Abstract
Objective
British Association of Urological Surgeons (BAUS) guidelines and government initiatives have put pressure on the effective use of outpatient resources. Follow up appointments need to be carefully managed to ensure efficient use of available resources. The aim of this study was to audit outpatient follow up service with particular attention to the appropriateness of the appointments made.
Methods
All patients attending a general urology clinic were assessed by a form completed for each individual appointment. The source of the appointment and the time interval was recorded and each follow up appointment was judged to be either appropriate or inappropriate by the person giving the consultation. For those deemed to be inappropriate, justification was sought and the notes independently reviewed by a different clinician to verify this categorisation.
Results
Of 164 appointments made, 143 patients attended for follow up. A total of 131 appointments were considered to be appropriate (92%) with only 12 deemed by the consulting clinician to be inappropriate (8%). The commonest cause for an inappropriate appointment was failure to appreciate that follow up had already been arranged for a different date. There was no correlation between the source of the referral and an inappropriate referral.
Conclusion
This audit suggests an effective use of the outpatient follow up resource with respect to the appropriateness and timing of follow up consultations. Other areas of resource management such as default rates should be investigated in an attempt to improve the efficiency of a service.
Keywords: outpatient, follow up, appointments, resources
Outpatient resource management is an increasingly important aspect of health care. Government initiatives have put demands on resources, with all new patients having to be seen by a specialist within 13 weeks of initial referral from primary care by December 2005. The British Association of Urological Surgeons (BAUS) set guidelines in 2000 recommending that no more than seven new and seven old patients be seen per consultant in a general urology clinic (A Quality Urological Service for Patients in the New Millennium, Council of the British Association of Urological Surgeons, October 2000, http://www.baus.org.uk). After adjustment for case load complexity, a maximum of 20 patients per clinic was also recommended, which could be increased to 25 patients with the help of a junior specialist registrar or SHO, and 30 patients with a senior specialist registrar. Most new patient consultations are more time consuming than those required for follow up. These recommendations have reduced the number of patients seen per clinic in the urology outpatient department, and, to comply with the above time frame stipulations, have resulted in either an increased ratio of new to follow up patients per clinic or, indeed, extra new patient clinics.
Further stipulations are enforcing a maximum time of six months from the time patients are placed on waiting lists for procedures or operations to the date these are actually performed. The national target for 2008 is a maximum wait of 18 weeks from GP referral to hospital treatment. This has resulted in an unofficial multi‐tiered system of follow up appointment management, with most patients waiting longer than ideal between consultations to vacate clinic time in favour of the increased new patient work load. Urology is also an increasingly outpatient based specialty, putting more strain on resources. It is, therefore, of vital importance that only patients who require review are offered further appointments and that these are at an appropriate time interval.
Increasingly, alternatives are being used in attempts to reduce the heavy burden of review consultations. Telephone follow up policies for many procedures, such as transurethral resection of the prostate, are now well established.1 Also, many patients, for example, with lower urinary tract symptoms of benign origin, are now followed up in primary care after initial specialist consultation. Newer initiatives have resulted in well defined patient groups. For example, stable prostate cancer patients can be followed up in specialist nurse led clinics that are run in parallel with consultant clinics.
A recent national review showed that only 66 of 318 urology consultants (21%) adhered to the BAUS guidelines for out patient workload/manpower.2 In many centres extra clinics, paid at additional sessional rates, are used to overcome the lack of resources at an extra cost to the health service. We set out to audit our follow up service in a bid to critically appraise the appropriateness of the appointments given and with a view to highlighting any recurring themes that may be addressed in an attempt to improve service efficiency.
Methods
Because of the increasing burden of follow up patients, a general urology weekend initiative follow up clinic was arranged. This clinic was arranged as if it was a general urology mid‐week clinic, therefore keeping the same case mix. Three consultants and three middle grade urologists staffed this clinic. Each member of the team was asked to complete a short form for each patient seen (available on line http://www.postgradmedj.com/supplemental). For each patient basic appointment information was collected including the source of the appointment and the time interval requested for the appointment. As there are no strict follow up protocols, even postoperatively, there were no automatic appointments generated, and all appointments involved decision making by the source. The grade of the clinician reviewing the patient was also recorded and a view was sought regarding the appropriateness of the appointment in question. There were no specific criteria for appropriateness, but the member of staff was asked to justify, via free text, any appointments deemed to be inappropriate. These patient notes were then re‐assessed by an independent consultant urological surgeon to verify their inappropriate nature. This ensured that all appointments, both appropriate and inappropriate had concordance of two clinicians. For the appropriate appointments, this was the member of staff at the source and the reviewing urologist. The data were then analysed to determine any recurring themes relating to inappropriate follow up appointments.
