Abstract
Objective
To examine changes in the rate of seeing patients between 1990 and 2004 and to see whether performance might be related to patient age, using data held on the patient administration system.
Method
Data collected in 1990 were compared with those collected in 2004. Age related data were examined for the following parameters: the number of patients arriving by ambulance; the time taken to process the attendance; the number of investigations; the number of emergency admissions; and the length of inpatient stay.
Results
Emergency department (ED) performance has fallen markedly since 1990. Between 1990 and 2004, there was a 54% increase in total patients with a disproportionate 198% increase in patients aged more than 70 years, including a 671% increase in those aged more than 90 years. The time taken to manage patients increased with age. In 2004, there was a marked rise in investigation rates, and the probability of having investigations increased with age. In 2004, older patients (aged more than 70 years) were 4.9 times more likely to require admission to hospital than younger patients (aged 30 years or less). Their average length of stay was 6.9 times longer. Younger patients were 3.3 times more numerous than older patients but older patients occupied 9.8 times more emergency bed days.
Conclusions
Pressure on emergency care is associated with a disproportionate increase in the number of elderly patients and with an increased tendency to investigate them. Population ageing is of central importance in planning health services.
Keywords: population ageing, emergency department efficiency
Publications from emergency departments (EDs) around the world have drawn attention to patient overcrowding and bed shortages. Specifically, there have been reports from developed countries such as the USA,1,2,3,4 Australia,5,6,7 New Zealand,8 and Canada.9,10,11 Until recently, overcrowding in EDs was a major problem in the UK too.12,13 Bed shortages have been cited as an important cause of congestion, implying that a large number of patients in the log‐jam have required admission.1,2,3,5,6,7,8,10 Although it is acknowledged that there are many interrelated factors which could be responsible, we thought that an important underlying cause might be an ageing population in these locations. In 1996, a disproportionate increase in attendances by elderly patients was reported from Leeds.14 Furthermore, elderly people (aged more than 70 years) had a fivefold higher rate of admission than patients aged less than 30 years. The authors alerted readers to the need to cater for this trend. A fivefold higher rate of hospital emergency admissions among elderly people has also been reported from the USA.15
Older people generally have more complex problems requiring more investigations, admissions, and critical care15; they require more assistance while in the department; and safe discharge to the community may be difficult to manage. It is also worth noting that patients from residential homes, many of whom are highly dependent and have considerable comorbidities, seem increasingly to be sent to EDs; this group of patients has been the subject of a study in Australia.16 Thus, we examined our own database to see whether we could distinguish trends which would support the hypothesis that overcrowding might be related to an ageing population. Our department is set in a small district general hospital in the South Midlands, UK.
Methods
Data collection and retrieval
Since June 1989, data for each attendance have been collected on the accident and emergency (A&E) module of the patient administration system (PAS). We used standard enquiry packages and ad hoc enquiries to retrieve data. The A&E standard enquiry packages retrieve data on total attendances and therefore all our data refer to the total number of attendances. It was thought that changes in the age of our catchment population and/or changes in referral patterns were likely to have been gradual. Therefore, for most of the analyses we have used only two time points and we have compared data collected for our first complete Korner year (1990) with the most recent complete Korner year (2004).
Performance profile
We constructed a “performance profile”, using annual data on patients of all ages from 1990 to 2004. We obtained total attendance figures from the PAS database and we used the PAS standard enquiry package “EPTD” to measure the percentage of patients who completed their attendance (from registration to discharge—designated “time in department”) within two hours. The two hour figure was chosen because it is a more stringent and therefore more sensitive test of performance than the government's current four hour target. It is not subject to “target pressures” (for example, moving patients to an observation area at four hours). This statistic had been used previously in departmental annual returns for the Oxford Deanery.
