Abstract
Objectives
To describe the characteristics of sex workers accessing care at a peer based clinic in San Francisco and to evaluate predictors of sexually transmitted infections (STI).
Methods
We conducted an observational study of sex workers at St James Infirmary. Individuals underwent an initial questionnaire, and we offered screening for STI at each clinic visit. We performed univariate, bivariate, and multivariable analyses to assess for predictors of STI in this population.
Results
We saw 783 sex workers identifying as female (53.6%), male (23.9%), male to female transgender (16.1%), and other (6.5%). 70% had never disclosed their sex work to a medical provider. Participants represented a wide range of ethnicities, educational backgrounds, and types of sex work. The most common substance used was tobacco (45.8%). Nearly 40% reported current illicit drug use. Over half reported domestic violence, and 36.0% reported sex work related violence. Those screened had gonorrhoea (12.4%), chlamydia (6.8%), syphilis (1.8%), or herpes simplex virus 2 (34.3%). Predictors of STI included African‐American race (odds ratio (OR) 3.3), male gender (OR 1.9), and sex work related violence (OR 1.9). In contrast, participants who had only ever engaged in collective sex work were less likely to have an STI (OR 0.4).
Conclusions
The majority of sex workers have never discussed their work with a medical provider. Domestic violence is extremely prevalent as is work related violence. Working with other sex workers appears to be protective of STIs. STI prevention interventions should target African‐American and male sex workers. Addressing violence in the workplace and encouraging sex workers to work collectively may be effective prevention strategies.
Keywords: sex work, sexually transmitted diseases, drug use, transgender health, violence
In June of 1999, the St James Infirmary (SJI) began providing free medical services for male, female and transgender sex workers in the San Francisco Bay Area. Leaders from the sex worker community, in collaboration with the San Francisco Department of Public Health STD Prevention and Control Section, started the clinic.1,2,3 The stated mission of SJI is to provide compassionate and non‐judgmental health care and social services for all sex workers while preventing occupational illnesses and injuries through a comprehensive continuum of services.4 SJI is a weekly, peer based clinic, with the majority of staff and board members being former or current sex workers. The clinic uses a harm reduction approach, with an emphasis on engaging sex workers in addition to identifying and reducing the individual and community level risks associated with sex work.5 Services offered include primary medical care, HIV and STI screening and treatment, transgender health, harm reduction and peer counselling, psychiatric evaluation and management, acupuncture, massage, support groups, food, clothing, and needle exchange. Additionally, clinic staff distributes safer sex supplies and offers HIV testing to sex workers in the setting of street and venue based outreach.6 The purpose of this study is to describe the characteristics of sex workers accessing health care at this specialty sex worker clinic and to evaluate predictors of sexually transmitted infections (STI) among those sex workers testing for gonorrhoea, chlamydia, syphilis and herpes simplex virus 2 (HSV‐2).
Methods
Since September 1999, we have been conducting an ongoing, prospective evaluation of all individuals accessing care at SJI. We limited this analysis to those current or past sex workers who sought care at SJI between September 1999 and November 2004. We defined sex work as the provision of sexual services or performances in exchange for money or goods of economic value including but not limited to drugs, housing, and food.7 Peer counsellors administered a structured intake questionnaire to sex workers during their initial visit to SJI. The questionnaire ascertained demographics, sex work history, drug use, social support, legal history, and violence. We modified the questionnaire in September 2001 to include additional questions about previous HIV and STI diagnoses, past drug use, and mental health history.
STI testing
At the initial and any subsequent clinic visits, SJI staff offered voluntary screening for STI to all clinic patients. The medical providers and/or harm reduction counsellors decided which test(s) to obtain based on patient request and clinical judgment. In particular, all individuals reporting unprotected oral, vaginal, and/or anal intercourse were encouraged to undergo STI screening. There were no set screening intervals. Screening included pharyngeal, rectal, and urine based chlamydia (CT) and gonorrhoea (GC) nucleic acid amplification tests (LCx, Abbott Labs and BDProbeTec, Becton Dickinson) as well as syphilis (Venereal Disease Research Laboratory Slide Test (VDRL) with confirmatory SerodiaTP‐PA, Fujirebio, Inc) and HSV‐2 antibodies (HerpeSelect 2 ELISA for HSV IgG, Focus Diagnostics).
