Abstract
We describe a lethal poisoning in a healthy woman caused by deliberate ingestion of aluminium phosphide (AlP), a pesticide used to kill rodents and insects. Toxicity of AlP and review of cases reported to the National Poisons Information Service (London) 1997–2003 are discussed.
Keywords: Aluminium phosphide, phosphine, poisoning, toxicology
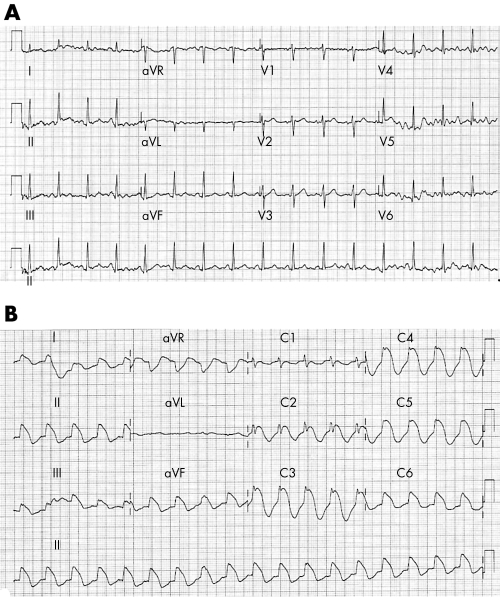
A previously well 41 year old Indian woman presented 2 hours after ingestion of a 10 g sachet of Fumino (aluminium phosphide (AlP) 56% w/w; United Phosphorus) mixed with water. She was distressed, vomiting, and had severe epigastric pain with blood pressure 70/58 mmHg, pulse 100 beats/min, oxygen saturation 86% on air, and temperature 37.1°C. Arterial blood gases (ABG) on 10 l/min oxygen showed pO2 37.7 kPa, pCO2 3.04 kPa, pH 7.27, bicarbonate 13.2 mmol/l, and base excess (BE) −14.4. Chest x ray showed bilateral pulmonary infiltrates and ECG a sinus tachycardia (fig 1A). She was treated with intravenous colloid (1 litre Gelofusion over 30 minutes), 200 mg hydrocortisone, 40 mg pantoprazole, 300 mg phenytoin, and 50 mmol sodium bicarbonate. Infusions of N‐acetylcysteine (6.5 g over 24 h) and magnesium sulphate (70 mmol/l over 24 hours) were commenced. She remained hypotensive and her clinical condition deteriorated with worsening hypoxia and metabolic acidosis (ABG on 15 l/min O2: pO2 10.6 kPa, pCO2 4.24 kPa, pH 7.16, bicarbonate 12 mmol/l, BE –16). She was paralysed, intubated, and ventilated. Metabolic acidosis was treated with 50 mmol/h sodium bicarbonate but despite fluid resuscitation, she required norepinephrine and later epinephrine infusion (maximum 3 µg/kg/min) to maintain blood pressure. Continuous venous–venous haemofiltration was commenced in an attempt to correct the acidosis. A portable echocardiograph (Sonoheart Elite) showed normal left ventricle (LV) size with moderately impaired LV function and cardiac index of 1.5 l/min/m2. A broad complex tachycardia (fig 1B) occurred, which was treated with amiodarone (300 mg over 1 hour). Serial creatinine kinase, and amylase were within normal limits. Subsequently she developed disseminated intravascular coagulation and adult respiratory distress syndrome. Despite supportive management she died 36 hour after admission.
Figure 1 Electrocardiographic changes following aluminium phosphide poisoning. (A) 12‐lead surface ECG recorded on admission showing sinus tachycardia. (B) ECG recorded 12 hours later showing extreme widening of the QRS complex despite amiodarone therapy.
DISCUSSION
AlP is a highly toxic, low cost rodenticide. Upon exposure to moisture, it liberates phosphine gas, which is absorbed rapidly by inhalation, dermally, or gastrointestinally. For this reason, patients in Nepal presenting within 1 hour of AlP ingestion undergo gastric lavage with vegetable oil.1 The gaseous nature of phosphine has potential for contamination of emergency service personnel exposed to victims, and when AlP tablets are swallowed, contamination of body tissues results.2,3 Our risk assessment suggested low potential for secondary contamination of the emergency department, as ingestion had occurred 2 hours previously and was accompanied by profuse vomiting. Her clothes were not stained with vomit and there was no characteristic garlic smell of phosphine. However, "off gassing" of phosphine in the patient's expired breath might have been a potential hazard. In the absence of respiratory protection, risk is minimised by treating the patient in a well ventilated area, and in ventilated patients by using a scavenging system.
