Abstract
Objectives
To evaluate changes in the prevalence of HIV infection among young heroin users in three Spanish cities, and their association with harm reduction programmes (HRPs).
Methods
Two cross sectional studies. The 1995 study included 596 users; half were street recruited and half were recruited at drug treatment centres. The 2001–03 study included 981 street recruited users. Face to face interviews were conducted using a structured questionnaire. Samples for HIV testing (saliva in 1995 and dried blood spot in 2001–03) were collected.
Results
The proportion who had ever injected (IDUs) decreased in all three cities. HIV prevalence in IDUs decreased by half in Barcelona (44.1% to 20.8%) and Seville (44.2% to 22.2%), but remained constant in Madrid (36.8% and 34.9%). This difference was attributable to a decrease in HIV prevalence in long term IDUs in Barcelona and Seville, but not in Madrid. The crude odds ratio for HIV prevalence in Madrid compared with Barcelona in long term IDUs was 2.3 (95%CI 1.4 to 3.7), increasing to 3.1 (95%CI 1.5 to 6.2) after adjusting for sociodemographic and risk factors. HIV prevalence in short term IDUs was similar in all cities. In 1992 Barcelona already had 20 heroin users in methadone maintenance programmes (MMPs) per 10 000 population aged 15–49 years; Seville reached this rate in 1994, and Madrid, not until 1998.
Conclusions
The prevalence of HIV infection did not decrease in long term injectors in Madrid. The delayed implementation of HRPs, especially MMPs, may be the most plausible hypothesis. This finding should shed light on decision making in countries in a similar epidemiological and sociological situation.
Keywords: HIV, substance related disorders, health policy, sharing needles
In 1995 a cross sectional study of prevalence of heroin injection and HIV infection was carried out in Barcelona, Madrid, and Seville.1 These cities were chosen because of their different geographical locations, prevalence of injection,2 and preventive policies.
The efficacy of harm reduction programmes (HRPs) in HIV prevention has been well described.3,4,5 HRPs were implemented in Spain during the 1990s, later than in other European countries. From only 4000 users in methadone maintenance programmes (MMPs) in 1991, the number increased to 65 000 in 1998.6 However, there was wide variability among regions as to HRP start up, intensity, coverage, and organisational characteristics.7 This delay was attributable to the opposition of some sectors, arguing what is being said in some Eastern and Central European countries to avoid implementing these programmes: that HRPs may promote injection and send “the wrong message” by not making drug cessation the only objective.8,9
In 2001, a cohort study (Itínere Project) was started in the same cities. The objective of this study is to compare the results of this cohort with those of 1995 to describe the evolution of injection, HIV infection and the main risk behaviours, and to explore their possible association with the development of HRPs during the 1990s.
Methods
Design and study population
Two cross sectional studies. The first was carried out between March and December 1995, and the second between May 2001 and December 2003. A detailed methodological description has been published elsewhere.10,11,12
Eligibility
Age 30 or younger, residence in the metropolitan area for most of the past 12 months, and current, regular heroin user (in 1995, lifetime use at least 12 times and at least once in the past month; in 2001–03, at least 12 times in the past 12 months and at least once in the past three months). Neither of the two samples included experimental users.
Recruitment procedures
The 1995 study
About half of the participants were recruited at admission in all the public drug treatment centres (hereinafter called “treatment users”). The other half were street recruited (“street users”) by chain referral procedures, combining targeted sampling13 with respondent driven sampling (RDS).14 Most participants (65%) were directly recruited by interviewers at drug scenes. Neither participants nor key informants received payment for recruitment or being interviewed, but they were invited for a drink or coffee.
The 2001–03 study
The whole sample was street recruited by targeted sampling and RDS. Workers visited all drug scenes to recruit the initial participants (17.1%); 1.7% answered advertisements, 34.1% were enrolled by key informants, and 47% were enrolled by participants themselves using RDS. A monetary incentive (€18) was offered for being interviewed or for recruiting others.
Data collection: interviews
A structured questionnaire was administered, including sociodemographics, social conflict, patterns of substance use, injection risk behaviour, sexual risk behaviour, and knowledge of HIV status, including dates of testing.