Statistical analysis
Predictor variables included demographics, history of previous HIV and STI diagnosis, and behaviour self reported in the questionnaire. We analysed each type of sex work as a distinct predictor variable. For the purpose of multivariable analysis, we categorised the sex workers into three mutually exclusive groups—those who had engaged in exclusively independent sex work, both independent and collective sex work, and exclusively collective sex work. Independent sex work included street based, independent massage, independent in‐call/out‐call, sex trades, webcam based sex work, phone sex, and independent modelling. Collective sex work included massage parlours, escort, brothels, stripping, bondage‐dominatrix‐sado‐masochism (BDSM), and pornography. The main outcome variable was any positive chlamydia, gonorrhoea, syphilis, or HSV‐2 screening test. Some individuals underwent repeat STI screening, so we calculated the percentage of positive STI results as the proportion of unduplicated sex workers with any positive test among the total population of individuals testing. We performed univariate analysis, calculating proportions and means/medians for the demographic, health history and behavioural data, as appropriate. We then performed bivariate analysis, using the χ2 test or Fisher's exact test for categorical variables and Student's t test for continuous predictor variables. We assessed for multicollinearity and normal distribution. We performed logistic regression using forward stepwise technique including those variables with a p value <0.2 by bivariate analysis.8 A p value of <0.05 was considered statistically significant. We evaluated all models using likelihood ratio and goodness of fit tests and conducted all analyses using Stata SE 8.0 statistical software (College Station, TX, USA).
We obtained approval to conduct this study by the committee on human research at the University of California San Francisco.
Results
Overall, we conducted intake questionnaires on 783 sex workers who identified as female (53.6%), male (23.9%), male to female (MTF) transgender (16.1%), or other gender (6.5%). Of these 783 sex workers, 230 underwent the original intake questionnaire and the remaining 553 were administered the modified intake questionnaire. Table 1 shows the characteristics of participants.
Table 1 Participant characteristics.
| Variable | % (n) | Male (n = 187) | Female (n = 419) | MTF (n = 126) | Other (n = 51) | p Value |
|---|---|---|---|---|---|---|
| Median age (range) (n = 783) | 33.1 (17–76) | 33 (17–58) | 30 (17–76) | 35 (18–60) | 31 (18–76) | <0.01 |
| Race/ethnicity (n = 783) | <0.001 | |||||
| White | 58.4 (457) | 63.1 (118) | 62.8 (263) | 31.8 (40) | 70.6 (36) | |
| African‐American | 8.9 (68) | 9.1 (17) | 6.9 (29) | 14.3 (18) | 7.8 (4) | |
| Latino/a | 10.1 (79) | 9.6 (18) | 6.0 (25) | 24.6 (31) | 9.8 (5) | |
| Asian‐Pacific Islander | 8.6 (67) | 2.1 (4) | 11.0 (46) | 11.1 (14) | 5.9 (3) | |
| Native American | 1.8 (14) | 1.6 (3) | 1.7 (7) | 3.2 (4) | 0 | |
| Mixed/other | 12.5 (98) | 14.4 (27) | 11.7 (49) | 15.1 (19) | 5.9 (3) | |
| Highest level of education (n = 743) | (n = 167) | (n = 404) | (n = 124) | (n = 48) | <0.001 | |
| ⩽8th grade | 7 (52) | 3.0 (5) | 8.7 (35) | 8.9 (11) | 2.1 (1) | |
