Abstract
Background
Non‐married persons are known to have poor mental health compared with married persons. Health differences between marital status groups may largely arise from corresponding differences in interpersonal social bonds. However, official marital status mirrors the social reality of persons to a decreasing extent, and living arrangements may be a better measure of social bonds. Little is known about mental health in different living arrangement groups. This study aims to establish the extent and determinants of mental health differences by living arrangement in terms of psychological distress (GHQ) and DSM‐IV psychiatric disorders (CIDI).
Methods
Data were used from the nationally representative cross sectional health 2000 survey, conducted in 2000–1 in Finland. Altogether 4685 participants (80%) aged 30–64 years were included in these analyses; comprehensive information was available on measures of mental health and living arrangements. Living arrangements were measured as follows: married, cohabiting, living with other(s) than a partner, and living alone.
Results
Compared with the married, persons living alone and those living with other(s) than a partner were approximately twice as likely to have anxiety or depressive disorders. Cohabiters did not differ from the married. In men, psychological distress was similarly associated with living arrangements. Unemployment, lack of social support, and alcohol consumption attenuated the excess psychological distress and psychiatric morbidity of persons living alone and of those living with other(s) than a partner by about 10%–50% each.
Conclusions
Living arrangements are strongly associated with mental health, particularly among men. Information on living arrangements, social support, unemployment, and alcohol use may facilitate early stage recognition of poor mental health in primary health care.
Keywords: living arrangements, marital status, psychological distress, psychiatric disorders
Variations in mortality and morbidity according to marital status have been widely reported, the married being in the most advantageous and the divorced in the most disadvantaged position.1,2,3 Regarding mental health differences, the divorced have the highest rates of psychological distress,4,5 and all non‐married groups have higher prevalences of depressive disorders and anxiety disorders compared with their married counterparts.6,7,8,9 In mental health, as in other aspects of ill health, the differences according to marital status are particularly pronounced in men.5,10
Mortality11,12,13 and morbidity2,14 are known to vary according to living arrangements independently of official marital status. Marital status mirrors the social reality and living arrangements of persons to a decreasing extent. For example, in Finland the proportion of cohabiters of all persons aged 15 to 64 living in union has increased from 10% in 1981 to 25% in 2000.15 Therefore, compared with official marital status, living arrangements may be a better indicator of real life social bonds. However, marital status should be taken into account in classification of living arrangements because marriage may represent stronger commitments to another person than cohabitation does.16,37 From the perspective of social bonds, living with someone else than a partner (that is, any “proximate other”), be it one's children, parent(s) or friend(s), may provide more daily social interaction than living alone, and should therefore be looked at as a separate class.
Less is known about the association between living arrangements and mental health. Cohabiting has been found to associate with psychological distress18 and depressive symptoms,17,37 but not with depressive disorders.7,29 Single parents have more psychological distress10 and psychiatric morbidity,6,19,20 and persons living alone, with parent(s) or with other(s) than a partner have high prevalences of psychiatric disorders compared with persons living with a partner.19 Living alone associates with high levels of psychological distress10 and depressive symptoms.21,22
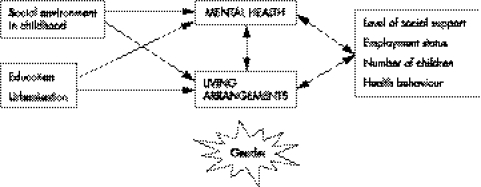
The social environment in childhood,20,23,24 education,25 employment status,6,7,8,10,25,26,27 number of children,6 urbanisation,7,28 level of social support,10,20,27,29 health behaviour,5,7 and gender6 are associated with mental health. These factors also tend to be connected with marital status and living arrangements,14,30 and therefore they may explain, mediate, or modify the association between mental health and living arrangements. We will consider the assumed causal order of the variables in interpreting their effects on the association between living arrangements and mental health. We hypothesise that adversities in childhood, education, and urbanisation usually precede both living arrangements and mental health problems and they may therefore partly explain the association between these two variables. Moreover, we hypothesise the level of social support to mediate the impact of living arrangements on mental health. Employment status, number of children, and health behaviour are expected to have a corresponding mediating role, but they also have other kinds of connections with the association between living arrangements and mental health, as these factors are known to affect both mental health and living arrangements and vice versa.3,5,6,14,20,29 In addition, gender may modify the associations. We present a simple model outlining the principal associations between these factors. Nevertheless, all these associations are likely to be reciprocal to some extent (fig 1).
Figure 1 Potential factors that may explain, mediate, or modify the association between living arrangements and mental health.
The purpose of this study was to find out whether there are mental health differences by living arrangement in the middle aged Finnish population in terms of psychological distress and psychiatric disorders. The second aim was to investigate whether living arrangement groups vary in terms of factors known to associate with poor mental health, and whether these variations contribute to living arrangement differences in mental health.
Methods
Data
We used data from the health 2000 survey, a nationally representative cross sectional study conducted in 2000–01 in Finland.4 The data were collected by computer aided interviews, self administered questionnaires, and a health examination, which included a structured mental health interview (CIDI). Our study concerned subjects aged 30 to 64, and in this age range the sample included 5871 subjects, of whom 4706 (80%) were interviewed with the CIDI. We excluded 21 persons with missing information on marital status or household size, and our final study population of 4685 people (2225 men, 2460 women) included 79.8% of the sample. For the analyses on the general health questionnaire (GHQ), 47 subjects were excluded because of missing or non‐valid data on the GHQ. Data on all variables included in the analyses were available for 4338 subjects (74%).