The 1995 study
Face to face interviews were held with treatment users in treatment centres by workers who did not belong to the staff of these centres. HIV test results were obtained from clinical records. Saliva samples were not requested. Street users were interviewed by the same workers, and a saliva sample using Orasure‐Epitope was requested.
The 2001–03 study
The face to face interviews were computer assisted. Participants were interviewed in health and social services centres that were not involved in drug dependence treatment. A dried blood spot was obtained. All participants signed an informed consent form.
Procedures for HIV testing
The 1995 study
Saliva samples were analysed by ELISA (HIV 1+2 Ortho). These results were available for only 78.5%, with no significant differences by city. Given that the positive predictive value of self report for persons with both self reported and laboratory results was 94%, we accepted self reported serostatus for the 16% with no laboratory results.1
The 2001–03 study
The dried blood samples were analysed by ELISA Genscreen HIV1/2 version 2 and New Lav Blot 1, Bio‐Rad, Marnes La Coquette, France. As the self reports had a positive predictive value of 99%, only positive samples from subjects who stated they were HIV negative or had not previously been tested were confirmed by western blot.
Data on harm reduction programmes
Data on MMP patients and the number of NEPs were provided by the persons responsible for the regional drug information systems. Qualitative data were also obtained from a report on NEPs in southern Europe.15
Statistical analysis
A univariate analysis, stratified by city and cross sectional study, was performed. The analysis was then restricted to the 1051 users who had ever injected (IDUs). The significant differences between the two cross sectional studies were analysed using the χ2 test, Student's t test, and Fisher's exact test.
Subsequent analyses focused on how the prevalence of HIV in IDUs had evolved in each city, stratifying by years since first injection (⩽5 years, >5 years). Crude odds ratios with their 95% confidence intervals were calculated for each city in the four strata resulting from crossing the two studies (1995 and 2001) and the two categories of the variable “years since first injection”. To determine if differences in the prevalence of infection by city in each of the four strata were attributable to differences in sample characteristics (arising from possible selection biases), the ORs were adjusted for sociodemographics and risk behaviours in four logistic regression models (one per stratum), in a model in a single step that included all the adjustment variables. The analysis was performed with SPSS (SPSS for Windows, version 12.0, 2003, Chicago) and Stata (Stata Statistical Software, release 8.0, 2003, College Station, TX).
Results
Sociodemographic characteristics
A total of 596 participants were recruited in 1995 and 981 in 2001–03 (table 1). There were about three men for each woman. Subjects in the 2001–03 study were significantly younger (41.9% aged 25 or younger v 30%); had a higher educational level, were more often foreigners (11% v 2%), more frequently had regular employment (31.5% v 23%), and more often derived their main source of income from work (34% v 20%). The two studies had about the same proportions of persons who were homeless most of the time or lived in institutions (<15%), or who had ever been in prison (40%).
Table 1 Sociodemographic characteristics, patterns of drug use, and sexual behaviours in two cross sectional studies carried out in Barcelona, Madrid, and Seville in 1995 and 2001–03 (%).
| Barcelona | Madrid | Seville | |||||
|---|---|---|---|---|---|---|---|
| 1995 | 2002 | 1995 | 2002 | 1995 | 2002 | ||
| 207 | 354 | 199 | 427 | 190 | 200 | ||
| Number | % | % | % | % | % | % | p Value† |
| Sociodemographic characteristics | |||||||
| Mean age | 26.1 | 24.9 | 26.4 | 26.3 | 26.7 | 25.6 | |
| Age ⩽25 | 35.3 | 53.1 | 27.6 | 32.8 | 26.8 | 41.5 | *** |
| Men | 74.4 | 69.2 | 75.9 | 71.7 | 83.2 | 82.5 | NS |
| Foreigners | 3.9 | 18.1 | 1.5 | 7.0 | 0.5 | 3.5 | *** |
| Level of education higher than primary | 21.7 | 65.5 | 28.1 | 59.0 | 14.2 | 23.5 | ** |