In the UK, AlP is available in the form of tablets or pellets (Phostoxin, Talunex, and Degesch) used as rodenticides, and supply is restricted under the Pesticides Act 1998 to qualified users. In India, AlP is cheap and widely available, and is responsible for many cases of poisoning. In our case, AlP was obtained in India and exposure confirmed by the patient, who was brought to hospital with the empty sachet. In a study of 559 cases of acute poisoning in India, 68% were due to AlP exposure, with 60% mortality.4,5 Clinical features of AlP poisoning are severe vomiting, resistant hypotension, and metabolic acidosis.6
Immediate release of phosphine gas from AlP when mixed with aqueous solutions leads to rapid absorption through the lungs and gut when swallowed. Its gaseous form and toxicity makes it a potential agent for chemical terrorism, and unregulated sales within the UK have been reported, with a potential for importing from developing countries where there is no control of supply.7
Toxicity of phosphine is related to oxidant free radicals and associated inhibition of enzymes of metabolism, such as cytochrome c oxidase.8 Apart from supportive treatment, novel therapies such as N‐acetylcysteine, replenishing cellular glutathione, and magnesium, which has been reported to have antioxidant properties, have been suggested.9 A characteristic feature of AlP poisoning is myocardial suppression and resistant hypotension. In rats exposed to AlP, N‐acetylcysteine increased survival time and reduced myocardial oxidative injury.10 Other agents include trimetazidine, which switches myocyte metabolism to glucose from fatty acids, thus reducing oxygen consumption, and may have a potential role.11
Between January 1997 and June 2003, there were 93 cases of AlP exposure reported to the National Poisons Information Service (London): 8 AlP ingestion, 57 phosphine gas inhalation, 3 topical exposure, 11 oral/inhalation or oral/topical, and 14 where the exposure route was unknown. Of these 93 cases, 17 were asymptomatic, 33 had respiratory symptoms, and 27 gastrointestinal symptoms. There was one death reported, an 80 year old man. However, most cases were due to accidental, relatively limited exposure in agricultural settings to phosphine gas. The incidence of self poisoning with AlP does not appear to be increasing.
The nature of this poison makes it a potential agent for chemical terrorists, and release of phosphine gas in an enclosed space would lead to respiratory toxicity, public chaos, and widespread contamination. Recognition of the characteristic garlic smell of phosphine gas should alert front line emergency staff to the possibility of AlP/phosphine exposure. Current management is supportive; however, survival is unlikely if more than 1.5 g is ingested.6
ACKNOWLEDGEMENTS
We are grateful to Mr N Edwards, Manager NPIS (London) for searching the NPIS (London) database.
Abbreviations
AlP - aluminium phosphide
LV - left ventricle
Footnotes
Competing interests: there are no competing interests
References
- 1.Jones A L, Volans G. Management of self poisoning. BMJ 1999320712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nocera A, Levitin H W, Hilton J M. Dangerous bodies: a case of fatal aluminium phosphide poisoning. Med J Aust 2000173133–135. [DOI] [PubMed] [Google Scholar]
- 3.British Broadcasting Corporation Millionaire's death sparks poison scare. http://news.bbc.co.uk/1/low/england/2314911.stm . Accessed 10 March 2004
- 4.Siwach S B, Gupta A. The profile of acute poisonings in Harayana‐Rohtak Study. J Assoc Physicians India 199543756–759. [PubMed] [Google Scholar]
- 5.Singh D, Jit I, Tyagi S. Changing trends in acute poisoning in Chandigarh zone: a 25‐year autopsy experience from a tertiary care hospital in northern India. Am J Forensic Med Pathol 199920203–210. [DOI] [PubMed] [Google Scholar]
- 6.Singh S, Singh D, Wig N.et al Aluminium phosphide poisoning: a clinico‐pathologic study. J Toxicol Clin Toxicol 199634703–706. [DOI] [PubMed] [Google Scholar]
- 7.British Broadcasting Corporation Rogue traders. http://bbc.co.uk/pressoffice/pressreleases/stories/003/02february/06/roguetraders.shtm . Accessed 10 March 2004
- 8.Chefurka W, Kashi K P, Bond E J. The effect of phosphine on electron transport in mitochondria. Pestic Biochem Physiol 1976665–84. [Google Scholar]
- 9.Chugh S N, Kolley T, Kakkar R.et al A critical evaluation of anti‐peroxidant effect of intravenous magnesium in acute aluminium phosphide poisoning. Magnes Res 199710225–230. [PubMed] [Google Scholar]
- 10.Azad A, Lall S B, Mittra S. Effect of N‐acetylcysteine and L‐NAME on aluminium phosphide induced cardiovascular toxicity in rats. Acta Pharmacol Sin 200122298–304. [PubMed] [Google Scholar]
- 11.Duenas A, Perez‐Castrillon J L, Cobos M A.et al Treatment of the cardiovascular manifestations of phosphine poisoning with trimetazidine, a new anti‐ischemic drug. Am J Emerg Med 199917219–220. [DOI] [PubMed] [Google Scholar]