Abstract
Developments in surgical technology and procedure have accelerated and altered the work carried out in the operating theatre/room, but team modelling and training have not co‐evolved. Evidence suggests that team structure and role allocation are sometimes unclear and contentious, and coordination and communication are not fully effective. To improve teamwork, clinicians need models that specify team resources, structure, process and tasks. They also need measures to assess performance and methods to train teamwork strategically. An effective training strategy might be to incorporate teamwork with other technical skills training in simulation. However, the measures employed for enhancing teamwork in training and practice will need to vary in their object of analysis, level of technical specificity, and system scope.
Keywords: teamwork, skill, surgery, training
Successful surgery and health care in general depends on effective teamwork.1 Evidence suggests that adverse events in surgery may often derive from an aspect of team system design.2,3,4,5 Enhancement of team performance in the operating theatre should therefore lead to increased safety. However, there is little research on teams in the operating theatre, so there are few models of teamwork for enhancing team performance.6 Change in surgical technology and procedures further exacerbate this problem.7 The development of minimally invasive surgery, for instance, has demanded an adaptation to new instruments and equipment.8,9 However, there has been little planning for preparing teams for that technology on any large scale.10,11 Adaptation to new technology is ad hoc and variable.12,13 Consequently, teamwork in the operating theatre is not as reliable as one would expect of a high risk domain.
Technological developments in surgery should parallel a broader system level analysis of human factors and ergonomics.14,15 Developments in other high risk domains provide valuable guidance for this, particularly on developing models and measures of teamwork in order to address the needs of professional training.16 However, it is stressed that teamwork measures designed for team training and assessment must reflect the technical requirements of teamwork in its context. This demands an understanding of what makes an effective team in terms of structure and process, together with a view that teamwork is integral to a professional's skill set for work in the operating theatre.
Structure of surgical teams
Team structure describes the arrangement of a team's composition. It reflects the way teamwork is organised and coordinated. Team structure enables individual team members to understand and appreciate their own functional roles and those of others.17 Explicit or anticipated team structure can serve to formalise behaviour, task allocation, roles, responsibility and authority.18 It therefore follows that team structure will vary according to the functional demands of the team, its tasks and objectives.
For some tasks a formalised hierarchical structure is an appropriate team design. For instance, procedural or line operations work such as checking equipment and instruments and general operating theatre preparation may be delegated to junior members of staff and guided by clear guidelines and protocol. More complex varied tasks may demand intense teamwork and team adaptation—for example, in shared planning, negotiation, and decision making. This less linear work may be inhibited by a hierarchical team structure and will therefore need a flatter collaborative structure. Operating theatre tasks and procedures vary within and between professional groups with a mix of procedural work and uncertainty, which may demand a mix of prescribed and fluid structuring.19
Ambiguity of team structure can lead to disagreement in teams on authority, task allocation, roles and responsibilities; this compromises team performance.20,21 This is evident in recent research of teamwork in the operating theatre. Lingard et al22 assessed verbal and non‐verbal exchanges in the operating theatre in a range of operations. Communication failures were frequent; communications were often too late, incomplete, or not received by those concerned and left unresolved. In one third of all ineffective communications recorded there were visible effects on team processes, including team tension, resource waste, delay, and procedural deviation. Lingard et al attributed their findings in part to ineffective team structure and protocol, a conclusion supported by subsequent research. Undre et al23 also found that operating theatre personnel tend to disagree on team structuring and show some dissatisfaction with teamwork. This is consistent with the finding by Grote et al24 that teamwork in the operating theatre lacks the formalisation of aviation cockpit crews.
