Abstract
Objectives
To describe changing characteristics of men who sold sex in London between 1994 and 2003.
Methods
A baseline survey of 823 male sex workers attending a specialist clinic, plus follow up of 628 men for 1379 person years.
Results
Men recruited earlier (1994 to 1996) were more likely than those recruited later (2000 to 2003) to be UK born and to self define as homosexual. Later recruits included more men from South/Central America and eastern Europe and a higher proportion reported regular female partners. Baseline prevalence of HIV was 9% (59/636), and multivariate analysis showed an associated with injecting drug use and unprotected sex with a casual partner. During follow up there were 49 incident cases of HIV. Survival analysis showed earlier recruitment (1994–6) to be associated with a higher incidence of HIV. The prevalence of gonorrhoea increased over time.
Conclusions
Men who sell sex are at risk of HIV and other STIs, but these risks do not appear to be directly linked to sex work. The changing demographics of these men is associated with different patterns of infection and poses challenges for service delivery.
Keywords: HIV, sexually transmitted infections, prostitution, epidemiology, London
Men working in the sex industry have been reported as having an increased risk of sexually transmitted infections (STI) linked to both commercial and non‐commercial partnerships.1,2,3,4,5 There are few specific healthcare services for these men, and limited health promotion initiatives despite reports of high levels of sexual and drug taking risk behaviours.6,7 Men who sell sex primarily to men do not necessarily self identify as homosexual or bisexual, but their sexual behaviour places them at increased risk for disease acquisition.8 Morse and others have suggested that men who sell sex could form a “core group” for HIV and other STIs, acting as a conduit for infections to pass between heterosexual, homosexual, and bisexual populations, but little is actually known about the risks of STI acquisition or transmission in this group.9,10,11,12 The availability of focused sexual health services aimed at sex workers has been a proved method of delivering sexual health interventions and should be supported by detailed epidemiological information of the local workforce in order to best plan and implement appropriate interventions strategies.13
In the United Kingdom recently there has been an increase in the rate of bacterial STIs, including outbreaks of syphilis among male sex workers (MSWs) possibly because of increased high risk sexual behaviour.14,15,16,17,18,19 Since the collapse of the Iron Curtain specialist sexual health services in Europe have reported an increase in the number of sex workers from eastern Europe and elsewhere, often from regions of the world with higher rates of poverty, STIs, and HIV (www.europap.net). It is unclear what effect this demographic shift, reflecting global population movements, would have on the incidence of STIs and HIV in the local workforce. Of the published studies there are conflicting findings.20,21,22
An early report from our unit documented a high prevalence of HIV infection in men selling sex in London, and subsequently a unique clinical and health promotion service, the Working Men's Project, was developed.2 In this paper we report results from the first 10 years of this service, including the prevalence and incidence of HIV and STI and reported risk behaviours.
Methods
Sample and recruitment
This article reports on men who attended the Working Men's Project clinic from 1994 to the end of 2003. The project is a dedicated clinical service for men who sell sex, located in a busy inner city sexually transmitted disease clinic in London, offering free and confidential screening, health care, and health promotion. Any man who self reported as selling sex or having sold sex in the last 12 months was included in the study. While it is not possible to confirm how representative these men are of the local sex industry, inclusion criteria were as broad as possible so that participants were drawn from all types of local sex work venues. Three methods of recruitment were used to gain access to these men: (1) a weekly informal clinic held at an agency involved in outreach work with street based male prostitutes; (2) regular advertising of the health service in the “gay press” and later on the web; and (3) making direct telephone and internet contact (that is, using chatrooms) to men advertising themselves as escorts or masseurs in the gay press. Although outreach work remained fairly constant throughout the study period advertising via the internet increased in line with general usage (see www.wmplondon.org.uk).