Age banding
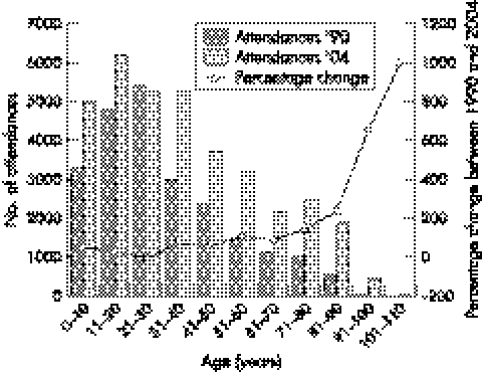
In subsequent analyses, data were banded for each decade of life to examine age related effects on performance. For these analyses, we exclusively compared the data from 1990 with those from 2004. Banded data (presented in fig 1 and tables 1–5) have been summarised in the text by pooling the results for patients aged 30 years or less, and by pooling the results for patients aged more than 70 years. We did this to facilitate comparisons with other publications.
Figure 1 The number of patients in each decade of life who attended the emergency department in 1990 is compared with the number of patients in each decade of life who attended the emergency department in 2004. The percentage change in attendances between 1990 and 2004 is plotted for each decade of life.
Table 1 Total number of attendances within each decade of life and the proportion of those patients who arrived by ambulance for 1990 and 2004.
| Age (years) | Attendances | Arrived by ambulance | ||
|---|---|---|---|---|
| 1990 | 2004 | 1990 | 2004 | |
| 0–10 | 3293 | 5005 | 0.053 | 0.076 |
| 11–20 | 4799 | 6205 | 0.097 | 0.117 |
| 21–30 | 5402 | 5230 | 0.110 | 0.141 |
| 31–40 | 2987 | 5261 | 0.127 | 0.149 |
| 41–50 | 2363 | 3715 | 0.137 | 0.181 |
| 51–60 | 1490 | 3181 | 0.197 | 0.206 |
| 61–70 | 1139 | 2163 | 0.320 | 0.323 |
| 71–80 | 1003 | 2458 | 0.478 | 0.513 |
| 81–90 | 562 | 1901 | 0.683 | 0.682 |
| 91–100 | 63 | 479 | 0.841 | 0.825 |
| 101–110 | 2 | 22 | 0.500 | 0.955 |
Table 2 Values for 1990 and 2004 are shown for the following parameters for each decade of life: the number of patients who did not wait to be seen (DNW); the number of patients who did wait (obtained by subtracting columns 2 and 3 of this table from columns 2 and 3 of table 1); and the proportion of the patients who did wait and who were diagnosed and treated in less than one hour (D&T<1 h).
| Age (years) | DNW | Waited | D&T<1 h | |||
|---|---|---|---|---|---|---|
| 1990 | 2004 | 1990 | 2004 | 1990 | 2004 | |
| 0–10 | 57 | 190 | 3236 | 4815 | 0.768 | 0.679 |
| 11–20 | 95 | 289 | 4704 | 5916 | 0.740 | 0.635 |
| 21–30 | 148 | 283 | 5254 | 4947 | 0.742 | 0.599 |
| 31–40 | 48 | 301 | 2939 | 4960 | 0.730 | 0.574 |
| 41–50 | 64 | 198 | 2299 | 3517 | 0.720 | 0.541 |
| 51–60 | 27 | 122 | 1463 | 3059 | 0.651 | 0.488 |
| 61–70 | 11 | 96 | 1128 | 2067 | 0.620 | 0.392 |
| 71–80 | 15 | 60 | 988 | 2398 | 0.503 | 0.285 |
| 81–90 | 3 | 38 | 559 | 1863 | 0.410 | 0.205 |
| 91–100 | 0 | 12 | 63 | 467 | 0.333 | 0.169 |
| 101–110 | 0 | 0 | 2 | 22 | 0.500 | 0.182 |
Table 3 Estimated probabilities of “time to diagnose and treat”, investigations and admissions among patients aged 30 years or less and patients aged over 70 years in 1990 and 2004.