Living arrangements
We classified living arrangements into four groups: married, cohabiting, living with other(s) than a partner, and living alone. Of men living with other(s) than a partner, 34% lived in households with children aged less than 18 years, 58% were single, and 33% were divorced or separated. Regarding women living with other(s) than a partner, 79% lived in households with children and 62% were divorced. Thus most of the women in this group seemed to be single parents, while those living with their parents or in communes constituted a minority.
Mental health measures
The CIDI is a fully structured mental health interview that enables the assessment of 12 month prevalences of mental disorders according to the DSM‐IV.31 We used a Finnish translation of the German, computerised version of the CIDI (M‐CIDI).32 We grouped the DSM‐IV diagnoses into two overlapping categories. “Any depressive disorder” included major depressive disorder or dysthymic disorder, and “any anxiety disorder” included panic disorder, social phobia, agoraphobia, or generalised anxiety disorder.
We measured psychological distress using the 12 item version of the GHQ.33,34 It is a self report instrument including questions on current symptoms of depression, anxiety, sleep disturbance, and social functioning. The total score (range 0–12) was accepted only with 10 or more valid items. We dichotomised responses and set the caseness threshold between 3 and 4 GHQ points.
Both measures have been reported as having good psychometric properties.31,32,33,34
Adversities in childhood
Family structure was based on the question “when starting school (that is, when you were about 7 years old), did you live…” followed by four response alternatives “at home with both your parents”, “with only one parent”, “with relatives such as grandparents”, and “in an orphanage or other institution”. The last three alternatives were classified as “not living with both parents”.
Parental adversities were based on the question: “When you think about your growth years—that is, before you were aged 16…?” followed by a list of 11 adversities. We assessed questions on parents' divorce, serious conflicts within the family, father's/mother's drinking problems, and father's/mother's mental problems. “Parental adversity” was defined as reporting ⩾1 adversity.
Sociodemographic variables
Education was classified as basic (no matriculation examination and at most a vocational course or on the job training), intermediate or higher education (university qualification). In these classes, the average number of years of full time education was 8.7 years (SD 1.65), 12.8 years (SD 2.60), and 17.9 years (SD 2.77), respectively. Unemployment was defined as being currently unemployed or laid off. Urbanisation level was classified as (1) urban ( = 10 largest cities), (2) other urban or semi‐urban, and (3) rural municipalities. Subjects reporting ⩾1 child were defined as having children.
Social support
We conceptualised social support as emotional and practical help from others and social contacts.35 Availability of help from others was asked using the following questions: “Who do you think really cares about you no matter what happened to you?” and “From whom do you get practical help when needed?”. Several alternatives could be chosen: spouse/partner; other relative; friend; fellow worker; neighbour; no one. The categories “⩾2 persons”, “1 person” and “no one” were constructed from the total score.
Subjects were asked how often they visit family, friends, or neighbours, and how often these visit the subject. Social contacts were classified as “rare” if subjects answered “once or few times a year” or “less frequently or never” to either question.
Health behaviour
Smoking status was classified as (1) never smoked regularly, (2) former regular smoker, or (3) current occasional smoker or current regular smoker of cigarettes, tobacco, or pipe. Exercise was recorded by asking the following question: “How much do you exercise and strain yourself physically in your leisure time?” Subjects who chose the alternative reflecting least exercise were classified as “no exercise”. Alcohol consumption was recorded by asking separately about consumption of beer, wine, and spirits during the past month. For men, we used the categories of “no alcohol”, “1–23 portions/week”, and “⩾24 portions/week”, and for women “no alcohol”, “1–15 portions/week” and “⩾16 portions/week”, according to the recommended classification of excess alcohol use in Finland.36
Statistical methods
The analyses were carried out with the survey procedures of Stata (version 8.0), which take the sampling design into account (StataCorp, College Station, 2003). The age adjusted distributions of the explaining or mediating variables according to living arrangements and the prevalence of the mental health problems by these variables are presented in tables 1 and 2.
Table 1 Age adjusted prevalence (%) of social adversities in childhood and distribution (%) of sociodemographic variables, social support variables, and health behaviour by gender and living arrangement, age group 30 to 64 years.
