Abstract
Study objectives
There are contradictory perspectives on the importance of conventional coronary heart disease (CHD) risk factors in explaining population levels and social gradients in CHD. This study examined the contribution of conventional CHD risk factors (smoking, hypertension, dyslipidaemia, and diabetes) to explaining population levels and to absolute and relative social inequalities in CHD. This was investigated in an entire population and by creating a low risk sub‐population with no smoking, dyslipidaemia, diabetes, and hypertension to simulate what would happen to relative and social inequalities in CHD if conventional risk factors were removed.
Design, setting, and participants
Population based study of 2682 eastern Finnish men aged 42, 48, 54, 60 at baseline with 10.5 years average follow up of fatal (ICD9 codes 410–414) and non‐fatal (MONICA criteria) CHD events.
Main results
In the whole population, 94.6% of events occurred among men exposed to at least one conventional risk factor, with a PAR of 68%. Adjustment for conventional risk factors reduced relative social inequality by 24%. However, in a low risk population free from conventional risk factors, absolute social inequality reduced by 72%.
Conclusions
Conventional risk factors explain the majority of absolute social inequality in CHD because conventional risk factors explain the vast majority of CHD cases in the population. However, the role of conventional risk factors in explaining relative social inequality was modest. This apparent paradox may arise in populations where inequalities in conventional risk factors between social groups are low, relative to the high levels of conventional risk factors within every social group. If the concern is to reduce the overall population health burden of CHD and the disproportionate population health burden associated with the social inequalities in CHD, then reducing conventional risk factors will do the job.
Keywords: inequalities, coronary heart disease, population
There are two apparently contradictory epidemiological perspectives—one concerning the causes of social inequalities in coronary heart disease (CHD) and another concerning the causes of population levels of CHD.
The perspective from social epidemiology
In social epidemiology it is has been established that conventional risk factors—smoking, hypertension, and cholesterol (and by extension the behaviours that influence hypertension and cholesterol such as diet, alcohol consumption, and physical activity)—do not explain social inequalities in CHD. Studies explored this issue from the late 1950s,1,2 and by 1981 Rose and Marmot concluded that most social inequality in CHD “remains unexplained”(page 13).3 Exact quantification of how much social inequality in CHD is explained by statistical adjustment for conventional risk factors varies but estimates typically range from 15% to 40%. Such numbers will probably underestimate the role of conventional risk factors because of measurement error, the absence of data regarding conventional risk factors across the lifecourse, and incomplete modelling of their interactions. Nevertheless, the idea that conventional risk factors do not explain social inequalities in CHD has been so widely accepted,4,5,6,7,8,9,10 even by the current authors,11,12 that over the past 20 years it has become a core concept in understanding the causes of social inequalities in CHD and health inequalities more generally.
Two apparently reasonable conclusions have been drawn from this concept. Firstly, is that there must be other unidentified factors that account for social inequalities in CHD and this has motivated novel avenues of research, especially on psychosocial explanations (for example, stress, control, and social capital).13,14 Secondly, some have argued that interventions focused on health behaviours and conventional risk factors are unlikely to appreciably reduce health inequalities.15,16 The idea that conventional physiological risk factors and behaviours provide only modest explanation of social inequalities in health not only influences research agendas and funding but also intervention strategies and health policy.16,17
The perspective from CHD epidemiology
In CHD epidemiology it has been established that conventional risk factors do explain most cases of CHD in many populations.18,19,20,21,22 The INTERHEART study, involving about 15 000 cases and controls from 52 countries, showed that exposure to nine potentially modifiable risk factors accounts for at least 90% of the population attributable risk (PAR) for first myocardial infarction.23 Exposure to at least one of the four conventional risk factors—dyslipidaemia, smoking, hypertension, and diabetes—had a PAR of 76%, and this is probably a conservative estimate because hypertension and diabetes were based on self report. In the British regional heart study, Whincup and colleagues reported that after accounting for regression dilution bias, smoking, blood pressure, and cholesterol had a PAR of 81%.24 Data from three large US cohorts involving more than 350 000 people, showed that those with favourable levels (that is, below standard clinical cut off points) of conventional risk factors experienced from 77% to 92% lower relative CHD mortality.25 Data from the same cohorts showed that exposure to at least one conventional risk factor accounted for 87% to 100% of fatal CHD cases and 84% to 92% of non‐fatal CHD among men and women respectively.26 It is nevertheless possible that in some circumstances, other risk factors such as binge alcohol consumption can also make large contributions to the population burden of CHD, albeit via arrythmic and cardiomyopathic rather then the traditional atherothrombotic processes associated with chronic CHD mechanisms.27
A paradox
So how do the risk factors that account for most cases of CHD in a population apparently not account for social gradients in CHD, when social inequalities simply emerge from sub‐grouping the population according to some indicator of social position? Our objective in this study is to use prospective data from a large well characterised cohort to illustrate how this apparent paradox may arise. We will show that conventional risk factors do account for most cases of CHD but that they do not explain the relative social gradient in CHD. We will then show how this situation arises because of the epidemiological preference for contrasting and explaining risk on a relative rather than absolute scale.