| High or technical school | 45.2 (336) | 41.3 (69) | 42.1 (170) | 60.5 (75) | 45.8 (22) | |
| College or grad school | 47.8 (355) | 55.7 (93) | 49.3 (199) | 30.6 (38) | 52.1 (25) | |
| Contact with family (n = 783) | 69.4 (543) | 68.4 (128) | 75.9 (318) | 51.6 (65) | 62.8 (32) | <0.001 |
| Presence of support network (n = 783) | 80.8 (633) | 77.5 (145) | 82.6 (346) | 81.0 (102) | 78.4 (40) | 0.51 |
| History of arrest (n = 757) | 49.4 (374) | 49.4 (81) | 43.7 (178) | 71.9 (87) | 40.8 (20) | <0.001 |
| Prostitution related conviction (n = 757) | 8.2 (62) | 4.4 (8) | 7.1 (29) | 19.0 (23) | 4.1 (2) | <0.001 |
| Partner/family violence (n = 783) | 53.4 (418) | 44.4 (83) | 55.1 (231) | 57.9 (73) | 60.8 (31) | <0.05 |
| Sex work related violence (n = 783) | 36.0 (282) | 26.7 (50) | 36.3 (152) | 53.2 (67) | 25.5 (13) | <0.001 |
| Customer | 27.8 (218) | 18.2 (34) | 28.4 (119) | 42.9 (54) | 21.6 (11) | <0.001 |
| Employer/manager/pimp | 9.1 (71) | 3.2 (6) | 12.4 (52) | 8.7 (11) | 3.9 (2) | <0.01 |
| Police | 8.4 (66) | 4.8 (9) | 7.9 (33) | 17.5 (22) | 3.9 (2) | 0.001 |
| Disclosure to medical provider (n = 714) | <0.05 | |||||
| Always | 12.6 (90) | 10.8 (18) | 11.7 (45) | 19.7 (23) | 8.9 (4) | |
| Sometimes | 17.4 (124) | 12.6 (21) | 17.4 (67) | 23.1 (27) | 20.0 (9) | |
| Never | 70.0 (500) | 76.6 (128) | 70.9 (273) | 57.3 (67) | 71.1 (32) |
MTF, male to female.
The mean age of participants was 33.1 (SD) 9.4; range 17–76), and this differed significantly by gender. Race/ethnicity and educational level also differed significantly by gender.
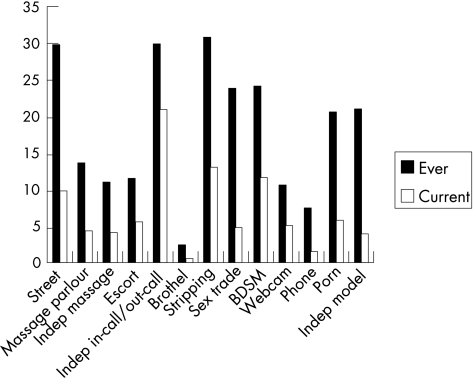
Sex work
As described in figure 1, clinic attendees participated in a diverse array of sex work activities including street based, massage parlour, independent sexual massage, escort, independent in‐call/out‐call, brothel, stripping/dancing, sex trades (for example, for housing, drugs, food), BDSM, webcam/internet, phone sex, pornography and independent modelling for customers. With sex specifically defined as oral, anal, vaginal intercourse, sharing sex toys, and/or manual stimulation, 95% of participants reported having sex as part of their sex work, and this finding did not differ by gender, though it vary by type of sex work. Strippers were less likely to have sex as part of their sex work (86.3%; p<0.001) as were those engaged in BDSM (85.7%; p<0.001).
Figure 1 Types of sex work.
Table 2 Health behaviour, STI history, and current STI.
| Variable | % (n) | Male | Female | MTF | Other | p Value‡ |
|---|---|---|---|---|---|---|
| Illicit drug use ever (n = 756) | 61.2 (463) | 71.3 (129) | 55.2 (224) | 64.5 (78) | 66.7 (32) | <0.01 |
| History of IDU (n = 756) | 22.9 (173) | 27.6 (50) | 16.3 (66) | 33.9 (41) | 33.3 (16) | <0.001 |
| Current use | ||||||
| Tobacco (n = 756) | 46.0 (348) | 48.6 (88) | 41.4 (168) | 57.0 (69) | 47.9 (23) | <0.05 |
| Any illicit drug (n = 755) | 39.6 (299) | 53.3 (96) | 35.7 (145) | 29.8 (36) | 45.8 (22) | <0.001 |
| Methamphetamines (n = 755) | 19.5 (147) | 29.8 (54) | 13.3 (54) | 24.8 (30) | 18.8 (9) | <0.001 |
| Heroin (n = 755) | 9.0 (68) | 8.3 (15) | 8.9 (36) | 8.3 (10) | 14.6 (7) | 0.57 |
| Cocaine/crack (n = 755) | 20.4 (154) | 27.1 (49) | 18.0 (73) | 17.4 (21) | 22.9 (11) | 0.06 |
| Current injection drug use (n = 756) | 7.9 (60) | 11.0 (20) | 5.9 (24) | 9.1 (11) | 10.4 (5) | 0.15 |
