Abstract
Problem
Rapid referral and management of patients with transient ischaemic attacks is a key component in the national strategy for stroke prevention. However, patients with transient ischaemic attacks are poorly identified and undertreated.
Design and setting
Before and after evaluation of quality improvement programme with controlled comparison in three primary care trusts reflecting diverse populations and organisational structures in an urban district in the North of England.
Key measures for improvement
The proportion of patients receiving antiplatelet drugs and safe driving advice on referral to a speciality clinic, and the numbers of referrals, adjusted for age, to the specialist clinic before and after the improvement programme.
Strategies for change
Interviews with patient and professionals to identify gaps and barriers to good practice; development of evidence based guidelines for the management of patients with transient ischaemic attacks; interactive multidisciplinary workshops for each primary care trust with feedback of individual audit results of referral practice; outreach visits to teams who were unable to attend the workshops; referral templates and desktop summaries to provide reminders of the guidelines to clinicians; incorporation of standards into professional contracts.
Effects of change
A significant improvement occurred in identification and referral of patients with transient ischaemic attacks to specialist clinics, with a 41% increase in referrals from trained practices compared with control practices. There were also significant improvements in the early treatment and safety advice provided to patients before referral.
Lessons learnt
A strategic approach to effective quality improvement across a diverse health community is feasible and achievable. Careful planning with patient and professional involvement to develop a tailored and multifaceted quality improvement programme to implement evidence based practice can work in very different primary care settings. Key components of the effectiveness of the model include contextual analysis, strong professional support, clear recommendations based on robust evidence, simplicity of adoption, good communication, and use of established networks and opinion leaders.
Keywords: quality improvement report, stroke prevention, clinical guidelines, transient ischaemic attacks, implementation of change
Stroke is the second most common cause of death worldwide1 and the predominant cause of adult neurological disability. There is now strong evidence that stroke prevention is a realistic proposition. The incidence of stroke is falling, despite an ageing population, owing to increased use of secondary preventive treatment and reduction of risk factors.2 One key element of stroke prevention is the management of patients with transient ischaemic attacks (TIAs). Since 15% of ischaemic strokes are preceded by a TIA,3 rapid access clinics have been advocated in national guidelines.4,5 Recent community based data confirm the early risk of stroke following TIA or minor stroke to be as high as 8–12% at 7 days.6 Patients suffering a TIA should be seen within the first few days for stroke prevention to be most effective. Despite the strong evidence of the benefits of secondary prevention, TIAs remain under‐recognised and undertreated.7 Only two thirds of UK hospitals have a neurovascular clinic and only just over half of these can see and investigate patients within 14 days.8
In 1999 a rapid access neurovascular clinic was established at Bradford Teaching Hospitals Trust to provide specialist review of all patients who had suffered a TIA. A multidisciplinary group of health professionals from primary and secondary care was convened to develop evidence‐based guidelines for the diagnosis, management, and referral of patients with TIA. There were three main goals of the guidelines: (1) to improve recognition of TIA symptoms; (2) to ensure that patients who had suffered a TIA were treated immediately with an antiplatelet agent and given advice not to drive; (3) to ensure that patients with suspected TIA were referred to the rapid access clinic for specialist review of diagnosis, investigations, and management.
A quality improvement strategy to support general practitioners in adopting the guidelines and achieving these goals was developed. It was based on methods that have been demonstrated to be effective in changing professional practice. The quality improvement strategy was pragmatic and based on interventions that were feasible and affordable. In order to evaluate the benefits of the strategy, it was implemented in one half of the local district with deferred implementation in the other half to provide a control comparison.
Setting
There are three primary care trusts in Bradford. Two (North Bradford and Bradford South and West with respective populations of 98 000 and 147 000) consist mainly of large partnerships (15 and 23 practices, respectively) and their populations are demographically and socioeconomically similar. Each has its own programme for training and development. The third (Bradford City, population 147 000, 42 practices) has a high proportion of single handed practices and a more culturally diverse and materially deprived population. Half of the practices in City had established a practice development programme that was run on a Wednesday and the other half on a Thursday. We randomly selected one of the peripheral South and West primary care trust, and one half of Bradford City practices to collaborate in developing a quality improvement programme and participate in a controlled before and after evaluation.
Box 1 Components of tailored and multifaceted change strategy
Developmental interventions
Four local consensus group meetings were convened between October 2002 and January 2003. These meetings of relevant stakeholders such as clinical governance leads, managers, and influential professionals from primary and secondary care were convened (a) to obtain commitment and ownership to improving quality of care using guidelines; (b) to adapt nationally recommended evidence based guidelines into a summarised local context; and (c) to identify barriers and incentives for changing practice and agree appropriate implementation strategies.