| Variable | Women | Men | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Married | Cohabiting | Living with other(s) than a partner | Living alone | All | Married | Cohabiting | Living with other(s) than a partner | Living alone | All | |
| Age | ||||||||||
| 30–44 | 41 | 62 | 55 | 27 | 42 | 38 | 63 | 53 | 47 | 44 |
| 45–54 | 35 | 27 | 33 | 34 | 34 | 38 | 25 | 32 | 32 | 35 |
| 55–64 | 24 | 11 | 12 | 39 | 24 | 24 | 15 | 15 | 21 | 21 |
| p | <0.001 | <0.001 | ||||||||
| Family structure in childhood | ||||||||||
| Not living with both parents | 8 | 10 | 10 | 11 | 9 | 8 | 10 | 7 | 12 | 9 |
| p | 0.0916 | NS | ||||||||
| Parental adversity | ||||||||||
| ⩾1 adversity | 32 | 38 | 39 | 35 | 34 | 27 | 34 | 19 | 32 | 28 |
| p | 0.0926 | <0.001 | ||||||||
| Education | ||||||||||
| High | 14 | 11 | 11 | 17 | 14 | 15 | 7 | 5 | 8 | 12 |
| Medium | 59 | 57 | 54 | 56 | 58 | 59 | 58 | 58 | 54 | 58 |
| Low | 27 | 32 | 35 | 27 | 28 | 26 | 35 | 37 | 38 | 30 |
| p | <0.01 | <0.001 | ||||||||
| Urbanisation | ||||||||||
| Rural | 25 | 23 | 19 | 12 | 22 | 24 | 19 | 32 | 23 | 24 |
| Semi‐urban | 44 | 39 | 38 | 37 | 42 | 44 | 44 | 44 | 44 | 44 |
| Urban | 31 | 38 | 43 | 51 | 36 | 32 | 37 | 24 | 33 | 32 |
| p | <0.001 | <0.05 | ||||||||
| Unemployment | ||||||||||
| Yes | 8 | 12 | 19 | 12 | 10 | 5 | 5 | 16 | 18 | 8 |
| p | <0.001 | <0.001 | ||||||||
| Having children | ||||||||||
| No children | 7 | 25 | 11 | 49 | 17 | 7 | 27 | 51 | 58 | 22 |
| p | <0.001 | <0.001 | ||||||||
| Emotional help from others | ||||||||||
| ⩾2 persons | 71 | 67 | 47 | 52 | 65 | 53 | 55 | 31 | 34 | 49 |
| ⩾1 person | 28 | 31 | 51 | 45 | 33 | 45 | 42 | 64 | 58 | 48 |
| no help | 1 | 2 | 2 | 3 | 2 | 2 | 3 | 5 | 8 | 3 |
| p | <0.001 | <0.001 | ||||||||
| Practical help from others | ||||||||||
| ⩾2 persons | 67 | 59 | 47 | 52 | 62 | 58 | 49 | 33 | 33 | 51 |
| ⩾1 person | 31 | 38 | 52 | 44 | 36 | 39 | 46 | 61 | 56 | 44 |
| no help | 2 | 3 | 1 | 4 | 2 | 3 | 5 | 6 | 11 | 5 |
| p | <0.001 | <0.001 | ||||||||
| Social contacts | ||||||||||
| Rare | 20 | 24 | 24 | 23 | 22 | 31 | 36 | 40 | 38 | 34 |
| p | NS | <0.05 | ||||||||
| Smoking | ||||||||||
| Non‐smoker | 65 | 44 | 52 | 59 | 60 | 40 | 33 | 48 | 34 | 39 |
| Former smoker | 20 | 26 | 15 | 15 | 19 | 34 | 34 | 21 | 23 | 31 |
| Current smoker | 15 | 30 | 33 | 26 | 21 | 26 | 33 | 31 | 43 | 30 |
| p | <0.001 | <0.001 | ||||||||
| Alcohol consumption | ||||||||||
| no alcohol | 30 | 31 | 33 | 31 | 31 | 14 | 10 | 31 | 22 | 16 |
| 1–23 portions/week (1–15 in women) | 66 | 62 | 61 | 64 | 65 | 74 | 71 | 54 | 57 | 69 |
| ⩾24 portions/week (⩾16 in women) | 4 | 7 | 6 | 5 | 4 | 12 | 19 | 15 | 21 | 15 |
| p | NS | <0.001 | ||||||||
| Exercise | ||||||||||
| No | 22 | 26 | 27 | 24 | 23 | 26 | 26 | 27 | 28 | 27 |
| p | NS | NS | ||||||||
| crude numbers (not weighted) | n = 1517 (62%) | n = 317 (13%) | n = 225 (9%) | n = 401 (16%) | n = 2460 (100%) | n = 1399 (63%) | n = 310 (14%) | n = 139 (6%) | n = 377 (17%) | n = 2225 (100%) |
Table 2 Age adjusted prevalence (%) of psychological distress and psychiatric disorders by gender, living arrangement, and social adversities in childhood, sociodemographic variables, social support variables, and health behaviour, age group 30 to 64 years.
| Variable | Women | Men | ||||
|---|---|---|---|---|---|---|
| Depressive disorder* | Anxiety disorder* | GHQ⩾4† | Depressive disorder‡ | Anxiety disorder‡ | GHQ⩾4§ | |
| Living arrangement | ||||||
| Married | 7 | 4 | 18 | 4 | 3 | 14 |
| Cohabiting | 8 | 5 | 20 | 2 | 2 | 12 |
| Living with other(s) than a partner | 14 | 8 | 23 | 10 | 5 | 20 |
| Living alone | 14 | 6 | 21 | 9 | 8 | 24 |
| p | <0.001 | <0.05 | NS | <0.001 | <0.001 | <0.001 |
| Family structure in childhood | ||||||
| Living with both parents | 9 | 5 | 19 | 5 | 4 | 15 |
| Not living with both parents | 11 | 6 | 23 | 7 | 5 | 19 |
| p | <0.01 | 0.0942 | <0.01 | NS | NS | NS |
| Parental adversity | ||||||
| No | 8 | 4 | 16 | 4 | 3 | 13 |
| ⩾1 adversity | 12 | 7 | 26 | 9 | 5 | 22 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | 0.0570 | <0.001 |
| Education | ||||||
| High | 8 | 5 | 21 | 3 | 3 | 15 |
| Medium | 9 | 5 | 19 | 5 | 3 | 15 |
| Low | 9 | 6 | 18 | 5 | 6 | 17 |
| p | NS | NS | NS | NS | <0.05 | NS |
| Urbanisation | ||||||
| Rural | 10 | 4 | 20 | 6 | 4 | 15 |
| Semi‐urban | 8 | 5 | 18 | 4 | 4 | 15 |
| Urban | 10 | 6 | 20 | 6 | 5 | 16 |
| p | NS | NS | NS | NS | NS | NS |
| Unemployment | ||||||
