Abstract
Background
Patient complaints are associated with increased malpractice risk but it is unclear if complaints might be associated with medical complications. The purpose of this study was to determine whether an association exists between patient complaints and surgical complications.
Methods
A retrospective analysis of 16 713 surgical admissions was conducted over a 54 month period at a single academic medical center. Surgical complications were identified using administrative data. The primary outcome measure was unsolicited patient complaints.
Results
During the study period 0.9% of surgical admissions were associated with a patient complaint. 19% of admissions associated with a patient complaint included a postoperative complication compared with 12.5% of admissions without a patient complaint (p = 0.01). After adjusting for surgical specialty, co‐morbid illnesses and length of stay, admissions with complications had an odds ratio of 1.74 (95% confidence interval 1.01 to 2.98) of being associated with a complaint compared with admissions without complications.
Conclusions
Admissions with surgical complications are more likely to be associated with a complaint than surgical admissions without complications. Further research is necessary to determine if patient complaints might serve as markers for poor clinical outcomes.
Keywords: patient complaints, patient safety, surgical complications, quality of care
Despite a commonplace desire to reduce patient complaints, a dearth of information exists detailing why patients complain. Published studies have suggested that provider‐patient communication has a strong influence on patient complaints, and providers with better communication skills generate fewer complaints.1,2 Yet providers with more complaints are more likely to have risk management file openings and lawsuits even after adjusting for their clinical volume.3 Although communication factors have been shown to have a role in malpractice activity,4,5 it remains unclear whether patient complaints might also be associated with adverse patient outcome.
With an increasing awareness of the prevalence of medical injuries6 and a desire to deliver patient centred care,7 knowing if patients spontaneously identify and complain about adverse outcomes might support a more active solicitation of patient reporting. This study investigated whether an association exists between unsolicited patient complaints and surgical postoperative complications.
Methods
The primary outcome for this study was unsolicited patient complaints. The Office of Patient Affairs (OPA) at Vanderbilt University Medical Center collects and electronically records unsolicited patient complaints. Along with the patient narrative, the OPA records the patient's medical record number, complaint date, and location of the complaint. Patient narratives are then coded into different complaint categories using a validated coding scheme.8,9 This coding scheme includes six broad complaint categories with 35 subcategories. The six broad categories are: communication; care and treatment; humaneness; accessibility and availability; environment problems; and money or payment issues. A single patient narrative can be associated with multiple complaints. For example, if a patient called the OPA and reported waiting an excessive amount of time to see their provider and that their provider did not listen to their concerns, the complaint would be coded as both related to accessibility and availability and communication.
Postoperative complications were identified through the University Health System Consortium (UHC) database.10 UHC member institutions submit surgical discharge abstract information to the consortium which then uses Diagnostic Related Groups (DRGs) and International Classification of Disease version 9 (ICD‐9‐CM) codes to identify rates of 25 specific surgical complications (box 1). Other information collected within the UHC database includes patient demographic data, length of stay, admission urgency, discharge disposition, admitting provider, and operative surgeon.
Analytical plan
The UHC and OPA databases were linked to create the analytical database. The study period included data colleted from July 1995 to December 1999. Linkage criteria included an exact match on medical record number and a complaint date between the admission date and 30 days after discharge. The date range was restricted to increase the likelihood that the complaint was related to that admission.
After merging the two datasets, all non‐surgical specialties requiring operating room time such as obstetrics/gynecology and anaesthesiology were eliminated. Patients who had expired during their admission were also eliminated as this outcome would have reduced the opportunity to generate a complaint. We excluded ophthalmologists, who represent a larger volume of low risk procedures. Only admissions in which the operating physician and the attending physician were recorded as the same individual were included within the analysis in order to increase the likelihood that the patient had a single surgical caregiver. Complaints were considered related to a surgical admission if the hospital location identified in the complaint was a surgical unit. Finally, for patients with multiple admissions we included only the earliest admission date so each admission would represent a unique patient.