Data collection
A structured proforma was completed by the doctor or nurse practitioner at the registration visit, and included demographic information, past medical history (including STI, psychiatric history, sexual abuse, drug use, and addiction), details of work in the sex industry (duration, numbers and gender of clients in the previous month, and condom use with their last four clients), sexual behaviour (numbers and genders of regular and casual partners, frequency of condom use with their regular and previous two casual non‐paying partners), and type of sexual activity with clients, regular, and casual partners. Men attended for voluntary follow up screening at varied intervals. At these visits further information was collected on recent risks and symptoms. If there were positive results that required treatment subjects were contacted by telephone or post at least three times to advise them to attend the project. Those who had initiated a vaccination programme were telephoned before their appointment for vaccination and if they failed to attend.
Laboratory testing
Screening was based on routine methods for most infections. Anatomical sites tested depended on reported sexual activity. Gonorrhoea was detected using Gram stain with culture confirmation (modified New York City selective agar, Biomerieux, UK) throughout the study period. Non‐gonococcal urethritis (NGU) was detected using direct microscopy of a dry mount from a urethral swab. Over the 10 years the study took place enzyme linked immunofluorescence assay, ligase chain reaction and, most recently, strand displacement amplification (Probetec, Becton Dickinson, UK) were used to detect urethral chlamydia. Direct immunofluorescence (Sterilab, UK) was used to identify chlamydia from pharyngeal and rectal specimens. A diagnosis of new genital herpes was based on positive culture from a clinical lesion in someone with no previous history. Serum samples were tested for antibodies to HIV‐1 and HIV‐2 using routine enzyme linked immunosorbent assay (ELISA) (Bayer Advia Centaur) screening tests with confirmation. Subjects who self reported HIV infection at baseline were retested for HIV. Syphilis was diagnosed using a combined IgG/IgM enzyme immunoassay (EIA) (Newmarket, UK), Treponema pallidum haemagglutination assay (TPHA) (Fujiribo, Mast Diagnostics UK), rapid plasma reagin (RPR) (Biokit, Lauch Diagnostics, UK), and fluorescent treponemal antibody (FTA) (this being superseded by a separate IgM ELISA (Mercia Diagnostics, UK). IgG and IgM ELISAs were used to screen for hepatitis A (Bayer Advia Centaur), hepatitis B core antibody (Bayer Advia Centaur) was used as evidence of past infection; hepatitis C (Bayer Advia Centaur) was screened for using a second or third generation chemoluminescent immunoassay confirmed using a third generation recombinant Inno Genetics line immunoassay.
Data management and statistical analysis
Data from proformas were entered into a database, linked to results of tests, and exported into statistical packages for analysis. All data were stored with a unique number and no personal identifying information.
Duration of follow up was calculated from the date of first visit to the most recent visit until the end of 2003, with loss to follow up being defined as having not attended the clinic for 1 year or more.
The population was stratified into three cohorts, of approximately equal intervals, based on year of first attendance (1994 to 1996, 1997 to 1999, 2000 to 2003) to explore changes over time. Factors associated with HIV infection at first visit (prevalent HIV) were also explored. We performed univariate analysis (χ2 tests for categorical variables and Kruskal‐Wallis test for continuous variables), and then developed stepwise logistic regression models to explore associations further. These models included factors found to be significant on univariate analysis, and key variables known to be associated with the outcome variable.
Survival analyses were undertaken to assess risks for seroconversion for men who were initially HIV negative. Since seroconversion is only known to have occurred between two dates (the date of the last negative test and the date of the first positive test) the data are interval censored. Accelerated failure time models (with a lognormal survival distribution) were therefore used to test for the association between characteristics of the MSW and the rate of seroconversion. Kaplan‐Meier graphs were used to visualise the data, using the date of the first positive test as the time of seroconversion. Patients who did not have a positive test during the period of follow up were censored at the time of the last visit.
All statistical analyses were undertaken using SPSS Version 12 or SAS Version 9.
Consent and ethics
Approval was obtained from the local research ethics committee. In the clinic, baseline data were requested as part of the registration visit and therefore signed consent was not sought. Screening was conducted with appropriate counselling and consent; infections were managed according to standard clinic protocol.