Results
A total of 164 follow up appointments were sent out at least six weeks in advance of the clinic. In total, 143 (87%) patients attended these clinics representing a default rate of 13%. There was a broad case mix, including 44 with lower urinary tract symptoms, 23 with urological malignancy, 17 with stone disease, 16 with raised prostrate specific antigen, 14 with infections, 11 with minor penile or scrotal pathology, 7 with undiagnosed pain, 5 with prostatitis, and 6 with other disorders. At the clinics 70% (n = 100) of patients were seen by a consultant with the remainder seeing either a specialist registrar or experienced clinical fellow (n = 43). Fifty six of 143 (39%) patients were discharged after their consultation, 44 (79%) of these were seen by the consultant. Eighteen of the 21 (86%) who failed to attend were also discharged.
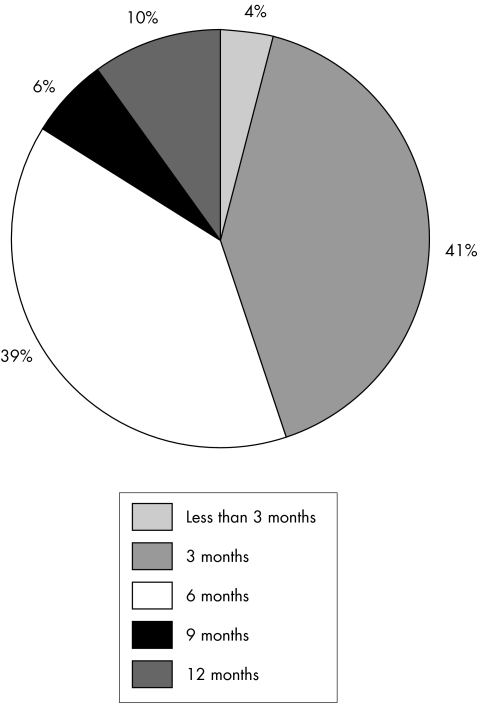
Fifty four per cent (n = 77) of the original appointments were made at the request of a consultant, with exactly half this amount being arranged at the request of a specialist registrar. Thirteen per cent (n = 19) of appointments were made by junior doctors from the urology ward and 3% (n = 4) by the urology specialist nurses. Only 3% (n = 4) of appointments originated from other sources, including other hospital wards. Forty one per cent (n = 58) and 39% (n = 56) of the follow up appointments were made for three and six months respectively. Five per cent of appointments (n = 7) were made for nine months and 11% (n = 16) for 12 months. Only 4% of appointments (n = 6) were made for less than three months (fig 1).
Figure 1 Time intervals for follow up appointments.
The vast majority of appointments (92%, n = 131) were considered, by the urologist performing the consultation, to be appropriate, with only 12 (8%) being classified as inappropriate (table 1). Eight of the inappropriate appointments were judged so by a consultant and four by a middle grade, with all of these subsequently confirmed to be inappropriate on notes review by the independent urologist.
Table 1 Numbers of appropriate and inappropriate appointments for a given appointment interval (as a percentage of all appointments).
| Appointment interval (months) | Total number of appointments | Appropriate referrals | Inappropriate referrals |
|---|---|---|---|
| <3 | 6 | 3 (2.1) | 3 (2.1) |
| 3 | 59 | 55 (38.5) | 4 (2.8) |
| 6 | 55 | 52 (36.4) | 3 (2.1) |
| 9 | 8 | 7 (4.9) | 1 (0.7) |
| 12 | 15 | 14 (9.8) | 1 (0.7) |
| Total | 143 | 131 (92) | 12 (8) |
Of the 12 inappropriate referrals, five were deemed to be so because follow up had already been arranged and carried out thus rendering their current appointment duplicate and unnecessary. Of the remaining inappropriate reviews, three patients had not completed their pending investigation, two had a medical condition requiring no follow up, such as simple urinary tract infection, and the time interval was deemed too short in two patients.
Most of the inappropriate appointments occurred at shorter time intervals; 25% at less than three months, 33% at three months, 25% at six months, 8% at nine months, and 8% at 12 months (table 1). There was no significant difference between the various sources of the referral with respect to the appropriateness of the review. We can explain this by our strict policy of making follow up appointments. Appointments being made from sources other than the consultants themselves are usually discussed with a consultant, registrar, or specialist nurse. There was also no difference in the frequency of inappropriate reviews when stratified for grade of reviewing clinician.