| Regular employment | 21.7 | 30.8 | 26.4 | 32.3 | 20.5 | 31.5 | *** |
| Job as main source of income in past 12 months | 18.8 | 33.8 | 24.6 | 37.9 | 17.4 | 28.5 | *** |
| Living mainly in a house or apartment in past 12 months | 91.8 | 81.9 | 87.9 | 86.8 | 83.7 | 91.5 | NS |
| Prison | NS | ||||||
| Never | 56.8 | 60 | 63.8 | 60.2 | 48.1 | 55.4 | |
| <1 year | 18.9 | 19.7 | 16.1 | 19.4 | 20.6 | 19.5 | |
| ⩾1 year | 24.3 | 20.3 | 20.1 | 20.4 | 31.2 | 25.1 | |
| Sexual behaviour (past 12 months) | |||||||
| Two or more sexual partners | 70.4 | 49.2 | 62.2 | 41.7 | 50.3 | 40.1 | *** |
| Sexual relation without condoms | 66.7 | 62.1 | 66.0 | 49.4 | 66.5 | 52.0 | *** |
| Sexual relations for money | 15.5 | 7.9 | 10.7 | 11.0 | 14.5 | 10.0 | * |
| Patterns of drug use and injecting | |||||||
| <18 years at first heroin use | 51.2 | 53.4 | 48.2 | 63.5 | 47.9 | 66.5 | *** |
| Injecting as first main route of heroin administration | 43.5 | 25.1 | 36.7 | 12.4 | 18.9 | 5.0 | *** |
| ⩽5 years since first heroin use | 30.0 | 37.9 | 32.2 | 22.7 | 21.6 | 25.5 | NS |
| Ever injected | 87.9 | 80.2 | 70.4 | 65.1 | 53.2 | 33.0 | ** |
| Injected in the past 12 months | 84.1 | 75.7 | 48.2 | 48.9 | 31.1 | 15.5 | NS |
| Injected in the past 30 days | 82.1 | 67.5 | 31.7 | 39.8 | 26.8 | 10.5 | NS |
| Injecting as current main route of heroin administration (past 30 days) | 80.7 | 64.1 | 20.3 | 19.7 | 20.5 | 0.0 | *** |
†Comparison between 1995 and 2001–03 in the global sample. NS, not significant. *p<0.05; **p<0.01; ***p<0.001.
Sexual behaviour
In all three cities there was a significant decrease in the proportion of persons who had had vaginal or anal relations with more than two persons of the opposite sex during the 12 months (from 61.3% to 44.1% overall) or who had had sexual relations in exchange for money (from 13.5% to 9.7%). In the latter case, the change was because of a major decrease among women, especially in Barcelona, as there was no significant change among men. There was also a significant reduction in the percentage of persons who had had sexual relations without condoms in the past 12 months (from 66.4% to 54.5%), which was mainly attributable to the decrease among men (from 66.5% to 48.5%) (table 1).
Patterns of drug use and prevalence of injecting
The percentage of those who began to use heroin before age 18 years and of users aged 25 years or younger was higher in 2001–03. However, whereas in Barcelona and Seville there was a significant decrease in all indicators of injecting prevalence, in Madrid the prevalence of injection in the past 30 days increased (from 31.7% to 39.8%) (table 1). In Seville, in 2001–03 no one stated that injecting was their current main route of administration.
Patterns of injecting and prevalence of injecting risk behaviour (table 2)
Table 2 Injecting behaviours of young heroin users who had ever injected in two cross sectional studies carried out in Barcelona, Madrid, and Seville in 1995 and 2001–03 (%).
| Barcelona | Madrid | Seville | |||||
|---|---|---|---|---|---|---|---|
| 1995 | 2001–03 | 1995 | 2001–03 | 1995 | 2001–03 | ||
| 182 | 284 | 140 | 278 | 101 | 66 | ||
| Number | % | % | % | % | % | % | p Value† |
| <18 at first injection | 33.5 | 32.2 | 40.0 | 36.0 | 35.6 | 40.6 | NS |
| Self injected at first injection | 26.0 | 21.8 | 18.6 | 19.8 | 21.8 | 24.2 | NS |
| ⩽5 years since first injection | 36.8 | 51.9 | 35.7 | 40.8 | 24.8 | 35.9 | *** |
| First drug injected | *** | ||||||
| Heroin | 95.0 | 84.2 | 73.0 | 46.3 | 86.0 | 56.9 | |
| cocaine, or cocaine+heroin mix | 5.0 | 12.6 | 27.0 | 53.7 | 14.0 | 43.1 | |
| Drugs most frequently injected‡ | *** | ||||||
| heroin | 93.5 | 39.7 | 71.0 | 10.0 | 96.0 | 16.7 | |
| cocaine, or cocaine+heroin mix | 6.5 | 60.4 | 29.0 | 90.4 | 4.0 | 83.9 | |
| Ever injected with a syringe used by someone else | 72.0 | 41.6 | 60.7 | 39.6 | 62.7 | 38.2 | *** |
| Injected with a syringe used by someone else in past 12 months | 33.0 | 23.2 | 20.0 | 15.1 | 18.8 | 6.6 | ** |
| Injected with a syringe used by someone else in past 30 days | 7.1 | 10.9 | 7.9 | 7.0 | 12.9 | 3.3 | |
†Comparison between 1995 and 2001–03 in the global sample. NS, not significant. *p<0.05, **p<0.01, * **p<0.001. ‡Past 30 days in 1995, and past 12 months in 2001.