Methods
We use prospective data on 2682 Finnish men in the Kuopio ischaemic heart disease risk factor study (KIHD).28,29 Baseline examinations were conducted from 1984 to 1989, with ascertainment of events through 1998. Our measure of social inequality was based on education, where we created three groups (primary school or less; some high school; completed high school or better).30 We stratified the population into lower and higher risk groups31 based on smoking (current compared with others) hypertension (> 140/90 mm Hg or medications), dyslipidaemia (low density lipoprotein >160 mmol/l) consistent with National Cholesterol Education Project (NCEP)/Adult Treatment Panel III (ATPIII) guidelines,32 and prevalent diabetes (fasting glucose ⩾6.1 mmol/l or diabetes drugs). Information on biological and behavioural risk factors was collected by standard procedures and has been described elsewhere.29 The outcome used here combines fatal (ICD9 codes 410–414) and non‐fatal CHD, classified according to MONICA criteria.33 We calculated the PAR associated with exposure to at least one risk factor and calculated absolute and relative risks associated with the educational inequalities in the whole KIHD population and a low risk segment of the population free from smoking, hypertension, dyslipidaemia, and diabetes. We used proportional hazard models to calculate the crude and adjusted relative educational inequalities in CHD. Hopelessness, defined as negative expectancies about oneself and the future, was measured by two questionnaire items that asked about the likelihood of reaching goals and the possibility of positive change in the future.34 The study received ethical approval from the University of Michigan Institutional Review Board.
Results
In this population, 34.7% were current smokers, 58.7% had hypertension, 42.7% had dyslipidaemia, 6.5% had diabetes, and 84.9% had at least one of these risk factors. There were 425 CHD events (108 fatal, 317 non‐fatal) during an average follow up of 10.5 years—402 (94.6%) occurred among men exposed to at least one of the conventional risk factors and more than 70% occurred among men who had at least two risk factors. We calculated the PAR for having at least one conventional risk factor to be 68% but this is an under‐estimate because they were measured with error,22 crudely categorised as simple dichotomous exposures, and taken from a single assessment at one point in the lifecourse.35 Nevertheless, our PAR is similar to the 76% found in the INTERHEART study23 and that more than 90% of cases occur among those exposed to at least one conventional risk factor is consistent with the findings from the large US cohorts.26
In table 1, we show the typical sort of analysis done in social epidemiology. Comparing those with less than a primary education with those with more than high school, the crude relative risk (RR) for CHD was 1.90 (95% CI:1.38 to 2.61). After control for conventional risk factors—smoking, hypertension, dyslipidaemia, and diabetes—the RR was 1.68 (95% CI:1.22 to 2.33)—a reduction in the excess RR of 24%. The crude social inequality adjusted for a psychosocial risk factor (hopelessness) was 1.65 (1.19 to 2.29)—a reduction in the excess RR of 28%.
Table 1 Age adjusted educational inequality in CHD with separate additional adjustment for conventional risk factors and hopelessness.
| (1) Relative risk adjusted for age only (least v most educated) | (2) Model 1 plus adjustment for smoking, hypertension, dyslipidaemia, diabetes | (3) Model 1 plus adjustment for hopelessness |
|---|---|---|
| 1.90 (1.38, 2.61) | 1.68 (1.22, 2.31) | 1.65 (1.19, 2.29) |
Based on these analyses, on one hand, we would conclude that most cases of CHD in this population can be attributed to conventional risk factors—consistent with observations from CHD epidemiology. On the other hand, adjustment for conventional risk factors explained only a modest proportion of the relative social inequality in CHD—consistent with observations from social epidemiology.