| No | 9 | 5 | 18 | 5 | 3 | 14 |
| Yes | 13 | 8 | 24 | 11 | 13 | 34 |
| p | <0.05 | <0.05 | <0.05 | <0.001 | <0.001 | <0.001 |
| Having children | ||||||
| ⩾1 child | 9 | 5 | 19 | 5 | 4 | 15 |
| No children | 11 | 7 | 20 | 6 | 5 | 18 |
| p | NS | 0.0877 | NS | NS | NS | <0.05 |
| Emotional help from others | ||||||
| ⩾2 persons | 8 | 4 | 16 | 3 | 3 | 13 |
| ⩾1 person | 11 | 6 | 23 | 7 | 4 | 17 |
| no help | 19 | 20 | 47 | 15 | 13 | 41 |
| p | <0.05 | <0.001 | <0.001 | <0.001 | <0.01 | <0.001 |
| Practical help from others | ||||||
| ⩾2 persons | 7 | 4 | 17 | 3 | 3 | 13 |
| ⩾1 person | 11 | 6 | 22 | 7 | 5 | 17 |
| no help | 20 | 18 | 47 | 14 | 10 | 32 |
| p | <0.01 | <0.001 | <0.001 | <0.001 | <0.01 | <0.001 |
| Social contacts | ||||||
| Frequent | 8 | 4 | 18 | 4 | 3 | 13 |
| Rare | 14 | 9 | 25 | 7 | 5 | 20 |
| p | <0.001 | <0.001 | <0.01 | <0.01 | <0.05 | <0.001 |
| Smoking | ||||||
| Non‐smoker | 9 | 4 | 19 | 5 | 3 | 14 |
| Former smoker | 9 | 5 | 20 | 5 | 3 | 15 |
| Current smoker | 11 | 7 | 20 | 6 | 7 | 18 |
| p | NS | <0.05 | NS | NS | <0.001 | NS |
| Alcohol consumption | ||||||
| no alcohol | 10 | 5 | 19 | 10 | 7 | 19 |
| 1–23 portions/week (1–15 in women) | 8 | 5 | 19 | 4 | 3 | 13 |
| ⩾24 portions/week (⩾16 in women) | 16 | 9 | 24 | 6 | 6 | 23 |
| p | <0.05 | NS | NS | <0.001 | <0.001 | <0.001 |
| Exercise | ||||||
| Yes | 8 | 4 | 18 | 4 | 4 | 14 |
| No | 13 | 7 | 24 | 8 | 4 | 20 |
| p | <0.001 | <0.01 | <0.001 | <0.01 | NS | <0.001 |
| All | 9 | 5 | 19 | 5 | 4 | 16 |
*n = 2460. †n = 2440. ‡n = 2225. §n = 2198.
The variation in the prevalence of mental health problems by living arrangements was analysed with logistic regression, adjusting for age and the potential explaining or mediating variables first separately or in sets and finally all of them simultaneously (tables 3–5). Only variables that were associated with both living arrangements and mental health measures among either gender were considered (p<0.1). Interactions between living arrangements and all the other independent variables were examined by including interaction terms in the logistic models. As a significant interaction was found between gender and living arrangements in the case of psychological distress (p<0.05), all results are shown separately for men and women. The results are presented as odds ratios with 95% confidence intervals.
Table 3 Differences in the 12 month prevalence of any depressive disorder according to living arrangement, adjusting for age, and social adversities in childhood, unemployment, social support variables, and alcohol consumption, by gender, age group 30 to 64 years (odds ratios with 95%CI).
| Living arrangement | Adjusting for: | ||||||
|---|---|---|---|---|---|---|---|
| Age | Age+Family structure in childhood+Parental adversity | Age+Unemployment | Age+Emotional help from others+Practical help from others+Social contacts | Age+Alcohol consumption | All | ||
| OR | OR | OR | OR | OR | OR | ||
| 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | ||
| Women | |||||||
| Married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Cohabiting | 1.02 | 1.00 | 1.01 | 0.96 | 0.91 | 0.91 | |
| 0.62 to 1.69 | 0.60 to 1.68 | 0.61 to 1.67 | 0.57 to 1.59 | 0.53 to 1.55 | 0.53 to 1.54 | ||
| Living with other(s) than a partner | 1.99 | 2.01 | 1.92 | 1.88 | 2.02 | 1.89 | |
| 1.32 to 3.01 | 1.33 to 3.04 | 1.27 to 2.89 | 1.23 to 2.87 | 1.34 to 3.06 | 1.23 to 2.91 | ||
| Living alone | 2.01 | 1.86 | 1.98 | 1.76 | 1.79 | 1.66 | |
| 1.40 to 2.89 | 1.28 to 2.72 | 1.38 to 2.85 | 1.21 to 2.55 | 1.23 to 2.62 | 1.12 to 2.45 | ||
| Men | |||||||
| Married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Cohabiting | 0.62 | 0.59 | 0.61 | 0.62 | 0.64 | 0.59 | |
| 0.29 to 1.32 | 0.27 to 1.29 | 0.29 to 1.32 | 0.29 to 1.34 | 0.29 to 1.37 | 0.27 to 1.29 | ||
| Living with other(s) than a partner | 2.58 | 2.90 | 2.37 | 1.91 | 2.27 | 1.76 | |
| 1.32 to 5.02 | 1.50 to 5.64 | 1.19 to 4.70 | 0.92 to 3.98 | 1.15 to 4.50 | 0.83 to 3.77 | ||
| Living alone | 2.39 | 2.41 | 2.15 | 1.94 | 2.24 | 1.62 | |
| 1.60 to 3.57 | 1.60 to 3.64 | 1.42 to 3.26 | 1.25 to 3.00 | 1.49 to 3.38 | 1.01 to 2.62 | ||
Table 4 Differences in the 12 month prevalence of any anxiety disorder according to living arrangement, adjusting for age, and social adversities in childhood, education, unemployment, social support variables, and health behaviour, by gender, age group 30 to 64 years (odds ratios with 95%CI).
