Abstract
Objectives
To determine the impact of reorganisation of an acute admissions process on numbers of people in the emergency department (ED) awaiting admission to a hospital bed in a major teaching hospital.
Methods
We studied all emergency medical patients admitted to St James' Hospital, Dublin, between 1 January 2002 and 31 December 2004. In 2002, patients were admitted to a variety of wards from the ED when a hospital bed became available. In 2003, two centrally located wards were reconfigured to function as an acute medical admissions unit (AMAU) (bed capacity 59), and all emergency patients were admitted directly to this unit from the ED (average 15 admissions per day). The maximum permitted length of stay on the AMAU was 5 days. We recorded the number of patients in the ED, who were awaiting the availability of a hospital bed, at 0700 and 1700 on the days of recording during the 36 month study period.
Results
The impact of the AMAU reduced overall hospital length of stay from 7 days in 2002 to 5 days in 2003 and 2004 (p<0.0001). The median number of patients waiting in the ED for a hospital bed reduced from 14 in 2002 to 9 in 2003 and 8 in 2004 (p<0.0001). While age and sex of patients did not differ over the years, the factors that independently contributed to the number of patients awaiting admission were the day of the week, the month of the year, and and the extent of the comorbidity index on the previous day's intake (p<0.0001).
Conclusions
This study found that reorganisation of a system for acute medical admissions can significantly impact on the number of patients awaiting admission to a hospital bed, and allow an ED to operate efficiently and at a level of risk acceptable to patients.
Keywords: emergency department, trolley wait times
Emergency department (ED) overcrowding is a worldwide problem that is important because it may decrease quality of patient care.1,2 It has been reported that inpatients who remain in the ED after admission have a longer average length of stay (LOS) in hospital than those who are promptly transferred to inpatient units.3 Moreover, qualitative patient satisfaction surveys have shown that patients are unhappy with the length of time they wait in the ED,4,5 and is the most frequent reason patients leave before medical evaluation.6,7 A relentless rise in emergency admissions in recent years has coincided with a reduction in hospital beds, resulting in severe problems in most acute hospitals.8,9,10 Having beds available when required is essential if an emergency admissions service is to operate efficiently and at a level of risk that is acceptable to patients. Moreover, it is recognised that an acute hospital can expect regular bed shortages for ED patients when hospital bed occupancy rates exceed 85%, and periodic bed crises if hospital bed occupancy rises to 90% or higher.11,12 As the demand for emergency medical services increases, overcrowded EDs are compelled to become more efficient at providing patient care. Given growing demands to maximise efficiency in acute hospital services, information on ED waiting times for a hospital bed is valuable, and a reduction in waiting times in the ED is an important government priority in England.13 Evidence suggests that with reorganisation it may be possible to improve patient care within existing resources.14
We have recently shown that the introduction of an acute medical admissions unit (AMAU) facilitated access to an acute medical service and reduced hospital costs by decreasing LOS.15 The aim of this study was to determine the impact of reorganisation of an acute admissions process on the number of patients awaiting admission to a hospital bed from the ED.
PATIENTS AND METHODS
Data relating to emergency medical patients admitted to St James' Hospital, Dublin, between 1 January 2002 and 31 December 2004 were recorded. The hospital, although a tertiary referral centre for various specialties, operates a daily sectored acute general medical intake, serving as a secondary care centre for emergency medical admissions for its local Dublin catchment area. In 2002, emergencies in acute medicine were initially assessed by the staff of the ED and referred by them to the on call medical team, consisting of a registrar and a senior house officer. All such patients identified as requiring hospitalisation, apart from cases admitted directly to the coronary care or intensive care units, were admitted to a variety of wards from a trolley in the ED, under the care of a named consultant physician, when a hospital bed became available. The on call roster is a 1:9 (that is, each team on call every ninth day) with two slots, each operated by teams from respiratory medicine and gastroenterology, one slot each contributed by specialty teams from diabetes/endocrinology, clinical pharmacology, and rheumatology, and one slot each contributed by two teams from general internal medicine (GIM).