Teamwork is not standardised in the operating theatre. Team performance will naturally vary if it depends heavily on team member familiarity rather than clear well structured work. This is especially so when teams are transient, as is often the case in surgery with high staff turnover and a dependence on agency staff. Indeed, a team may only perform as well as the model of effectiveness that is understood and shared among its members.17
Skills of professional teamwork
The implication is that effective team performance and training requires a clear specification of what exactly the team should be doing, when, where and how. A surgical textbook specifies the stages in an operation and the exact sequence of actions for a complex operation. Similarly, models of teamwork should also specify teamwork tasks and their sequences related to surgical work. Teamwork should be more standardised, but not over‐automated because work in the operating theatre is varied and ever changing with technology. Team performance depends on an agreement among team members on their work and agreement between their structure, behaviour, and the function it serves. Teamwork models must therefore derive from an analysis of tasks in their natural context.
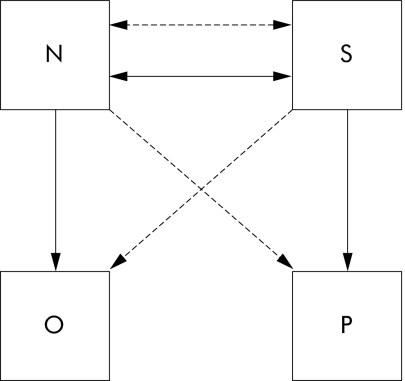
Teamwork behaviours are contingent upon the tasks and processes that serve a particular function—in other words, they are task dependent.25 The model shown in fig 1 schematically represents the traditional surgeon‐nurse set up where the surgeon conducts surgery using a wide range of instruments and provisions. These main tasks depend on a bidirectional exchange of objects and information. Both the nurse and surgeon therefore need skills in timing their exchanges and ensuring that what is communicated is clear, comprehensible, and of an appropriate volume and tone for that context. Both members of this unit need to monitor each other's states and their process in order to coordinate effectively; the nurse must anticipate the surgeon's requirements and the surgeon must appreciate that the nurse depends on others to work effectively. The surgeon primarily controls their work. However, the nurse may need to shift control temporarily if an issue or a problem arises that compromises their performance or the patient's safety.
Figure 1 Model of intraoperative teamwork between surgeon (S) and scrub nurse (N). This represents the traditional surgeon‐nurse set up where the surgeon conducts surgery with the assistance of the scrub nurse. The surgeon requests instruments and swabs (objects = O) and the nurse provides and confirms them. The two‐way arrows between the nurse and surgeon represent this exchange of information and object. The vertical arrows represent the action of the nurse or surgeon on the object or patient (P), respectively. The diagonal arrows with broken lines show that the surgeon is able to bypass the circuit of object exchange between surgeon and nurse—for example, in taking instruments from an instrument tray. The nurse is also able to remove instruments or objects from the patient and to tend to other aspects of surgery such as untangling tubes and wires from equipment.
Some technical demands of this teamwork are perhaps less obvious. For instance, are there crisis conditions that dictate the surgeon should bypass the nurse and take instruments directly from a trolley or tray? Scrub nurses help to maintain a tidy operative zone, but what other tasks or conditions change that rule? This team unit is not isolated in reality; it is embedded within a larger system. While operating, both the nurse and surgeon may have to attend to other systems. Mid operation, someone may ask the nurse a question regarding stock or the surgeon a question regarding the remaining cases of the day. In short, this team needs to share an understanding of the behaviours and skills required to work effectively.
Mapping teamwork skills to models
As shown in fig 1, professional skills are highly integrated and interdependent. Simplifying the complexity of a unit of teamwork in description is necessary for modelling and measuring teamwork. This allows trainers and trainees to discuss aspects of their work using a common understanding of terms. Defining teamwork models and developing measures of teamwork from them is a difficult challenge. Teamwork also has different levels of analysis, depending on the object and purpose of measurement.
Researchers developing broad observational measures of teamwork in surgery6,26 have adopted of a set of behavioural constructs adapted from the generalised model of teamwork developed by Dickinson and McIntyre,27 although there are other models to consider.28 Broad behavioural constructs act as a useful taxonomy; a model of teamwork achieved through a map of task dependent behaviours. For example, we can map the technical requirements described in the surgeon‐nurse teamwork to the following constructs:
cooperation, in terms of the response of team members to each others' requests;
communication, in terms of content, clarity of information exchange;
coordination, in terms of object and information exchange;
leadership, in terms of the effectiveness of team control;
monitoring, in terms of assessing each others' work and the situation.