The draft guidelines were piloted in two meetings held in January 2003 with a broad range of stakeholders including staff, service users, and carers.
Dissemination interventions
A stepwise approach to disseminating the guidelines was taken in order to provide the greatest coverage of health professionals from the limited resources available.
Step 1: Education meetings. A protected learning time event for doctors, nurses and practice managers working in secondary care and across the interface of primary and secondary care was held in each primary care trust (PCT). An interactive approach was taken with small group discussions, problem based learning, case histories, and worked examples. Local opinion leaders were identified by each PCT and were given specific training about leading the meetings.
The aims of the education strategy were (a) to use existing education systems and events to promote the guidelines; (b) to establish local smaller “interactive” discussion groups adopting a variety of teaching methods, rather than larger didactic sessions; (c) to share local audit information and the expertise of local speakers; and (d) to provide events that were accessible, accredited, and met the needs of the target audience.
Step 2: Educational outreach visits. Following the education meetings, each practice was contacted by the relevant clinical governance lead and offered an outreach visit. Nineteen practices accepted the offer (nine in City PCT and 10 in South and West PCT). These were visited by the project leader who presented key messages from the relevant guideline and discussed the practice's implementation strategy during a 1 hour session. An information pack containing a range of materials to support implementation was given out at each visit (copies of the guideline, information leaflets, electronic and paper copies of referral forms).
Step 3: Postal dissemination. A copy of the information pack was posted to any practice that did not request a visit.
Reinforcing interventions
The guidelines were designed, piloted and presented in a clear and concise format to improve readability.
Guideline reminders were developed for clinicians; these included laminated posters, desktop coasters and electronic referral templates.
A marketing strategy was developed which included a tailored communication strategy to target health professionals through a variety of channels including internet and local intranets and meetings of key stakeholders.
Local service user and carers were actively involved in the development of the guidelines and patient information.
Strategies for change
Local ownership and involvement of relevant stakeholders was seen as a key step in achieving change (box 1). During the development of the guideline, interviews were undertaken with patients and professionals to identify gaps in current services, barriers to good practice, and educational needs. The TIA evidence base and aspects of cost effectiveness were reviewed by a multiprofessional group who met on five occasions. Draft versions of the guidelines were circulated widely to health professionals in the target practices to promote awareness about the topic and allow feedback on the emerging recommendations and guidance. Details of the implementation programme can be found at www.learnonline.nhs.uk/pace.
An audit of referrals to the rapid access clinic was undertaken to provide practice specific data on numbers of referrals and their appropriateness. A training workshop was run by local stroke specialists in South and West primary care trust and in City for the half of the practices selected for the change strategy. Those who attended included general practitioners, nurses, practice management staff, and pharmacists. These workshops used case histories and an interactive format to ensure relevance and participation and included feedback of the audit results. When representatives from practices were unable to attend the workshops, individual practice visits were offered to present and discuss the emerging guideline. A total of 19 outreach visits (9 in City and 10 in South and West) were arranged.
To remind clinicians about the diagnosis of TIA, criteria for referral and the treatment advice, specific paper and electronic referral forms were developed that provided prompts to reinforce the guidance. Key recommendations were also summarised on coasters that were distributed to general practitioners.
Finally, the importance of building change into the medical services contracts was recognised. For South and West primary care trust the audit results were linked to quality targets in the Personal Medical Services contract agreements.
Key measures of improvement
Three main outcome measures were identified: the numbers of referrals to the rapid access clinic and the number of patients with a confirmed diagnosis of TIA, both before (27 months—from the start of data recording at the clinic) and after (19 months—to the end of the funded evaluation) the intervention were measured. Following the intervention the proportion of TIA patients who were receiving an antiplatelet drug (either already prescribed, prescribed after the ischaemic event or contraindicated) when seen in the rapid access clinic was combined with the proportion of drivers who had been advised not to drive into a single outcome measure of overall compliance with best practice recommendations described in the guideline.
Effects of change
We found large overall differences in referral rates between City and the other two primary care trusts. The outcomes were therefore evaluated by comparing the two City groups, comparing South and West with North primary care trust, and combining these two comparisons in a single significance test, adjusted for age.