In 2003, two of the modern centrally located wards, with close proximity to the ED and diagnostic imaging department, were reconfigured to function as an AMAU. A detailed operational plan for the unit was devised following extensive discussions with all interested parties in the year prior to its inception. Two GIM physicians, both of whom had prior experience in the operation of AMAUs in the UK, were recruited to act as medical and deputy directors of the unit, respectively. The nursing staff was recruited based on prior experience on acute medical units. Again, emergencies in acute medicine were initially assessed by the staff of the ED and referred by them to the on call AMAU team, consisting of a registrar and two senior house officers, whose sole responsibility was the acute intake. All such patients requiring hospitalisation were admitted directly to the AMAU from a trolley in the ED. The 59 bed capacity of the AMAU is sufficient that, with an average of 15 admissions each day, <70% of all admissions would be predicted to receive their entire hospital care within the unit (maximum permitted stay in AMAU is 5 days). Those patients requiring a longer stay were transferred from the AMAU to the appropriate specialty or general medical beds. In 2003 and 2004, the on call roster remained a 1:9, with each physician on call for 24 hours, and a post‐call ward round carried out each morning in the AMAU, with other fixed commitments cancelled to accommodate this. Radiology, endoscopy, laboratory services, physiotherapy, occupational therapy, and social services prioritised appropriate requests from the AMAU. All patients identified as suitable for fast track discharge had a provisional discharge date identified on the post‐call ward round. Medical teams reviewed these patients early on the morning of discharge, so that discharge could be confirmed and arrangements made to transfer the patient to the discharge lounge to free up beds for patients waiting on trolleys in the ED. The discharge manager's role was to help identify patients suitable for early discharge, and to work with the multidisciplinary team to ensure timeliness of discharge.
A patient database was acquired by linking the patient administration system (PAS) to the hospital in patient enquiry (HIPE) scheme. HIPE is a national database of coded discharge summaries from acute public hospitals in the Republic of Ireland. Sixty hospitals participate in the system and it is an invaluable source of hospital activity level and accreditation. Ireland has used the International Classification of Diseases, (ninth revision, clinical modification; ICD‐9‐CM) for both diagnosis and procedure coding since 1990, with updates every 5 years. Linking the HIPE dataset with the PAS dataset permits application of routinely collected data for the purposes of research, planning, and quality control. Data collected include hospital number, patient's name, date of birth, sex, area of residence by county, dates of admission and discharge, diagnosis (principal and up to nine additional secondary diagnoses), procedures (principal and up to nine additional secondary procedures), and consultant responsible for care. Separately logged were the patients in the ED accepted for medical admission but awaiting the availability of a bed in the AMAU; the numbers of such patients were recorded at 0700 and 1700 on the recording day between 2002 and 2004. Data collection techniques and criteria remained constant throughout the study period.
Statistical methods
Univariate analysis was employed to study the factors influencing waiting times at 0700 and 1700 for medical beds, including day of week, month of year, and team on call. The Charlson comorbidity method was used to compute a weighted index for each patient.16 A higher weighting score (based on 19 diagnostic categories) indicates more comorbid disease. The prior day index was calculated to assess whether intense intakes influenced waiting times on subsequent days. Log linear (Poisson) regression analysis was used to identify factors that may have influenced emergency waiting times between 2002 and 2004. Statistical significance was set at p<0.05. All analyses were performed using JMPin (version 5.1, SAS Institute Inc.) or Stata (version 7.0, Stata Corporation) statistical packages.
RESULTS
In total, 17 211 episodes were recorded among 11 928 patients admitted acutely via the ED in the 36 month study period (1 January 2002 to 31 December 2004). There was an overall increase of 4.4% (5476 to 5715 episodes) from 2002 to 2004 in acute medical episodes presenting to the hospital requiring emergency admission. The median age of admissions was 65.6 years (interquartile range (IQR) 44.5 to 77.5), and 10% of those admitted were older than 84 years. Male patients made up less than half (48.4%). The median LOS was 6 days (IQR 2 to 13). There were1485 episodes (8.4%) that had a LOS >30 days. Demographic characteristics for patients admitted between 2002 and 2004 were compared, considering each year separately. Sex (p = 0.068) and age (p = 0.83) did not differ between the years, whereas the Charlson case mix index was significantly lower in 2002 than in 2004 (p<0.0001).
