Abstract
Objectives
To evaluate the effect of introducing an extended scope physiotherapy (ESP) service on patient satisfaction, and to measure the functional outcome of patients with soft tissue injuries attending an adult emergency department (ED), comparing management by ESPs, emergency nurse practitioners (ENPs), and all grades of ED doctor.
Methods
The ESP service operated on four days out of every seven in a week in an urban adult ED. A satisfaction questionnaire was sent to all patients with a peripheral soft tissue injury and fractures (not related to the ankle) within one week of attending the ED. Patients with a unilateral soft tissue ankle injury were sent the acute Short Form 36 (SF‐36) functional outcome questionnaire, with additional visual analogue scales for pain, at 4 and 16 weeks after their ED attendance. Waiting times and time spent with individual practitioners was also measured.
Results
The ESP service achieved patient satisfaction that was superior to either ENPs or doctors. Overall 55% of patients seen by the ESP service strongly agreed that they were satisfied with the treatment they received, compared with 39% for ENPs and 36% for doctors (p = 0.048). Assessment of long‐term outcome from ankle injury was undermined by poor questionnaire return rates. There was a trend towards improved outcomes at four weeks in those patients treated by an ESP, but this did not achieve statistical significance.
Conclusion
Adding an ESP service to the interdisciplinary team achieves higher levels of patient satisfaction than for either doctors or ENPs. Further outcomes research, conducted in a wider range of emergency departments and integrated with an economic analysis, is recommended.
Keywords: emergency medical services, physical therapy (specialty), delivery of health care
Nurses and allied health professionals are increasingly adopting new roles within the UK National Health Service, adapting skills and using proactive education programmes to expand their scope of practice.1 It is, however, essential to demonstrate that individuals who are treating patients have the necessary skills and competencies to deliver high quality care.2
An extended scope physiotherapist (ESP) is a physiotherapist who has additional skills in assessment, diagnosis, and management. In the adult emergency department (ED) of the Bristol Royal Infirmary an ESP is able to autonomously manage new patient presentations of soft tissue injuries and associated fractures, request radiographs, prescribe limited medications, and refer to other services as required. The addition of an ESP to the interdisciplinary team increases access to a practitioner with specialist skills for patients and staff.3 Although research relating to the role and effectiveness of ESPs has been published, this has concentrated on ESPs in orthopaedic, rheumatology, and spinal outpatient clinics.4,5,6,7,8,9 There is no published research evaluating patient satisfaction with ESPs in the ED. However, studies of patient satisfaction with ENPs have all reported positive outcomes in relation to communication, education, and care received.10 There is little research concerning the role of an ESP managing an independent caseload in the ED and the effects on treatment outcomes, but a recent randomised trial reported that initial assessment by a physiotherapist led to an increased time before patients returned to normal activities, compared with usual ED care.11 In the present study we also aimed to evaluate the effect of introducing an ESP in the adult ED, comparing three different practitioners: doctors, emergency nurse practitioners (ENPs), and ESPs.
Objectives
To compare patient satisfaction between ESP, ENP, and all grades of doctor in an adult ED.
To evaluate functional outcome from unilateral soft tissue ankle injury, comparing management by ESP, ENP, and all grades of ED doctor.
Method
We undertook this single centre study in the adult ED of the Bristol Royal Infirmary between September 2003 and April 2004. The Central and South Bristol Research Ethics Committee approved the study.
ESP service
The ESP service provided a range of representative early shifts (8.30 am to 3.30 pm) and late shifts (12.30 pm and 7.30 pm) on four days out of every seven days of the week. An ESP independently managed a caseload from arrival to disposal and was trained to request x rays, prescribe limited medication, and independently manage patients with peripheral soft tissue injuries and associated fractures. The ESP service used the same protocols as the other practitioners.
Data collection
The ED notes relating to all patients attending between 8:30 am and 7:30 pm were reviewed by hand on a daily basis, seeking patients eligible to be included in either part of the study (patient satisfaction or outcome from soft tissue ankle injury). Where available, data were also collected for each of the three practitioner groups concerning the arrival to discharge time, arrival to first contact with the treating clinician and time spent with the treating clinician.
Patient satisfaction questionnaire
A patient satisfaction questionnaire was developed and piloted in February 2003 (see Appendix 1 online at http://www.emjonline.com/supplemental/). It was sent to all patients with a peripheral soft tissue injury or fracture (not related to the ankle) within one week of attending the ED. Patients were only sent the questionnaire if they had attended the ED during a period when the ESP service was present. This is because patient satisfaction is known to be strongly associated with waiting time,12 which might be reduced when an ESP was present. The proportion of patients who reported that they were “very satisfied” with various aspects of the service was compared between the three professional groups: ESPs, ENPs, and doctors using a Pearson χ2 test. All returned patient satisfaction questionnaires were scanned using optical character reader Teleform 8.0 software to automate data entry. A total of 550 patients was required to detect a change from 30% to 50% in the proportion responding “very satisfied” (ESP 140 patients, all other practitioners 410 patients).