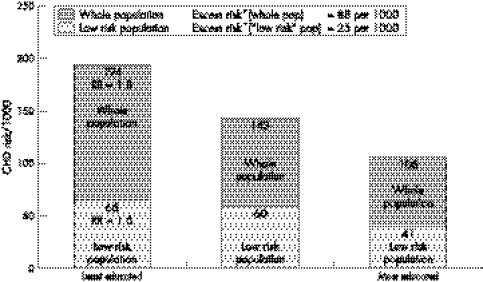
To illustrate what would happen to the social inequality and levels of CHD, if conventional risk factors were removed from the population, we excluded all men exposed to at least one conventional risk factor (84.9% of the sample and 94.6% of the cases) to create a low risk population.31 Table 2 shows the calculations of risk and both absolute and relative social inequalities in CHD in the whole population and in the low risk population (that is, not currently smoking, without hypertension, dyslipidaemia, or diabetes). If conventional risk factors were removed from the whole population, CHD risk would reduce by 64% from 158 to 57 per 1000. Among the least educated, risk would reduce by 66% from 194 to 66 per 1000. While a relative social inequality (RR = 1.61) would still remain in the low risk population, the absolute social inequality in CHD—as shown by change in the excess risk—would reduce by 72% from 88 to 25 per 1000 (fig 1).
Table 2 Distribution of cases of CHD by education in the whole KIHD population and a low risk subset of the KIHD population.
| Whole population (n = 2682) | Number (%) | Number of cases (%) | Risk per 1000 (95% CI) | Crude relative risk*† (95% CI) | Excess risk† (per 1000) (95% CI) |
|---|---|---|---|---|---|
| Education | |||||
| < Primary school | 1121 (41.8) | 218 (51.3) | 194 (171, 218) | 1.83 (1.36, 2.47) | 88 (51, 125) |
| Some high school | 1128 (42.1) | 161 (37.9) | 143 (122, 163) | 1.35 (0.99, 1.83) | 37 (1, 72) |
| High school graduate | 433 (16.1) | 46 (10.8) | 106 (77, 135) | 1.0 | 0 |
| Total | 2682 | 425 | 158 | – | – |
| Low risk population (n = 404, 15.1%) | |||||
| Education | |||||
| < Primary school | 122 (30.2) | 8 (34.8) | 66 (22, 109) | 1.61 (0.50, 5.18) | 25 (−34, 84) |
| Some high school | 184 (45.5) | 11 (47.8) | 60 (26, 94) | 1.46 (0.48, 4.48) | 19 (−33, 71) |
| High school graduate | 98 (24.3) | 4 (17.4) | 41 (2, 80) | 1.0 | 0 |
| Total | 404 | 23 | 57 | – | – |
*Crude relative risk is calculated directly from this cross tabulation and so is slightly different from the RH of 1.90 mentioned above, which is model based and accounts for survival time. †Compared with the highest education category. All confidence intervals for simple risk calculations and risk differences are asymptotic 95% CI. All confidence intervals for relative risks are Mantel‐Haenszel 95% CI.
Figure 1 Relative and excess risks associated with social inequality in CHD in the whole KIHD population and a low risk subset of that population. *Excess and relative risk compares least with most educated.
Discussion
Our intention in this paper was to show that explanations for social inequalities in CHD can depend on whether one is interested in explaining relative or absolute social inequalities. Certainly this approach needs to be examined in other populations. In this Finnish cohort, conventional risk factors account for the vast majority of CHD cases and for a substantial portion of absolute social inequalities in CHD. In a low risk population free from conventional risk factors, the excess risk among the least educated is 72% lower. This 72% reduction in excess risk is probably conservative, given our crude definition of a low risk population. On this point, table 3 shows that in the low risk population, there were no differences in overweight or blood pressure but the least educated men were more likely to be former smokers, have higher total cholesterol and low density lipoprotein (LDL), lower levels of vigorous physical activity and cardiorespiratory fitness, and were 4.5 cm shorter than better educated men. This suggests that there remain residual differences associated with known risk factors that are not captured by our clinically defined categorisation of low risk36 but that nevertheless may contribute to both overall levels and social inequalities in CHD risk in this segment of the population. Thus, it is probable that at least some of the residual absolute social inequality in CHD (excess risk = 25/1000) in the low risk population is also partly attributable to increased levels of conventional risk factors that did not meet out clinical cut‐points. However, it may also be the case that the residual social inequality in CHD that persists in a population with no conventional CHD risk factors is attributable to the direct effects of other novel mechanisms such as stress, job control, etc, that do not work through conventional risk factors. There are plausible hypotheses concerning direct psycho‐neuro‐endocrine mediation37 of social inequality that may bypass conventional risk factor mechanisms. Nevertheless, in this population such non‐conventional CHD mechanisms account for a small number of cases compared with those accounted for by conventional risk factor mechanisms. This should not be taken to mean that psychosocial processes are unimportant to CHD.38 When psychosocial processes influence behaviours and/or conventional risk factors they are extremely important antecedent causes of conventional risk factors. However, if psychosocial processes are hypothesised to not operate through conventional risk factors, then their contribution to population levels and absolute social inequalities in CHD may be small, but they may contribute importantly to relative CHD inequality.