Factors influencing ED waiting times at 0700 and 1700
The number of patients awaiting admission was essentially similar at 0700 and 1700 (table 1). Log linear regression analysis confirmed three factors as independently contributing to numbers of patients waiting; the day of week, the month of the year, and the extent of the comorbidity index on the previous intake. Compared with an arbitrary reference day (Sunday), the other weekdays showed an increased number of patients awaiting medical admission at 0700. The increase varied from as little as 9% on Saturday to 25% on Friday; there were larger increases between Monday and Thursday inclusive (between 52% and 79%). There was a significant monthly variation; compared with a peak in January there was a progressive month by month reduction to a nadir in August and September, with 50% reduction from January base numbers. The sum of the Charlson index had a significant impact, with increasing numbers waiting on the subsequent day, and a higher score (more comorbid disease) predicting longer ED waiting times. The consultant team did not significantly impact on numbers of patients waiting.
Table 1 Factors influencing number of patients awaiting admission at 0700 and 1700.
| Variable | 0700 | 1700 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rate ratio | SE | p | 95% CI | Rate ratio | SE | P | 95% CI | |||||||||
| Day | ||||||||||||||||
| 2 | 1.55 | 0.060 | <0.001 | 1.44 to 1.68 | 1.52 | 0.060 | 0.000 | 1.40 to 1.64 | ||||||||
| 3 | 1.86 | 0.069 | <0.001 | 1.73 to 2.0 | 1.79 | 0.069 | 0.000 | 1.65 to 1.93 | ||||||||
| 4 | 1.73 | 0.065 | <0.001 | 1.60,1.86 | 1.68 | 0.065 | 0.000 | 1.56 to 1.81 | ||||||||
| 5 | 1.56 | 0.060 | <0.001 | 1.45 to 1.69 | 1.54 | 0.060 | 0.000 | 1.43 to 1.66 | ||||||||
| 6 | 1.32 | 0.051 | <0.001 | 1.22 to 1.44 | 1.25 | 0.051 | 0.000 | 1.16 to 1.36 | ||||||||
| 7 | 1.11 | 0.046 | 0.011 | 1.03 to 1.21 | 1.09 | 0.046 | 0.033 | 1.01 to 1.19 | ||||||||
| Month | ||||||||||||||||
| 1 | 1.0 | 1.0 | ||||||||||||||
| 2 | 0.87 | 0.03 | <0.001 | 0.80 to 0.93 | 0.87 | 0.034 | 0.001 | 0.81 to 0.94 | ||||||||
| 3 | 0.75 | 0.030 | <0.001 | 0.70 to 0.81 | 0.76 | 0.030 | 0.000 | 0.70 to 0.82 | ||||||||
| 4 | 0.61 | 0.026 | <0.001 | 0.56 to 0.66 | 0.62 | 0.026 | 0.000 | 0.56 to 0.669 | ||||||||
| 5 | 0.64 | 0.027 | <0.001 | 0.59 to 0.70 | 0.65 | 0.027 | 0.000 | 0.60 to 0.70 | ||||||||
| 6 | 0.67 | 0.028 | <0.001 | 0.62 to 0.73 | 0.67 | 0.028 | 0.000 | 0.62 to 0.73 | ||||||||
| 7 | 0.52 | 0.023 | <0.001 | 0.48 to 0.57 | 0.53 | 0.023 | 0.000 | 0.48 to 0.57 | ||||||||
| 8 | 0.48 | 0.023 | <0.001 | 0.44 to 0.53 | 0.49 | 0.023 | 0.000 | 0.45 to 0.54 | ||||||||
| 9 | 0.48 | 0.022 | <0.001 | 0.44 to 0.52 | 0.48 | 0.022 | 0.000 | 0.44 to 0.53 | ||||||||