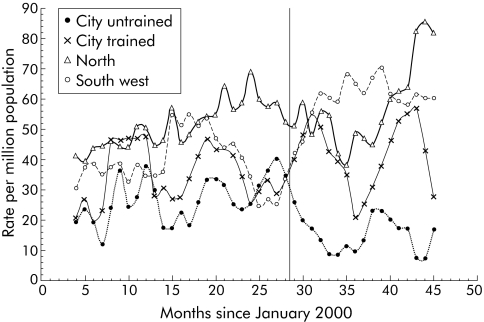
There was a significant difference in the change in referral rate to the rapid access clinic between the practices that were part of the quality improvement programme and those that were not (fig 1, table 1). There was a 41% increase in referrals from trained practices compared with control practices. This difference demonstrated improved access to specialist services for patients in the practices receiving training. Total referrals from the trained South and West primary care trust, which were initially lower than those in the North, rose to the same level after the intervention. Referral rates declined in the control (untrained) but not in the trained City practices. Rates for confirmed TIA diagnosis followed the same pattern, but the difference did not quite reach significance. Referral rates in the North rose in the final 6 months, possibly related to the spread of the guidelines and recommendations beyond the intervention practices.
Figure 1 Monthly appropriate referrals to TIA clinic by primary care trust group (moving average; intervention at 28 months).
Table 1 Referral rates in the different practices.
| N (rate per million per month) | City: control | City: TIA training | North: control | South and West: TIA training | Pooled significance† | Combined odds ratio estimate | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| N (rate) | Standardised rate | N (rate) | Standardised rate | N (rate) | Standardised rate | N (rate) | Standardised rate | |||
| Diagnosis of TIA | ||||||||||
| Before (27 months) | 29 (13) | (19) | 39 (22) | (25) | 113 (45) | (38) | 124 (30) | (27) | 0.089 | 1.33 |
| After (19 months) | 13 (8) | (12) | 31 (25) | (28) | 107 (61) | (48) | 147 (51) | (45) | ||
| Diagnosis not TIA | ||||||||||
| Before (27 months) | 9 (4) | (9) | 12 (7) | (8) | 40 (16) | (14) | 47 (11) | (12) | 0.054 | 1.82 |
| After (19 months) | 2 (1) | (3) | 12 (9) | (11) | 23 (13) | (11) | 42 (14) | (14) | ||
| Total referrals | ||||||||||
| Before (27 months) | 38 (17) | (28) | 51 (28) | (34) | 153 (61) | (51) | 171 (41) | (38) | 0.018 | 1.41 |
| After (19 months) | 15 (10) | (15) | 43 (34) | (39) | 130 (74) | (59) | 189 (65) | (60) | ||
†Mantel‐Haenzel χ2 test.
Adherence to best practice standards was significantly higher in practices that had received the training programme than in the controls (table 2). The improvement occurred principally for driving advice for the non‐City practices and for the antiplatelet advice for the City practices. This may reflect the higher car ownership in the more affluent non‐City areas, and the existing high levels of aspirin prescribing that limits scope for improvement.
Table 2 Compliance with best practice recommendations in the different practices.
| N (%) complying with best practice recommendations | City: control | City: TIA programme | Standardised difference in % (TIA – AF) | North: control | SW: TIA programme | Standardised difference in % (trained – untrained) | Pooled significance† | Combined odds ratio (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Total n | 15 | 43 | ∗ | 130 | 187 | ∗ | ∗ | ∗ |
| Driving advice | 12 (80.0%) | 35 (81.4%) | 0.1% | 75 (57.7%) | 133 (71.1%) | 13.3% | 0.010 | 1.9 (1.2 to 3.2) |
| Antiplatelet drugs | 11 (73.3%) | 37 (86.0%) | 15.4% | 120 (92.3%) | 167 (89.3%) | −3.7% | 0.714 | 0.9 (0.4 to 1.8) |
| Both recommendations | 8 (53.3%) | 29 (67.4%) | 15.5% | 70 (53.8%) | 122 (65.2%) | 11.3% | 0.016 | 1.8 (1.1 to 2.8) |
∗Standardised or adjusted for age and sex.
†Mantel‐Haenzel χ2 test.
Lessons learned
The National Service Framework for Older People stipulates that patients suffering from a TIA should be referred urgently to a rapid response neurovascular clinic using a locally agreed protocol.5 This intervention improved the identification and referral of patients who had had a TIA to specialist services where they could be appropriately investigated and treated. In addition, there was an improvement in the early treatment of patients with effective antiplatelet agents and the provision of safe advice about driving. The increase in the number of inappropriate referrals following the change programme was small and non‐significant. It was felt that this increase was inevitable due to diagnostic uncertainty and was acceptable to ensure that the right patients received the right care at the right time.