Discussion
Healthcare services are being constantly audited to ensure good clinical practice and effective use of resources. The aim of this study was to evaluate outpatient review appropriateness and to highlight areas of inefficiency requiring evaluation and alteration. We failed to identify any major trend that would lend itself to critical analysis and practice alteration. We accept a degree of inefficiency is not only present but would probably be unavoidable given the number of origins of follow up appointments possible and the sheer numbers of staff involved.
Almost half of those follow up appointments deemed to be inappropriate were secondary to duplication and this is an area of concern, albeit minor. It is of course far more acceptable to have appointment duplication rather than omission. This small number of repeated appointments may be necessary to eliminate or at least reduce the number of patients who manage to fall through the safety net and fail to have a review consultation generated. Another source of inefficiency is the default rate of attendance to clinics. We have shown this to be 13% in our practice, which is similar to that quoted previously.3 However, again, this may be unavoidable so that significant pathology is not missed. We accept that at the time of writing we are unaware of the number of patients inappropriately escaping follow up because of institutional error.
In general, our outpatient facility is efficient, organised and, in the main, consultant led. We believe that this, along with an active discharge policy from both the ward and the clinic, results in a more appropriate use of both medical time and resource. Many patients are initially offered a specialist opinion and once treatment is started are referred back to primary care for ongoing follow up. On discharge, there is instruction for re‐referral should the clinical picture change. In addition to this, telephone follow up by specialist nurses is commonplace for particular circumstances and again these are all done under consultant supervision and direction with strict criteria having to be fulfilled. Here, once again, rapid access to consultant clinics is assured should the need arise.
Clinic numbers in excess of guidelines drawn up by BAUS, could possibly lead to a situation of time pressure resulting in the clinician opting for a further review rather than investing the time required to resolve patient issues there and then with a view to active discharge if appropriate. Some government initiatives may, in themselves, be counterproductive. Studies have suggested that the two week wait cancer initiative is unlikely to improve cancer outcomes.4 This is because of the natural history of most urological cancers, particularly prostate cancer, and may not be appropriate in other specialties. However, such initiatives may introduce further inefficiencies into the outpatient setting by reducing flexibility and perhaps taking up urgent patient slots despite not filling the criteria for a HSC 205 suspected cancer referral.
Follow up appointments is only one aspect of outpatient resources. A model for determining the resource requirements for urology outpatient load has been proposed before. This was based on following up new patient referrals and calculating costs entailed in further investigation, follow up, and treatment.5 This has led to further assessment of the appropriateness of new patient referrals, both urgent and routine, and the use of ancillary outpatient resources, for example, phlebotomy and radiology
Conclusion
We conclude that the great majority of outpatient follow up appointments in our institution are appropriate due to a combination of factors including a largely consultant directed service, adherence to BAUS clinic number guidelines, and an active discharge policy. The use of telephone follow up has also greatly increased the efficiency of the service.
Further work is required to determine default patterns, if present, and to expand the current assessment to include urgent and routine referrals from both primary and secondary care.
The form used in the study is available on line (http://postgradmedj.com/supplemental).
Footnotes
Funding: none.
Conflicts of interest: none.
The form used in the study is available on line (http://postgradmedj.com/supplemental).
References
- 1.Brough R J, Pidd H, O'Flynn K J.et al Identification of patients requiring out‐patient follow‐up after transurethral prostatectomy: is there a role for nurse‐led screening of post‐operative outcomes by telephone? Br J Urol 199678401–404. [DOI] [PubMed] [Google Scholar]
- 2.Gilmore P E, Shackley D C, Clarke N W.et al National review of urology outpatient practice in the UK. Postgrad Med J 20058155–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simmons A V, Atkinson K, Atkinson P.et al Failure of patients to attend a medical outpatient clinic. J R Coll Physicians Lond 19973170–73. [PMC free article] [PubMed] [Google Scholar]
- 4.Allen D, Popert R, O'Brien T. The two week cancer initiative in urology: useful modernisation? J R Soc Med 200497279–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Payne S R, Brough R J, Mellor D E. Resource implications of outpatient referrals to a general urological service. Ann R Coll Surg Engl 199779111–114. [PMC free article] [PubMed] [Google Scholar]