In ever injectors (423 in 1995 and 628 in 2001–03), there was no significant change in the proportion of those who injected for the first time before age 18 (36.2% and 34.7%), or in those who were injected for the first time by someone else (77.5% and 78.8%), but the proportion of those who had injected for five years or less changed significantly (33.6% and 45.3%). There was also a major change in the substances injected. Whereas in 1995 cocaine—alone or mixed with heroin—was the first drug injected for just 14.4%, and was the drug most frequently injected in the past 12 months for just 11%, the corresponding figures for 2001–03 were 35.4% and 73.7%, respectively. This change was notable in Seville, and even more so in Madrid. There was a significant decrease in the prevalence of those who had ever injected with borrowed needles or syringes (from 66.4% to 40.4%) or who had done so in the past 12 months (from 25.3% to 17.9%), whereas the proportion of those who had done so in the past 30 days remained stable.
What is already known about the topic
The efficacy of harm reduction programmes (methadone maintenance and needle exchange) to prevent HIV infection has been recognised since the end of the 1980s.
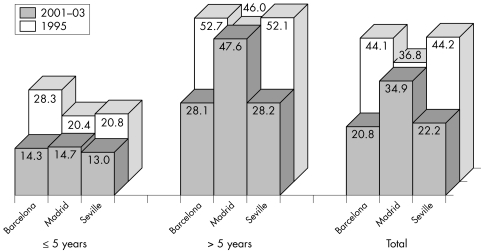
Prevalence of HIV in injection drug users (fig 1)
Figure 1 Prevalence of HIV infection among young injecting heroin users in two cross sectional studies carried out in Barcelona, Madrid, and Seville in 1995 and 2001–2003, by time since first injection.
The percentage of HIV infected IDUs decreased by about half in Barcelona (from 44.1% to 20.8%; p<0.001) and Seville (from 44.2% to 22.2%; p<0.01), whereas it remained practically the same in Madrid (36.8% and 34.9%). After stratifying by years since first injection, this differential trend was seen to be attributable to a change in those who had injected for more than five years (long term injectors). The prevalence in this group decreased in Barcelona (52.7% in 1995 and 28.1% in 2001–03; p<0.001) and Seville (52.1% and 28.2%; p<0.01), but not in Madrid (46.0% and 47.6%) (fig 1). In contrast, the prevalence of infection among those who had injected for five or fewer years decreased in all three cities, although the difference did not reach statistical significance in Seville because of the small sample size. In Madrid, 55% of long term injectors had been diagnosed as HIV positive before 1998, and in another 12% of cases it is reasonable to assume that they were infected before that year (considering various parameters: date of first injection and date and result of their tests). An analysis of the crude odds ratios of prevalence by city and of the logistic regression models shows that adjusting for sociodemographic variables and risk behaviours does not change the findings of the stratified analysis; significant differences among cities were found only in long term injectors in Madrid in 2001–03, whereas the odds ratio in comparison with Barcelona increased after adjustment, from 2.3 (CI:1.4 to 3.7) to 3.1 (CI:1.5 to 6.2) (table 3).
