Abstract
Objective
The purpose of this study was to validate an algorithm recommended by current literature for the patients with acute flank pain and evaluate the validity of bedside ultrasonography (US) performed by emergency physicians (EP) as a part of this algorithm.
Materials and methods
This prospective validation study was carried out over a 5 month period in a tertiary care hospital adult emergency department (ED) with annual attendance of 55 000. Adult patients presenting to the ED with unilateral acute flank pain during the study period were enrolled into the study consecutively. Oral consent was obtained after the protocol was briefly explained to the patient and before the administration of analgesia. A protocol form was recorded for each patient enrolled into the study, and patients were followed up under the guidance of a previously designated algorithm in the ED. Data were analysed with SPSS software. The χ2 test was used to compare the dichotomised data of patients, diagnosed with and without stones, and to select the significant parameters to be used in the logistic regression.
Results
Of the 227 patients enrolled, 176 were proven to have urinary tract stones. There were 122 patients discharged from ED without further investigation except urinalysis and bedside US. Of these 122 directly discharged patients, 99 had a urinary stone, and the others did not have a life threatening disorder. Four of the 227 patients were admitted to the hospital. The remaining 51 patients did not have stones detected, and their pain subsided. Having a previous history of stones, radiation of pain to the groin, accompanying nausea, and detection of pelvicalyceal dilatation using bedside US performed by the EPs were found to be the most significant parameters in determining urinary stones in logistic regression analysis. Sensitivity and specificity of these parameters were: previous history of stones 59% and 66%, radiating pain to the groin 68% and 49%, nausea 71% and 51%, and detection of pelvicalyceal dilatation by bedside US 81% and 37%.
Conclusion
Bedside US performed by EPs could be used safely in the evaluation of patients with acute flank pain as a part of a clinical algorithm. Previous history of urinary stones, radiation of pain to the groin, accompanying nausea. and detection of pelvicalyceal dilatation are major parameters and symptoms of urinary stone disease, and could be used in the algorithms.
Keywords: bedside ultrasound, emergency, renal colic
Management of patients with acute flank pain suspected for renal colic is often delayed in the emergency department (ED), because of time consuming laboratory examinations. Furthermore, requesting advanced tests and imaging for patients with non‐complicated renal colic in the ED may not be cost effective. Extensive investigation to detect urinary stone is not necessary. In addition to textbook chapters about emergency ultrasonography (US) usage in detecting urinary stones in patients complaining of acute flank pain, two algorithms have been published in the literature.1,2,3 The second algorithm is mainly about the treatment and disposition of the patients with acute flank pain rather than diagnostic issues. Therefore, Noble and Brown's algorithm2 was used for this study. This algorithm was designed mainly to exclude life threatening disorders such as abdominal aortic aneurysm or acute renal failure, and to prevent unnecessary delay in diagnosis and treatment in patients with acute flank pain in the ED. However, this algorithm has not yet been validated in daily medical practice.
Bedside US is a rapid, safe, and noninvasive imaging system for urinary obstruction and has been used by EPs in the ED not only to detect urinary obstructions but also to exclude other abdominal pathologies such as renal failure, aortic aneurysm, free fluid, and gallstones.2,3,4,5,6 Therefore, this study was designed to safely, effectively, and economically diagnose renal colic in patients presenting to the ED with acute flank pain while excluding other clinical conditions, using a safe and standard algorithm including bedside US and other diagnostic options.