Assessment of outcome
For the outcome study, we recruited patients who presented to the ED with a unilateral soft tissue injury of the ankle and no associated fracture. We used a well‐established functional outcome questionnaire with proved reliability and sensitivity, the acute Short Form 36 (SF‐36). The acute SF‐36 is useful for comparing general and specific populations, and differentiating between the health benefits produced by different treatments.13 A visual analogue scale (VAS) was added to measure pain levels at rest and during activity at the time of completing the questionnaire and before the injury. This allowed a pre‐injury baseline to be established, thereby optimising the value of the SF‐36. Eligible patients were sent a questionnaire four weeks after their ankle injury. If they replied to this questionnaire a second identical questionnaire was sent 16 weeks after the injury.
We analysed the SF‐36 and additional VAS using non‐parametric statistics. Both median values with ranges, and means with standard deviations, are reported to facilitate understanding and future sample size calculations. Where statistical comparisons were made we used a Kruskal–Wallis test.
Results
During the period of the study there were 11 771 minor injury attendances to the Bristol Royal Infirmary emergency department. A total of 780 patients were sent patient satisfaction questionnaires and 489 patients were recruited to the ankle injury outcome study. The patient satisfaction questionnaire yielded a 45% return rate (n = 351). Satisfaction was consistently higher for the ESP service than for either of the other professional groups in all seven of the domains studied (table 1). Overall, 55% of patients strongly agreed that they were satisfied with the treatment they received, compared with 39% for ENPs and 36% for doctors.
Table 1 Percentage of patients who responded “strongly agree” to the individual questions in the patient satisfaction questionnaire, comparing extended scope physiotherapist (ESP), emergency nurse practitioner (ENP) and doctor (all grades).
| Question | ESP | ENP | Doctor | p value* |
|---|---|---|---|---|
| I felt I received good advice and information about my condition | 48.4 | 24.3 | 25.5 | 0.03 |
| I was given enough time to ask questions and discuss my condition | 45.5 | 18.9 | 27.7 | 0.05 |
| I felt confident the member of staff could deal with my condition | 48.4 | 37.8 | 31.9 | 0.123 |
| I felt confident the member of staff would have got a second opinion if necessary | 47.2 | 27.0 | 25.0 | 0.08 |
| The member of staff explained the results of the assessment | 50.0 | 29.7 | 19.1 | 0.01 |
| The member of staff explained what would happen next regarding my injury | 43.8 | 27.0 | 26.7 | 0.049 |
| Over all I was satisfied with the treatment received | 54.5 | 38.9 | 35.6 | 0.048 |
*Pearson χ2 test.
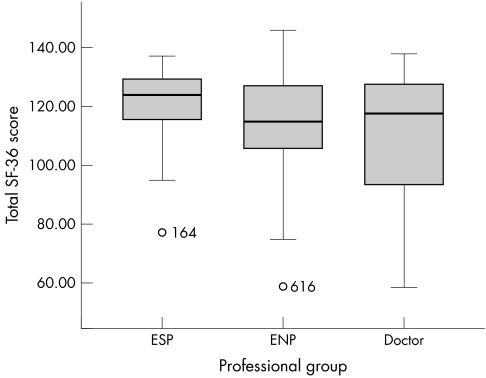
The SF‐36 questionnaire and VAS were sent to 489 patients. The return rate at one month was 22%, and only 4.5% at both one and three months. Due to the poor return rate at three months only the one month data are presented here. The number of valid SF‐36 data sets at one month was 91/489 (18.6%). Figure 1 shows total SF‐36 scores comparing ESP, ENP, and doctor. The total number of valid VAS at one month was 104, and the results from these are summarised in table 2. Graphical investigation showed the VAS results to be highly skewed before injury, and slightly skewed after injury.
Figure 1 Combined Short Form 36 (SF‐36) results at one month after injury, comparing extended scope physiotherapist (ESP), emergency nurse practitioner (ENP), and doctor (all grades). In this analysis, a higher number indicates a better health status.