| 10 | 0.59 | 0.025 | <0.001 | 0.54 to 0.64 | 0.59 | 0.026 | 0.000 | 0.54 to 0.64 | ||||||||
| 11 | 1.07 | 0.043 | 0.101 | 0.99 to 1.16 | 1.06 | 0.044 | 0.134 | 0.98 to 1.154 | ||||||||
| 12 | 0.50 | 0.026 | <0.001 | 0.45 to 0.55 | 0.50 | 0.026 | 0.000 | 0.454 to 0.56 | ||||||||
| Sum CI* | 1.005 | 0.0020 | 0.002 | 1.002 to 1.008 | 1.01 | 0.0015 | 0.000 | 1.00 to 1.01 | ||||||||
| Consultant group | ||||||||||||||||
| 1 | 1.0 | 1.0 | ||||||||||||||
| 2 | 0.98 | 0.028 | 0.561 | 0.93 to 1.04 | 0.99 | 0.028 | 0.646 | 0.93 to 1.04 | ||||||||
| 3 | 1.03 | 0.027 | 0.270 | 0.978 to 1.08 | 1.03 | 0.027 | 0.266 | 0.978 to 1.08 | ||||||||
| 4 | 0.98 | 0.028 | 0.510 | 0.93 to 1.04 | 0.98 | 0.028 | 0.576 | 0.93 to 1.04 | ||||||||
| % >70* | 1.0 | 0.0007 | 0.654 | 0.998 to 1.001 | 0.82 | 0.101 | 0.114 | 0.65 to 1.05 | ||||||||
*Lag 1 day. CI, Charlson index.
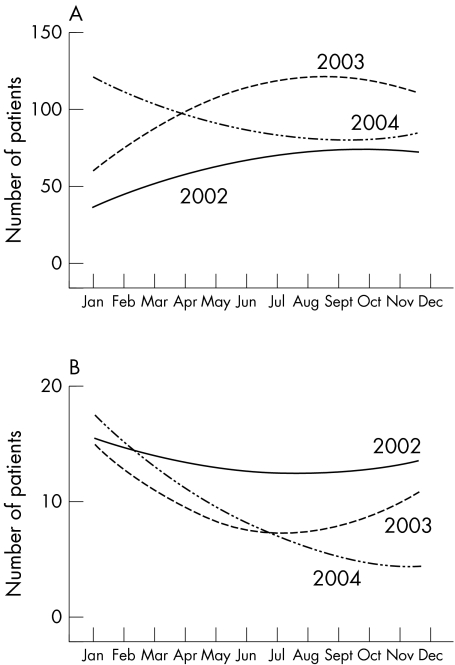
Delayed discharges (LOS >30 days) and ED waiting times
There are approximately 220 unprotected medical beds available in the hospital for the emergency intake function (fig 1). In 2002, a median of 65 (95% CI 52 to 80) were occupied by patients awaiting long term care (LTC); in 2003, this increased to 107 (93 to 124) with a slight but significant reduction by 2004 to a median of 91 (74 to 105). It can be calculated ,using a simple one compartment model, that an average intake of 15 patients with a median stay of 5 days' duration requires 124 beds at 100% occupancy or 138 beds at 90% occupancy. The impact of the AMAU reduced median LOS from 7 days (3 to 14) in 2002 to 5 days (2 to 11) in 2003 and 5 days (2 to 12) in 2004 (p<0.0001). The median number of patients waiting at 0700 in 2002 was 14 (8 to 19); this fell to 9 (4 to 13) in 2003 and 8 (3 to 14) in 2004 (p<0.0001). For the last 6 months of 2004, the numbers fell to a median of 4 (2 to 8).
Figure 1 (A) Long term care patients by year; (B) admission census of patients waiting admission by year.
Comparing the graphs of numbers of patients listed for LTC and occupying medical beds, it is evident that a relatively lower level of bed occupancy in 2002 was associated with a high level of ED waiting times. With the advent of the AMAU, there was an initial fall in numbers of ED waiting times in the first half of 2003; however, the simultaneous closure of public LTC beds in 2003 and abolition of contract beds in the private sector due to a funding crisis was associated with a rapid increase in LTC patients, with a peak of 128 acute medical beds occupied. In 2004, a substantial reduction of inappropriate bed occupancy (those patients listed for LTC and occupying acute medical beds) to a nadir of 75 allowed AMAU functionality to be re‐established, resulting a dramatic fall in ED waiting times.