Table 3 Distribution of selected characteristics (means or percentage) in the low risk population according to education.
| Risk factor | Education | p Value | ||
|---|---|---|---|---|
| <primary school | Some high school | High school graduate | ||
| Former smokers (%) | 58.20 | 53.26 | 48.98 | p<0.001 |
| HDL cholesterol (mmol/l) | 1.42 | 1.33 | 1.35 | p = 0.06 |
| LDL cholesterol (mmol/l) | 3.34 | 3.31 | 3.17 | p = 0.06 |
| Total cholesterol (mmol/l) | 5.24 | 5.17 | 4.99 | p = 0.02 |
| Diastolic blood pressure (mm Hg) | 81.61 | 81.00 | 80.53 | p = 0.41 |
| Systolic blood pressure (mm Hg) | 123.47 | 123.62 | 122.55 | p = 0.59 |
| Self report weight at 20 (kg) | 68.67 | 68.11 | 68.37 | p = 0.84 |
| Self report heaviest weight (kg) | 82.60 | 82.45 | 82.42 | p = 0.99 |
| Current weight (kg) | 77.33 | 78.10 | 78.02 | p = 0.84 |
| Height (cm)* | 171.42 | 173.70 | 176.09 | p<0.0001 |
| Vigorous physical activity (log h/y) | 3.83 | 4.28 | 4.68 | p<0.0001 |
| Cardiorespiratory fitness (ml 02/kg/min) | 33.08 | 35.04 | 36.56 | p<0.001 |
*Not adjusted for age.
Limitations
A potential limitation of these analyses is the assumption that all cases exposed to at least one of the conventional risk factors were actually caused by conventional risk factors singly or in combination.36 Additionally, we are aware of the theoretical limitations of using PAR to assess the contribution of certain risk factors to the amount of disease because it is possible that different combinations of risk factors can mean that the PAR can sum to more than 100%.39 Nevertheless, it is difficult to propose an alternative set of risk factors that might be the true causal culprits masquerading behind conventional risk factors. Thus, while attributing 94.6% of cases to conventional risk factors may be too high, we also know that the PAR is underestimated at 70%–75%. Wherever the true PAR lies between 70% and 95%, it is reasonable for the purposes of this illustration to conclude that the contribution of conventional risk factors to CHD is large and of major public health importance.20,21
A further limitation is that the illustration of overall and social inequality in CHD in the low risk segment of the population is admittedly based on small numbers as shown by the wide confidence intervals reported in table 2. However, this is unavoidable and results from the fact that the prevalence of conventional risk factors is high and the number of cases attributable to having at least one risk factor is high (94.6% of all cases). Our population is not overly extreme in this regard. Similarly small proportions of individuals with no conventional risk factors have been noted in other studies,25 and should be expected in populations where chronic CHD is a major cause of death.
Basing our estimates on the low risk population, as defined here, is nevertheless artificial, because it would not be possible in practice to entirely eliminate conventional risk factors from populations. However, our purpose was to show the principle behind examining these issues from both an absolute and relative perspective and so we have presented the most extreme case. A less extreme reduction in conventional risk factors (than the 100% shown here) would still substantially reduce the absolute burden of CHD associated with the social gradient because the prevalence of conventional risk factors is high (exceeds 80%) and the proportion of CHD cases attributable to them is high in each educational group, and this is a focus of future studies. Furthermore, if the change to a low risk population like the one described here could be achieved, this would be considered socially progressive because the absolute and relative reduction in CHD is largest among the least educated.40
Explaining relative and absolute social inequalities in CHD
When investigating relative social inequalities in CHD, the apparent paradox may arise that the factors that explain most cases of CHD do not seem to explain relative social inequalities in CHD. In our example, we showed that adjustment for conventional risk factors only reduced the relative educational inequalities in CHD by 24%. While this is an underestimate, such results are normally interpreted to mean that most of the effects of social inequality on CHD do not work through mechanisms linked to conventional risk factors,14 and so other potential causes of relative social inequalities need to be investigated. If we pursue this line of reasoning in these data, adjustment of the relative educational inequalities for a single identified psychosocial risk factor, such as hopelessness,34 reduces the relative educational inequality by 28%, compared with the reduction of 24% achieved by adjusting for four conventional risk factors. If we ignore that this effect of hopelessness on CHD is partly confounded by conventional risk factors, these results would normally be interpreted to mean that hopelessness is at least as important a mechanism for explaining the relative inequality as conventional risk factors. However, if we could intervene and remove all hopelessness from this population we would eliminate 14% of CHD cases, compared with over 90% of cases eliminated through removing smoking, hypertension, dyslipidaemia, and diabetes.