| Self reported infections* (n = 543) | ||||||
| Genital herpes | 9.6 (52) | 8.7 (11) | 12.3 (34) | 3.0 (3) | 10.3 (4) | <0.05 |
| Gonorrhoea | 14.4 (78) | 23.6 (30) | 10.1 (28) | 15.8 (16) | 10.3 (4) | <0.01 |
| Chlamydia | 13.4 (73) | 12.6 (16) | 17.4 (48) | 1.0 (1) | 20.5 (8) | <0.001 |
| Genital warts | 11.6 (63) | 7.9 (10) | 15.6 (43) | 6.9 (7) | 7.7 (3) | <0.05 |
| Syphilis | 5.0 (27) | 7.9 (10) | 1.8 (5) | 10.9 (11) | 2.6 (1) | 0.001 |
| HIV (n = 495) | 8.7 (43) | 16.0 (19) | 1.2 (3) | 20.0 (19) | 5.3 (2) | <0.001 |
| Any STI† (n = 456) | 105 (23) | 31.9 (36) | 17.9 (45) | 25.0 (18) | 30.0 (6) | <0.05 |
| Gonorrhoea† | ||||||
| Pharyngeal (n = 199) | 6.0 (12) | 8.8 (5) | 1.1 (1) | 10.3 (4) | 18.2 (2) | 0.01 |
| Rectal (n = 120) | 4.2 (5) | 7.3 (3) | 0 | 5.3 (2) | 0 | 0.50 |
| Urine (n = 421) | 1.9 (8) | 5.7 (6) | 0.4 (1) | 1.6 (1) | 0 | 0.01 |
| Chlamydia† | ||||||
| Pharyngeal (n = 171) | 0.6 (1) | 2.3 (1) | 0 | 0 | 0 | 0.50 |
| Rectal (n = 97) | 5.2 (5) | 3.4 (1) | 3.4 (1) | 8.8 (3) | 0 | 0.71 |
| Urine (n = 428) | 1.9 (8) | 3.7 (4) | 1.7 (4) | 0 | 0 | 0.43 |
| HSV‐2† (n = 230) | 34.8 (80) | 41.4 (24) | 30.4 (38) | 34.3 (12) | 50 (6) | 0.33 |
| Syphilis† (n = 387) | 1.8 (7) | 2.1 (2) | 0.9 (2) | 3.3 (2) | 5.3 (1) | 0.15 |
MTF, male to female; IDU, injecting drug use.
*These data were ascertained on the modified questionnaire only.
†Prevalence of any STI, gonorrhoea, chlamydia, HSV‐2, and syphilis was calculated as the proportion of individuals with any positive STI result among all individuals tested for each particular STI. Overall, 456 individual sex workers (58.2%) were tested for one or more STI.
‡We performed a Fisher exact test if fewer than five outcomes in any category, otherwise we used a χ2 test.
Social support
Overall, 69.4% of participants stated that they were in contact with their family, though MTF were less likely to be so. Eighty one per cent of sex workers reported having a support network or community. The presence of a network/community did not differ by gender but did by current type of sex work. Street based sex workers were less likely to have a network/community (60.0%; p<0.001). On the other hand, strippers were more likely to report having a network/community (93.1%; p = 0.001) as were those involved with BDSM (91.1%; p<0.05).
Legal history
Almost half of participants had been arrested in the past, with MTF sex workers more likely to be arrested and convicted of sex work related charges. Those most likely to be arrested included those involved with street based work (74.2%; p<0.001), sex trades (63.7%; p<0.001), and escort (65.2%; p<0.001).
Violence
Fifty three per cent of participants reported a history of family/partner violence. In addition, 36.0% reported a history of sex work related violence. MTF sex workers were at significantly higher risk of work violence, customer violence, and police violence. Also at higher risk of work related violence included those engaged in street based sex work (61.8%; p<0.001), sex trades (56.6%; p<0.001), massage parlours (48.1%; p = 0.01), and stripping (43.2%; p<0.05). Legal history was also significantly associated with violence, with 47.1% of those ever arrested experiencing work related violence compared to 25.9% of those without a history of arrest (p<0.001).