DISCUSSION
We describe a novel approach to the management of ED patients awaiting admission following reorganisation of an acute admissions process. With the introduction of the AMAU in 2003, the average hospital LOS decreased from 7 days in 2002 to 5 days in 2003 and 2004. Despite an increase in acute medical episodes requiring emergency hospitalisation between 2002 and 2004, the number of patients awaiting admission for a hospital bed was significantly shorter in 2003 and 2004 after the introduction of the AMAU compared with 2002. While the age and sex of patients presenting to the ED did not differ over the years, the three factors that independently contributed to the number of patients awaiting admission were the day of the week, the month of the year, and the extent of the comorbidity index on the previous day's intake.
We linked the hospital PAS and HIPE data set to define a clinically useful database relating to emergency admissions. The Irish Department of Health uses HIPE data to measure and compare hospitals' performance. The case mix directly influences funding given to a hospital, with more efficient hospitals rewarded at the expense of the less efficient. Therefore, the quality of clinical coding is desirable to make such comparisons more meaningful and to provide a firm basis for both clinical and management decisions. In our study, we found that the HIPE database was very powerful in predicting the number of patients awaiting admission. We also used a validated method in adjusting for the differences in the number of patients awaiting admission related to the frequency of comorbid diseases,16 as the presence of comorbidity is significantly associated with longer LOS and hospital costs.17,18,19
Although the use of administrative data allowed us to study a large number of patients over a 3 year period, it also had several limitations. The principal limitation of this study was our inability to definitively specify cause and effect relationships between the reorganisation of an admissions process and the improvement in the number of patients awaiting admission. Although many of these relationships may seem intuitive, they were not conclusively proved. Secondly, our data captured the total number of ED patients waiting for a hospital bed at two specific time points only, 0700 and 1700, and may not be representative of what happens at other time points during a 24 hour period. Moreover, our definition captured the number of patients awaiting admission at these two time points, rather than the actual time that patients waited for a hospital bed. A final limitation worth mentioning regards external validity. We studied an ED in the Republic of Ireland, which possibly functions differently from those in the UK and elsewhere. While there have been numerous initiatives in the UK designed to cope with the increase in emergency hospital admissions,20,21,22,23 there have been no prior Irish studies. A study from Bournemouth showed that having senior leadership with an acute care physician in the AMAU at all times avoided unnecessary admissions.24 Furthermore, a study from Scotland found that following reorganisation of acute medical care with the establishment of a “physician of the week” approach in an AMAU, more patients were discharged early.25 In contrast to the above studies, our AMAU has some important differences in that it has a 59 bed capacity to cope with an average of 15 admissions per day, and patients are permitted to stay in the unit a maximum of 5 days. Different models will be appropriate for different hospitals, but this model has worked well for us.
A prior study of emergency admissions found that almost half of the acute in patient bed days were inappropriate for acute care.26 Importantly, if discharge decisions are made during the consultant's ward round, then the frequency of these ward rounds can influence LOS.27 Better organisation of discharge policy over the weekend has also been identified as a factor that can contribute to reductions in LOS.28 However, like others, we have found that one of the main contributors towards prolonged LOS is discharge delay pending placement of the patient into residential care or the initiation of community support services.29 In one region of England, it was found that LOS increased with declining socioeconomic status after controlling for level of bed provision.30 Moreover, we have recently shown that a useful patient characteristic for predicting LOS is patient age;31 presumably this reflects greater need for pre‐discharge social care planning.