Table 2 Means and medians of the visual analogue scales for pain and function one month after injury, comparing extended scope physiotherapist (ESP), emergency nurse practitioner (ENP) and doctor (all grades).
| Variable | ESP (n = 16) | ENP (n = 38) | Doctor (n = 50) | *p value | |||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (range) | Mean (SD) | Median (range) | Mean (SD) | Median (range) | ||
| Pre‐injury pain | 0.16 (0.22) | 0.00 (0.00–0.65) | 0.38 (0.77) | 0.00 (0.00–0.38) | 0.38 (1.33) | 0.00 (0.00–8.00) | 0.47 |
| Post‐injury pain | 1.50 (1.72) | 0.43 (0.00–4.45) | 1.97 (2.49) | 1.00 (0.00–1.97) | 1.97 (1.85) | 1.00 (0.00–6.70) | 0.58 |
| Pre‐injury function | 0.68 (1.50) | 0.08 (0.00–5.70) | 0.20 (0.44) | 0.00 (0.00–0.20) | 0.20 (1.41) | 0.00 (0.00–6.90) | 0.67 |
| Post‐injury function | 2.34 (2.66) | 0.80 (0.00–7.25) | 2.49 (2.62) | 1.55 (0.00–2.49) | 2.49 (2.16) | 1.55 (0.00–8.25) | 0.08 |
In this analysis, lower scores indicate reduced pain and increased function.
*Kruskal–Wallis test.
Both the SF‐36 and the VAS show a trend towards improved pain and function one month after injury in patients managed by an ESP, compared with management by an ENP or doctor, but the numbers are small and should therefore be interpreted with caution.
The waiting time analysis showed that patients managed by an ESP waited less time to be seen and less time overall than those managed by an ENP or doctor (table 3). Patients also spent more time with the ESP than they did with either a doctor or ENP. Although these results do not reach statistical significance there is an interesting trend, with patients who saw an ESP spending 36% of their ED stay with a clinician, compared with 20% for doctors and 19% for ENPs. In addition, the overall ED stay of patients who saw an ESP was reduced. These observations may have a significant impact on patient satisfaction.
Table 3 Comparison of time waiting to be seen, time spent with the patient, and total arrival to discharge time of patients with minor injuries managed by an extended scope physiotherapist (ESP) or emergency nurse practitioner (ENP) or doctor (all grades)*.
| ESP | ENP | Doctor | |
|---|---|---|---|
| Time waiting to be seen | 43 (n = 21) | 55 (n = 71) | 80 (n = 93) |
| Time spent with patient | 25 (n = 22) | 15 (n = 74) | 20 (n = 77) |
| Total arrival to discharge time | 69 (n = 23) | 79 (n = 80) | 99 (n = 91) |
*All times are mean values and measured in minutes.
Discussion
A wide range of new initiatives in the ED, such as “see and treat” and “streaming”, have been advocated as ways of improving waiting times without reducing the quality of care.14 However, many of these initiatives lack good evidence to support them.15 We therefore set out to evaluate the effect of introducing an ESP service on both patient satisfaction and clinical outcomes.
Our patient satisfaction study showed strong support for an ESP service. This superior satisfaction may reflect the appropriate use of a physiotherapist's skills, and satisfaction may itself be a good indicator of quality of care.16 There are, however, many other important factors to consider. Patients who were managed by an ESP spent almost twice as much time with the treating clinician, and the more time a practitioner spends with a patient the more satisfied they are likely to be. In addition, the overall ED stay of patients who saw an ESP was reduced. These factors alone will have a powerful influence on patient satisfaction, and it is therefore unclear how much of the improved satisfaction was due to the reduced stay and increased attention, and how much was due to the unique skills of an ESP.
Patients may have preconceived ideas about treatment by different members of the interdisciplinary team, which may also be influenced by previous experiences or education. Patients are frequently managed by a single member of the interdisciplinary team (ENP, doctor, or ESP), and will receive different levels of information depending on experience, personality, time pressures, and the communication skills of the practitioner. Patients who saw an ESP felt they received significantly better advice about their condition, were given time to ask questions, and received a clear explanation of the results of their assessment, as well as the management plan. All of these factors are important when educating and empowering patients to recover effectively from soft tissue injuries. These factors may also explain the increased time spent with the physiotherapist, and also suggest that ESPs may be less “efficient” than other practitioners in terms of the number of patients seen and treated within a set period of time.
The SF‐36 and VAS failed to show any statistically significant difference in the outcome of patients who attended the ED with unilateral soft tissue ankle injuries. The return rate of the questionnaire was much lower than expected, undermining the comparisons made. However, despite the small number of patients there is a trend for management by an ESP to be associated with reduced pain, improved physical function, and improved general health status one month after injury. This is in contrast to the recently published study of initial physiotherapy assessment in an ED,11 and is difficult to reconcile. Our results are inconclusive and based on smaller numbers, but do not support the idea that ESP management has an adverse effect on outcome. Differences in training and competencies, or patient case mix may also be relevant and deserve further study.
