Abstract
High concentration oxygen therapy has long been a mainstay of prehospital treatment. Guidelines for its administration have for many years also cautioned its use with patients with chronic obstructive pulmonary disease (COPD).1 Successive guidelines and prehospital textbooks have advocated the use of 28% oxygen masks and re‐emphasised the importance of the dangers of hyperoxia, often drawing upon the classic theory of hypoxic drive. Despite this, the reality remains that ambulance crews have tended to overoxygenate such patients. One study demonstrated that 80% of patients sampled with acute exacerbation of their COPD received oxygen in excess of 28% from the ambulance crew.2 Is this a worrying development or a reassuring sign that prehospital providers are rightly more concerned about the dangers of hypoxia than hyperoxia? And if the guidelines are right, then how are the hearts and minds of ambulance paramedics and technicians won?
Keywords: Prehospital care, hyperoxia, COPD
It was not so long ago that ambulance crews regarded oxygen as something approaching a wonderdrug. Cheap and clean, a sort of medical wet‐wipe – “something to freshen you up, sir”. Not always therapeutic, but never harmful. Apocryphal stories of oxygen‐induced apnoea seemed a long way off. In an age where frontline ambulance crews are adopting more and more clinical skills, we need to re‐evaluate if overoxygenation is harmful, and if so, by what mechanism does it occur? Just like any other drug, we need to understand the benefits and the problems associated with oxygen. More than that, we need to believe it. Re‐examining how COPD hyperoxia occurs increases our understanding of the dangers of treatment and goes some way to avoiding the adverse consequences associated with overoxygenation. A far more complex and altogether more credible picture emerges than the classic view of hypoxic drive.
Oxygen is arguably the most widely used therapeutic agent used in the prehospital care environment. Metabolic reactions occurring with insufficient oxygen lead to acidosis. Thus hypoxia, poor oxygenation of the tissues, is associated with a high mortality and can lead to diminished consciousness, cardiac arrhythmias and subsequent cardiac arrest within minutes. Supplementary oxygen is indicated whenever tissue oxygenation is impaired.
Chronic obstructive pulmonary disease is characterised by airflow obstruction, which is usually progressive, not fully reversible, and does not change markedly over several months. The disease is predominantly caused by smoking.3 It is estimated that approximately 900 000 patients in England and Wales have been diagnosed with COPD although the numbers may be closer to 1.5 m allowing for underdiagnosis.4,5 In 1999 approximately 30 000 deaths were related to COPD in the UK, amounting to about 5% of all deaths.6 Morbidity is also high, with up to 1 in 8 emergency hospital admissions due to COPD each staying for 9 days on average. It thus represents a major cause of mortality and morbidity and furthermore has a major economic impact, directly costing the NHS £491 m.5 How such patients are treated by healthcare professionals in the hospital and prehospital environments is therefore of great importance.