The extent to which a third variable reduces the RR in an exposure‐outcome association (sometimes taken as an indication of confounding of the association) depends on the relative distributions of the exposure over strata of the third variable and the strength of its association with the outcome. In this case there is a more extreme relative distribution of education over strata of hopelessness than over strata of the conventional risk factors (partly because the prevalence of conventional risk factors is high in this population), and so hopelessness seems to be a stronger confounder (in this case interpreted as a mechanism) of the association between education and CHD.
This situation is symmetrical with the point made by Geoffrey Rose two decades ago.41 If everyone in a population smoked, then relative social inequalities in lung cancer would be associated with social differences in other causes of lung cancer, such as asbestos exposure. However, while intervening on asbestos exposure would reduce relative social inequalities in lung cancer, it would do far less to mitigate the population burden of lung cancer because smoking causes most cases of lung cancer in all social groups. Evaluating the “importance” of different risk factors for elucidating the mechanisms behind social inequalities in CHD should not be based only on reductions in relative risk. It is widely recognised that a singular reliance on relative indicators can be misleading for both clinical practice42 and public health policy.43 Geoffrey Rose put it succinctly, “Relative risk is not what decision‐taking requires … relative risk is only for researchers; decisions call for absolute measures.” (page 19).44
Explaining the mechanisms behind relative social inequalities in CHD is a legitimate and important focus of research because it may lead to an understanding of novel and reversible CHD risk factors that will reduce social inequality in CHD. Nevertheless, explanations for relative social inequalities need to be understood within the context of what causes the population health burden of CHD—that is, what causes most cases of CHD. In populations where the prevalence of conventional risk factors is high, it is possible that there are small or even no differences in their prevalence across social groups such that they cannot account for relative CHD differences across social groups but contribute substantially to the absolute risk of CHD within all social groups.31 For instance, the Whitehall II study has reported no social inequality in perhaps the primary CHD risk factor—cholesterol.45 We have shown here that removing conventional risk factors from the population may have little effect on relative social inequalities but a large effect on absolute social inequalities as indicated by a reduction in the excess risk. Importantly, this also means that whatever proximal and distal factors may be proposed as causes of relative social inequalities in CHD, if their behavioural and biological mechanisms do not involve conventional risk factors then they probably account for a small proportion of CHD cases.
What is already known on this subject
Conventional risk factors seem not to explain social inequalities in CHD. Therefore, there must be other risk factors that generate the social gradient in CHD. This idea has become a powerful influence on how people understand social inequalities in CHD and what should be done to reduce them.
What this paper adds
Understanding the causes of social inequalities in CHD may depend on whether one is interested in explaining absolute or relative inequalities in CHD. Conventional risk factors account for the vast majority of CHD cases and for a substantial portion of absolute social inequalities in CHD—72% of the excess risk. An absolute risk approach to understand social inequalities in CHD focuses attention on those risk factors that cause most cases of disease attributable to social inequality. If the concern is to reduce the overall population health burden of CHD and the disproportionate population health burden associated with the social inequalities in CHD, then reducing conventional risk factors will do the job.
