Abstract
Objective
To explore whether heterosexual bridging among syphilis‐positive men who have sex with men (MSM) contributes to increased infection rates among adolescent women in Baltimore City, Maryland.
Methods
Interview data for patients with primary, secondary and early‐latent syphilis from January 2001 to July 2005 were linked with their corresponding field records for named exposed contacts to assess prevalence of male bisexual activity and risk profiles of potential male bisexual bridgers and their female sex partners.
Results
None of the women with syphilis reported having known heterosexual relationships with a bisexual man. However, 3.9% and 11.0% of the male sex partners of adolescent females and women aged >25 years with syphilis, respectively, self‐reported as MSM or named male sex partners. Likewise, 10.3% of syphilis‐positive MSM named female sex partners and 3.0% of syphilis‐positive men who did not self‐identify as MSM named both male and female sex partners.
Conclusions
Sexual network links exist between syphilis‐positive MSM and heterosexual women, but the extent of bisexual behaviour among men is not detectable by self‐identification and disclosure to female sex partners.
Since the mid‐1990s syphilis rates in Baltimore City, Maryland, USA, have declined sharply. However, increases in early syphilis cases reported in recent years imply that a new epidemic may be emerging among men who have sex with men (MSM) and adolescent females.1 Such findings have raised questions about what additional prevention and control strategies are needed, and whether the recent outbreaks among these populations are linked.
Studies measuring the prevalence of bisexual behaviour among HIV‐positive MSM suggest that at least a small proportion of heterosexual transmission is due to sexual network links between MSM and heterosexual women.2,3,4,5 Further, they show that many bisexual men do not self‐identify as such and thus may not be readily targeted for intervention. Although much media attention has been given to men on the “down low” (ie those who identify as heterosexual, but also have male partners), undisclosed bisexuality is also true of other MSM.6,7 This report explores whether heterosexual bridging among syphilis‐positive MSM, regardless of sexual self‐identity, contributes to increased infection rates in young women.
Methods
Baltimore Syphilis Surveillance System data are collected by disease intervention specialists who conduct field investigations and interviews for index cases and infected partners. They record an extensive history, including demographics, pregnancy status, sexual risk behaviours, HIV status and testing, symptoms, and exposed sexual and needle‐sharing partners. Data are recorded on standard CDC forms and entered into the Baltimore City Health Department's STD MIS database.
Interview data for patients with primary, secondary and early‐latent syphilis from January 2001 to July 2005 were linked to their corresponding field records of named contacts. Frequency with which syphilis‐positive women reported having sex with a bisexual men, prevalence of bisexual activity among male partners of syphilis‐positive women and prevalence of bisexual activity among syphilis‐positive men who do and do not self‐identify as MSM, as well as risk profiles of potential male bisexual bridgers and their female sex partners, were assessed.
Results
Evidence of bridging
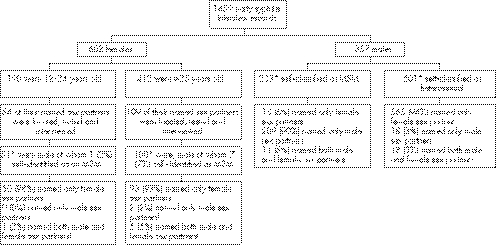
Figure 1 summarises the sexual partnership patterns based on the linking of interview and field records of syphilis‐positive 12–24‐year‐old females, women aged ⩾25 years, MSM and heterosexual men. None of the syphilis‐positive women reported having had known heterosexual relationships with a bisexual man as a risk factor. However, examination of interviews with the male sex partners of adolescent females showed one self‐reported MSM behaviour and one other named male sex partners. Thus, combining both methods of identification showed 3.9% of male sex partners of adolescent females as potential bisexual bridgers. Among interviewed male sex partners of women aged ⩾25 years, seven self‐reported MSM behaviour and seven named male sex partners. Of these, only three were the same men, thereby implicating 11.0% of male sex partners of women aged ⩾25 years as potential bisexual bridgers. Examination of interviews with named sexual partners of syphilis‐positive MSM showed that 10.3% also named female sex partners, of whom at least one third named a 12–24‐year‐old female sex partner. Among men who did not self‐identify as MSM, 3.0% named both male and female sex partners, of whom at least half named a 12–24‐year‐old female sex partner.