| Event | Year | Probability (95% CI) | |
|---|---|---|---|
| Event | age ⩽30 years | Event | age >70 years | ||
| D&T<1 h | 1990 | 0.748 (0.740 to 0.755) | 0.464 (0.439 to 0.489) |
| D&T<1 h | 2004 | 0.637 (0.630 to 0.645) | 0.247 (0.235 to 0.260) |
| Full blood count | 1990 | 0.019 (0.017 to 0.022) | 0.199 (0.180 to 0.219) |
| Full blood count | 2004 | 0.114 (0.109 to 0.119) | 0.616 (0.602 to 0.629) |
| Electrocardiograph | 1990 | 0.003 (0.002 to 0.004) | 0.225 (0.205 to 0.246) |
| Electrocardiograph | 2004 | 0.034 (0.031 to 0.036) | 0.475 (0.461 to 0.489) |
| X ray | 1990 | 0.286 (0.278 to 0.294) | 0.453 (0.429 to 0.478) |
| X ray | 2004 | 0.385 (0.377 to 0.392) | 0.606 (0.592 to 0.620) |
| Admission | 1990 | 0.081 (0.076 to 0.085) | 0.459 (0.435 to 0.483) |
| Admission | 2004 | 0.127 (0.122 to 0.132) | 0.602 (0.588 to 0.616) |
Notice that for each event, the difference between the probabilities for each age group increases from 1990 to 2004—there is a widening gap.
Table 4 Values for 1990 and 2004 are shown for the proportion of patients having full blood counts, electrocardiographs, and x rays with respect to total attendances in each age band (see table 1).
| Age (years) | Full blood counts | Electrocardiograph | X rays | |||
|---|---|---|---|---|---|---|
| 1990 | 2004 | 1990 | 2004 | 1990 | 2004 | |
| 1–10 | 0.011 | 0.031 | 0.001 | 0.004 | 0.267 | 0.291 |
| 11–20 | 0.017 | 0.112 | 0.005 | 0.028 | 0.328 | 0.470 |
| 21–30 | 0.026 | 0.195 | 0.001 | 0.068 | 0.260 | 0.373 |
| 31–40 | 0.040 | 0.231 | 0.026 | 0.097 | 0.282 | 0.382 |
| 41–50 | 0.043 | 0.262 | 0.043 | 0.136 | 0.282 | 0.412 |
| 51–60 | 0.081 | 0.345 | 0.087 | 0.215 | 0.322 | 0.460 |
| 61–70 | 0.144 | 0.457 | 0.160 | 0.331 | 0.368 | 0.503 |
| 71–80 | 0.190 | 0.593 | 0.219 | 0.439 | 0.434 | 0.570 |
| 81–90 | 0.210 | 0.636 | 0.237 | 0.501 | 0.473 | 0.635 |
| 91–100 | 0.238 | 0.656 | 0.206 | 0.549 | 0.587 | 0.672 |
| 101–110 | 0.000 | 0.500 | 0.000 | 0.500 | 0.500 | 0.727 |
Table 5 The proportions of the total number of patients in each age band (see table 1) who were admitted in 1990 and 2004.
| Age (years) | Admitted | Average length of stay in days (2004) | Total bed occupancy in days (2004) | |
|---|---|---|---|---|
| 1990 | 2004 | |||
| 0–10 | 0.095 | 0.140 | 1.3 | 862 |
| 11–20 | 0.076 | 0.106 | 1.8 | 1078 |
| 21–30 | 0.076 | 0.138 | 2.4 | 1579 |
| 31–40 | 0.093 | 0.174 | 2.4 | 1992 |
| 41–50 | 0.108 | 0.205 | 3.5 | 2394 |
| 51–60 | 0.168 | 0.287 | 4.5 | 3762 |
| 61–70 | 0.264 | 0.418 | 6.4 | 5325 |
| 71–80 | 0.425 | 0.560 | 9.8 | 12 720 |
| 81–90 | 0.514 | 0.632 | 14.2 | 16 216 |
| 91–100 | 0.524 | 0.700 | 16.8 | 5258 |
| 101–110 | 0.000 | 0.632 | 10.4 | 124 |
The data for average length of stay and total bed occupancy were available for 2004 only.