| Living arrangement | Adjusting for: | ||||||
|---|---|---|---|---|---|---|---|
| Age | Age+Family structure in childhood+Parental adversity | Age+Education | Age+Unemployment | Age+Emotional help from others+Practical help from others+Social contacts | Age+Smoking+Alcohol consumption | All | |
| OR | OR | OR | OR | OR | OR | OR | |
| 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | |
| Women | |||||||
| Married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Cohabiting | 1.14 | 0.93 | 1.12 | 1.12 | 1.15 | 1.03 | 0.92 |
| 0.64 to 2.02 | 0.49 to 1.76 | 0.63 to 2.00 | 0.63 to 1.99 | 0.65 to 2.03 | 0.57 to 1.87 | 0.49 to 1.72 | |
| Living with other(s) than a partner | 1.96 | 1.97 | 1.92 | 1.86 | 1.88 | 1.79 | 1.70 |
| 1.21 to 3.18 | 1.20 to 3.24 | 1.19 to 3.11 | 1.14 to 3.04 | 1.16 to 3.05 | 1.08 to 2.98 | 1.00 to 2.89 | |
| Living alone | 1.56 | 1.58 | 1.56 | 1.53 | 1.34 | 1.41 | 1.37 |
| 1.00 to 2.43 | 1.01 to 2.48 | 1.00 to 2.43 | 0.98 to 2.39 | 0.85 to 2.10 | 0.88 to 2.26 | 0.84 to 2.24 | |
| Men | |||||||
| Married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Cohabiting | 0.80 | 0.81 | 0.76 | 0.79 | 0.79 | 0.78 | 0.77 |
| 0.37 to 1.71 | 0.38 to 1.73 | 0.36 to 1.62 | 0.37 to 1.71 | 0.37 to 1.69 | 0.36 to 1.71 | 0.35 to 1.67 | |
| Living with other(s) than a partner | 1.70 | 1.83 | 1.60 | 1.37 | 1.46 | 1.47 | 1.25 |
| 0.76 to 3.81 | 0.81 to 4.14 | 0.70 to 3.65 | 0.60 to 3.10 | 0.63 to 3.39 | 0.64 to 3.40 | 0.52 to 2.98 | |
| Living alone | 2.89 | 2.96 | 2.71 | 2.26 | 2.50 | 2.25 | 1.79 |
| 1.85 to 4.51 | 1.88 to 4.66 | 1.74 to 4.22 | 1.41 to 3.62 | 1.58 to 3.94 | 1.42 to 3.59 | 1.09 to 2.94 | |
Table 5 Differences in the prevalence of psychological distress (GHQ⩾4) according to living arrangement, adjusting for age, economic and social adversities in childhood, sociodemographic variables, social support variables, and alcohol consumption, by gender, age group 30 to 64 years (odds ratios with 95%CI).
| Living arrangement | Adjusting for: | |||||||
|---|---|---|---|---|---|---|---|---|
| Age | Age+Family structure in childhood+Parental adversity | Age+Unemployment | Age+Children | Age+Emotional help from others+Practical help from others+Social contacts | Age+Alcohol consumption | All | ||
| OR | OR | OR | OR | OR | OR | OR | ||
| 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | ||
| Women | ||||||||
| Married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Cohabiting | 1.12 | 1.11 | 1.11 | 1.12 | 1.10 | 1.09 | 1.05 | |
| 0.81 to 1.54 | 0.81 to 1.54 | 0.80 to 1.52 | 0.81 to 1.55 | 0.79 to 1.52 | 0.79 to 1.51 | 0.74 to 1.48 | ||
| Living with other(s) than a partner | 1.35 | 1.37 | 1.30 | 1.35 | 1.25 | 1.36 | 1.22 | |
| 0.97 to 1.89 | 0.97 to 1.93 | 0.93 to 1.83 | 0.97 to 1.89 | 0.88 to 1.78 | 0.96 to 1.93 | 0.84 to 1.79 | ||
| Living alone | 1.23 | 1.24 | 1.21 | 1.24 | 1.09 | 1.17 | 1.06 | |
| 0.93 to 1.61 | 0.93 to 1.65 | 0.92 to 1.59 | 0.92 to 1.67 | 0.82 to 1.45 | 0.88 to 1.56 | 0.75 to 1.50 | ||
| Men | ||||||||
| Married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Cohabiting | 0.90 | 0.88 | 0.90 | 0.92 | 0.91 | 0.84 | 0.87 | |
| 0.61 to 1.33 | 0.60 to 1.30 | 0.60 to 1.33 | 0.61 to 1.38 | 0.61 to 1.35 | 0.57 to 1.26 | 0.57 to 1.31 | ||
| Living with other(s) than a partner | 1.64 | 1.79 | 1.46 | 1.72 | 1.47 | 1.51 | 1.43 | |
| 1.06 to 2.56 | 1.15 to 2.80 | 0.93 to 2.29 | 1.06 to 2.79 | 0.91 to 2.35 | 0.94 to 2.41 | 0.82 to 2.50 | ||
| Living alone | 2.01 | 1.94 | 1.74 | 2.08 | 1.75 | 1.74 | 1.43 | |
| 1.52 to 2.67 | 1.45 to 2.58 | 1.29 to 2.34 | 1.44 to 2.99 | 1.30 to 2.35 | 1.30 to 2.33 | 0.94 to 2.16 | ||
The percentage change in the association between living arrangements and mental health after adjusting for a specific variable was calculated as 100×(OR(base model)−OR(base model+variable))/(OR(base model)−1).