The effects of deliberate population interventions to reduce conventional risk factors are limited,46 but nevertheless, improvements in conventional risk factors have occurred in many countries47 and in all social groups, albeit unequally.48,49 Furthermore, their contributions to CHD decline via combinations of secular shifts, primary and secondary prevention has been reported in several countries.50,51 The determinants of cholesterol levels, blood pressure, and insulin resistance have not been fully explicated, and processes including fetal and early life development may be important. Improved understanding of the genesis of these conventional risk factors could increase ability to intervene effectively especially among children and adolescents.52
People make behavioural choices but they do so within layers of social context.12 Simply admonishing people for their bad habits is at worst victim blaming, at best naive. Health behaviours are influenced over the lifecourse35,52 at multiple levels by the material, psychosocial, cultural, and family conditions in which people live.53 The development and maintenance of smoking, diet, and exercise habits that influence levels of conventional CHD risk factors cannot be construed simply as the result of individual choice because choice is shaped by the physical, cultural, and social environments in which people live and work. A combination of population wide shifts in the distribution of risk factors and individual change strategies for those at high risk, in both early and later life is required. Ultimately this will mean engaging the political and economic forces that have interests in maintaining profits from the sale of products and services that influence conventional CHD risk factors.
Policy implications
The effectiveness of planned interventions to change levels of conventional risk factors and health behaviours has proved to be limited. Nevertheless, reducing levels of these risk factors will reduce the population health burden of social inequalities in CHD because it will reduce absolute risk in all social groups. We should increase our efforts to find ways to influence the multiple pathways from international, national, and local policy through to individual behaviour and treatment that will reduce conventional risk factors among current and future generations in richer and poorer countries.
The findings of this study in no way alleviate the need to better understand and ameliorate the uneven distribution of conventional CHD risk factors across social groups.12 However, using an absolute risk approach to understand social inequalities in CHD focuses attention on those risk factors that cause most cases of disease attributable to social inequality.54,55,56 So if the concern is to reduce the overall population health burden of CHD and the disproportionate population health burden associated with the social inequalities in CHD, then reducing conventional risk factors will do the job. We should increase efforts to find ways to influence the multiple pathways from international, national, and local policy46,57,58 through to individual behaviour that will reduce conventional risk factors among current and future generations in richer and poorer countries.
Acknowledgements
We thank George A Kaplan and Jukka T Salonen for access to the KIHD study data and George Kaplan and Hal Morgenstern for comments on an initial draft.
Contributions
All authors contributed to the analysis, interpretation, and writing of the manuscript.
Footnotes
Funding: JL and GDS were supported in part by the Robert Wood Johnson Foundation, Investigator Awards in Health Policy Research Program. The ideas expressed here are the authors and do not represent the Robert Wood Johnson Foundation. JL and KB were supported by grant 5P50 NDO3898605 from the National Institute of Child Health and Development. JL was additionally supported by grant HL44199 from the National Heart, Lung, and Blood Institute. SH was supported by a contract from the National Cancer Institute (263‐MQ‐314803). None of these funding agencies had any role in the conception, design, analysis, or writing of the manuscript.
Conflicts of interest: none.
References
- 1.Pell S, D'Alonzo C A. Blood pressure, body weight, serum cholesterol, and smoking habits among executives and nonexecutives. J Occup Med 19613467–470. [PubMed] [Google Scholar]
- 2.Holme I, Hjermann I, Helgeland A.et al Coronary risk factors and socioeconomic status: the Oslo study. Lancet 19763081396–1398. [DOI] [PubMed] [Google Scholar]
- 3.Rose G, Marmot M G. Social class and coronary heart disease. Br Heart J 19814513–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marmot M G, Shipley M J, Rose G. Inequalities in death—specific explanations of a general pattern? Journal Short Form workform 198411003–1006. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan G A, Keil J E. Socioeconomic factors and cardiovascular disease—a review of the literature. Circulation 1993881973–1998. [DOI] [PubMed] [Google Scholar]
- 6.Adler N E, Boyce W T, Chesney M A.et al Socioeconomic inequalities in health. No easy solution. JAMA 19932693140–3145. [PubMed] [Google Scholar]
- 7.Evans R G, Barer M L, Marmor T R.Why are some people healthy and others not?. New York: Aldine de Gruyter, 1994
- 8.Macintyre S. The Black Report and beyond: what are the issues? Soc Sci Med 199744723–745. [DOI] [PubMed] [Google Scholar]
- 9.Syme S L, Balfour J L. Explaining inequalities in coronary heart disease. Lancet 1997350231–232. [DOI] [PubMed] [Google Scholar]
- 10.House J S, Williams D R. Understanding and reducing socioeconomic and racial/ethnic disparities in health. In: Smedley B, Syme SL, eds. Promoting health: intervention strategies from social and behavioral research. Washington, DC: National Academy Press, 200181–124.