Table 3 Predictors of STI among sex workers: bivariate and multivariable analyses.
| STI testing | STI positive | Odds ratio (95% CI) | ||
|---|---|---|---|---|
| % (n) | % (n) | Unadjusted | Adjusted* | |
| All participants (n = 783) | 58.2 (456) | 23.0 (105) | ||
| Predictor variable (n) | ||||
| Ethnicity (783) | ||||
| African‐American (68) | 47.1 (32) | 50.0 (16) | 3.8 (1.8 to 7.8) | 3.3 (1.3 to 8.3) |
| White (457) | 58.4 (267) | 19.9 (53) | 0.7 (0.4 to 1.0) | |
| Latino/a (79) | 62.0 (49) | 28.6 (14) | 1.4 (0.7 to 2.7) | |
| Asian‐Pacific Islander (67) | 61.1 (41) | 17.1 (7) | 0.7 (0.3 to 1.5) | |
| Native American (14) | 50 (7) | 14.3 (1) | 0.6 (0.1 to 4.6) | |
| Mixed/other (98) | 61.2 (60) | 23.3 (14) | 1.0 (0.5 to 1.9) | |
| Gender (783) | ||||
| Male (187) | 60.4 (113) | 31.9 (36) | 1.9 (1.2 to 3.0) | 1.9 (1.0 to 3.6) |
| Female (419) | 59.9 (251) | 17.9 (45) | 0.5 (0.3 to 0.8) | |
| MTF (126) | 57.1 (72) | 25.0 (18) | 1.1 (0.6 to 2.0) | |
| Other (51) | 39.2 (20) | 30.0 (6) | 1.5 (0.5 to 3.9) | |
| Education (743) | ||||
| Middle school or less (52) | 55.8 (29) | 13.8 (4) | 0.5 (0.2 to 1.5) | |
| High or technical school (336) | 55.4 (186) | 21.5 (40) | 0.9 (0.6 to 1.4) | |
| College or grad school (355) | 61.7 (219) | 25.1 (55) | 1.3 (0.8 to 1.9) | |
| Type of sex work (ever) | ||||
| Independent only (218) | 56.9 (124) | 28.2 (35) | 1.5 (0.9 to 2.4) | |
| Collective and independent (336) | 62.5 (210) | 24.8 (52) | 1.2 (0.8 to 1.8) | |
| Collective only (143) | 55.9 (80) | 11.2 (9) | 0.4 (0.2 to 0.8) | 0.4 (0.1 to 0.9) |
| Violence | ||||
| Sex work related violence (282) | 1.9 (1.1 to 3.3) | |||
| Domestic violence (418) | 56.7 (237) | 24.9 (59) | 1.2 (0.8 to 1.9) | |
| Legal history | ||||
| History of arrest (374) | 54.5 (204) | 27.4 (56) | 1.6 (1.0 to 2.4) | |
| Sex work related conviction (62) | 56.4 (35) | 28.6 (10) | 1.4 (0.6 to 3.0) | |
| Drug use | ||||
| Tobacco use (current) (348) | 55.2 (192) | 27.6 (53) | 1.6 (1.0 to 2.4) | |
| Illegal drug use (current) (299) | 61.5 (184) | 21.2 (39) | 0.8 (0.5 to 1.3) | |
| Injection drug use (current) (60) | 51.7 (31) | 22.6 (7) | 1.0 (0.4 to 2.3) | |
*Final multivariable model built using forward stepwise technique, including variables significant at p<0.2 in bivariate analysis. The final multivariable model adjusted for age, race/ethnicity, educational level, category of sex work, current drug use, and history of sex work related violence.
Sex work disclosure
Seventy per cent of patients had never disclosed their sex work to a healthcare provider before their initial visit to SJI. MTF sex workers were significantly more likely to disclose to providers. The reasons for not disclosing one's sex work history included negative past experiences with disclosure (4.8%), fear of disapproval (31.2%), embarrassment (7.6%), and not thinking their sex work was relevant to their health needs (31.8%).
Drug use
The most common substance reported was tobacco, with 46.0% of participants currently smoking (table 2).
Nearly 40% of participants reported current illicit drug use. Male sex workers were the most likely to be actively using drugs, particularly methamphetamines. Although there were no gender differences in current injecting drug use (IDU), MTF were more likely to have a history of IDU and were more likely to be current smokers.