Results
The association between risk factors for mental health problems and living arrangements varied according to gender, but education, urbanisation, unemployment, having children, emotional and practical help from others, and smoking had significant associations in men and women (p<0.05) (table 1). Women had a higher prevalence of psychological distress (GHQ⩾4) and depressive and anxiety disorders than men (table 2). Living arrangement associated with all mental health measures except for psychological distress in women (p value 0.22). Unemployment, emotional and practical help from others and social contacts associated with all mental health measures in men and women. Current smokers had anxiety disorders more often than never and former smokers did. Education only associated with anxiety disorder in men. Family structure in childhood associated with poor mental health only in women. Urbanisation did not associate with any mental health measure, whereas sedentary life style associated with increased risk of psychological distress and depressive disorders.
What is already known on this topic
Non‐married persons are known to have poor mental health compared with married persons
Compared with married persons, persons living alone and those living with other(s) than a partner had high odds for depressive and anxiety disorders, with stronger associations in men (tables 3 and 4). The excess anxiety disorders in men living with other(s) than a partner did not reach statistical significance. Adjusting for unemployment reduced the excess morbidity by about 10%–50%, lack of social support by 10%–40%, and adverse health behaviour by 10%–35%. Adjusting for childhood adversities and education only had a very modest effect on the association between living arrangements and psychiatric morbidity, the only pronounced exception being the fact that childhood adversities accounted for 15% of the excess prevalence of depressive disorders among women living alone. Adjusting for all variables reduced the excess morbidity by about 50%–65% in men, but only about 10%–35% in women. Excess depressive disorders in men and women living alone and in women living with other(s) than a partner remained statistically significant, whereas odds for anxiety disorders remained significantly increased in men living alone and in women living with other(s) than a partner. In both sexes, education showed an interaction with living arrangements in the case of anxiety disorders (p<0.001). This interaction emerged from the fact that no anxiety cases were found in the small group of highly educated persons living with other(s) than a partner.
What this paper adds
Living arrangements are strongly associated with mental health, particularly among men.
Part of these differences are accounted for by differences in social support, unemployment, and alcohol consumption.
In women, the prevalence of psychological distress did not vary according to living arrangements, but among men, those living alone and those living with other(s) than a partner had excess psychological distress (table 5). After adjustment, the differences were no longer statistically significant. Unemployment, lack of social support, as well as alcohol consumption reduced the odds by about 20%–30% each. Among men, a significant interaction (p<0.05) was found between living arrangements and having children: living alone was associated with an increased risk of psychological distress only among those who had children.
In women, cohabiters had slightly higher odds for poor mental health, compared with the married, in terms of all measures of mental health, whereas cohabiting men had somewhat lower odds. However, these differences were not statistically significant.
Discussion
This study provides new information on the mental health of the growing population of non‐married persons in different living arrangements. Our dataset offers excellent opportunities for assessing the mental health of the Finnish population, as an array of background variables and reliable mental health measures were available.4 In our data, living arrangements were strongly associated with mental health. Compared with married persons, persons living alone and persons living with other(s) than a partner had high odds for psychological distress and psychiatric disorders, with stronger associations in men. Unemployment, lack of social support, as well as alcohol consumption attenuated the excess poor mental health of persons living alone and of those living with other(s) than a partner by about 10%–50% each, with greater effects in men.
Living arrangements
In line with previous studies, we found persons living alone to be disadvantaged by all mental health measures. Depressive and anxiety disorders,19 high GHQ scores,10 and depressive symptoms21,22 have been found to associate with living alone. Supporting our study, the associations have been stronger in men.21 Longitudinal studies are needed to find out the importance of two plausible but opposite causal pathways: persons with poor mental health being selected into living alone, and living alone causing poor mental health.
Policy implications
In primary health care, early stage recognition of poor mental health may be more successful with better information of people's immediate living arrangements.
Targeting of interventions—such as social support groups—to those in disadvantaged living arrangements (for example, bereaved persons, divorced persons, and persons living alone) may increase their effectiveness.
We did not find cohabiters to differ significantly from married persons. Some previous studies have reported that cohabiters have high levels of depressive and other psychological symptoms compared with the married,18,37 whereas significant differences have not been found in depressive disorders.7,29 Further work is needed on the mental health of the growing proportion of cohabiters.15
Persons living with other(s) than a partner had high odds for poor mental health. After adjustment, the probability of psychiatric disorders in women remained significantly increased. Previous studies indirectly support ours, as depressive disorders6,19,20 and anxiety disorders19 have been common in single parents.
Factors contributing to living arrangement differences in mental health
Childhood adversities were only weakly associated with living arrangements, and the level of education and urbanisation were not strongly connected with mental health. Consequently, these factors did not contribute to the high prevalence of mental disorders among persons who do not live with a partner. The only noticeable exception to this general finding was that childhood adversities accounted for a part of the excess prevalence of depressive disorders among women living alone.
The level of social support seemed to be a strong mediator of the impact of living arrangements on mental health. Not receiving practical or emotional help from anyone was most common in men and women living alone, and correspondingly, adjusting for social support reduced their excess mental health problems by about 20%–40%. The association between social support and mental health problems, particularly depression, may partly result from the impact of depression on one's self perception of social support. There is, however, also evidence based on longitudinal studies on the effect of social support on the risk of depression.38
Adjusting for unemployment attenuated the excess depressive and anxiety disorders in men living alone by 17%–33%, but it had very little effect on the psychiatric morbidity of women living alone. This is attributable to the small difference in the unemployment rate between married women and women living alone as well as the weaker association between unemployment and mental disorders among women than among men.
The number of children was not connected with the excess mental disorders among persons not living in a partnership, because having children was only weakly associated with mental disorders. Regarding psychological distress in men, a plausible explanation for the interaction between living alone and having children is that most (78%) of the men who lived alone but had children were divorced, and divorce has been shown to be associated with increased psychological distress.5,18
Health behaviours contributed to the associations between living arrangements and mental health. Of men and women living alone, 43% and 26%, respectively, were current smokers, and in separate analyses adjusting for current smoking attenuated their excess anxiety disorders by about 15%–20%. Moreover, excess alcohol consumption by men living alone contributed to their poor mental health by about 10%–30%.