MATERIALS AND METHODS
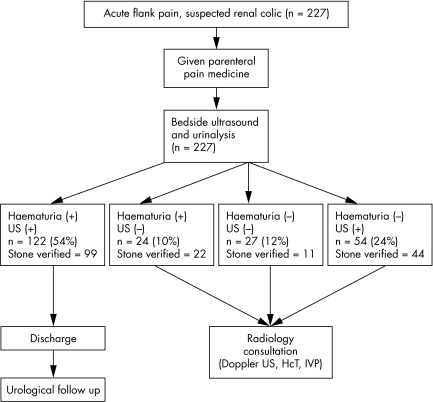
This prospective clinical study was carried out in an ED of a tertiary care university hospital with an annual attendance of 50 000. Patients who presented with complaints of unilateral acute flank pain suspected for renal colic were enrolled into the study. Before the study started, lecturers from each of the departments of emergency medicine, urology, and radiology developed a scientifically plausible algorithm consistent with the hypotheses and purposes of the study by referring to similar examples in the literature.1,2 Patient examinations, treatment and referral were conducted according to that patient flow chart (fig 1). Patients <14 years old, those with fever, who were pregnant, or who refused to give informed consent were excluded from the study. Each eligible patient was examined and an emergency physician or training resident filled a protocol form. After a detailed medical history and physical examination, patients were given analgesics in the form of a standard intravenous dose of 0.05 mg/kg morphine sulphate or 0.5 mg/kg meperidine and/or 75 mg intramuscular diclofenac sodium. If the pain persisted, a urologist's opinion was sought concerning the lack of response.
Figure 1 Emergency department algorithm of flank pain patients suspected for renal colic. US, ultrasound; HCT, helical computed tomography; IVP, intravenous pyelography.
Following the administration of analgesic, urine samples were taken from all patients for microscopic analysis, as indicated on the flowchart, and bedside US was performed in the ED by a senior emergency medicine training resident or a residency trained emergency physician, who had previously having undergone an hour long programme of bedside US training taught by a radiology specialist. The programme included information regarding renal pelvicalyceal dilatation and measurement of aortic diameter at the bedside. All senior emergency medicine training residents and physicians performing the bedside US as part of the algorithm had already been using it during their routine clinical practice before undergoing the programme specifically organised for the study.
Using bedside US, both kidneys were examined and compared for the presence of pelvicalyceal dilatation on the painful side. Abdominal aortic diameters were also measured to check for aneurysm. For aortic diameters, the following levels were used: diaphragmatic level, superior mesenteric artery level, coeliac trunk level, renal artery level, and 20 mm above the iliac bifurcation. Upper limit for aortic diameter was accepted to be 30 mm, with 25 mm being the median and 20 mm being the lower limit.5
Detecting 10 or more red cells on urinalysis (centrifuged at 700 g for 3 min) were regarded as microscopic haematuria and any value below that was regarded as absence of haematuria.6
After getting the results of urinalysis and bedside US, the patients were followed according to the algorithm. All patients were referred to the urology outpatient clinic to be examined by a urologist either on the same or a following day. The presence or absence of urinary stones in these patients were decided based on the results of the further diagnostic tests, obtained from outpatient clinic records, and the results of patient follow up. The patients who failed to present to the outpatient clinic, who were diagnosed not to have a stone, or whose file was not available, were contacted by phone in 2 months. These standard questions in the phone interview with such patients were as follows:
Have you passed the stone during urination?
Have you been to a follow up visit/check‐up?
If so, what was done and what were you told to do?
Were you diagnosed with another disease?
Has the pain recurred? If so, what did you do?
Based on the outpatient clinical records, follow up, and phone interviews, the patients were either diagnosed as having stones or not, with or without other pathologies, such as urinary tract infection, intestinal colic, and pelvic inflammatory disease. In this evaluation, those who had stones demonstrated on intravenous urography (IVU), urinary tract spiral computed tomography (CT), or US, or who had passage of the stone were regarded to be patients with proven stones, whereas those in whom no stone was demonstrated, the pain did not recur, and a different diagnosis was made were regarded not to have stones, and comprised the control group.
Statistical analysis
All prospective documented data were analysed with SPSS statistical package (version 10.0 for Windows). The χ2 test was used to compare the dichotomised data of patients, diagnosed with and without stones, and to select the significant parameters to be used in the logistic regression. The following parameters were also included in the logistic regression model as they are often used in clinical assessments: costovertebral tenderness, family history of stone, tenderness on the course of the ureter, accompanying sweating, and suprapubic tenderness. Statistical significance was set at p<0.05.