Time to diagnose and treat
To obtain an estimate of the time needed to actually manage patients, we subtracted the initial waiting time (the time between registration and first contact with a doctor or emergency nurse practitioner) from the total time in department in the ad hoc analyses. We designated the time elapsed between the first contact with a doctor or emergency nurse practitioner and the discharge or admission time as “time needed to diagnose and treat”. For each age band, we calculated the proportion of patients who were “diagnosed and treated” within one hour. (We have not counted patients who did not wait to be seen or who left before treatment.) We chose to examine a one hour period for this parameter because it is close to the median time in 2004, and thus produces percentages close to 50% (that is, it is close to the mid point on the scale and it is precisely half the two hour period that we used as a reference for the total “time in department”).
Indicators of case‐mix
We used the proportion of patients who arrived by ambulance, the proportion who had investigations, and the proportion who were admitted, as surrogate indicators of case‐mix, clinical complexity, and dependency. We reasoned that patients who require ambulance transport, investigations, and admission to hospital are likely to consume more resources and take longer to process. (These analyses are not corrected for patients who left before treatment, some of whom arrived by ambulance and/or were investigated.) Bed shortages have been cited as an important cause of emergency department congestion2,3,5,6,7,8,10 and we therefore examined the relation between patient age and length of stay for ED patients admitted to a hospital bed.
Confidence limits
We calculated 95% confidence intervals for estimated probabilities of events by assuming a binomial distribution for the number of occurrences of the event in a given number of trials; the limits are those for two 2.5% tails. Differences are significant when the confidence levels do not overlap.
Age adjusted data
We used age adjusted data to distinguish the effect of age on our performance from other factors such as changes in the tendency to investigate patients. We did this by calculating what the number of patients would have been in each age band in 2004 if the age distribution (proportion of patients in each age band) had been that of 1990 but the distribution of the other factors had been that of 2004.
Detailed method for age adjustment
We obtained confidence limits for the age adjusted estimate of the probability of an event by assuming a beta distribution for the unknown conditional probability of the event for each age band in 2004. We parameterised the distribution with the number of patients and the observed frequency of the event. We then scaled the probability density function by the number of patients in the particular age band in 1990. We then calculated the mean and variance of the frequency of the event that would have been expected to have been observed in that age band in 2004 had the number of patients been that of 1990. We then summed these two parameters for all 11 age bands and divided by the total number of attendances in 1990. We thus obtained an age adjusted mean and variance of the estimated relative frequency of the event. The 95% confidence limits were computed as mean±1.96 standard error (SE).
Results
Relation between annual attendances and performance: the performance profile
There has been an approximately linear increase in attendances between 1990 (21 712 attendances) and 2004 (35 640 attendances). In 1990, the percentage of patients whose total “time in department” was less than two hours was 82.8%. Thereafter, there was a decline in performance until 2000 when only 41.1% of patients completed their attendance within two hours. Between 2000 and 2004, when resources were being invested in the government's four hour target, there was a progressive and striking improvement in performance, such that 53.2% of patients in 2004 completed their attendance within two hours. However, we were unable to return to the level of performance achieved in 1990.
Medical and nursing staff levels
Medical staffing levels in 2004 were better than in 1990 when the average caseload for each service‐equivalent doctor was 4820 patients per annum; in 2004, the average annual caseload was 3938 patients. In 1990, there were 1294 patients for each whole‐time‐equivalent trained nurse whereas in 2004 there were 1234.
Changes in age distribution between 1990 and 2004
The failure to attain the level of performance achieved in the early 1990s was difficult to explain in view of improvements made in process and medical staffing. It was therefore thought that the type of patients seen might have changed. Patient age distribution was examined in 1990 and 2004 (fig 1). There has been a remarkable shift to the right between 1990 and 2004, such that the median age has increased by 10 years. The increase in total caseload between 1990 and 2004 was 54% but in 2004 the proportion of patients aged more than 70 years was 198% higher than in 1990. Furthermore, the proportion of patients aged more than 90 years was 671% higher. Despite this dramatic increase in number, elderly patients still comprised a comparatively small group (4860 aged more than 70 years compared with 16 441 aged 30 years or less in 2004).