Methodological considerations
Among the participants of the health 2000 survey, a considerable proportion of those not reliably interviewed with the CIDI suffered from psychological symptoms as measured by the Beck depression inventory and the GHQ.32 Among drop outs, there was an excess of persons living alone and of those living with other(s) than a partner.39 Thus, our results may underestimate differences in mental health between living arrangement groups.
In our sample, high GHQ scores associated strongly with depressive (OR 9.89, 7.73 to 12.65) and anxiety disorders (OR 8.54, 6.24 to 11.69). GHQ is a screening instrument that also detects subjects with current symptoms of diagnostically sub‐threshold disorders, whereas the CIDI application used in this study recognises full fledged DSM‐IV disorders. Mental health differences by living arrangements seemed to be smaller in psychological distress than in psychiatric disorders. In addition to differences in the severity of symptoms detected, this finding may be related to the different timeframe of the measures used; the CIDI measures 12 month prevalences, whereas the GHQ measures current psychological distress.
The cross sectional nature of our data did not enable the actual testing of the assumed causal ordering of the variables. Longitudinal data are needed to assess the complex associations between mental health, living arrangements, and associated factors. Moreover, a considerable part of the differences remained even after adjusting for all our variables. Thus, important explaining or mediating variables were not taken into account; such factors might include genetic risk factors40; traumatic life events or personality traits.24
Conclusions
Living arrangements are strongly associated with mental health, particularly among men. Part of these differences is associated with differences in social support, unemployment, and alcohol consumption. Previous studies on the efficacy of primary prevention programmes provide substantial evidence that depressive symptoms can be reduced.41 Our findings may be helpful in developing targeted prevention strategies to reduce mental health problems by locating population groups at particularly high risk, and by understanding the causes of these increased risks. In primary health care, early stage recognition and intervention on poor mental health may be more successful with better information of people's immediate living arrangements.
Footnotes
Funding: this work was funded by a grant from the Academy of Finland (No.203418), and a fellowship and a grant to Pekka Martikainen (70631, 210752).
Competing interest: none declared.
References
- 1.Martikainen P, Martelin M, Koskinen S.et al Differences in mortality by marital status in Finland from 1976 to 2000: analyses of changes in marital status distributions, socio‐demographic and household composition, and cause of death. Popul Stud (Camb) 20055999–115. [DOI] [PubMed] [Google Scholar]
- 2.Murphy M, Glaser K, Grundy E. Marital status and long‐term illness in Great Britain. J Marriage Fam 199759156–164. [Google Scholar]
- 3.Wyke S, Ford G. Competing explanations for associations between marital status and health. Soc Sci Med 199234523–532. [DOI] [PubMed] [Google Scholar]
- 4. Aromaa A, Koskinen S, eds. Health and functional capacity in Finland. Baseline results of the health 2000 health examination survey. Helsinki: Hakapaino Oy, 2004
- 5.Stansfeld S A, Fuhrer R, Shipley M J.et al Psychological distress as a risk factor for coronary heart disease in the Whitehall II study. Int J Epidemiol 200231248–255. [DOI] [PubMed] [Google Scholar]
- 6.Klose M, Jacobi F. Can gender differences in the prevalence of mental disorders be explained by sociodemographic factors? Arch Women Ment Health 20047133–148. [DOI] [PubMed] [Google Scholar]
- 7.Lindeman S, Hamalainen J, Isometsa E.et al The 12‐month prevalence and risk factors for major depressive episode in Finland: representative sample of 5993 adults. Acta Psychiatr Scand 2000102178–184. [DOI] [PubMed] [Google Scholar]
- 8.Kessler R C, Berglund P, Demler O.et al The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS‐R). JAMA 20032893095–3105. [DOI] [PubMed] [Google Scholar]
- 9.Wang J, El‐Guebaly N. Sociodemographic factors associated with comorbid major depressive episodes and alcohol dependence in the general population. Can J Psychiatry 20044937–44. [DOI] [PubMed] [Google Scholar]
- 10.Harrison J, Barrow S, Gask L.et al Social determinants of GHQ score by postal survey. J Public Health Med 199921283–288. [DOI] [PubMed] [Google Scholar]
- 11.Helsing K J, Szklo M, Comstock G W. Factors associated with mortality after widowhood. Am J Public Health 198171802–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lund R, Due P, Modvig J.et al Cohabitation and marital status as predictors of mortality—an eight year follow‐up study. Soc Sci Med 200255673–679. [DOI] [PubMed] [Google Scholar]
- 13.Davis M A, Neuhaus J M, Moritz D J.et al Living arrangements and survival among middle‐aged and older adults in the NHANES I epidemiologic follow‐up study. Am J Public Health 199282401–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joung I M, Stronks K, van de Mheen H.et al Health behaviours explain part of the differences in self reported health associated with partner/marital status in the Netherlands. J Epidemiol Community Health 199549482–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miettinen A. Population data in Finland 1900–2004. Yearbook of Population Research in Finland 200541191–198. [Google Scholar]