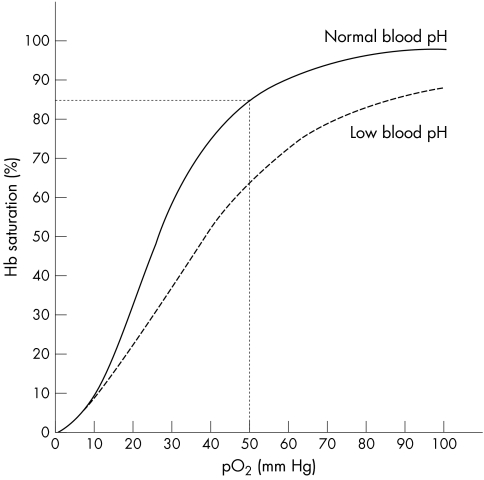
Respiratory failure is not uncommon during acute exacerbations of COPD, as impaired external respiration leads to reduced oxygen tension (<8 kPa) with or without carbon dioxide retention. Type I respiratory failure is characterised by hypoxaemia without hypercapnia whilst patients with type II respiratory failure showed hypoxaemia with an elevated PaCO2 (between 6.0 kPa and 6.7 kPa).7,8,9,10 Good saturation is still possible, however, with considerably diminished oxygen tension (fig 1). A number of papers have explored arterial oxygen tension (PaO2) levels in the hope of establishing what constitutes a ‘safe' level of hypoxaemia. Despite mixed results, figures of around 50 mmHg (6.7 kPa) have attracted a certain consensus, providing a basis for the original guideline saturation of over 85%, although other recommendations vary between 85 and 92%.3,7,11,12,13,14 Significant variation is possible, and acclimatisation to considerably lower levels has been noted in some asymptomatic COPD patients. In one study, 13 out of 15 COPD patients developed a PaO2 below 50 mmHg when undertaking light exercise in simulated aircraft cabin pressures and yet remained asymptomatic.15 Healthy examples are also available. Acclimatised mountaineers exercising at 19 000 feet have been noted with saturations as low as 36%‐ a figure usually associated with hypoxic death.16 Whilst occurring by differing mechanisms, acclimatisation is thought to occur due to an increase in minute ventilation and a secondary polycythemia (erythrocytosis), increasing the carrying capacity of the blood. Whilst beneficial in the short term, excessive red blood cells causes circulatory problems due to increases in blood volume and viscosity.
Figure 1 Oxygen‐haemoglobin dissociation curve at normal body temperature.
Around 10% of patients admitted to hospital with acute exacerbations of their COPD present with type II respiratory failure.7 Carbon dioxide retention and pH are indirectly linked, due to the formation of carbonic acid in the blood, but when occurring over an extended period, a compensatory metabolic alkalosis is likely to develop. Thus many such COPD patients are found to have a raised PaCO2 without a concomitant decrease in pH. During acute exacerbations, however, this mechanism is too slow and may already be operating at limit, resulting in acidaemia. Reduction of blood pH below 7.3 is associated with depression in neurological and cardiorespiratory function and multi‐organ failure and is associated with a higher incidence of ICU admission and heavy costs.17,18 Reduction in pH also results in a rightward shift in the oxyhaemoglobin dissociation curve and a reduced saturation at a given oxygen tension (fig 1). Whatever the aetiology, hypercapnia and/or acidosis develop at a much slower rate than hypoxaemia.
Whilst hypercapnia occurs secondary to increasing severity of respiratory failure, surprisingly the highest PaCO2 levels have been noted following oxygen therapy.7,19 Indeed it is almost impossible for the PaCO2 to be above 100 mmHg (13 kPa) or the pH to be below 7.16 unless the patients have been oxygenated. Many such patients experience a resolution of this hypercapnia following reduction in oxygen concentration.7,20
During the 1950s and 60s, it was postulated that administration of high concentration oxygen to patients dependant on hypoxia to stimulate their breathing might lead to a progressive decline in this hypoxic respiratory drive, a reduction in ventilation and subsequent hypercapnia.21 Whilst some studies have questioned the role of hyperoxic respiratory depression as the primary mechanism for hypercapnia, a slight reduction in minute ventilation remains a likely cause of carbon dioxide retention.22,23,24,25,26,27 Many non‐specialist textbooks have over‐emphasised the reduction in ventilation, hypothesising that the patient would become bradypnoeic, hypoxic, and ultimately apnoeic. The effects of hypercapnia and acidosis have been less well‐emphasised.
Even in the late 1960s, the classic understanding of ‘hypoxic drive' was proposed only in conjunction with oxygen‐induced relief of hypoxic pulmonary vasoconstriction (HPV). HPV occurs in COPD patients with poorly ventilated pulmonary regions where hypoxia causes localised vasoconstriction to occur in the pulmonary capillaries, balancing ventilation, and perfusion. Reoxygenation of these pulmonary capillaries causes vasodilatation and creates a significant ventilation‐perfusion mismatch and an increase in physiological dead space in some COPD patients.28 This mechanism has gained in acceptance over recent years. Higher concentrations of oxygen may also result in absorption atelectasis due to alveolar denitrogenation, further reducing lung function, whilst it is postulated that the Haldane effect (the binding of oxygen and haemoglobin resulting in an increase in unbound CO2 and a reduction in pH) may also result in slight increases in systemic acidity.