Results
Sample and demographics
Between September 1994 and December 2003, 823 men attended the project. During the follow up period 628 men completed a total of 1379 person years of follow up (median 16 months, range 2 months to 9.8 years).
Baseline characteristics are shown in table 1.
Table 1 Baseline characteristics of men using the Working Men's Project, 1994 to 2003.
| n = 823 (%) | ||
|---|---|---|
| Age (years) | ||
| Range | 15–59 | |
| Mean (SD) | 25.4 (5.4) | |
| Under 18 | 12 (1.5) | |
| Missing | 0 | |
| Country of birth | ||
| UK | 304 (37.2) | |
| Other western Europe | 207 (25.3) | |
| Eastern/Central Europe | 42 (5.1) | |
| South/Central America | 128 (15.6) | |
| Asia | 27 (3.3) | |
| Australia | 46 (5.6) | |
| Africa | 43 (5.3) | |
| Other | 21 (2.6) | |
| Missing | 5 | |
| Orientation | ||
| Homosexual | 625 (77.1) | |
| Bisexual | 145 (17.9) | |
| Heterosexual | 41 (5.1) | |
| Missing | 12 | |
| Months in sex work | ||
| Range | 0–240 | |
| Median (IQR) | 10 | |
| Missing | 24 | |
| Age sex work | ||
| 16 or under | 4 (0.5) | |
| 17–19 | 66 (8.0) | |
| 20–29 | 611 (74.2) | |
| 30 or older | 142 (17.3) | |
| Range | 15–59 | |
| Median (IQR) | 24.5 | |
| Missing | 0 | |
| Past STI* | ||
| Gonorrhoea | 178 (21.6) | |
| Chlamydia/NSU | 160 (19.5) | |
| Genital herpes | 36 (4.4) | |
| syphilis | 16 (1.9) | |
| Any† | 390 |
IQR, interquartile range; NSU, non‐specific urethritis.
*Past STI based on self report
†Gonorrhoea, chlamydia, trichomoniasis, genital herpes, genital warts, syphilis.
Over the three time periods there were no changes in age, duration of sex work, or age at first sex work. Over time the proportion of the men who had been born in the United Kingdom fell from 44.3% (102/230) in the years 1994 to 1996 to 30.7% (96/313) in 2000 to 2003 (p = 0.001). The biggest increases were seen in sex workers from South/Central America and east Europe, rising from 9% to 33% and 0.3% to 8%, respectively.
Overall, 76% (622/823) self identified as homosexual, 18% (146/823) were bisexual, 5% (41/823) heterosexual, and 1% (14/823) were not known. The pattern of self assigned sexual orientation changed over time. The number of homosexuals decreased from 188/230 (81.7%) in 1994 to 1996 to 222/310 (71.6%) in 2000 to 2003 with a corresponding rise in heterosexuals (2.6% (6/230) in 1994 to 1996 to 8.4% (26/331) in 2000 to 2003) and bisexuals (15.7% (36/230) in 1994 to 1996 to 19.9% (62/311) in 2000 to 2003 (p = 0.004)). It should be noted that of those originating from eastern Europe and South/Central America the numbers identifying as being heterosexual were higher than their UK and western European born counterparts: 26.2% (11/42) and 10.9% (13/120), respectively, versus 3% (9/305) and 1.9% (4/207).
Sex work health and safety
The majority of men (792, 96%) reported sex with male clients solely, 11 (1%) with male and female clients, three (<1%) with female clients exclusively; in 17 (2%) cases it was not documented. The median number of female clients and male clients in the preceding month was two (range 0–36) and 20 (range 0–250), respectively. When questioned about condom use with their previous four male clients 96% (508/528) reported consistent condom use for anal sex. There has been a small but not statistically significant increase in the proportion of MSWs selling unprotected anal sex over time (1994 to 1996, 3/218 (1.4%); 1997 to 1999, 7/260 (2.7%); 2000 to 2003, 11/294 (3.7%); p = 0.105). More men (562/771, 72.9%) reported unprotected oral intercourse (UPOI) with clients. There has been no change in the proportion of MSWs reporting having UPOI in the study period.