Table 3 Crude and adjusted odds ratios and confidence limits of association between HIV prevalence, and city by year of cross sectional study and years since first injection. Young heroin users who had ever injected in two cross sectional studies carried out in Barcelona, Madrid and Seville in 1995 and 2001–03.
| Years since first injection | City | 1995 | 2001–03 | ||
|---|---|---|---|---|---|
| Crude OR | Adjusted OR | Crude OR | Adjusted OR | ||
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | ||
| ⩽5 | Barcelona | 1 | 1 | 1 | 1 |
| Madrid | 0.6 (0.2 to 2.0) | 0.9 (0.1 to 6.5) | 1.0 (0.5 to 2.0) | 1.3 (0.5 to 3.5) | |
| Seville | 0.7 (0.3 to 1.6) | 0.2 (0.0 to 1.2) | 0.9 (0.2 to 3.2) | 0.7 (0.1 to 4.3) | |
| >5 | Barcelona | 1 | 1 | 1 | 1 |
| Madrid | 0.8 (0.4 to 1.3) | 1.2 (0.5 to 2.8) | 2.3 (1.4 to 3.7) | 3.1 (1.5 to 6.2) | |
| Seville | 1 (0.5 to 1.8) | 1.3 (0.6 to 2.3) | 1.0 (0.5 to 2.3) | 1.5 (0.5 to 4.8) | |
Adjusted for the following variables (included and retained in the model): sex, employment status, educational level, prison, first drug injected, drug most frequently injected, sexual relation without condoms, sexual relations for money, injected in past 30 days, ever borrowed, and borrowed in past 30 days.
What this paper adds
The main finding of this study is the differential trend in HIV prevalence in long term injectors in Madrid compared with those in Barcelona or Seville.
The delayed implementation of harm reduction programmes probably meant a lost opportunity to prevent HIV dissemination in Madrid.
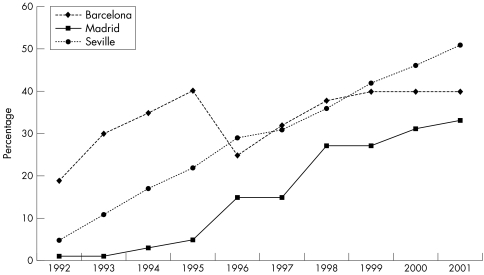
Development of harm reduction programmes
NEPs in all three cities began in 1991. In 1996 the rate of syringes per 10 000 population aged 15–49 years was 181 in Madrid region and 297 in Barcelona. In 1998 both areas had similar rates (around 500). However, whereas there were only 55 syringe exchange points in Madrid region, there were more than 150 in Barcelona. This was largely because of the participation of pharmacies, which represented 90% or more of syringe exchange points. In Seville, these programmes were much less well developed as the number of persons who injected as the main route had decreased, although no good data are available on the number of syringes distributed. With respect to MMPs, whereas in Barcelona 20 persons per 10 000 population aged 15–49 were already being treated with methadone in 1992, and in Seville this rate was exceeded in 1995, this rate was not reached in Madrid until 1998 (fig 2).
Figure 2 Rate of persons in methadone treatment per 10 000 population aged 15–49 years in Madrid, Barcelona, and Seville, 1992–2001.
Discussion
The main finding of this study is the differential trend in the prevalence of HIV in IDUs in Madrid in comparison with those in Barcelona or Seville. In 1995, all three cities had an extremely high HIV prevalence. Six or seven years later the prevalence had decreased by half in Seville and Barcelona, whereas it remained practically the same in Madrid, because HIV prevalence in Madrid did not decrease among those injecting for longer than five years.
What could explain this differential trend? Firstly, it could simply be attributable to selection biases in recruitment. However, this hypothesis, although impossible to rule out, is unlikely. In 1995, there were no significant differences in HIV prevalence between treatment IDUs and street IDUs. In 2001–03, the main recruitment method was RDS, followed by recruitment by users over 30 or former users. Over 80% of the participants in the three cities were recruited using these two methods. RDS strongly reduces the most important biases that could be introduced by targeted sampling.14 Other indicators of uniform recruitment methods among cities in 2001–03 were the similar proportions of people who had been in treatment in the past 12 months (60% in Barcelona and Madrid and 66% in Seville), and of those who had obtained at least half of their syringes through NEPS (over 85%). Finally, the crude odds ratio for HIV prevalence among long term injectors in Madrid in comparison with Barcelona in 2001–03 was 2.3 (95% CI 1.4 to 3.7), and rose to 3.1(95% CI 1.5 to 6.2) after adjusting for sociodemographic characteristics or risk behaviours, which suggests that the difference is not explained by a differential recruitment bias for these characteristics.