Self reported history of STI
Forty four percent of sex workers described a history of any STI, including genital herpes, gonorrhoea, chlamydia, genital warts, syphilis, non‐gonococcal urethritis, trichomonas, and pelvic inflammatory disease. In addition, 91.2% of patients had undergone HIV testing in the past, with 8.7% having tested positive. Prevalence of known HIV infection was highest among MTF and men.
Current STI
Overall, 58.2% of patients underwent testing for STI. Compared with those who did not test, STI testers were significantly younger (31.8 v 34.8 years old), though testing uptake did not differ by gender, current drug use, type of sex work, or ethnicity. Those with a known diagnosis of HIV, however, were significantly less likely to undergo STI screening (39.5%; p<0.01). Among testers, the proportion of those with at least one positive test included 34.3% for HSV‐2, 12.4% for gonorrhoea, 6.8% for chlamydia, and 1.8% for syphilis. In bivariate analysis, there was no association found between presence of an STI and educational level, drug use, domestic violence or violence in the setting of sex work.
African‐American sex workers were at highest risk of having an STI (50%; p<0.001) and, specifically, HSV‐2 (70.6%; p = 0.001). Those ever engaging in escort work were more likely to be diagnosed with any STI (35.7%; p<0.05), as were those engaging in phone sex (43.6%; p = 0.001). Another predictor of positive STI included a history of chlamydia (40.4%; p<0.05). Eighty per cent of those with a reported history of genital herpes were found to have antibodies against HSV‐2, and over 34% of those without a known history of genital herpes were found to have HSV‐2 antibodies (p<0.05). Lastly, those with a history of arrest were more likely to have an STI (27.4%; p<0.05).
In multivariable analysis, predictors of testing positive for an STI included African‐American race (OR 3.3; 95% confidence interval (CI) 1.3 to 8.3), male gender (OR 1.9, 95% CI 1.0 to 3.6), and having a history of sex work related violence (OR 1.9; 95% CI 1.1 to 3.3). On the other hand, those with a history of only engaging in collective sex work were significantly less likely to test positive for an STI (OR 0.4; 95% CI 0.1 to 0.9).
Discussion
By characterising sex workers seeking care at a peer based specialty clinic, we have gained a window into the diverse sex industry in San Francisco. The sex workers covered a wide range of socioeconomic and racial/ethnic backgrounds and engaged in an extensive array of types of sex work.9 Even defining sex work broadly, nearly all of these individuals, including strippers and phone sex workers, reported being sexually active in their sex work.
As has been seen in other studies, sex workers commonly reported illicit drug use.10 As we have demonstrated before, however, the most common substance used in this population was tobacco.11 Violence, particularly at the hands of partners and family members, was markedly common in the lives of the sex workers we studied.12 We also demonstrated the significant risk of customer, sex work employer/manager/pimp, and police related violence.12,13 Street based and sex trade sex workers had the highest risk of sex work violence. None the less, many types of “indoor” sex work, including massage and stripping, were also associated with an increased risk of work related violence.14
While nearly all participants had previously tested for HIV, the vast majority had never discussed their sex work history in the healthcare setting. In our study, both self reported history of STI and documented STI prevalence was, overall, lower than has been seen in other studies of urban sex workers.11,15,16,17 None the less, there were factors found to be associated with increased risk of STI in this population, including African‐American race, male gender, and sex work related violence. Furthermore, risk of STI differed significantly by type of sex work. Interestingly, those working collectively with other sex workers were less likely to have an STI.
While this study depicts the landscape of the sex industry in San Francisco, there certainly are limitations. In particular, we had limited information on specific sexual practices with different types of sexual partners and, thus, could not fully explore the complex set of factors that constitute STI risk. While we attempted to ascertain detailed sexual histories, many of the sex workers expressed difficulty in accurately quantifying the number of partners and sex acts. Another limitation of this study was the use of a convenience sample of sex workers accessing health care at a sex work specific clinic. This self selected population may not represent the larger population of female, male, and transgender sex workers in San Francisco and, therefore, estimates of STI prevalence may be biased. Furthermore, STI screening was offered to but not performed on all patients. Furthermore, repeat testing and the interval of such testing were, ultimately, decided by each individual patient.