Effective and appropriate bed usage is one of the essential elements in efficient care and management of ED patients. Juggling the demands for beds against supply is problematic in the medical specialties, because the major component of the workload arises from emergency admissions; for the Republic of Ireland, 84% of all medical inpatients are admitted as emergencies. As the demand for emergency medical services increases, AMAUs provide a focus of clinical care for medical staff rather than having patients spread across several different wards, and facilitate an efficient high quality emergency admissions process with a view to a shorter LOS.15,16,17,18,19,26,27,28,29,30,31,32 The factors felt to be important in the success of the AMAU in our study were: (a) planning from the very early stages by a group including all clinicians involved in acute intake and senior members of the management team; (b) a willingness by clinicians to accept that reorganisation would involve a change in working practices, including cancellation of other fixed commitments while on call, and a post‐intake ward round carried out at least once every 24 hours; (c) a willingness by management to accept that some extra resources would be required (in particular, the appointment of a discharge planning coordinator, physiotherapist, occupational therapist, social worker, and clerical support in the AMAU was seen as vital); (d) the cooperation of colleagues in other specialties, such as radiology, endoscopy, and laboratory services, to provide fast track services; and (e) the appointment of ward managers committed to making the culture change of the new system work. Importantly, no changes occurred external to the AMAU at this time, either in the hospital or the health system, that may have influenced any changes observed.
Over the past 20 years, the average LOS for hospital admissions in the Republic of Ireland as a whole has fallen from 9.7 days in 1980 to 6.6 days in 2000.31 Factors contributing to a shorter LOS include an increased use of day case capacity and the recognition that earlier discharge is possible for many patients without having an adverse effect on clinical outcomes. As LOS reduces, scrutiny and monitoring of re‐admissions are increasingly relevant, particularly with the growing number of elderly patients requiring acute emergency care. While we did not examine re‐admission rates in our study, we have previously reported that many re‐admissions to hospital may not be preventable, representing fresh events in patients with chronic illnesses and frequent comorbidity.33
Having beds available when required is essential if an ED is to operate efficiently and at a level of risk that is acceptable to patients. Our experience suggests that reorganisation of a system for acute general medical admissions in the Republic of Ireland can significantly impact on the number of patients awaiting admission. In the current social, political, and economic environment of limited resources for healthcare, the importance of efficiency in the ED is to allow limited resources to be used most efficiently towards improving the quality of care that is rendered. Moreover, a direction for further research to adequately assess ED efficiency and quality, would be to evaluate measures for use of emergency care, impact of care, identification of at risk groups, patient satisfaction, quality of life, and cost effectiveness.
Abbreviations
AMAU - acute medical admissions unit
ED - emergency department
GIM - general internal medicine
HIPE - hospital in patient enquiry
LOS - length of stay
LTC - long term care
PAS - patient administration system
Footnotes
Competing interests: none declared
References
- 1.Miro O, Antonio M T, Jimenez S.et al Decreased health care quality associated with emergency department overcrowding. Eur J Emerg Med 19996105–107. [DOI] [PubMed] [Google Scholar]
- 2.Andrulis D P, Kellerman A, Hintz E A.et al Emergency departments and crowding in United States teaching hospitals. Ann Emerg Med 199120980–986. [DOI] [PubMed] [Google Scholar]
- 3.Krochmal P, Riley T A. Increased health care costs associated with ED overcrowding. Am J Emerg Med 199412265–266. [DOI] [PubMed] [Google Scholar]
- 4.Goldwag R, Berg A, Yuval D.et al Predictors of patient dissatisfaction with emergency care. Isr Med Assoc J 20024603–606. [PubMed] [Google Scholar]
- 5.Cross E, Goodacre S, O'Cathain A.et al Rationing in the emergency department: the good, the bad, and the unacceptable. Emerg Med J 200522171–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weissberg M P, Heitner M, Lowenstein S R.et al Patients who leave without being seen. Ann Emerg Med 198615813–817. [DOI] [PubMed] [Google Scholar]