- 11.Davey Smith G, Shipley M J, Rose G. The magnitude and causes of socioeconomic differentials in mortality: further evidence from the Whitehall study. J Epidemiol Community Health 199044265–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lynch J W, Kaplan G A, Salonen J T. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med 199744809–819. [DOI] [PubMed] [Google Scholar]
- 13.Adler N E, Marmot M, McEwen B S.et alSocioeconomic status and health in industrial nations. New York: New York Academy of Sciences, 1999
- 14.Marmot M G.Status syndrome. New York: Times Books, 2004
- 15.Lantz P M, House J S, Lepkowski J M.et al Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of US adults. JAMA 19982791703–1708. [DOI] [PubMed] [Google Scholar]
- 16.Raphael D. Barriers to addressing the societal determinants of health: public health units and poverty in Ontario, Canada. Health Promotion International 200318397–405. [DOI] [PubMed] [Google Scholar]
- 17.Smedley B, Syme S L.Promoting health: intervention strategies from social and behavioral research. Washington, DC: National Academy Press, 2001 [PubMed]
- 18.Stamler J. Established major risk factors. In: Marmot M, Elliot P, eds. Coronary heart disease epidemiology. Oxford: Oxford University Press, 199235–66.
- 19.Yusuf S, Reddy S, Ounpuu S.et al Global burden of cardiovascular diseases: part 2: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation 20011042855–2864. [DOI] [PubMed] [Google Scholar]
- 20.Yusuf S, Reddy S, Ounpuu S.et al Global burden of cardiovascular diseases: part 1: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 20011042746–2753. [DOI] [PubMed] [Google Scholar]
- 21.Magnus P, Beaglehole R. The real contribution of the major risk factors to the coronary epidemics ‐ time to end the ‘only‐50%' myth. Arch Intern Med 20011612657–2660. [DOI] [PubMed] [Google Scholar]
- 22.Beaglehole R, Magnus P. The search for new risk factors for coronary heart disease: occupational therapy for epidemiologists? Int J Epidemiol 2002311117–1122. [DOI] [PubMed] [Google Scholar]
- 23.Yusuf S, Hawken S, Ounpuu S.et al Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case‐control study. Lancet 2004364937–952. [DOI] [PubMed] [Google Scholar]
- 24.Whincup P, Emberson J, Morris R.et al INTERHEART. Lancet 2005365117. [DOI] [PubMed] [Google Scholar]
- 25.Stamler J, Stamler R, Neaton J D.et al Low risk‐factor profile and long‐term cardiovascular and noncardiovascular mortality and life expectancy. Findings for 5 large cohorts of young adult and middle‐aged men and women. JAMA 19992822012–2018. [DOI] [PubMed] [Google Scholar]
- 26.Greenland P, Knoll M D, Stamler J.et al Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA 2003290891–897. [DOI] [PubMed] [Google Scholar]
- 27.Leon D A, Chenet L, Shkolnikov V M.et al Huge variation in Russian mortality rates 1984–94: artefact, alcohol, or what? Lancet 1997350383–388. [DOI] [PubMed] [Google Scholar]
- 28.Salonen J T. Is there a continuing need for longitudinal epidemiologic research? The Kuopio ischaemic heart disease risk factor study. Ann Clin Res 19882046–50. [PubMed] [Google Scholar]
- 29.Lynch J W, Kaplan G A, Cohen R D.et al Do cardiovascular risk factors explain the relation between socioeconomic status, risk of all‐cause mortality, cardiovascular mortality, and acute myocardial infarction? Am J Epidemiol 1996144934–942. [DOI] [PubMed] [Google Scholar]
- 30.Lynch J, Kaplan G A, Salonen R.et al Socioeconomic status and carotid atherosclerosis. Circulation 1995921786–1792. [DOI] [PubMed] [Google Scholar]
- 31.Stamler J, Neaton J D, Garside D B.et al Current status: six established risk major factors—and low risk. In: Marmot M, Elliott P, eds. Coronary heart disease epidemiology. Vol 2. London: Oxford University Press, 200432–70.
- 32.Cleeman J I, Grundy S M, Becker D.et al Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel Iii). JAMA 20012852486–2497. [DOI] [PubMed] [Google Scholar]
- 33.Tunstall‐Pedoe H, Kuulasmaa K, Amouyel P.et al Myocardial infarction and coronary deaths in the World Health Organization MONICA project—registration procedures, event rates, and case‐fatality rates in 38 populations from 21 countries in 4 continents. Circulation 199490583–612. [DOI] [PubMed] [Google Scholar]
- 34.Everson S A, Goldberg D E, Kaplan G A.et al Hopelessness and risk of mortality and incidence of myocardial infarction and cancer. Psychosom Med 199658113–121. [DOI] [PubMed] [Google Scholar]
- 35.Davey Smith G, Lynch J. Life course influences on coronary heart disease. In: Marmot M, Elliot P, eds. Coronary heart disease epidemiology. 2nd ed. London: Oxford University Press, 2005568–590.