Box 1 Major postoperative complications identified by University Health System Consortium database
Postoperative stroke
Aspiration pneumonia
Postoperative pulmonary compromise
Postoperative gastrointestinal hemorrhage or ulceration
Postoperative urinary tract complications
Cellulitis or decubitus ulcer
Septicemia
Postoperative or intraoperative shock due to anesthesia
Reopening of surgical site
Mechanical complication due to device or implant
Miscellaneous complications of procedures
Shock or cardiorespiratory arrest
Complications relating to central/peripheral nervous system
Postoperative acute myocardial infarction
Postoperative cardiac abnormality except acute myocardial infarction
Postoperative infections except pneumonia and wound
Procedure related perforations/lacerations
Postoperative coma or stupor
Nosocomial pneumonia following procedure
Postoperative physiological and metabolic derangements
Complications related to anesthetic agents/CNS depressants
Venous thrombosis and pulmonary embolism
Wound infection
Post‐procedural hemorrhage or hematoma
Other complications of procedure
Characteristics between admissions associated with a complaint and admissions not associated with complaints were compared using χ2 tests for categorical variables and t tests for continuous variables. As hospital length of stay was significantly skewed, we used the Wilcoxon rank sum test to compare admissions associated with complaints with those not associated with complaints. Logistic regression models were constructed with patient complaint (yes/no) as the dependent variable. Only clinically significant variables were initially included in the model based on a priori hypotheses. The surgical subspecialty was dichotomized into general surgeons and non‐general surgeons. Patients' co‐morbidities were dichotomized into individuals with no co‐morbid conditions and those with one or more co‐morbid illness. The final model was adjusted for patient clustering by individual surgeons using generalized estimating equations.
All statistical calculations were performed using SAS software version 8.2. The Vanderbilt University Institutional Review Board reviewed and approved this study.
Results
Over the study period 16 713 individuals were admitted to the surgical services. Demographic information on the patients is presented in table 1. Major complications were reported in 12.6% of admissions. Only 0.9% (n = 151) of surgical admissions generated any unsolicited complaint.
Table 1 Demographic characteristics of study patients.
| Characteristic | Total (N = 16713) | Complaint associated with admission (N = 151) | No complaint associated with admission (N = 16562) | p value |
|---|---|---|---|---|
| Mean (SD) age (years) | 50.8 (17.6) | 49.2 (15.8) | 50.8 (17.6) | 0.23 |
| Sex, n (%) female | 7278 (43.6%) | 67 (44.4%) | 7211 (43.5%) | 0.84 |
| Race, n (%) white* | 14130 (87.7%) | 136 (92.5%) | 13994 (87.7%) | 0.08 |
| No (%) major complications | 2099 (12.6%) | 29 (19.2%) | 2070 (12.5%) | 0.01 |
| Median (IQR) length of stay (days) | 4 (2–7) | 5 (2–8) | 4 (2–7) | 0.02 |
| No (%) emergency or urgent admissions | 6286 (37.6%) | 62 (41.1%) | 6224 (37.6%) | 0.38 |
| No (%) with no co‐morbid illnesses† | 6853 (42.1%) | 54 (38.6%) | 6799 (42.2%) | 0.39 |
| No (%) general surgeon service | 4124 (24.l7%) | 40 (26.5%) | 4084 (24.7%) | 0.60 |
| No (%) commercial insurance source | 10673 (63.9%) | 98 (64.9%) | 10575 (63.9%) | 0.79 |
| No (%) discharged home | 15000 (89.8%) | 136 (90.1%) | 14864 (89.8%) | 0.90 |
*Data missing in 3.6% (n = 607) observations.
†Data missing in 2.9% (n = 448) observations.
A total of 132 unique surgeons were identified within the study, with 31 (23.5%) general surgeons, 29 (22%) otolaryngologists, 28 (21.2%) orthopedic surgeons, 13 (9.9%) urologists, and 10 (7.6%) neurosurgeons. The remaining 21 (15.9%) surgeons included cardiothoracic, vascular, trauma, and plastic surgeons.
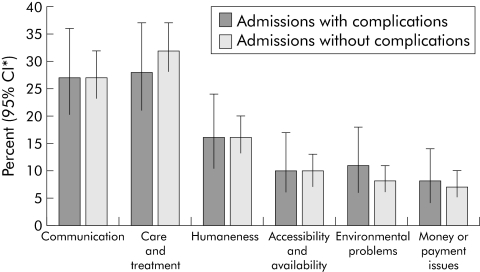
A total of 509 distinct complaints were identified within 151 admissions. The most common type of complaint concerned patient care and treatment, representing 28% (95% confidence interval (CI) 21 to 37) of complaints made by patients who experienced a surgical complication and 32% (95% CI 28 to 37) of complaints made by patients who had not experienced a complication. There were no statistically significant differences in complaint categories between patients who experienced a surgical complication and those who did not (fig 1).