Figure 1 Summary of sexual partnership patterns based on the linking of interview and field records of syphilis‐positive adolescent females, women aged ⩾25 years, men who have sex with men (MSM) and heterosexual men. *Total after having de‐duplicated names. †Men who named male sexual partners were not necessarily the same as those who self‐identified as MSM.
Risk factors of potential male bisexual bridgers and their female sex partners
Unique people from all four analyses were combined to examine risk factors of men who are potential bisexual bridgers and their female sex partners. A total of 33% of both potential male bisexual bridgers and their female sex partners reported having engaged in high‐risk behaviours such as the exchange of sex for money or drugs, or cocaine or injection drug use.
Discussion
Although the data presented here do not allow us to measure the actual proportion of syphilis transmission that occurs between bisexual syphilis‐positive men and their female sex partners, they provide evidence of heterosexual bridging among MSM. For sexually transmitted infections, such as syphilis, where the incidence is low, identifying such potential transmitters is essential to eliminate the disease, and should continue to be the focus of future research. Our findings show that the extent of bisexual behaviour among men is not detectable by self‐identification and disclosure to female sex partners. More nuanced categorisations of MSM, including bisexual and down‐low categories, may need to be created and captured during data entry into syphilis surveillance systems. Such categories which are based on self‐identification and also on who are named as sex partners would aid in the identification of potential bisexual bridgers at whom prevention activities could be targeted.
Key Messages
Sexual network links exist between syphilis‐positive men who have sex with men (MSM) and heterosexual women
The extent of bisexual behaviour among men is not detectable by self‐identification and disclosure to female sex partners
More nuanced categorisations of MSM based on self‐identification and also on who respondents name as sex partners would aid in the identification of potential bisexual bridgers at whom prevention activities could be targeted
Acknowledgements
We thank the Disease Intervention Staff and Supervisors of the Baltimore City Health Department for their daily dedication to finding and eliminating disease. We also thank Rafiq Miazed and Sheridan Johnson for their assistance in this project.
Footnotes
Funding: This work was supported by the Centers for Disease Control Syphilis Elimination funding for the Baltimore City Health Department and NIAID RO‐1 AI45724.
Competing interests: None.
Contributors: SDC was responsible for the analysis and writing. GO and PB helped compile the data and assisted with writing. AMR and JME developed the project and contributed to the analysis and writing.
Ethical approval: The authors collected data during routine public health activities of disease control and analysed data for programme evaluation. This activity was therefore designated as public health practice and non‐research. In accordance with the Code of Federal Regulations, Title 45, Part 46, The Public Service Act, human subjects review is not required for public health non‐research activities.
References
- 1.Schumacher C M, Bernstein K T, Zenilman J M.et al Changes in demographics and risk behaviors of early syphilis cases depending on epidemic phase [abstract TO‐204]. Oral presentation at the 16 thInternational Society for Sexually Transmitted Diseases Research Conference, Amsterdam, The Netherlands 2005
- 2.Chu S Y, Peterman T A, Doll L S.et al AIDS in bisexual men in the United States: epidemiology and transmission to women. Am J Public Health 199282220–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kahn J G, Gurvey J, Pollack L M.et al How many HIV infections cross the bisexual bridge? An estimate from the United States. AIDS 1997111031–1037. [DOI] [PubMed] [Google Scholar]
- 4.Kalichman S C, Roffman R A, Picciano J F.et al Risks for HIV infection among bisexual men seeking HIV‐prevention services and risks posed to their female partners. Health Psychol 19984320–327. [PubMed] [Google Scholar]
- 5.Montgomery J P, Mokotoff E D, Gentry A C.et al The extent of bisexual behaviour in HIV‐infected men and implications for transmission to their female sex partners. AIDS Care 200315829–837. [DOI] [PubMed] [Google Scholar]
- 6.Denizet‐Lewis B. Double lives on the down low. The New York Times 3 Aug 2003
- 7.Villarosa L. AIDS fears grow for black women. The New York Times 5 Aug 2004