A number of important components for achieving changes in professional practice have been identified.9 These include strategic planning, contextual analysis, and use of a multifaceted approach to implementation. The particularly novel aspects of our project included the stepwise and pragmatic intervention to improve quality, and our findings that a strategic approach to change is feasible and can be implemented across a diverse health community. The intervention described recognised the complex influences on professional behaviour and adopted a whole systems approach to change, covering as many aspects as we pragmatically could. Professionals were successfully involved in the collaborative development of evidence‐based guidelines and in the implementation of these guidelines using dynamic interventions that were informed by those targeted for change. This tailored and multifaceted change strategy recognised that people have different learning needs. A stepwise approach to meeting these needs allowed concentration on resource intensive one to one outreach visits for those who really wanted them. The importance of building quality improvement into professional contracts was recognised.
Box 2 Components of an effective implementation strategy used in study intervention
Contextual analysis at start of process to identify barriers and facilitators for change.
Strong professional support.
Clear recommendations of the clinical context.
Robust research evidence base demonstrating effectiveness of guidance.
Guidance that is not too complex or expensive to adopt.
Good communication and use of established social networks and opinion leaders.
There is an imperfect evidence base to inform how to change professional behaviour.10,11 This rigorously designed and conducted study used a before and after design with control comparisons to provide robust evidence about the effectiveness of an implementation programme. A recent evaluation of the impact of NICE guidance identified factors that were important in successful implementation.12 Our multifaceted intervention benefited from some of the key components identified from this study and previous reviews (box 2).
Conclusions
Healthcare organisations have limited resources for education and quality improvement and require better evidence about how to use these wisely. However, finding generalisable evidence that is appropriate to varied local contexts can be difficult. The model of change that is described here can be developed to provide a systematic approach to the implementation of evidence‐based practice across the health community. This model combines careful planning with a multifaceted approach to changing practice that can work in very different primary care settings. It is a major advance from the haphazard and poorly coordinated approach to dealing with national and local clinical guidelines that has existed historically, and it provides a structured and strategic framework for getting changes into clinical practice. Further research is required to determine if it is a generalisable and sustainable model for implementing the ever increasing volume of guidance in primary care.
Acknowledgements
The authors thank all the general practitioners and primary care staff in Bradford for their help and support in the success of this programme.
Footnotes
Funding: Department of Health.
Competing interests: none.
The project was reviewed and approved by the Bradford Local Ethics Committee
Further details on the guideline and supporting materials can be found at www.learnonline.nhs.uk/pace/Guidance + Documents.
References
- 1.Murray C J L, Lopez A D. Mortality by cause for eight regions of the world: global burden of disease study. Lancet 19973491269–1276. [DOI] [PubMed] [Google Scholar]
- 2.Rothwell P M, Coull A J, Criteret al Change in stroke incidence, mortality, case fatality, severity and risk factors in Oxfordshire, UK from 1981–2004 (Oxford Vascular Study). Lancet 20043631925–1933. [DOI] [PubMed] [Google Scholar]
- 3.Hankey G J. Impact of treatment of people with transient ischaemic attacks on stroke incident and public health. Cerebrovasc Dis 19966(Suppl 1)26–33. [Google Scholar]
- 4.Intercollegiate Working Party for Stroke National clinical guidelines for stroke. London: Royal College of Physicians, 2000
- 5.Department of Health National service framework for older people. London: Department of Health, 2001. (available at www.doh.gov.uk/nsf )
- 6.Coull A J, Lovett J K, Rothwell P M.et al Population based study of early risk of stroke after transient ischaemic attack or minor stroke implications for public education and organisation of services. BMJ 2004328326–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelly J, Hunt B J, Lewis R R.et al Transient ischaemic attacks: underreported, overdiagnosed, undertreated. Age Ageing 200130379–381. [DOI] [PubMed] [Google Scholar]
- 8.Intercollegiate Working Party for Stroke National sentinel audit of stroke organisational audit report. London: Royal College of Physicians, 2004
- 9.University of York Getting research into practice. Effective Health Care 1999
- 10.Grimshaw J M, Eccles M P, Walker A E.et al Changing physicians' behaviour: what works and thoughts on getting more things to work. J Contin Educ Health Prof 200222237–243. [DOI] [PubMed] [Google Scholar]
- 11.Greenhalgh T, Robert G, Bate P.et alHow to spread good ideas: a systematic review of the literature on diffusion, dissemination and sustainability of innovations in health service delivery and organisation. London: National Coordinating Centre for NHS Service Delivery and Organisation (NCCSDO), 2004
- 12.Sheldon T, Cullum N, Dawson D.et al What's the evidence that NICE guidance has been implemented? Results from a national evaluation. BMJ 2004329999–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]