Researchers have also made the distinction between task work and teamwork and defined teamwork as a non‐technical skill.25,29 This suggests that teamwork is not a task but a generic behaviour. However, the effectiveness of teams in surgery, such as that depicted in fig 1, depends on behaviours that are task‐specific. Communications can amount to tasks in a work protocol. Furthermore, the difference between a surgical task and a communication is not in the absence or presence of technicality, or whether one is a task or not; the difference is in behaviour, according to task demands.
Teamwork measures and their characteristics
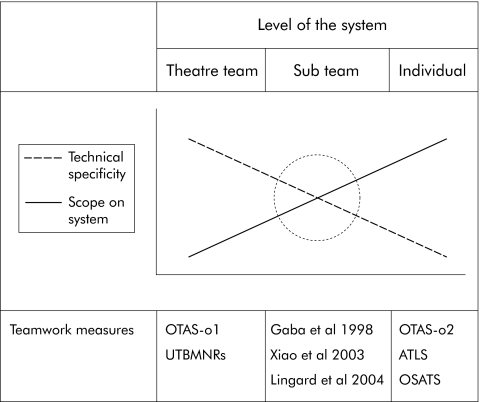
In defining teamwork assessments, we might instead describe them in terms of their object of analysis, technical specificity, and system scope. Figure 2 shows that an observational assessment of an individual's skill may specify a high level of technical detail but have very little system scope as it excludes the performance of other team members (for example, OSATS).30 Technical assessments naturally isolate certain tasks and exclude associated tasks in that system of work such as the surgeon‐nurse interaction. In contrast, an assessment accounting for the whole team in surgery may be low in technical specificity but higher in scope, such as the Anaesthetists' Non‐Technical Skills (ANTS) developed by Fletcher et al.31 Some team assessments might be even broader in their system scope and include constructs such as team cohesion or team culture that serve to characterise large teams, groups or organisational units. Different types of assessment may employ similar constructs such as communication and coordination. However, as assessments differ in object and purpose of measurement, models of teamwork are likely to need different sets of constructs to reflect the level of task detail and the level of the system under analysis.
Figure 2 Simple representation of a spectrum of teamwork measurement showing teamwork measures for surgery and associated work in theoretical categories to illustrate their basic differences. These characteristics relate to different levels of technical specificity and system scope. Where measures have multiple components, they may lie on different positions within the spectrum of teamwork measurement. Measures are also likely to overlap in their characteristics. ATLS, Advanced Trauma Life Support; OSATS, Objective Structured Assessment of Technical Skills;30 UTBMNRs, University of Texas Behavioural Markers for Neonatal Resuscitation;26 OTAS, Observational Teamwork Assessment in Surgery with components (o1 and o2).6 The circle denotes a theoretical optimal teamwork measurement for training and assessment in surgery.
Implications for team assessment
We can form several predictions from the arguments provided, in view of the limitations naturally placed on team assessment and training design. Measures that are very broad and fail to account for specific tasks and their demands will be less effective in measuring team performance than measures that do account for specific tasks and their demands. However, broad measures may be useful for describing aspects of large systems of teamwork. Measures that are very high in technical specificity may be practicable for training individuals or small teams separate from larger teams. However, highly technical measures exclude demands needed to perform within the context of the wider teamwork environment. For example, we might assess surgeons on their individual skills in a surgical simulator (for example, OSATS), perhaps focusing on leadership and communication. However, those teamwork elements may not account for the wider system of teamwork between the surgeon, anaesthetist and circulating nurses, and other external demands.