RESULTS
Of the 227 patients enrolled, 147 (64.8%) were men and 80 (35.2%) were women, with a mean (SD) age of 38.4 (14.0) years (median 37, range 16–76). Based on the diagnostic studies and follow up, 176 patients were proved to have a urinary stone, while the remaining 51 had none. Urinary stone disease was diagnosed with IVU, US, spiral CT, and spontaneous passage in 71, 40, 11, and 54 patients respectively. The mean (SD) ages were 38.7 (13.5) (median 37, range 17–76) and 37.3 (15.7) years (median 37, range 16–76) in the patients with and without stone, respectively.
Of the 227 patients, 122 had haematuria and a bedside US with pelvicalyceal dilatation, 24 had haematuria but a negative bedside US, 27 had neither haematuria nor a positive bedside US, and 54 had no haematuria but had a positive bedside US (fig 1). In the control group, a number of pathologies other than stones were diagnosed during the follow up, including urinary tract infection, ureterovesical junction obstruction, uterine myoma, ovarian cyst, renal cyst, and cholelithiasis. The final diagnosis of these patients is shown in table 1.
Table 1 Follow up results for the controls.
| Flow‐chart | Outpatient clinic or telephone follow up results | No. of patients | Total | |||
|---|---|---|---|---|---|---|
| Haematuria+, US+ | IVP normal. No diagnosis. Followed up | 9 | 23 | |||
| Lower urinary tract infection | 5 | |||||
| Ureterovesical junction obstruction | 1 | |||||
| Uterus myoma | 1 | |||||
| Ovarian cyst | 1 | |||||
| Renal cyst | 1 | |||||
| No examination. No pain. No diagnosis | 5 | |||||
| Haematuria+, US− | No problem in test results and follow ups. No pain | 2 | 2 | |||
| Haematuria−, US− | CUT, bedside US, radiological US, spiral urinary CT normal | 6 | 16 | |||
| Urine analysis, bedside US, radiological US normal. No pain in follow up | 5 | |||||
| Cholelithiasis | 1 | |||||
| Tests and IVP normal. | 1 | |||||
| Non‐specific abdominal pain. Hospitalised in general surgery ward and discharged after monitoring | 1 | |||||
| Food intoxication | 1 | |||||
| Tests normal. Lumber pain | 1 | |||||
| Haematuria−, US+ | Prostate carcinoma (previously diagnosed) | 1 | 10 | |||
| Medullary nephrocalcinosis | 1 | |||||
| Horseshoe kidney | 1 | |||||
| Diagnosis of lower urinary tract infection at ED | 1 | |||||
| Intestinal colic | 1 | |||||
| Diagnosis of pyelonephritis at ED | 1 | |||||
| No other diagnosis made | 3 |
IVP, intravenous pyelography; US, ultrasonography, CUT, complete urine test; CT, computerised tomography; ED, emergency department.
One patient with inadequate response to analgesics and with mid‐urethral stone, one patient with urinary retention and advanced hydronephrosis on US, and one patient with haemorrhagic renal cyst were hospitalised. Another patient whose aetiology of pain could not be determined at the emergency department was also hospitalised in the general surgery department. The remaining 223 patients were managed according to the procedure dictated in the patient flow chart and were discharged with recommendations of subsequent outpatient clinic visit after their pain relieved. No death or life threatening condition was recorded during the three‐month follow up period.
By χ2 test, radiation of pain to the groin (p = 0.024), previous history of stone (p = 0.020), accompanying nausea (p = 0.010), vomiting (p = 0.020), presence of macroscopic haematuria (p = 0.010), costovertebral tenderness (p = 0.036), presence of microscopic haematuria (p = 0.010), and detection of pelvicalyceal dilatation on bedside US (p = 0.008) were found to be significant parameters for detection of urinary stone.
Logistic regression analysis, which was conducted with the inclusion of these significant parameters as well as those frequently used in clinical assessment, indicated that radiation of pain to the groin (p = 0.035), previous history of stone (p = 0.006), accompanying nausea (p = 0.016), and detection of pelvicalyceal dilatation on bedside US (p = 0.038) were significant independent variables in predicting urinary stone (table 2).