Relation between age and mode of arrival
Table 1 shows the number of attendances for each decade of life in 1990 and in 2004 together with the corresponding proportions of these patients who arrived by ambulance. Patients seen in 2004 were more likely to have arrived by ambulance than in 1990 (probability 0.214 (CI 0.210 to 0.218) compared with 0.152 (CI 0.147 to 0.156)). Furthermore, the proportion of patients who use ambulance transport increases with increasing age. Age adjusted data show that had the age distribution been that of 1990 but the probability of arriving by ambulance within each decade of life been that of 2004, the net probability would have been 0.176 (CI 0.172 to 0.180). This implies that increasing age accounts for about 61% (≡ (0.214–0.176)/(0.214–0.152)) of the increase in ambulance usage seen in 2004.
Relation between age and “time to diagnose and treat”
In 1990, the median time needed to diagnose and treat was 29 minutes whereas in 2004 it was 50 minutes. Table 2 shows the proportions of patients diagnosed and treated within one hour in each decade of life, both in 1990 and 2004. In both 1990 and 2004, there was a progressive decline in performance with increasing age. However, this decline was much steeper in 2004 than in 1990—there was a significant, age related “widening gap” (see table 3).
In 1990 the probability of a patient being diagnosed and treated within one hour was 0.710 (CI 0.704 to 0.716) whereas in 2004 it was 0.535 (CI 0.529 to 0.540). Had the age distribution been that of 1990 but the probability within each decade of life been that of 2004, the overall probability would have been 0.567 (CI 0.561 to 0.572). This implies that increasing age per se accounts for about 18% of the reduction in performance between 1990 and 2004. The age related widening gap, however, suggest that in 2004 other factor(s) were amplifying the effect of increasing age on performance.
Relation between age and the number of investigations
We looked at the number of investigations because it was judged that these would be surrogate indicators both of clinical complexity and the time needed to process the attendance. Furthermore, a change in the tendency to investigate patients might explain the widening gap. Table 4 shows the proportion of patients having full blood counts (FBCs), electrocardiographs (ECGs), and x rays for each decade of life in 1990 and 2004.
Patients seen in 2004 were more likely to have FBCs (probability 0.257 (CI 0.252 to 0.261) compared with 0.047 (CI 0.044 to 0.050) in 1990), more likely to have ECGs (probability 0.148 (CI 0.144 to 0.152) compared with 0.039 (CI 0.036 to 0.041)), and were more likely to have x rays (probability 0.431 (CI 0.426 to 0.436) compared with 0.303 (CI 0.297 to 0.309)) than in 1990. Combined, age adjusted data show that had the age distribution been that of 1990 but the probability within each decade of life been that of 2004, the probability of an FBC would have been 0.218 (CI 0.214 to 0.222), the probability of an ECG would have been 0.112 (CI 0.109 to 0.115), and the probability of an x ray would have been 0.414 (CI 0.409 to 0.420). This implies that increasing age accounts for about 18%, 33%, and 13% of the increase between 1990 and 2004 in the proportion of patients having FBCs, ECGs, and x rays, respectively. We again found an age related widening gap with respect to investigation rates in 2004 (table 3).
Relation between age and rate of admission to a hospital bed
We examined the proportion of patients admitted to hospital for each decade of life in 1990 and 2004 (table 5).
The proportion of patients admitted to hospital was consistently higher in 2004 than in 1990 for every decade of life. In both 1990 and 2004, older patients were more likely to be admitted than younger patients and there was a widening gap in the tendency to admit elderly patients since 1990 (table 3).
Relation between age and length of stay in a hospital bed
An analysis of the length of stay shows (as expected) that elderly patients spent longer in hospital (table 5). In 2004, 1920 patients aged 30 years or less required an emergency admission and they occupied 3519 bed days (average length of stay 1.8 days). Over the same period of time, 2765 patients aged 70 years or more were admitted and they occupied a total of 34 318 bed days (average length of stay 12.4 days). Thus, patients aged 70 years and over occupied 9.8 times more emergency bed days than patients aged 30 years or less. Indeed, the 325 patients admitted to hospital aged more than 90 years occupied 1.6 times more bed days than the 1920 patients admitted to hospital aged 30 years or less (table 5).
