment, 11% requiring urgent CABG and 6% requiring management of procedure based complications (groin haematomas) or tertiary centre investigation and management.
In terms of transport arrangements, 84% of patients discharged home made their own arrangements, 5% required a hospital car, and 5% a taxi. The 6% transferred back to the DGH to await CABG required ambulance (intermediate crew, not emergency 999) transport.
Subgroup analysis of referral patterns
Nine hospitals referred patients to the RTU, with a wide variety of referral rates (table 1).
Patients receiving prior local angiography had a waiting time from referral to PCI of 9 (SD 4) days (range 2–21 days). However, the time from admission to the DGH to referral was 8 (SD 5) days. Performing a local angiogram resulted, therefore, in a waiting time from admission to PCI of 17 (SD 6) days.
Discussion
The creation of a dedicated RTU backed up by a coordinated clinical and logistical management pathway from the point of admission at the referral centre to procedure led to a 62% reduction in waiting times. This provides more efficient, evidence based care that is far more equitable than previously shown.9 This initiative shows the feasibility of network‐wide coordination in the management of such patients and can be achieved without an increase in capital or immediate revenue expenditure. The vast majority of patients transferred to the revascularisation facility underwent angiography within 24 hours of referral. This was achieved for two fundamental reasons. Firstly, clinicians at the DGH centres had agreed to provide complete information about patients, even when this entailed further tests for the investigation of concomitant conditions. Secondly, dedicated slots were booked in the catheter laboratory to accommodate these patients. Furthermore, good patient information ensured that very few patients required hospital transport after they were discharged. Additional ambulance resources were not used, as these patients would have been transferred anyway, but a well planned and efficient system of advanced allocation of ambulances was required to deliver patients from any of nine referring hospitals to the interventional centre for a procedure the same day.
The concept of RTU can be summarised as containing the following components:
Coordination at network level between all interested stakeholders, including the ambulance service
An agreed, novel, care pathway that includes a referral form that ensures that each patient is fully prepared for angiography with or without revascularisation
Ongoing assessment of progress
This concept is applicable with local modification to a nationwide problem. The first National Interhospital Transfer Audit showed with considerable clarity the extent of the challenge set by patients waiting for angiography. The RTU concept, if rolled out across the country, could tackle this problem efficiently and with considerable savings in bed days, as well as staff and patient frustration.
The main limitation of this study is that a small proportion of patients referred to RTU were unsuitable for its 24 hour “turnover” deadline. Complex cases and those with valvular disease, for example, were excluded. Nevertheless, the mechanics of the RTU have been widened so that similar facilities are now being planned for other patients groups, including those requiring urgent electrophysiological procedures, patients awaiting cardiac surgery, and even those awaiting transfer to the regional neurological unit. A second limitation is that the ideal philosophy of care for these patients will remain for them to undergo invasive investigation and treatment in their own hospitals. A great deal of resource has therefore been appropriately dedicated to opening new catheter laboratories in DGHs to achieve this. The latter initiative will, however, take some time, and will probably still result in large numbers of patients who require transfer from one hospital to another.
Conclusion
Delivering standards laid out in the National Service Framework, reducing inequalities of care across the region, and facilitating evidence based strategies of care represents a challenging and complex issue. For high risk patients suffering ACS who need early invasive investigation, a coordinated network wide approach together with the creation of a RTU can have a significant impact on achieving these goals. Further improvements can be expected through increased capacity of this verified strategy. This project is comparatively simple to implement and is applicable to most revascularisation centres serving a network of referral centres.
The referral form is available on line (http://www.postgradmedj.com/supplemental).
Acknowledgements
We acknowledge the commitment of a wide range of healthcare professionals and managers in the success of this project. Specifically, we thank the consultant cardiologists both in Southampton and in the referral centres; nurses on E3 ward; catheter laboratory staff; Duncan Goodes and Dr Tony Jones from the Central South Coast Cardiac Network; Dr Faz Ordoubadi and Mrs Dot Crone.
Abbreviations
DGH - district general hospital
CABG - coronary artery bypass graft
PCI - percutaneous coronary intervention
RTU - regional transfer unit
ACS - acute coronary syndrome
Footnotes
Funding: none.
Competing interests: none declared.
The referral form is available on line (http://www.postgradmedj.com/supplemental).
References
- 1.Murray G, Lopez A D. Mortality by cause for eight regions of the world: global burden of disease Study. Lancet 19973491269–1276. [DOI] [PubMed] [Google Scholar]
- 2.British Cardiac Society guidelines and Medical Practice Committee, and Royal College of Physicians Clinical effectiveness and Evaluation Unit Guideline for the management of patients with acute coronary syndrome without persistent ECG ST elevation. Heart 200185133–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Archbold R A, Curzen N P. The role of revascularization in the management of non‐ST elevation acute coronary syndromes: who should you refer? Clin Med 2004432–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collinson J, Flather M, Fox K A.et al Clinical outcomes, risk stratification, and practice patterns of unstable angina and myocardial infarction without ST elevation: prospective registry of acute ischaemic syndromes in the UK (PRAIS‐UK). Eur Heart J 2000211450–1457. [DOI] [PubMed] [Google Scholar]
- 5.Yusef S, Flather M, Pogue J.et al Organization to assess strategies for ischaemic syndromes (OASIS) registry investigators. Variations between countries in invasive cardiac procedures and outcome in patients with suspected unstable angina or MI without initial ST elevation. Lancet 1998352507–514. [DOI] [PubMed] [Google Scholar]
- 6.Wallentin L, Lagerqvist B, Husted S.et al Outcomes at 1 year after an invasive compared with a non‐invasive strategy in unstable coronary‐artery disease: the FRISC II invasive randomised trial. Lancet 20003569–16. [DOI] [PubMed] [Google Scholar]
- 7. Cannon CP, Weintraub WS, Demopoulos LA, et al, for the TACTICS‐IMI 18 Investigators. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes trated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med 20013441879–1887. [DOI] [PubMed] [Google Scholar]
- 8.Curzen N. Troponin in patients with chest pain. BMJ 20043291357–1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Miller C, Lipscomb K, Curzen, N Are district general hospital patients with unstable angina at a disadvantage? Postgrad Med J 20037993–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bellenger N G, Eichhofer J, Crone D.et al Hospital stay in patients with non‐ST‐elevation acute coronary syndromes. Lancet 20043631399–1400. [DOI] [PubMed] [Google Scholar]
- 11.CHD Collaborative National Interhospital Transfer Audit. Presented at the CHD national transfer meeting 2004 and the British Cardiac Society annual meeting 2004. http://www.heart.nhs.uk