Table 2 Logistic regression analysis results of parameters to detect urinary stone.
| Variable | LRC | Wald | SD | p* | OR | 95 % CI | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Radiation of pain | 0.751 | 4.469 | 1 | 0.035 | 2.119 | 1.056 to 4.251 | ||||||
| History of stone | 1.011 | 7.583 | 1 | 0.006 | 2.748 | 1.338 to 5.643 | ||||||
| Nausea | 0.844 | 5.783 | 1 | 0.016 | 2.326 | 1.169 to 4.629 | ||||||
| Costovertebral angle tenderness | 0.725 | 3.050 | 1 | 0.081 | 2.065 | 0.915 to 4.660 | ||||||
| No suprapubic tenderness | −0.766 | 3.676 | 1 | 0.055 | 0.465 | 0.212 to 1.017 | ||||||
| Bedside US positive | 0.781 | 4.289 | 1 | 0.038 | 2.184 | 1.043 to 4.573 | ||||||
| Constant | −2.640 | 7.735 | 1 | 0.005 | 0.71 | |||||||
LRC, logistic regression coefficient; Wald, value for Wald statistics. *p value for Wald statistics.
DISCUSSION
Three main subjects should be discussed as a result of this study: the validation of a currently available algorithm, bedside US performed by EPs as a part of this algorithm, and the value of other clinical signs and symptoms in this study. In the medical literature, there are many studies comparing emergency bedside US with other imaging modalities in renal colic.8,9,10 In most of these studies, US was performed by radiologists, technicians, or urologists, but by EPs in only four of them.8,10,11,12,13 The sensitivity and specificity of bedside US performed by EPs was found to be 72–92% and 73–96% respectively.11,12 Handerson found sensitivity for both kidney‐ureter‐bladder film and bedside US of 97.1%.8 However, Rowland found the accuracy of bedside US to be 58% even though the providers were given a three day US course before the study. Methodological differences, the quality of the equipment, the quality and length of US courses, and the experiences of providers could be the reason of mismatch between the studies. As a result, bedside US is being used in daily medical practice of EPs routinely and influences their clinical decision making.
In this study, a currently recommended algorithm was validated. With this algorithm, more than 50% of patients with acute flank pain were safely discharged from the ED without investigations other than urinalysis and bedside US performed by EPs. In this study, bedside US was found to have a sensitivity of 80.7%, specificity of 37.2%, χ2 value of 7.108, logistic regression analysis p value of 0.038, and odds ratio of 2.184. Sensitivity, specificity, and χ2 values for microscopic haematuria were 68%, 51%, and 6.707, respectively. Our study suggests that bedside US was more reliable than microscopic haematuria as a diagnostic tool for patients with suspected for renal colic. As US is an operator dependent technique, more structured and detailed training programmes may increase the diagnostic value of bedside US.
We also looked at the value of clinical signs and symptoms to detect urinary stone in patients with acute flank pain. It is known that flank pain may be accompanied by groin pain, particularly when the stone is in the ureter. Statistical analysis of our data revealed that when flank pain radiated to the groin, its sensitivity and specificity were 68.2% and 49% respectively, and reached statistical significance (p = 0.035) in logistic regression analysis. Similarly, accompanying nausea, which was reported to be one of the usual components of the disease,5 was found to be a significant (p = 0.016) predictor of stone disease in logistic regression analysis. Previous history of urinary stone disease was another significant parameter in our study, with sensitivity and specificity ratios of 59.1% and 66.7% respectively, and p value of 0.006 in logistic regression analysis. As observed in our results of the statistical analyses, diagnostic certainty is higher for patients with suspected renal colic (urinary stone disease) presenting to the emergency department with complaints of unilateral flank pain radiating to the groin, accompanied by nausea, and with a prior history of stone. The diagnosis for renal colic can be even more certain if bedside US detects pelvicalyceal dilatation.