Policy implications
To curtail an HIV epidemic, harm reduction programmes must be developed on time and on a scale proportional to the damage observed. The Spanish experience may facilitate decision making in other countries with similar social and epidemiological conditions.
A second explanation could be differences in the strategy of laboratory analysis. These differences are unlikely to introduce major bias, given that we are dealing with injectors with a high prevalence of infection, and because the biases that might be produced by the different types of samples (lower sensitivity in saliva) and by not carrying out a confirmation test (not ruling out some false positives) would tend to cancel each other out.
Thirdly, the differential trend could be attributable to different rates of mortality or migration. However, there is no evidence of lower mortality in Madrid; if anything, the reverse may be true: 48.9% of those infected in Barcelona had been in antiretroviral treatment, compared with 38% in Madrid and 35% in Seville. No information is available to evaluate migration, but a restricted analysis of those who had lived over five years in each city did not change the trends in HIV prevalence.
Fourthly, the differential trend might be attributable to the different availability among cities of treatments with a high capacity for retention (as is the case of methadone). However, considering the time when these programmes were implemented in each city, it is logical to think that the differential trend found in Madrid should actually be much larger.
Fifthly, the trend could be attributable to a phenomenon that constitutes another important finding of this study: that cocaine or heroin‐cocaine mixtures are replacing heroin as the most frequently injected substance in the three cities. This change has also been described,16 and is of concern, because the risk of HIV infection is much higher among cocaine injectors.17 Although this does not seem to be the main reason why HIV prevalence has not decreased in Madrid (the variable was included in the adjusted model), it suggests we may need to rethink the role of HRPs. Another hypothesis is whether this differential trend could be related with the implementation of HRPs. The data on harm reduction programmes show that 20 persons per 10 000 population aged 15–45 years were in MMPs in Barcelona in 1992 and in Seville in 1995, whereas in Madrid this rate was not reached until 1998, despite ample knowledge of the preventive capacity of MMPs.3,4 In the mid‐90s, this difference between Madrid and Barcelona had already been noted,7 a difference that was even more important given the estimated number of users in each city—higher in Madrid than in Barcelona.18,19 In fact, among HIV positive IDUs in Madrid who had injected for over five years, more than two of three became infected before 1998, before MMPs could have benefited a large number of users.
Few data are available to evaluate the association between the trend in HIV infection and syringe exchange programmes. The programmes in all three cities began in 1991. However, in Seville the percentage of frequent injectors was already very low, so that the demand for syringes was, logically, lower. Thus, it is difficult to compare the data from Seville with Madrid and even more so with Barcelona.2
Although an aetiological association cannot be established between the late development of HRPs, especially MMPs, in Madrid and the continued high prevalence of HIV in long term IDUs, we know of no more plausible hypothesis that can better explain the differential evolution in these cities. It would be useful to have data on the use of preventive services during the years in which the differential HIV incidence among cities seems to have occurred. Such information could have helped strengthen the hypothesis about the effect of methadone availability. Unfortunately, however, our data on the use of services refer to lifetime use or to the past 12 months. However, HRPs obviously not only have a direct affect on those who use them, but also have an indirect effect on the community at large.20 What is more, Seville and Barcelona started with a disadvantage, as they had higher prevalences in the mid‐90s. Furthermore, the trend in young injectors, who were able to benefit more consistently in each city, has been similar in all three cities, and preliminary data on HIV incidence in Barcelona and Madrid in the 2001–03 study show a similar incidence among IDUs in both cities.21
Furthermore, indicators of injecting in 2001–03 confirmed the trend described in 1995.11 This downward trend began in the early 1980s. At least in the early stages there must have been other decisive factors in addition to the catalysing effect that HIV prevention policies may have had in producing the changes that occurred in all areas.11,22
In all three cities the percentage of those who had ever injected with used syringes also decreased. Some authors have suggested that the concomitant existence of different prevalences of HIV infection and similar prevalences of risk behaviours among geographical areas could partly be explained by the type of heroin in each area.23 As brown heroin must be heated before it can be dissolved, it is thought this could inactivate the virus and decrease transmission.24 In our study, however, this does not seem to be a plausible explanation. By the mid‐1990s, brown heroin was already practically the only type that existed in Madrid and Seville, whereas white heroin continues to exist in Barcelona.