The model in fig 2 suggests that, in order to assess any given unit of teamwork, the ideal assessment may be one that optimises technical specificity and scope. This suggests using a single assessment which specifies the behaviour that is contingent upon certain tasks and processes—for example, the assessment by Gaba et al of anaesthetists' work.32 Alternatively, an effective assessment may comprise two separate components, one comprising a task checklist and the other a set of behavioural scales.6
Implications for teamwork skills training
Our aim must be to identify effective and ineffective teamwork in the operating theatre for modelling purposes, to build upon the former and to reduce the latter. This would afford transfer of best practice from one team to another and a specification of the resources needed for one procedure or another. The result may be an overall improvement in safety and in the work experience in the operating theatre for all involved, and prevention of unhelpful group behaviours and attitudes that tend to permeate health care.33 Task analysis and ergonomic studies need to determine and document team processes, structure, and behaviours in context.
Team training for the operating theatre needs strategic design to make use of multiple methods of teamwork skills training. There will be numerous team units to assess; table 1 illustrates the various arrangements for the main professional groups in the operating theatre. Observation offers a valuable method of measuring teamwork objectively and useful for studying a range of team factors and is particularly useful for feedback exercises in team training.34 Clearly, any modelling of the whole operating theatre team must involve representatives from all theatre professionals. There are numerous other issues to address in training teamwork skills; these are covered in a number of reviews which provide valuable lessons and guidance from team training in other high risk domains.25,35
Table 1 Spectrum of teamwork measurement in the system of surgery, including anaesthesia.
| Observational measures for teamwork skills training | |||
|---|---|---|---|
| Object of analysis | Professional individual | Intraprofessional team | Interprofessional team |
| Professionals | A, N or S | A‐A, N‐N or S‐S | S‐A, S‐N, A‐N or A‐N‐S |
| Teamwork assessment | ANTS (2003) | Gaba et al (1998 ) | OTAS (2004) |
This table cites tools that assess individuals and teams on teamwork in varying degrees of technical specificity. ANTS, Anaesthetist's Non‐Technical Skills Assessment; OTAS, Observational Teamwork Assessment in Surgery; A, anaesthetists; N, nurses; S, surgeons and their combinations. The hyphen (‐) denotes interaction within or between professional groups.
Team training in a simulated operating theatre
Team training scenarios can take place in a virtual operating theatre with a moderate fidelity mannequin as the virtual patient.36 Realistic surgical crisis scenarios incorporate technical difficulties for all team members including anaesthetists, nurses and surgeons. The concurrent problems have included difficult intubation, venous haemorrhage and cardiac arrest, and additional problems for nurses and operating department practitioners. Clinicians and psychologists assessed individual skill in teamwork and problem solving. After the simulation participants supplied ratings of their own performance to compare with those of trainers, and also received individual and collective feedback on their performance. Training and assessment of broader teamwork behaviours and individual work met some of the criteria mentioned, as it was high in technical specificity and broad in scope. However, we need to develop a more integrated approach to skills training. It is also unclear what sort of training individuals should have before they enter full scale simulation. How many training sessions do clinicians need? What is the best strategy for teamwork skills training in surgery?
Organisational factors
There are many challenges for establishing standardised, efficient, and effective teamwork training in the hospital context. The development of teams will demand more integration of clinicians and team researchers in the measurement process, at least in the development stage. Paradoxically, the conditions for such collaboration define a learning culture that has yet to be established. Structures for promoting safety in the workplace do exist,37 and a considerable body of knowledge and guidance is available on teamwork and team performance in other domains. This should inform the development of teamwork in health care. To develop models of performance and to implement them in practice, there needs to be a joint investment of resources at all levels within a generative healthcare organisation.38
Conclusions
Ad hoc adaptation to new technology and procedures in the operating theatre is unlikely to produce the reliable teams that one might imagine would exist now and in the future. Training in the principles of teamwork and generic teamwork skills may be beneficial, but training teamwork skills independent of tasks and of context will have limited benefit. The aim, of course, is to improve the technical skills of surgeons, nurses, and anaesthetists so that they can reliably deal with the demands of existing and new procedures in the operating theatre. By definition, a technical skill refers to any actions or mental faculty acquired through practice and learning pertaining to a particular craft or profession.39 On that basis, teamwork is a technical skill. Team training in surgery must be based on effective and valid models and measures of teamwork which account for the behaviours and processes demanded of particular tasks and context. Indeed, a technical rationale to teamwork engineering may be the only way to convince healthcare practitioners of the value of team research, training, and other intervention measures devised to improve system safety.