Non‐commercial partnerships
The majority of men reported non‐commercial partners. Almost half (369 45%) had a regular partner, 317 (86%) had only male partners, 50 (14%) only female partners, and two reported both male and female regular partners. Condom use with these regular partners was inconsistent: 38 (73%) of the 52 men with regular female partners reported unprotected vaginal sex, 10 (19%) protected vaginal sex, two (4%) were not having vaginal sex, and in two cases (4%) it was not documented. Of the 319 MSWs with regular male partners 128 (40%) were having protected anal sex, 117 (37%) unprotected anal sex, 57 (18%) did not have anal sex, and in 17 cases (5%) it was not documented. The most recent recruits (2000–2003) are more likely to have reported unprotected anal intercourse (UPAI) with their regular male partners than in previous years (36/114 (31.6%) in 1994 to 1996, 30/120 (25%) in 1997 to 1999; 55/131 (42.0%) in 2000 to 2003; p = 0.015). There is a significant increase in the proportion of MSWs whose regular partners are female: 11/114 (9.6%) in 1994 to 1996 to 25/134 (18.7%) in 2000 to 2003; p = 0.024).
The median number of casual male partners in the preceding month was two (range 0–50). Out of the 587 MSWs who reported having sex with at least one non‐commercial casual male partner (CMPs) in the last month 314 (53%) had protected anal sex, 66 (11%) had one or more episodes of unprotected anal sex, and 207 (35%) had no anal sex. The rate of unprotected anal sex with casual male partners steadily increased in the study period: 7.4% (13/176) in 1994 to 1996; 10.3% (21/203) in 1997 to 1999; and 15.7% (33/210) in 2000 to 2003 p = 0.01).
Mental health issues
A high proportion (699/823, 85%) reported having taken recreational drugs, including 33 (5%) who had used crack and 71 (10%) who had injected. One in five (163/815) reported previous mental illness including 35 who had attempted suicide. Twenty one per cent (170/808) reported a history of sexual abuse either as a child or an adult.
Prevalence and incidence of infections
HIV
The prevalence of HIV at baseline was 9.3% (59/636) (table 2).
Table 2 Baseline prevalence and incidence of infections*.
| Number tested | Number positive | Prevalence (%) | Person years of follow up | Incident cases | Incidence (per 100 person years) | |
|---|---|---|---|---|---|---|
| HIV | 636 | 59 | 9 | 1309 | 49 | 3.7 |
| Hepatitis C | 361 | 10 | 3 | 1395 | 7 | 0.5 |
| Hepatitis B | 797 | 155 | 19 | N/A | ||
| Syphilis | 748 | 16 | 21 | 1395 | 17 | 1.2 |
| Gonorrhoea | 748 | 68 | 9 | 1395 | 195 | 13.9 |
| Chlamydia | 748 | 56 | 7 | 1395 | 109 | 7.8 |
*See text for methods of calculating incidence.
Factors associated with prevalent HIV are shown in table 3 and include earlier year of recruitment, older age, self identifying as homosexual or bisexual, and a history of injecting drug use (table 3).