Our study had several weaknesses. Firstly, it was conducted in a single centre, and the wider applicability of our findings is unknown. Secondly, it also evaluated the work of a single ESP, and it is therefore impossible to say to what extent the findings are attributable to one individual, or to all ESPs in general. Finally, the observational methodology employed is less robust than the randomised design employed by Richardson et al.11
The ED is unlikely to benefit from more than one or two whole time equivalent ESPs within an interdisciplinary team, mainly because ESPs are not as versatile as ENPs or ED doctors. This specificity of treatment limits the number of patients that they can see (20–30% of all patients attending our adult ED), but they are capable of managing a specific minor injuries “stream” with good throughput, high patient satisfaction, and clinical outcomes that may be superior to current practice.
Conclusion
This study shows that an ESP achieves higher levels of patient satisfaction than either doctors or emergency nurse practitioners in the management of soft tissue injuries and associated fractures. Much of this may be attributable to reduced waiting time and increased clinician contact for patients seeing an ESP, as well as the specialist skills of this professional group. We failed to demonstrate any significant difference in the outcome of unilateral ankle soft tissue injuries, possibly due to poor questionnaire return rates, but a trend favouring management by an ESP was observed. Further outcomes research, integrated with a formal economic analysis, is required.
Expansion of professional boundaries is being actively encouraged within the modern NHS, but a programme of formal evaluation, to provide robust information on which future decisions can be based, must accompany such initiatives. This will also ensure that a patient focus is maintained, and that the most appropriate skills are used to create the optimal interdisciplinary team.
Acknowledgements
We thank Sue Taylor, Head of Physiotherapy at United Bristol Healthcare Trust, Mike Paynter, lead Emergency Nurse Practitioner, Bristol Royal Infirmary Emergency department, and Rebecca McClellan for their assistance with this study.
Authors' contributions
C M McClellan initiated the research with the support of R Greenwood and J Benger. The protocols were designed by all authors. Data were collected by C M McClellan and analysed by R Greenwood. The manuscript was drafted by C M McClellan and revised by R Greenwood and J Benger. The guarantor for the paper is C M McClellan.
Abbreviations
ED - emergency department
ENP - emergency nurse practitioner
ESP - extended scope physiotherapist
SF‐36 - Short Form
VAS - visual analogue scale
Footnotes
This study was supported by the United Bristol Healthcare Trust and INSEAD.
Competing interests: none declared
References
- 1.Department of Health Freedom to practice: dispelling the myths. London: The Stationery Office, 2004
- 2.Alberti K G. Skillmix: an advance or an excuse? Emerg Med J 200320112–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hattam P, Smeatham A. Evaluation of an orthopaedic screening service in primary care. Br J Clin Governance 1999445–49. [PubMed] [Google Scholar]
- 4.Daker‐White G, Carr A J, Harvey I.et al A randomised controlled trial. Shifting the boundaries of doctors and physiotherapists in orthopaedic outpatients departments.J Epidemiol Community Health 199953643–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hourigan P G, Weatherley C R. The physiotherapist as orthopaedic assistant in a back pain clinic. Physiotherapy 199581546–548. [Google Scholar]
- 6.Langridge J C, Moran C J. A comparison of two methods of managing patients suffering from rheumatoid arthritis. Physiotherapy 199480109–113. [PubMed] [Google Scholar]
- 7.Byrne G. Patient satisfaction with emergency nurse practitioners in A&E.J Clin Nurs 2000983–93. [DOI] [PubMed] [Google Scholar]
- 8.Hockin J, Bannister G. The extended role of a physiotherapist in an outpatient orthopaedic clinic. Physiotherapy 199480281–284. [Google Scholar]
- 9.Weale A E, Bannister G. Who should see orthopaedic outpatients: physiotherapists or surgeons? Ann R Coll Surg Eng (Suppl) 19957771–73. [PubMed] [Google Scholar]
- 10.Byrne G. Patient satisfaction with emergency nurse practitioners in A&E.J Clin Nurs 2000983–93. [DOI] [PubMed] [Google Scholar]
- 11.Richardson B, Shepstone L, Poland F.et al Randomised controlled trial and cost consequences study comparing initial physiotherapy assessment and management with routine practice for selected patients in an accident and emergency department of an acute hospital. Emerg Med J 20052287–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor C, Benger J R. Patient satisfaction in the emergency department. Emerg Med J 200421528–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ware J E. SF‐36 survey update. Spine 2000243130–3139. [DOI] [PubMed] [Google Scholar]
- 14.Lammy D. Reforming emergency care; for patients. Emerg Med J 200320112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leaman A M. See and treat: a management driven method of achieving targets or a tool for better patient care? One size does not fit all. Emerg Med J 200320118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomas L H, Bond S. Measuring patient's satisfaction with nursing. J Adv Nurs 199623747–756. [DOI] [PubMed] [Google Scholar]