In some medical circles, the very existence of overoxygenation is still hotly contended. Many intensive care specialists in particular still remain sceptical that high concentration oxygen may cause retention of carbon dioxide. Many have highlighted significant problems with some retrospective studies which correlate poorer patient outcome with use of high concentration oxygen without establishing that groups contained patients of a similar severity. A large scale, well‐controlled trial is still called for by most parties.
It is likely that hyperoxic‐induced hypercapnia is mediated by an altogether more complicated set of mechanisms than previously understood within the standard medical (and especially prehospital) textbooks. The relative contributions of HPV, absorption atelectasis, respiratory depression, and the Haldane effect, as well as some other possibilities remain the main focus of research. A genetic cause for individual susceptibility to carbon dioxide retention is by no means out of the question.
Vacillating over the underlying physiological mechanism behind hyperoxic‐induced hypercapnia may seem rather unimportant when discussing prehospital oxygen therapy for the COPD patient. Notwithstanding the need for further studies and the objections of the intensivists, the evidence suggests that COPD hyperoxia is associated with greater mortality and morbidity and a good indicator of ICU or other ‘more complicated' and costly admissions.7 Yet it is also true that excessive prehospital oxygen prescription stems in part from a poor understanding of the consequences and presentation of hypercapnia and an arguably justifiable mistrust of the simplistic mechanism they believe to mediate it.
Among front line ambulance crews, the view persists that COPD patients with a good saturation and an adequate respiratory rate cannot be hyperoxygenated, since they are clearly not hypoxaemic or bradypnoeic. The spectre of hypoxic drive continues to haunt the perception of the issue. One well‐known prehospital textbook advocates use of uncontrolled oxygen with all COPD patients, commenting (correctly) on the dearth of evidence supporting the concept of severe, sudden, oxygen‐induced hypoventilation and apnoea.29 No mention is made of the problems of carbon dioxide retention and respiratory acidosis.
Most studies rightly reinforce the importance of focusing on the dangers of hypoxaemia, especially in the prehospital environment. Furthermore, in the absence of arterial blood gas analysis, detection of hypercapnia and acidosis is difficult, verging on impossible. Clinical manifestations include headache (partly due to an increase in cerebral blood flow), depression, drowsiness, and reduced level of consciousness. Tremor and even occasional seizures are possible, whilst reflex vasoconstriction and peripheral vasodilatation may accompany tachycardia. Clearly, distinguishing hypercapnia from hypoxaemia from such clinical signs and symptoms is not a viable proposition.
In the light of the problems of overoxygenation, a number of schemes to identify COPD patients at increased risk of carbon dioxide retention with the use of credit card size warning cards are being piloted.30,31,32 This is hoped to help with continuing problems of poor identification of COPD patients, both by themselves, relatives and ambulance crews. One study found that only 35% of patients correctly identified themselves as COPD, while 47% of them thought they had asthma. A similarly poor recognition was seen with ambulance crews.33 However, such schemes are far from foolproof. In a small study, only 5 of 19 patients showed their card on readmission to hospital and the authors suggested such cards would be ineffective without vigorous and continuing staff and patient education.34
Whether detected or not, the number of treatment options available for ambulance crews are very limited and ultimately come down to titrating oxygen concentration to saturation. Maintaining a saturation above 85% avoids the problems of hypoxaemia in the chronically hypoxic patient, whilst minimising the risk of carbon dioxide retention.35 Emphasising the rationale for such a treatment is especially important for the prehospital clinician, since any adverse effects associated with hyperoxia will rarely be seen or appreciated by the crew. Hypercapnia is unlikely to manifest itself in the ambulance, even during extended journeys. Should bradypnoea occur before arrival at hospital, this is far more likely to be due to exhaustion than hypercapnia.36
Nevertheless, appreciation of the long‐term impact of oxygen‐induced hypercapnia is an important objective for the ambulance service. Maintaining COPD saturation around the 90–93% mark seems counterintuitive when 100% oxygen and a much higher saturation is available.37 Nevertheless this may result in substantially favourable outcomes for the minority of COPD patients at risk of retention. However, inappropriate oxygen prescription is likely to continue to some degree until prehospital carers gain a greater understanding of the dangers of hypercapnia and the true mechanisms by which respiratory acidosis occurs. Explanations based on the semi‐mythical, poorly evidenced and rightly mistrusted theory of classical hypoxic drive are unlikely to consolidate prehospital use of low flow oxygen.