Although it is difficult to confirm definitively, all the evidence suggests that Madrid lost an opportunity to prevent the dissemination of HIV among injectors during the first half of the 1990s by not rapidly implementing MMPs while other cities were doing so. A similar situation may currently be taking place in other areas which already have high prevalences of infection,25 but which in some cases even prohibit MMPs. The description of what has happened in Spain may facilitate decision making in a context of public debate on the effectiveness of certain measures.
Ackowledgements
We acknowledge the contribution of all the participants and of those persons and institutions who were involved in recruitment and follow up, who allowed us the use of their centres for the interviews, and who helped with project management: (a) In Madrid: Fundación de Ayuda contra la Drogadicción (FAD), Programas Municipales de Sida e Instituto de las Adicciones, Médicos del Mundo, CAID de Torrejón de Ardoz, Centro Sanitario Sandoval, Subdirección General de Sanidad de Instituciones Penitenciarias, Agencia Antidroga. (b) In Barcelona: ABD, Spott, Ambit, CECAS, Secretaria de Serveis Penitenciaris, Rehabilitació i Justícia Juvenil; (c) In Seville: Ayuntamiento de Sevilla, Centros de Tratamiento Ambulatorios de Drogodependencias de la Diputación Provincial de Sevilla, Centro Tratamiento Alcoholismo Anclaje, Antaris, Centro de Día AVAT, Asociación Aspad. We also thank Kathryn M Fitch for translation and suggestions.
Abbreviations
HRP - harm reduction programme
MMP - methadone maintenance programme
RDS - respondent driven sampling
IDU - injecting drug user
Footnotes
Funding: supported mainly by Fundación para Investigación y la Prevención del Sida en España (Fipse 3035/99); analysis also funded by RTIC: FIS C03‐091 Red de Trastornos Adictivos (RTA) and FIS G03‐005 Red de Centros de Investigación en Epidemiología y Salud Pública (RECEPS).
Conflicts of interest: none.
Project Itinere Group: Mireia Ambros, Silvina Basani, Francisco Bru, Antonia Domingo, David Fernández, Francisco González, Victoria Jiménez, Eusebio Mejías, Montserrat Neira, José Pulido, Luis Royuela, Sofía Ruiz, and Teresa Silva.
References
- 1.de la Fuente L, Bravo M J, Lew C.et al [The prevalence of human immunodeficiency virus infection and the risk behaviors in the heroin addicts of Barcelona, Madrid and Seville: an example of the advantages of centering studies on addicts and not just on intravenous users]. Med Clin (Barc) 1999113646–651. [PubMed] [Google Scholar]
- 2.de la Fuente L, Barrio G, Vicente J.et al Intravenous administration among heroin users having treatment in Spain. Int J Epidemiol 199423805–811. [DOI] [PubMed] [Google Scholar]
- 3.Drucker E, Lurie P, Wodak A.et al Measuring harm reduction: the effects of needle and syringe exchange programs and methadone maintenance on the ecology of HIV. AIDS 199812S217–S230. [PubMed] [Google Scholar]
- 4.Gibson D R, Flynn N M, McCarthy J J. Effectiveness of methadone treatment in reducing HIV risk behavior and HIV seroconversion among injecting drug users. AIDS 1999131807–1818. [DOI] [PubMed] [Google Scholar]
- 5.Gibson D R, Flynn N M, Perales D. Effectiveness of syringe exchange programs in reducing HIV risk behavior and HIV seroconversion among injecting drug users. AIDS 2001151329–1341. [DOI] [PubMed] [Google Scholar]
- 6.de la Fuente L, Bravo M J, Barrio G.et al Lessons from the history of the human immunodeficiency virus/acquired immunodeficiency syndrome epidemic among Spanish drug injectors. Clin Infect Dis 200337S410–S415. [DOI] [PubMed] [Google Scholar]
- 7.Domingo‐Salvany A, Perez K, Torrens M.et al Methadone treatment in Spain, 1994. Drug Alcohol Depend 19995661–66. [DOI] [PubMed] [Google Scholar]
- 8.Des Jarlais D C, Hammett T M, Wei L.et al Opiate agonist maintenance treatment for injecting drug user peer educators. Addiction 2004991355–1356. [DOI] [PubMed] [Google Scholar]