Figure 1 Subject category of patient complaints. *CI, confidence interval.
Surgical admissions associated with patient complaints had a longer median length of stay than admissions without complaints (5 days v 4 days, p = 0.04). Major complications occurred in 19.2% of surgical admissions associated with a patient complaint and in 12.5% of admissions not associated with complaints (p = 0.01). Surgical admissions associated with a complication had an odds ratio of 1.74 (95% CI 1.01 to 2.98) of being associated with a patient complaint. This relationship remained significant after adjusting for patient length of stay, patient age, co‐morbid illness, surgical subspecialty, and patient race (table 2).
Table 2 Multivariate predictors of patient complaints.
| Characteristic* | Odds ratio (95% CI) |
|---|---|
| Manor complication status | |
| One or more complications | 1.74 (1.01 to 2.98) |
| Patient age | 0.99 (0.98 to 1.00) |
| Length of stay | 1.01 (1.00 to 1.02) |
| Patient race | |
| Non‐white | 0.52 (0.26 to 1.04) |
| Co‐morbid conditions | |
| One or more co‐morbid conditions | 1.03 (0.70 to 1.52) |
| Surgical specialty | |
| Surgical subspecialty† | 1.05 (0.60 to 1.81) |
*Referent categories for characteristics are no complication for “Major complication status”; white for “Patient race”; no co‐morbid conditions for “Co‐morbid conditions”; and general surgeon for “Surgical subspecialty”.
†Surgical subspecialties include otolaryngologists, urologists, neurosurgeons, cardiothoracic, orthopedic, vascular, trauma, and plastic surgeons.
Discussion
Patient dissatisfaction is an inevitable part of clinical care and most medical centers have designated individuals to receive and address complaints.11 Although patient‐provider communication can have a significant influence on whether a patient complains or not, it is unclear whether other aspects of the care experience (including complications) might also have an influence. In our study, surgical admissions associated with a patient complaint were more likely to be associated with major surgical complications, although overall the patient complaint rate was low.
Prior research has evaluated potential reasons behind unsolicited patient complaints. In a study which reviewed the narrative of over 12 000 patient complaints, 29% were categorized as related to care and treatment.9 These care and treatment assertions included diagnostic, treatment, and medication errors.2 While this study relied entirely on patient reports to identify care problems, our study used administrative data collected from discharge abstracts. Using a similar patient complaint scoring system, we found that less than a third of patient complaints associated with a surgical complication were coded as related to care and treatment.
One potential implication of our study is that patient complaints may have value as markers for poor clinical outcomes and might even serve as potential “sentinel events”. This differs from the traditional perception that patient complaints are predominantly representative of dissatisfaction with a healthcare provider or system. Previous research has suggested that patients regularly identify medical care errors and that patients could have an important role in improving patient safety and quality of care.12,13,14 Although patient complaints might represent an important source of information regarding poor clinical outcomes, it is important to note that a complaint was rare in our study, thus limiting the value of spontaneous patient complaints. As such, actively soliciting patient observations and complaints might be more useful in improving patient safety than a purely passive strategy.
We are unable to determine from this study whether surgical complications experienced by patients who complained are preventable or directly related to poor quality of care. Patients might have experienced a non‐preventable poor outcome and chose to register a complaint regardless of the quality of care provided. The decision to complain may be driven by the provider‐patient communication patterns surrounding the adverse outcome rather than the adverse outcome itself.15 Previous studies have suggested that negligence and quality of care may actually have little to do with malpractice suits.16,17 Indeed, a study by Morris et al determined that 69% of surgical patients who experienced an adverse event never filed a claim and, of the claims that were filed, 30% were withdrawn or dismissed before presentation to a jury.15 Nevertheless, with only a paucity of adverse events being identified through malpractice claims and risk management, more efficient and effective means of detecting substandard care are required.
Our study has several limitations. Firstly, the data on complications were based on ICD‐9‐CM codes and previous studies have suggested that administrative data can be inaccurate for detecting substandard care.18,19 Secondly, patient complaints were linked to an admission based on the timing of the complaint with respect to the admission. It is possible that some complaints might not have been associated with the surgical admission. Furthermore, some patients might have complained outside the 30 day limit we placed on the study.