References
- 1.Institute of Health and Care Development Ambulance Service Basic Training Manual Bristol, IHCD 1997
- 2.Dennison A K O, O'Brien C, Stableforth D. The use of oxygen in acute exacerbations of chronic obstructive pulmonary disease: a prospective audit of pre‐hospital and hospital emergency management. Clin Med 20005449–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Institute for Clinical Excellence Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care, Clinical Guideline. London: NICE, 12, 2004
- 4.Soriano J B, Maier W C, Egger P.et al Recent trends in physician diagnosed COPD in women and men in the UK. Thorax 200055789–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The National Collaborating Centre for Chronic Conditions Chronic Obstructive Pulmonary Disease:National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary care. Thorax 200459(SuI) pp 1–NaN232. [PMC free article] [PubMed] [Google Scholar]
- 6.Office for National Statistics Mortality statistics: Cause, 1999. London: HMSO, 2000
- 7.Plant P K, Owen J L, Elliott M W. One year period prevalence study of respiratory acidosis in acute exacerbations of COPD: implications for the provision of non‐invasive ventilation and oxygen administration. Thorax 200055550–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelly A M, McAlpine R, Kyle E. How accurate are pulse oximeters in patients with acute exacerbations obstructive airways disease? Respir Med 200195336–340. [DOI] [PubMed] [Google Scholar]
- 9.Moloney E D, Kiely J L, McNicholas W T. Controlled oxygen therapy and carbon dioxide retention during exacerbations of chronic obstructive pulmonary disease. Lancet 2001357526–528. [DOI] [PubMed] [Google Scholar]
- 10.Madison J M, Irwin R S. Chronic Obstructive Pulmonary Disease. Lancet 1998352467–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joint Royal Colleges Ambulance Liaison Committee Pre‐hospital Clinical Guidelines, Issue 1. London: JRCALC, 2001
- 12.Murphy R, Mackway‐Jones K, Sammy I.et al Emergency oxygen therapy for the breathless patient: Guidelines prepared by North West oxygen group. Emerg Med J 200118421–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pearson M G, Alderslade R, Allen S C.et al Guidelines for the management of COPD. Thorax 199752(5)S1–S28. [Google Scholar]
- 14.Siafakas N M, Vermeire P, Pride N B.et al Optimal assessment and management of chronic obstructive pulmonary disease : a European Respiratory Society consensus statement. Eur Respir J 199581398–1420. [DOI] [PubMed] [Google Scholar]
- 15.Christensen C C, Ryg M, Refvem O K.et al Development of severe hypoxaemia in chronic obstructive pulmonary disease patients at 2438 m altitude. Eur Respir J 200015635–639. [DOI] [PubMed] [Google Scholar]
- 16. In: Oh T E. ed. Intensive Care Manual. London: Butterworths, 1990
- 17.Murphy R, Driscoll P, O'Driscoll P. Emergency oxygen therapy for the COPD patient. Emerg Med J 200118333–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plant P K, Owen J L, Elliott M W. One year period prevalence study of respiratory acidosis in acute exacerbations of COPD: implications for the provision of non‐invasive ventilation and oxygen administration. Thorax 200055550–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Westlake E K, Simpson T, Kaye M. Carbon dioxide narcosis in emphysema. Q J Med94155–173. [PubMed] [Google Scholar]