Discussion
When we examined patient age as a possible cause of declining performance in 2004 compared with 1990, we found there had been dramatic increases in attendances among older people. These people formed a numerically small group (4860 aged more than 70 years compared with 16 440 aged less than 30 years in 2004) but our data show that these patients took longer to manage, they required more investigations, they were more likely to need admission, and they had a longer length of stay. Our results, which showed an approximate fivefold increase in emergency admissions among patients aged more than 70 years compared with patients aged 30 years or less, are comparable with those reported from Leeds in 199614 and from the USA in 1992.15 This suggests that a fivefold, age related difference might be found elsewhere.
Bed shortages are an important cause of emergency department congestion2,3,5,6,7,8,10 and our results show that not only are elderly people more often admitted but their length of stay and bed occupancy are much higher than those of younger patients. It thus becomes apparent that quite small increases in the number of elderly patients who attend our emergency departments can have a dramatic effect on efficiency and on the functioning of the whole hospital. It is therefore of vital importance to make provision for older people and to plan for future trends.
More patients came to hospital by ambulance in 2004 than in 1990 and 61% of this increase is due to population ageing. The remaining small increase could have been caused by an increased acuity in case‐mix and/or by changes in the threshold for calling an ambulance. Changes in the delivery of primary care might also have affected ambulance usage. We noted a considerable increase both in the number of investigations performed and in the rate of admission between 1990 and 2004. These changes might likewise be related to an increased acuity in case‐mix and/or to changes in threshold for investigation and admission. The increased rate of investigation and admission can be expected to have increased the time needed to process attendances and thus to contribute to ED congestion. In both 1990 and 2004, older patients were more often investigated and admitted than younger patients. Furthermore, in 2004, we noted an age related escalation in the number of investigations and admissions (the widening gap) and this can be expected to have amplified the effect of ageing on the time needed to process attendances.
We present this as an observational study and cannot determine the exact reasons for the changes in practice over the past 14 years. However, it is our impression that the threshold for investigations has reduced over time, a phenomenon which has been noted in the USA and attributed to “advancing technology” and “escalating standards of care”.3 A growing number of patients with chronic disease might also have contributed to the increased number of investigations and admissions. It is worth noting that an increasing rate of admission over time (1990–94) has been reported from Leeds.14 Therefore, this phenomenon might be part of a national trend. Whatever the mechanism(s) for the changes in our workload and practice, the observation stands that we are now seeing more elderly patients and they take quantifiably longer to manage, and they require more investigations and more admissions than younger patients.
Measures taken in support of the government's four hour targets (increase in numbers of medical and nursing staff since 2000, modernisation of the department, nurse‐requested investigations, management of the “back door”, opening of a medical assessment unit) were impressive but not sufficient to return performance to the level seen in 1990. We attribute this to population ageing and to higher standards of care since 1990.
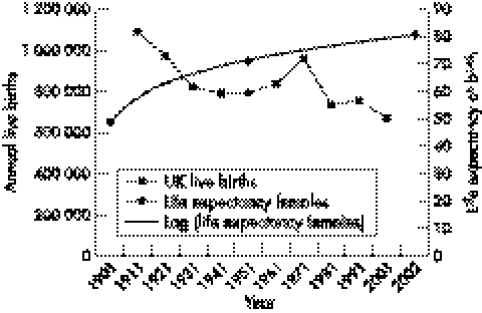
We believe that the needs of older people are of central importance in planning emergency health care in the UK and in other developed countries. In the UK, increasing life expectancy and a declining birthrate have caused the population to age (fig 2). This effect is likely to become far more pronounced as people born in the 1960s' “baby boom” begin to enter old age. The currently falling birthrate means that there will be a declining population of young adults in the UK able to care for the elderly population and to support them economically. Better services for older people might include a domiciliary geratology service—available, in particular, for patients in residential and nursing homes; the provision of community nurses specialising in geratology and chronic disease; training for all primary care physicians in geratology; more community beds for elderly patients; more rapid‐access geratology and falls clinics; geratology assessment units with links to acute services, occupational therapy, and social care; and better management of “exit block”.