- 16.Ren X S. Marital status and quality of relationships: the impact on health perception. Soc Sci Med 199744241–249. [DOI] [PubMed] [Google Scholar]
- 17.Brown S L, Bulanda J R, Lee G R. The significance of nonmarital cohabitation: marital status and mental health benefits among middle‐aged and older adults. J Gerontol B Psychol Sci Soc Sci 200560S21–S29. [DOI] [PubMed] [Google Scholar]
- 18.Willitts M, Benzeval M, Stansfeld S. Partnership history and mental health over time. J Epidemiol Community Health 20045853–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bijl R V, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of the Netherlands mental health survey and incidence study (NEMESIS). Soc Psychiatry Psychiatr Epidemiol 199833587–595. [DOI] [PubMed] [Google Scholar]
- 20.Cairney J, Boyle M, Offord D R.et al Stress, social support and depression in single and married mothers. Soc Psychiatry Psychiatr Epidemiol 200338442–449. [DOI] [PubMed] [Google Scholar]
- 21.Hughes M E, Waite L J. Health in household context: living arrangements and health in late middle age. J Health Soc Behav 2002431–21. [PMC free article] [PubMed] [Google Scholar]
- 22.Aro A R, Nyberg N, Absetz P.et al Depressive symptoms in middle‐aged women are more strongly associated with physical health and social support than with socioeconomic factors. Nord J Psychiatry 200155191–198. [DOI] [PubMed] [Google Scholar]
- 23.Huurre T, Aro H, Rahkonen O. Well‐being and health behaviour by parental socioeconomic status: a follow‐up study of adolescents aged 16 until age 32 years. Soc Psychiatry Psychiatr Epidemiol 200338249–255. [DOI] [PubMed] [Google Scholar]
- 24.De Graaf R, Bijl R V, Ravelli A.et al Predictors of first incidence of DSM‐III‐R psychiatric disorders in the general population: findings from the Netherlands Mental Health Survey and Incidence Study. Acta Psychiatr Scand 2002106303–313. [DOI] [PubMed] [Google Scholar]
- 25.Fryers T, Melzer D, Jenkins R. Social inequalities and the common mental disorders: a systematic review of the evidence. Soc Psychiatry Psychiatr Epidemiol 200338229–237. [DOI] [PubMed] [Google Scholar]
- 26.Lahelma E. Unemployment and mental well‐being: elaboration of the relationship. Int J Health Serv 199222261–274. [DOI] [PubMed] [Google Scholar]
- 27.Pevalin D J, Goldberg D P. Social precursors to onset and recovery from episodes of common mental illness. Psychol Med 200333299–306. [DOI] [PubMed] [Google Scholar]
- 28.Hodiamont P P, Rijnders C A, Mulder J.et al Psychiatric disorders in a Dutch health area: a repeated cross‐sectional survey. J Affect Disord 20058477–83. [DOI] [PubMed] [Google Scholar]
- 29.Wu Z, Penning M, Pollard M.et al “In sickness and in health” does cohabitation count? J Fam Issues 200324811–838. [Google Scholar]
- 30.Martelin T, Koskinen S, Aromaa A. Variation of health and functional capacity according to region, education and marital status. In: Aromaa A, Koskinen S, eds. Health and functional capacity in Finland. Baseline results of the health 2000 health examination survey. Helsinki: Hakapaino Oy, 2004100–107.
- 31.Wittchen H U, Lachner G, Wunderlich U.et al Test‐retest reliability of the computerized DSM‐IV version of the Munich‐composite international diagnostic interview (M‐CIDI). Soc Psychiatry Psychiatr Epidemiol 199833568–578. [DOI] [PubMed] [Google Scholar]
- 32.Pirkola S P, Isometsa E, Suvisaari J.et al DSM‐IV mood‐, anxiety‐ and alcohol use disorders and their comorbidity in the Finnish general population. Results from the health 2000 study. Soc Psychiatry Psychiatr Epidemiol 2005401–10. [DOI] [PubMed] [Google Scholar]
- 33.Goldberg D P, Gater R, Sartorius N.et al The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 199727191–197. [DOI] [PubMed] [Google Scholar]
- 34.Pevalin D J. Multiple applications of the GHQ‐12 in a general population sample: an investigation of long‐term retest effects. Soc Psychiatry Psychiatr Epidemiol 200035508–512. [DOI] [PubMed] [Google Scholar]
- 35.Suurmeijer T P, Doeglas D M, Briancon S.et al The measurement of social support in the ‘European research on incapacitating diseases and social support': the development of the social support questionnaire for transactions (SSQT). Soc Sci Med 1995401221–1229. [DOI] [PubMed] [Google Scholar]
- 36.Seppä K. Alkoholiongelman varhaistoteaminen. In: Salaspuro M, Kiianmaa K, Seppä K, eds. Päihdelääketiede. Jyväskylä: Kustannus Oy Duodecim, 1998
- 37.Brown S L. The effect of union type on psychological well‐being: depression among cohabitors versus marrieds. J Health Soc Behav 200041241–255. [PubMed] [Google Scholar]
- 38.Kendler K S, Myers J, Prescott C A. Sex differences in the relationship between social support and risk for major depression: a longitudinal study of opposite‐sex twin pairs. Am J Psychiatry 2005162250–256. [DOI] [PubMed] [Google Scholar]
- 39.Laiho J, Nieminen T. eds Terveys 2000 ‐tutkimus. Aikuisväestön haastatteluaineiston tilastollinen laatu. Otanta‐asetelma, tiedonkeruu, vastuskato ja estimointi‐ ja analyysiasetelma. Helsinki: Yliopistopaino, 2004
- 40.Agerbo E, Byrne M, Eaton W W.et al Marital and labor market status in the long run in schizophrenia. Arch Gen Psychiatry 20046128–33. [DOI] [PubMed] [Google Scholar]
- 41.Jane‐Llopis E, Hosman C, Jenkins R.et al Predictors of efficacy in depression prevention programmes. Meta‐analysis. Br J Psychiatry 2003183384–397. [DOI] [PubMed] [Google Scholar]