- 9.Moshkova A. Substitution therapy: overcoming ignorance. Harm Reduction News 200341–1. [Google Scholar]
- 10.Barrio G, de la Fuente L, Royuela L.et al Cocaine use among heroin users in Spain: the diffusion of crack and cocaine smoking. Spanish Group for the Study on the Route of Administration of Drugs. J Epidemiol Community Health 199852172–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de la Fuente L, Barrio G, Royuela L.et al The transition from injecting to smoking heroin in three Spanish cities. The Spanish Group for the Study of the Route of Heroin Administration. Addiction 1997921749–1763. [PubMed] [Google Scholar]
- 12.de la Fuente L, Brugal M T, Ballesta R.et al Metodología del estudio de cohortes del proyecto Itinere sobre consumidores de heroína en tres ciudades españolas y características básicas de los participantes [Cohort study methodology of the ITINERE project on heroin users in three Spanish cities and main characteristics of the participants]. Rev Esp Salud Pública 200579475–491. [PubMed] [Google Scholar]
- 13.Watters J K, Biernacki P. Targeted sampling: options for the study of hidden populations. Social Problems 198936416–430. [Google Scholar]
- 14.Heckathorn D D. Respondent ‐driven sampling: a new approach to the study of hidden populations. Social Problems 199744174–179. [Google Scholar]
- 15.Centre de Estudis Epidemiològics sobre la Sida de Catalunya CESCAT. Les Programmes d'ëchange de Seringes pour la Prévention du HIV dans les pays du Sud de l'Europe.PESESUD 1997. In: Barcelona 1998. Barcelona, CESCAT 2004
- 16.Welp E A, Lodder A C, Langendam M W.et al HIV prevalence and risk behaviour in young drug users in Amsterdam. AIDS 2002161279–1284. [DOI] [PubMed] [Google Scholar]
- 17.Tyndall M W, Currie S, Spittal P.et al Intensive injection cocaine use as the primary risk factor in the Vancouver HIV‐1 epidemic. AIDS 200317887–893. [DOI] [PubMed] [Google Scholar]
- 18.Paredes D, Del Llano J, Ruiz M.Estimación de la prevalencia de la adicción a la heroína en la Comunidad de Madrid durante 1992. Madrid: Comunidad de Madrid, 1992
- 19.Domingo‐Salvany A, Hartnoll R L, Maguire A.et al Analytical considerations in the use of capture‐recapture to estimate prevalence: case studies of the estimation of opiate use in the metropolitan area of Barcelona, Spain. Am J Epidemiol 1998148732–740. [DOI] [PubMed] [Google Scholar]
- 20.Hurley S F, Jolley D J, Kaldor J M. Effectiveness of needle‐exchange programmes for prevention of HIV infection. Lancet 19973491797–1800. [DOI] [PubMed] [Google Scholar]
- 21.Toro C, Brugal M T, Vallejo F.et al Incidencia de infección por VIH en los jóvenes consumidores de heroína (inyectores y no inyectores) de Madrid y Barcelona (PROYECTO ITÍNERE) [Incidence of HIV infection among young heroin users (injecting and non‐injecting) from Madrid, Barcelona and Seville (ITINERE PROJECT). Sociedad Española Interdisciplinaria del Sida. VIII Congreso Nacional sobre el Sida, Madrid 2004
- 22.de la Fuente L, Saavedra P, Barrio G.et al Temporal and geographic variations in the characteristics of heroin seized in Spain and their relation with the route of administration. Drug Alcohol Depend 199640185–194. [DOI] [PubMed] [Google Scholar]
- 23.Garfein R S, Monterroso E R, Tong T C.et al Comparison of HIV infection risk behaviors among injection drug users from East and West Coast US cities. J Urban Health 200481260–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clatts M C, Heimer R, Abdala N.et al HIV‐1 transmission in injection paraphernalia: heating drug solutions may inactivate HIV‐1. J Acquir Immune Defic Syndr 199922194–199. [DOI] [PubMed] [Google Scholar]
- 25.United Nations Joint United Nations Programme on HIV/AIDS. Report on the global HIV/AIDS epidemic 2002. Geneva: UNAIDS, 2002