Footnotes
Funding: Patient Safety Research Program, Department of Health, London and BUPA Foundation, London, UK.
Competing interests: none.
References
- 1.Borrill C, Carletta J C, Carter A.et alThe effectiveness of health care teams in the National Health Service. Final Report to Department of Health. London: Department of Health, 2001
- 2.Brennan T A, Leape L L, Laird N M.et al Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med 1991324370–376. [DOI] [PubMed] [Google Scholar]
- 3.Vincent C, Taylor‐Adams S, Stanhope N. Framework for analyzing risk and safety in clinical medicine. BMJ 19983161154–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kohn L T, Corrigan J M, Donaldson M S.To err is human: building a safer health system Washington, DC: National Academy Press, 1999 [PubMed]
- 5.Reason J. Human error: models and management. BMJ 2000320768–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Healey A N, Undre S, Vincent C A. Developing observational measures of performance in surgical teams. Qual Saf Health Care 200413(Suppl I)i33–i40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nyssen S. Integrating cognitive and collective aspects of work in evaluating technology. IEEE Transactions on Systems, Man, and Cybernetics—Part A: Systems and Humans 200434743–748. [Google Scholar]
- 8.Welty G, Schippers E, Grablowitz V.et al Is laparoscopic cholecystectomy a mature technique? Surg Endosc 200216820–827. [DOI] [PubMed] [Google Scholar]
- 9.Veelen M, Nederlof E, Goossens C.et al Ergonomic problems encountered by the medical team related to products used for minimally invasive surgery. Surg Endosc 2003171077–1081. [DOI] [PubMed] [Google Scholar]
- 10.Cuschieri A. Whither minimal‐access surgery: tribulations and expectations. Am J Surg 1995169745–746. [DOI] [PubMed] [Google Scholar]
- 11.Strasberg S M, Ludbrook P A. Who oversees innovative practice? Is there a structure that meets the monitoring needs of new techniques.J Am Coll Surgeons 2003196938–948. [DOI] [PubMed] [Google Scholar]
- 12.Edmondson A C. Speaking up in the operating room: how team leaders promote learning in interdisciplinary action teams. J Manage Stud 2003406 [Google Scholar]
- 13.Carthey J, de Leval M R, Reason J T. The human factor in cardiac surgery: errors and near misses in a high technology medical domain. Ann Thorac Surg 200172300–305. [DOI] [PubMed] [Google Scholar]
- 14.Calland J, Guerlain S, Adams R.et al A systems approach to surgical safety. Surg Endosc 2002161005–1014. [DOI] [PubMed] [Google Scholar]
- 15.Vincent C, Moorthy K, Sarker S K.et al Systems approach to surgical quality and safety: from concepts to measurements. Ann Surg 2004239475–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baker D P, Gustafson S, Beaubien J.et alMedical teamwork and patient safety: the evidence‐based relation. Literature review. AHRQ Publication No. 05‐0053. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ), 2005
- 17.Rouse W B, Cannon‐Bowers J A, Salas E. The role of mental models in team performance in complex systems. IEEE Transactions on Systems, Man and Cybernetics—Part A: Systems and Humans 1992221296 [Google Scholar]
- 18.Tesluk P J, Mathieu E, Zaccaro S J. Task aggregation issues in the analysis and assessment of team performance. In: Brannick MT, Salas E, Prince C, eds. Team performance assessment and measurement: theory, methods, and applications. Series in applied psychology. Mahwah, NJ: Lawrence Erlbaum Associates, 1997
- 19.Xiao Y, Seagull F J, Mackenzie C F.et al Adaptation of team structure of trauma resuscitation teams. Proceedings of the Human Factors and Ergonomics Society 46th Annual Meeting 2002569–573.