This study has several limitations. Firstly, because US is an operator dependent technique, the results may be variable. Nevertheless, operator dependence of both techniques may have had an effect on our results. Secondly, it is possible that some of the patients in the control group may have missed a small stone during urination, or a stone of insufficient size may have been missed on IVU, US, or even spiral CT. If some of these patients had undetected stones, this may alter the sensitivity and specificities of certain clinical markers, which may be stated as another constraint of our study.
This study is the first to validate a current algorithm and prospectively investigate the clinical characteristics of patients with renal colic patients in the ED, and to combine these characteristics with bedside US. As a significant percentage of bedside US negative patients were ultimately proven to have renal stones, for safety this group of patients should have a secondary or follow up definitive diagnostic study, unless the accuracy of bedside US by EPs is shown to be much higher with further training and experience than in this study. Furthermore, addition to the algorithm of predictive parameters found to be significant in this study such as history of prior stone, radiation of pain to the groin, and accompanying nausea in the initial evaluation of the acute flank pain patients could improve its accuracy.
Abbreviations
CT - computed tomography
ED - emergency department
EP - emergency physician
IVU - intravenous urography
US - ultrasonography
Footnotes
Competing interests: there are no competing interests
References
- 1.Swadron S, Mandavia D P. Renal ultrasound. In: Ma OJ, Mateer JR, eds. Emergency ultrasound. New York: McGraw Hill Professional, 2002199
- 2.Noble V E, Brown D F M. Renal ultrasound. Emerg Med Clin N Am 200422641–659. [DOI] [PubMed] [Google Scholar]
- 3.Wright P J, English P J, Hungin A P S.et al Managing acute renal colic across the primary‐secondary care interface: a pathway of care based evidence and consensus. BMJ 20023251408–1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marston W A, Ahlquist R, Johnson G J.et al Misdiagnosis of ruptured abdominal aortic aneurysms. J Vasc Surg 19971617–22. [DOI] [PubMed] [Google Scholar]
- 5.Pomper S R, Fiorillo M A, Anderson C W.et al Hematuria associated with ruptured abdominal aortic aneursym. Internat Surg 199580261–263. [PubMed] [Google Scholar]
- 6.Eskelinen M, Ikomen J, Lipponen P. Usefulness of history taking, physical examination and diagnostic scoring in acute renal colic. Eur Urol 199834467–473. [DOI] [PubMed] [Google Scholar]
- 7.Kuhn M, Bonnin R L, Davey M J.et al Emergency department ultrasound scanning for abdominal aortic aneurysm: Accessible, accurate and advantageous. Ann Emerg Med 200036219–223. [DOI] [PubMed] [Google Scholar]
- 8.Henderson S O, Hoffner R J, Asabona J L.et al Bedside emergency department ultrasonography plus kidneys, ureters and bladder vs intravenouspyelography in the evaluation of suspected renal colic. Acad Emerg Med 19985666–671. [DOI] [PubMed] [Google Scholar]
- 9.Sheafor D H, Hertzberg B S, Freed K S.et al Nonenhanced helical CT and US in the emergency evaluation of patients with renal colic: prospective comparison. Radiology 2000217792–797. [DOI] [PubMed] [Google Scholar]
- 10.Sinclair D, Wilson S, Toi A.et al The evaluation of suspected renal colic: ultrasound scan vs excretory urography. Ann Emerg Med 198918556–559. [DOI] [PubMed] [Google Scholar]
- 11.Rosen C L, Brown D F, Sagarin MJ et a l. Ultrasonography by emergency physicians in patients with suspected renal colic. J Emerg Med 199816865–870. [DOI] [PubMed] [Google Scholar]
- 12.Mandavina D P. Ultrasound training for emergency physicians—a prospective study. Acad Emerg Med 200071008–1014. [DOI] [PubMed] [Google Scholar]
- 13.Rowland J L, Kuhn M, Bonnin R L.et al Accuracy of emergency department bedside ultrasonography. Emerg Med (Fremantle) 200113305–313. [DOI] [PubMed] [Google Scholar]