In summary, patients with complaints associated with a surgical admission were more likely to have experienced a surgical complication than those who did not complain. However, very few patients actually complained over the course of the study, thus limiting the usefulness of spontaneously generated patient complaints as a marker for substandard surgical care. More active institutional efforts at promoting patient reporting as well as collecting and analyzing patient complaints might prove useful for identifying safety concerns associated with surgical care.
Acknowledgements
The authors thank Stephen Deppen and Martha Newton for their assistance in preparing the analytical database and the Department of Veterans Affairs, Tennessee Valley Healthcare System, GRECC Unit for its administrative support in the preparation of the manuscript.
Footnotes
Dr Murff is a VA Clinical Research Scholar, VA Clinical Research Center of Excellence. The funding organization had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, and in the preparation, review, or approval of the manuscript.
Competing interests: The authors report no conflict of interests related to this study or the preparation of this manuscript.
This study was reviewed and approved by the Vanderbilt University Institutional Review Board.
References
- 1.Hickson G B, Clayton E W, Entman S S.et al Obstetricians' prior malpractice experience and patients' satisfaction with care. JAMA 19942721583–1587. [PubMed] [Google Scholar]
- 2.Pichert J W, Miller C S, Hollo A H.et al What health professionals can do to identify and resolve patient dissatisfaction. Jt Comm J Qual Improv 199824303–312. [DOI] [PubMed] [Google Scholar]
- 3.Hickson G B, Federspiel C F, Pichert J W.et al Patient complaints and malpractice risk. JAMA 20022872951–2957. [DOI] [PubMed] [Google Scholar]
- 4.Hickson G B, Clayton E W, Githens P B.et al Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA 19922671359–1363. [PubMed] [Google Scholar]
- 5.Levinson W, Roter D L, Mullooly J P.et al Physician‐patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA 1997277553–559. [DOI] [PubMed] [Google Scholar]
- 6.Weingart S N, Wilson R M, Gibberd R W.et al Epidemiology of medical error. BMJ 2000320774–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corrigan J M, Kohn L T, Donaldson M S.et alCrossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press, 2001 [PubMed]
- 8.Hickson G B, Pichert J W, Federspiel C F.et al Development of an early identification and response model of malpractice prevention. Law Contemp Problems 1997278–29. [Google Scholar]
- 9.Pichert J W, Federspiel C F, Hickson G B.et al Identifying medical center units with disproportionate shares of patient complaints. Jt Comm J Qual Improv 199925288–299. [DOI] [PubMed] [Google Scholar]
- 10.University HealthSystem Consortium http://www.uhc.org
- 11.Allsop J, Mulcahy L. Dealing with clinical complaints. In: Vincent C, ed. Clinical risk management: enhancing patient safety. London: BMJ Publishing Group, 2001
- 12.Weingart S N, Toth M, Eneman J.et al Lessons from a patient partnership intervention to prevent adverse drug events. Int J Qual Health Care 200416499–507. [DOI] [PubMed] [Google Scholar]
- 13.Blendon R J, DesRoches C M, Brodie M.et al Views of practicing physicians and the public on medical errors. N Engl J Med 20023471933–1940. [DOI] [PubMed] [Google Scholar]
- 14.Weingart S N, Gandhi T K, Seger A C.et al Patient‐reported medication symptoms in primary care. Arch Intern Med 2005165234–240. [DOI] [PubMed] [Google Scholar]
- 15.Morris J A, Jr, Carrillo Y, Jenkins J M.et al Surgical adverse events, risk management, and malpractice outcome: morbidity and mortality review is not enough. Ann Surg 2003237844–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Entman S S, Glass C A, Hickson G B.et al The relationship between malpractice claims history and subsequent obstetric care. JAMA 19942721588–1591. [PubMed] [Google Scholar]
- 17.Brennan T A, Sox C M, Burstin H R. Relation between negligent adverse events and the outcomes of medical‐ malpractice litigation. N Engl J Med 19963351963–1967. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy E P, Iezzoni L I, Davis R B.et al Does clinical evidence support ICD‐9‐CM diagnosis coding of complications? Med Care 200038868–876. [DOI] [PubMed] [Google Scholar]
- 19.Weingart S N, Iezzoni L I, Davis R B.et al Use of administrative data to find substandard care: validation of the complications screening program. Med Care 200038796–806. [DOI] [PubMed] [Google Scholar]