- 20.Gladstein D. Groups in context: a model of group task effectiveness. Admin Sci Q 198429499–517. [Google Scholar]
- 21.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care 200413(Suppl I)i85–i90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lingard L, Espin S, Whyte S.et al Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care 200413330–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Undre S, Sevdalis N, Healey A N.et al Teamwork in the operating room: cohesion or confusion? J Eval Clin Pract 200612182–189. [DOI] [PubMed] [Google Scholar]
- 24.Grote G, Zala‐Mezö E, Grommes P. The effects of different forms of co‐ordination on coping with workload. In: Dietrich R, Childress TM, eds. Group interaction in high‐risk environments. Germany: Ashgate 200439–55.
- 25.Paris C, Salas E, Canon‐Bowers J A. Teamwork in multi‐person systems: a review and analysis. Ergonomics 2000431052–1075. [DOI] [PubMed] [Google Scholar]
- 26.Thomas E J, Sexton J B, Helmreich R L. Translating teamwork behaviours from aviation to healthcare: development of behavioural markers for neonatal resuscitation. Qual Saf Health Care 200413(Suppl I)i57–i64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dickinson T L, Mcintyre R M. A conceptual framework for teamwork measurement. In: Brannick MT, Salas E, Prince C, eds. Team performance assessment and measurement: theory, methods, and applications Series in applied psychology. Mahwah, NJ: Lawrence Erlbaum Associates, 1997
- 28.Militello L G, Kyne M M, Klein G.et al A synthesized model of team performance. Int J Cognit Ergon 1999131131–158. [Google Scholar]
- 29.Fletcher G, McGeorge P, Flin R.et al The role of non‐technical skills in anaesthesia: a review of current literature. Br J Anaesth 200288418–429. [DOI] [PubMed] [Google Scholar]
- 30.Martin J A, Regehr G, Reznick R.et al Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 199784273–278. [DOI] [PubMed] [Google Scholar]
- 31.Fletcher G, Flin R, Mcgeorge P.et al Anaesthetists' non‐technical skills (ANTS): evaluation of a behavioural marker system. Br J Anaesth 200390580–588. [DOI] [PubMed] [Google Scholar]
- 32.Gaba D M, Howard S K, Flanagan B.et al Assessment of clinical performance during simulated crises using both technical and behavioural ratings. Anesthesiology 199889123–147. [DOI] [PubMed] [Google Scholar]
- 33.Lingard L, Reznick R, Espin S.et al Team communications in the operating room: talk patterns, sites of tension, and implications for novices. Acad Med 200277232–237. [DOI] [PubMed] [Google Scholar]
- 34.Annett J, Cunningham D, Mathias‐Jones P. A method for measuring team skills. Ergonomics 2000431076–1094. [DOI] [PubMed] [Google Scholar]
- 35.Salas E, Burke C S, Bowers C A.et al Team training in the skies: does crew resource management (CRM) training work? Human Factors 200143641–674. [DOI] [PubMed] [Google Scholar]
- 36.Aggarwal R, Undre S, Moorthy K.et al The simulated operating room: comprehensive training for surgical teams. Qual Saf Health Care 200413(Suppl I)i27–i32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilson K A, Burke C S, Priest H A.et al Promoting health care safety through training reliability teams, Qual Saf Health Care 200514303–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hudson P. Applying the lessons of high‐risk industries to health care. Qual Saf Health Care 2003127–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Trumble W R, Stevenson A. eds. The Shorter Oxford Dictionary. 5th edn. Oxford University Press 2002