Despite these limitations, there is value in assessing the local sex work environment and using this as the basis for public health interventions. Indeed, additional work must also be done to maximise the uptake of voluntary STI screening, particularly among HIV infected sex workers. This study suggests that STI prevention efforts in San Francisco must increasingly target sex workers who are African‐American, male, and work independently of other sex workers. Moreover, anti‐violence interventions should be an integral part of STI prevention. Our finding of decreased risk of STI among those individuals who have worked collectively with other sex workers is intriguing and warrants further study.
The St James Infirmary represents a novel collaborative effort between public health officials and the sex worker community. Through this unique model, sex workers have helped define public health priorities for their own community and public health officials have gained access to this hidden and stigmatised population.
Acknowledgements
We thank all the sex workers who participated in this study, the staff and volunteers at St James Infirmary, and the staff at City Clinic/Department of Public Health, including Wendy Wolf, Bob Kohn, Charlotte Kent, and Dr Will Wong.
Abbreviations
BDSM - bondage‐dominatrix‐sado‐masochism
CT - chlamydia
GC - gonorrhoea
HSV - herpes simplex virus
IDU - injecting drug use
MTF - male to female
SJI - St James Infirmary
STI - sexually transmitted infections
Footnotes
Funding: This study was supported by the National Institute for Drug Abuse (K23 DA01674), the Ford Foundation, the San Francisco Department of Public Health, and the University of California San Francisco School of Medicine Student Research Training Program.
References
- 1.Lutnick A. The St James Infirmary: a history. Sexuality Culture 200610(2) [Google Scholar]
- 2.Cohan D L, Breyer J, Cobaugh C.et alSocial context and the health of sex workers in San Francisco. In: XV International AIDS Conference. 2004
- 3.Cohan D L, Cloniger C, Breyer J.et al Sex worker health, San Francisco style: a peer‐based specialty clinic in San Francisco. In: National HIV Prevention Conference 2001
- 4. www.stjamesinfirmary.org
- 5.Rekart M L. Sex‐work harm reduction. Lancet 20053662123–2134. [DOI] [PubMed] [Google Scholar]
- 6.Breyer J, Cloniger C, Cohan D L.et al Training sex workers as disease prevention and health promotion and maintanence educators. In: National STD Prevention Conference 2002
- 7.Alexander P. Sex work and health: a question of safety in the workplace. J Am Med Women's Ass 19985377–82. [PubMed] [Google Scholar]
- 8.Bagley S C, White H, Golomb B A. Logistic regression in the medical literature: standards for use and reporting, with particular attention to one medical domain. J Clin Epidemiol 200154979–985. [DOI] [PubMed] [Google Scholar]
- 9.Harcourt C, Donovan B. The many faces of sex work. Sex Transm Infect 200581201–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harcourt C, van Beek I, Heslop J.et al The health and welfare needs of female and transgender street sex workers in New South Wales. Aust N Z J Public Health 20012584–89. [DOI] [PubMed] [Google Scholar]
- 11.Cohan D L, Kim A, Ruiz J.et al Health indicators among low income women who report a history of sex work: the population based Northern California Young Women's Survey. Sex Transm Infect 200581428–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Day S, Ward H. Violence towards female prostitutes. Violence in sex work extends to more than risks from clients. BMJ 2001323230. [PMC free article] [PubMed] [Google Scholar]
- 13.Potterat J J, Brewer D D, Muth S Q.et al Mortality in a long‐term open cohort of prostitute women. Am J Epidemiol 2004159778–785. [DOI] [PubMed] [Google Scholar]
- 14.Raphael J, Shapiro D L. Violence in indoor and outdoor prostitution venues. Violence Against Women 200410126–139. [Google Scholar]
- 15.Ward H, Day S, Weber J. Risky business: health and safety in the sex industry over a 9 year period. Sex Transm Infect 199975340–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ward H, Day S, Green A.et al Declining prevalence of STI in the London sex industry, 1985 to 2002. Sex Transm Infect 200480374–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wallace J, Porter J, Weiner A, Steinberg A. Oral sex, crack smoking, and HIV infection among female sex workers who do not inject drugs. Am J Public Health 199787470. [DOI] [PMC free article] [PubMed] [Google Scholar]