- 36.Jackson R, Lawes C M M, Bennett D A.et al Treatment with drugs to lower blood pressure and blood cholesterol based on an individual's absolute cardiovascular risk. Lancet 2005365434. [DOI] [PubMed] [Google Scholar]
- 37.McEwen B S. Protective and damaging effects of stress mediators. N Engl J Med 1998338171–179. [DOI] [PubMed] [Google Scholar]
- 38.Lynch J W, Davey Smith G, Kaplan G A.et al Income inequality and mortality: importance to health of individual income, psychosocial environment, or material conditions. BMJ 20003201200–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health 19988815–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Victora C G, Vaughan J P, Barros F C.et al Explaining trends in inequities: evidence from Brazilian child health studies. Lancet 20003561093–1098. [DOI] [PubMed] [Google Scholar]
- 41.Rose G. Sick individuals and sick populations. Int J Epidemiol 19851432–38. [DOI] [PubMed] [Google Scholar]
- 42.Davey Smith G, Egger M. Who benefits from medical interventions? BMJ 199430872–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vågerö D, Erikson R. Socioeconomic inequalities in morbidity and mortality in western Europe. Lancet 1997350516. [DOI] [PubMed] [Google Scholar]
- 44.Rose G.The strategy of preventive medicine. Oxford: Oxford University Press, 1992
- 45.Marmot M G, Bosma H, Hemingway H.et al Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet 1997350235–239. [DOI] [PubMed] [Google Scholar]
- 46.Ebrahim S, Davey Smith G. Exporting failure? Coronary heart disease and stroke in developing countries. Int J Epidemiol 200130201–205. [DOI] [PubMed] [Google Scholar]
- 47.Evans A, Tolonen H, Hense H ‐ W.et al Trends in coronary risk factors in the WHO MONICA Project. Int J Epidemiol 20013035S–440. [DOI] [PubMed] [Google Scholar]
- 48.Fiore M C, Novotny T E, Pierce J P.et al Trends in cigarette smoking in the United States. The changing influence of gender and race. JAMA 198926149–55. [PubMed] [Google Scholar]
- 49.Cooper R, Cutler J, Desvigne‐Nickens P.et al Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: findings of the national conference on cardiovascular disease prevention. Circulation 20001023137–3147. [DOI] [PubMed] [Google Scholar]
- 50.Unal B, Critchley J A, Capewell S. Modelling the decline in coronary heart disease deaths in England and Wales, 1981–2000: comparing contributions from primary prevention and secondary prevention. BMJ 2005331614–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Laatikainen T, Critchley J, Vartiainen E.et al Explaining the decline in coronary heart disease mortality in Finland between 1982 and 1997. Am J Epidemiol 2005162764–773. [DOI] [PubMed] [Google Scholar]
- 52.Lynch J, Davey Smith G. A life course approach to chronic disease epidemiology. Annu Rev Public Health 2005261–35. [DOI] [PubMed] [Google Scholar]
- 53.Graham H. Gender and class as dimensions of smoking‐behavior in Britain—insights from a survey of mothers. Soc Sci Med 199438691–698. [DOI] [PubMed] [Google Scholar]
- 54.Emberson J R, Whincup P H, Morris R W.et al Social class differences in coronary heart disease in middle‐aged British men: implications for prevention. Int J Epidemiol 200433289–296. [DOI] [PubMed] [Google Scholar]
- 55.Marmot M. Risk factors or social causes? Int J Epidemiol 200433297–298. [DOI] [PubMed] [Google Scholar]
- 56.Emberson J R, Whincup P H, Morris R W.et al Reducing social inequalities and the prevention of coronary heart disease. Int J Epidemiol 2004331152–1153. [DOI] [PubMed] [Google Scholar]
- 57.Beaglehole R, Bonita R, Horton R.et al Public health in the new era: improving health through collective action. Lancet 20043632084–2086. [DOI] [PubMed] [Google Scholar]
- 58.Faergeman O.Coronary artery disease. Genes, drugs and the agricultural connection. Amsterdam: Elsevier, 2003