Table 3 Factor associated with being HIV positive at baseline (univariate analysis).
| Prevalence of HIV (%) | p Value | |
|---|---|---|
| Year group of recruitment | ||
| 1994 to 1996 | 22/156 (14.1) | 0.04 |
| 1997 to 1999 | 14/223 (6.3) | |
| 2000 to 2003 | 23/257 (8.9) | |
| Country of birth | ||
| UK | 22/212 (10.4) | 0.508 |
| other | 37/423 (8.7) | |
| Age | ||
| 15–19 years | 1/60 (1.7) | 0.001* |
| 20–24 years | 18/267 (6.7) | |
| 25–29 years | 26/212 (12.3) | |
| ⩾30 years | 14/97 (14.4) | |
| Sexual orientation | ||
| Homosexual | 53/477 (11.1) | 0.001 |
| Bisexual | 4/121 (3.3) | 0.006 |
| Heterosexual | 1/32 (3.1) | 0.167 |
| History of IDU | ||
| Yes | 16/60 (26.7) | <0.001 |
| No | 41/570 (7.2) | |
| Time in sex work | ||
| <6 months | 17/316 (5.4) | 0.001* |
| 7–12 months | 9/100 (9.0) | |
| 13–24 months | 13/109 (11.9) | |
| >2 years | 15/95 (15.8) | |
| UPAI with casual partner | ||
| Yes | 12/58 (20.7) | 0.005 |
| No | 31/393 (7.9) | |
| UPAI with client | ||
| Yes | 3/18 (16.7) | 0.25 |
| No | 48/586 (8.2) |
IDU, injecting drug use; UPAI, unprotected anal intercourse.
*Test for trend.
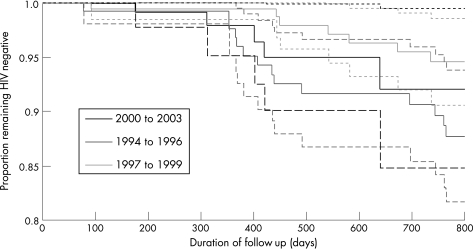
In multivariate analysis, including the above variables, only injecting drug use and reporting unprotected sex with a casual partner remained significantly associated with HIV. During follow up there were 49 incident cases of HIV. To account for the different times in follow up we used survival analysis to test for factors associated with seroconversion. The only factor significantly increasing the rate of seroconversion was first attending the clinic between 1994 to 1996 compared with men attending for the first time between 1997 and 1999 (p = 0.007) or between 2000 and 2003 (p = 0.02) (fig 1).
Figure 1 Kaplan‐Meier curve demonstrating the proportion of male sex workers remaining HIV negative according to year first attended the clinic.
Bacterial STIs
The baseline prevalence of gonorrhoea (from any site) significantly increased over the study period: 14/210 (6.7%) 1994 to 1996, 18/259 (6.9%) 1997 to 1999, and 36/279 (12.9%) in 2000 to 2003; p = 0.013). Prevalent gonorrhoea infection was more common in men who identified as homosexual or bisexual (66/699, 9.4%) than heterosexual (1/41, 2.4%), but this was not statistically significant. The prevalence of chlamydia (from any site) and primary and/or secondary syphilis did not change significantly over time.
Discussion
This observational cohort has shown that there have been significant changes in country of birth, self identified sexual orientation, sexual risk taking behaviour, and prevalence of gonorrhoea over the 10 year period. In particular, there has been a decline in the proportion of men who had been born in the United Kingdom with an associated increase in the proportion of MSWs whose regular partners are female, from 9.6% in 1994 to 1996 to 18.7% in 2000 to 2003. This is associated with changes in origin, with those men in the study who were from eastern Europe being more likely than United Kingdom or western European born men to identify as bisexual or heterosexual. Only half of eastern Europeans are self identified as homosexual.
The prevalence of HIV infection in homosexual and bisexual men in the United Kingdom is currently 7%, with the incidence of HIV infection being 3.5% nationally.23 The prevalence of HIV in this cohort overall was higher at 9% (9.5% in those self defining as homosexual or bisexual); the incidence in our study population was similar (at 3.7%), although it was calculated differently. We found a higher incidence of HIV in men presenting in the early (1994 to 1996) than the later years. The sample was not large enough to establish other independent risk factors for changes in HIV, but the data are compatible with the hypothesis that the temporal decline is the result of changing characteristics of the sex workers, including a decline in the proportion of homosexual identified men in the later groups.