Figure 2 The changing birthrate and life expectancy in the UK. Average annual UK live births for each decade obtained from www.optimumpopulation.org and female life expectancy in years obtained from www.statistics.gov.uk. Increasing life expectancy and a declining birthrate have caused the population to age. This effect is likely to become much more extreme as those born in the 1960s' “baby boom” begin to enter old age.
Conclusions
In the UK, EDs and their patients have experienced major difficulties in terms of overcrowding during much of the past decade. We believe that this has been caused both by changes in practice (for example, increased investigation and admission) and by ageing of the population using EDs. We expect the difficulties in relation to an ageing population to intensify appreciably during the first half of the twenty first century. This must be anticipated and effective plans prepared.
Acknowledgements
We would like to thank Carol Mortimer (librarian) for supplying copies of the references. We would also like to thank the referees for their helpful and constructive suggestions for improving the presentation of the paper.
Authors' contributions
G George and B Todd wrote the paper. C Jell (Senior Information Analyst) supplied the data and B Todd led on data presentation and interpretation.
Abbreviations
ED - emergency department
PAS - patient administration system
Footnotes
Competing interests: none declared
References
- 1.Trzeciak S, Rivers E P. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J 200320402–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Derlet R W, Richards J R. Emergency department overcrowding in Florida, New York, and Texas. South Med J 200295846–849. [PubMed] [Google Scholar]
- 3.Derlet R W, Richards J R. Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med 20003563–68. [DOI] [PubMed] [Google Scholar]
- 4.Schneider S, Zwemer F, Doniger A.et al Rochester, New York: a decade of emergency department overcrowding. Acad Emerg Med 200181044–1050. [DOI] [PubMed] [Google Scholar]
- 5.Fatovich D M, Hirsch R L. Entry overload, emergency department overcrowding, and ambulance bypass. Emerg Med J 200320406–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fatovich D M, Nagree Y, Sprivulis P. Access block causes emergency department overcrowding and ambulance diversion in Perth, Western Australia. Emerg Med J 200522351–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunn R. Reduced access block causes shorter emergency department waiting times: An historical control observational study. Emerg Med (Fremantle) 200315232–238. [DOI] [PubMed] [Google Scholar]
- 8.Ardagh M, Richardson S. Emergency department overcrowding—can we fix it? N Z Med J 2004117U774. [PubMed] [Google Scholar]
- 9.Kollek D. Emergency department overcrowding. Can Med Assoc J 2002167626–627. [PMC free article] [PubMed] [Google Scholar]
- 10.Upfold J. Emergency department overcrowding: ambulance diversion and the duty to care. Can Med Assoc J 2002166445–446. [PMC free article] [PubMed] [Google Scholar]
- 11.Forster A J, Stiell I, Wells G.et al The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad Emerg Med 200310127–133. [DOI] [PubMed] [Google Scholar]
- 12.BBC News £30m pumped into casualty. 29 September 1998. http://news.bbc.co.uk/1/hi/health/183053.stm (accessed 27 April 2005)
- 13.Alberti G. NHS emergency care services are the envy of the world. 2004/0381. Available at: http://www.dh.gov.uk (accessed 27 April 2005)
- 14.Wass A, Zoltie N. Changing patterns in accident and emergency attenders. J Accid Emerg Med 199613269–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanders A B. Care of the elderly in emergency departments: conclusions and recommendations. Ann Emerg Med 199221830–834. [DOI] [PubMed] [Google Scholar]
- 16.Finucaine P M, Wundke R, Whitehead C.et al Profile of people referred to an emergency department from residential care. Aust N Z J Med 199929494–499. [DOI] [PubMed] [Google Scholar]