- 7.Fernandes C M, Daya M R, Barry S.et al Emergency department patients who leave without seeing a physician: The Toronto Hospital experience. Ann Emerg Med 1994241092–1096. [DOI] [PubMed] [Google Scholar]
- 8.Capewell S. The continuing rise in emergency admissions. BMJ 1996312991–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kendrick S. The pattern of increase in emergency hospital admissions in Scotland. Health Bull 199654169–183. [PubMed] [Google Scholar]
- 10.Blatchford O, Capewell S. Emergency medical admissions: taking stock and planning for winter. BMJ 19973151322–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bagust A, Place M, Posnett J W. Dynamics of bed use in accommodating emergency admissions: stochastic simulation model. BMJ 1999319155–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cooke M. Whole system is responsible for solving overcrowding of departments. BMJ 2002325389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Audit Commission Acute hospital portfolio: accident and emergency. London: The Audit Commission, 2001
- 14.The Audit Commission Lying in wait: the use of medical beds in acute hospitals. London: Honeypress Ltd, 1992
- 15.Moloney E D, Smith D, Bennett K.et al Impact of an acute medical admission unit on length of hospital stay, and emergency department wait times. QJM 200598283–289. [DOI] [PubMed] [Google Scholar]
- 16.Charlson M E, Pompei P, Ales K L.et al A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 198740373–383. [DOI] [PubMed] [Google Scholar]
- 17.Gross P A, Cataruozolo P, DeMauro P.et al Severity adjustment for length of stay: is it always necessary? Clin Perform Qual Health Care 19975169–172. [PubMed] [Google Scholar]
- 18.Ishizaki T, Imanaka Y, Oh E.et al Association of hospital resource use with comorbidity status and patient age among hip fracture patients in Japan. Health Policy 200469179–187. [DOI] [PubMed] [Google Scholar]
- 19.Kinnunen T, Saynajakangas O, Tuuponen T.et al Impact of comorbidities on the duration of COPD patients' hospital episodes. Respir Med 200397143–146. [DOI] [PubMed] [Google Scholar]
- 20.Council of International Hospitals Confronting the challenge: seven tactics for managing the rise in emergency admissions. London: Council of International Hospitals, 1996
- 21.Scottish Intercollegiate Working Party Acute medical admissions and the future of general medicine. Edinburgh: RCP, 1998
- 22.Dorward A J. Patterns of acute medical receiving in Scotland. Health Bull 199755162–166. [PubMed] [Google Scholar]
- 23.NCCSDO Reducing attendances and waits in emergency departments. A systematic review of present innovations. 2005. www.sdo.lshtm.ac.uk/pdf/evalmodels_cooke_final.pdf
- 24.Armitage M, Raza T. A consultant physician in acute medicine: the Bournemouth model for managing increasing numbers of medical emergency admissions. Clin Med JRCPL 20022331–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanlon P, Beck S, Robertson G.et al Coping with the inexorable rise in medical admissions: evaluating a radical reorganisation of acute medical care in a Scottish district general hospital. Health Bulletin 199755176–184. [PubMed] [Google Scholar]
- 26.Armstrong S H, Peden N R, Nimmo S.et al Appropriateness of bed usage for inpatients admitted as emergencies to internal medicine services. Health Bull 200159388–395. [PubMed] [Google Scholar]
- 27. Griffiths M, Water WE, Acheson , eds. Variation in hospital stay after inguinal herniorrhaphy. BMJ 19791787–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmidt W P, Taeger D, Buecker‐Nott H J.et al The impact of the day of the week and month of admission on the length of hospital stay in stroke patients. Cerebrovasc Dis 200316247–252. [DOI] [PubMed] [Google Scholar]
- 29.Black D, Pearson M. Average length of stay, delayed discharge and hospital congestion. BMJ 2002325610–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.NETRHA Patient census study: social factors analysis. North East Thames Regional Health Authority, Management Services Report no.1249, 1983
- 31.Moloney E D, Bennett K, Silke B. Length of hospital stay, diagnoses and pattern of investigation following emergency admission to an Irish Teaching Hospital. Ir Med J 200497170–172. [PubMed] [Google Scholar]
- 32.McLaren E H, Summerhill L E, Miller W J.et al Reorganising emergency medical admitting: the Stobhill experience, 1992–1997. Health Bull 199957108–117. [PubMed] [Google Scholar]
- 33.Moloney E D, Bennett K, Silke B. Patient and disease profile of emergency medical readmissions to an Irish Teaching Hospital. Postgrad Med J 200480470–474. [DOI] [PMC free article] [PubMed] [Google Scholar]