The rates of gonorrhoea increased over time reflecting the national increase in bacterial STIs and increasing sexual risk behaviours demonstrated in this cohort and nationally.24 The rise in unprotected anal intercourse with regular, paying and non‐paying partners, together with the sustained rates of unprotected vaginal intercourse with regular female partners and concurrency, demonstrates the potential for onward transmission of infections to men and women.
There were several limitations to our study. We assume some selection bias in our study as we relied on a sample of clinic attendees, who would be more likely to be symptomatic and who may not adequately represent all types of MSWs in London. While this will have been limited by the outreach to sex work venues, it is likely that some bias will remain. Changes in diagnostic methods over time may also have affected our comparisons; tests for chlamydia have become more sensitive and therefore we may be underestimating the initial prevalence. While subjects with positive STI results and those requiring vaccinations were recalled, nearly 20% of participants were lost to follow up. Hence, the incidence estimation is likely to be biased. However, MSWs are a “hidden and elusive” population and it is unlikely that a lower lost to follow rate over such a long period of time is possible. Finally, while data collection was prospective, the healthcare professionals changed and this may have led to inconsistencies in recording. We tried to minimise further bias through carrying out coding in a consistent way at the end of the study period.
In previous studies there have been conflicting findings on sexual self identification as a correlate of HIV risk among MSWs.24,25 In our cohort the demographic shift in region of birth and self assigned sexual orientation have led to a greater number of self identifying heterosexual MSWs and a decline in the overall risk of HIV. This finding, however, must be counterbalanced with the number of sexual partners, the greater rates of sexual risk behaviour being taken when MSWs have sex with men, the increasing numbers of MSWs who have regular female partners with whom they are having unprotected vaginal sex, and the increase in rates of gonorrhoea in the sample.
In our cohort although HIV risk declined over time it remains high and, coupled with a significant increase in baseline prevalence of gonorrhoea, is a cause of concern. Condom use for anal sex with clients appears to be high, however, rates of UPAI with clients and non‐commercial partners have increased, as has the number of regular female partners with whom they report unprotected vaginal sex. It is crucial that policy makers and specialist sexual services are aware of the changing risk behaviours of sex workers in the local work force and the social and/or political reasons behind it if they hope to provide successful risk reducing sexual health interventions.
Contributors
GS conceived the study, collected and analysed the data, and drafted the manuscript; HW helped with the design of the study, statistical analysis, interpretation of the data, and critical review of the manuscript; ACG performed further statistical analysis; JG and BMH collected data; all authors reviewed the manuscript.
Abbreviations
CMPs - casual male partner
EIA - enzyme immunoassay
ELISA - enzyme linked immunosorbent assay
FTA - fluorescent treponemal antibody
MSWs - male sex workers
NGU - non‐gonococcal urethritis
NSU - non‐specific urethritis
RPR - rapid plasma reagin
STI - sexually transmitted infections
TPHA - Treponema pallidum haemagglutination assay
UPAI - unprotected anal intercourse
UPOI - unprotected oral intercourse
References
- 1.Day S, Ward H. Sex workers and the control of sexually transmitted disease. Genitourin Med 199773161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tomlinson D, Hillman R, Harris J R W.et al Screening for sexually transmitted disease in London‐based male prostitutes. Genitourin Med 199167103–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elifson K, Boles J, Swent M. Risk factors associated with HIV infection among male prostitues. Am J Public Health 19938379–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coutinho R, van Andel R, Rijsdijk T. Role of male prostitutes in spread of sexually transmitted diseases and human immunodeficiency virus. Genitourin Med 198864207–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Belza M, Llacer A, Mora R.et al Sociodemographic characteristics and HIV risk behaviour patterns of male sex workers in Madrid, Spain. AIDS Care 200113677–682. [DOI] [PubMed] [Google Scholar]
- 6.Pleak R, Meyer‐Bahlburg H. Sexual behaviour and AIDS knowledge of young male prostitutes in Manhattan. J Sex Res 199027557–587. [Google Scholar]
- 7.Waldorf D, Murphy S. Intravenous drug use and syringe sharing practices of call men and hustlers. In: Plant M, ed. AIDS, drugs and prostitution. London: Tavistock/Routledge 1990109–131.