- 20.Murphy R, Driscoll P, O'Driscoll P. Emergency oxygen therapy for the COPD patient. Emerg Med J 200118333–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Campbell E J M. The J Burns Amberson Lecture. The management of acute respiratory failure in chronic bronchitis & emphysema. Am Rev Respir Dis 196796626–639. [DOI] [PubMed] [Google Scholar]
- 22.Aubier M, Murciano D, Milic‐Emili J.et al Effects of administration of O2 on ventilation and blood gases in patients with chronic obstructive pulmonary disease during respiratory failure. Am Rev Respir Dis 1980122747–754. [DOI] [PubMed] [Google Scholar]
- 23.Sassoon C S, Hassell K T, Mahutte C K. Hyperoxic‐induced hypercapnia in stable chronic obstructive pulmonary disease. Am Rev Respir Dis 1987135907–911. [DOI] [PubMed] [Google Scholar]
- 24.Dick C R, Liu Z, Sassoon C S.et al O2‐induced change in ventilation and ventilatory drive in COPD. Am J Respir Crit Care Med 1997155(2)609–614. [DOI] [PubMed] [Google Scholar]
- 25.Robinson T D, Freiberg D B, Regnis J A.et al The role of hypoventilation and ventilation‐perfusion redistribution in oxygen‐induced hypercapnia during acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 20001611524–1529. [DOI] [PubMed] [Google Scholar]
- 26.Feller‐Kopman D, Schwartzstein R. The role of hypoventilation and ventilation‐perfusion redistribution in oxygen‐induced hypercapnia during acute exacerbations of chronic obstructive pulmonary disease‐ Reply to Robinson et al. (2000). Am J Respir Crit Care Med 20011631755. [DOI] [PubMed] [Google Scholar]
- 27.Calverley P M A. Oxygen‐induced hypercapnia revisited. Lancet 20003561538–1539. [DOI] [PubMed] [Google Scholar]
- 28.Madison J M, Irwin R S. Chronic Obstructive Pulmonary Disease. Lancet 1998352467–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Caroline N L.Emergency Care in the Streets. Philadelphia: Lippincott, Williams and Wilkins, 1995
- 30.Dennison A K O, O'Brien C, Stableforth D. The use of oxygen in acute exacerbations of chronic obstructive pulmonary disease: a prospective audit of pre‐hospital and hospital emergency management. Clin Med 20025449–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wolstenholme R J, Pilling A, Bassett C. Reply to Denniston et al. Clin Med 20033(2)183–184. [PubMed] [Google Scholar]
- 32.O'Driscoll R. The use of oxygen in acute exacerbations of chronic obstructive pulmonary disease: a prospective audit of pre‐hospital and hospital emergency management – Letters to the Editor. Clin Med 20033(2)183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dennison A K O, O'Brien C, Stableforth D. The use of oxygen in acute exacerbations of chronic obstructive pulmonary disease: a prospective audit of pre‐hospital and hospital emergency management. Clin Med 20025449–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wolstenholme R J, Pilling A, Bassett C. Reply to Denniston et al.Clin Med 20033(2)183–184. [PubMed] [Google Scholar]
- 35.Moloney E D, Kiely J L, McNicholas W T. Controlled oxygen therapy and carbon dioxide retention during exacerbations of chronic obstructive pulmonary disease. Lancet 2001357526–528. [DOI] [PubMed] [Google Scholar]
- 36.Singer M, Bellingan G. Reply to Denniston et al. Clin Med 20033(2)184. [PubMed] [Google Scholar]
- 37.Joint Royal Colleges Ambulance Liaison Committee Pre‐hospital Clinical Guidelines, Issue 3. London: JRCALC, 2004