- 8.Boles J, Elifson K. Sexual identity and HIV: the male prostitute. J Sex Res 19943139–46. [Google Scholar]
- 9.Thomas J C, Tucker M J. The development and use of the concept of a sexually transmitted disease core. J Infect Dis 1996174S134–S143. [DOI] [PubMed] [Google Scholar]
- 10.Moses S, Plummer F A, Ngugi E N.et al Controlling HIV in Africa: effectiveness and cost of an intervention in a high‐frequency STD transmitter core group. AIDS 19915407–411. [PubMed] [Google Scholar]
- 11.Aral S O, Holmes K K. Epidemiology of sexual behaviour and STD. In: Holmes KK, et al eds. Sexually transmitted diseases. 2nd ed. New York: McGraw Hill, 1990
- 12.Morse E, Simon P, Ofosky H.et al The male street prostitute: a vector for transmission of HIV infection into the heterosexual world. Soc Sci Med 19915535–539. [DOI] [PubMed] [Google Scholar]
- 13.Mak R, Traen A, Claeyssens A.et al Hepatitis B vaccination for sex workers: do oureach programmes perform better? Sex Transm Infect 200379157–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Health Protection Agency Renewing the focus: HIV and other sexually transmitted infections in the United Kingdom in 2002. An update November 2003. London: Health Protection Agency, 2003
- 15.Stolte I G, Dukers N H, de Wit J B.et al Increase in sexually transmitted infections among homosexual men in Amsterdam in relation to HAART. Sex Transm Infect 200177184–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fenton K A, Rogers P A, Simms I.et al Increasing gonorrhoea reports—not only in London. Lancet 20003551907. [DOI] [PubMed] [Google Scholar]
- 17.Donovan B, Bodsworth N J, Rohrsheim R.et al Increasing gonorrhoea reports—not only in London. Lancet 20003551908. [PubMed] [Google Scholar]
- 18.Chen S Y, Gibson S, Katz M H.et al Continuing increases in sexual risk behavior and sexually transmitted diseases among men who have sex with men: San Francisco, Calif, 1999–2001, USA. Am J Public Health 2002921387–1388. [PMC free article] [PubMed] [Google Scholar]
- 19.Dukers N H, Goudsmit J, de Wit J B.et al Sexual risk behaviour relates to the virological and immunological improvements during highly active antiretroviral therapy in HIV‐1 infection. AIDS 200115369–378. [DOI] [PubMed] [Google Scholar]
- 20.The EPI‐VIH Study group HIV infection among people of foreign origin voluntarily tested in Spain. A comparison with national subjects. Sex Transm Infect 200278250–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hiltunen‐Back E, Haikala O, Kosela P.et al Epidemics due to imported syphilis in Finland. Sex Transm Dis 200229746–751. [DOI] [PubMed] [Google Scholar]
- 22.D'Atuono A, Andola F, Carla E M.et al Prevalence of STDs and HIV infection among immigrant sex workers attending sex workers attending an STD centre in Bologna, Italy. Sex Transm Infect 200177220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Health Protection Agency HIV and other sexually transmitted infections in the United Kingdom in 2002. Annual Report. London: Health Protection Agency, 2003
- 24.Williams M L, Timpson S, Kovdal A.et al HIV risk among a sample of drug using male sex workers. AIDS 2003171402–1404. [DOI] [PubMed] [Google Scholar]
- 25.Deren S, Estrada A, Stark M.et al A multisite study of sexual orientation and injection drug use as predictors of HIV serostatus in out‐of‐treatment male drug users. J AIDS 199715289–295. [DOI] [PubMed] [Google Scholar]