Abstract
Medically unexplained physical symptoms (MUPS) are physical symptoms for which no relevant organic pathology can be found. Patients with MUPS commonly present to the emergency department (ED) but are rarely considered in emergency medicine teaching or literature. Management of these patients is frequently more challenging than where there is an obvious organic pathology. This review provides the emergency physician with background knowledge regarding the classification and aetiology of MUPS. It then provides strategies for more effective management, such as exploring the contribution of psychosocial factors with patients, explaining negative test results, and providing reassurance and avoiding creating iatrogenic anxiety. Early recognition of the fact that symptoms may not result from organic disease and an appreciation of the role of psychosocial factors may improve outcomes by reducing unnecessary investigation and admission, and avoiding reinforcement that encourages further similar presentations and unhelpful coping mechanisms.
Keywords: emergency medicine, psychosomatic medicine, somatoform disorders
Medically unexplained physical symptoms (MUPS) are physical symptoms for which no relevant organic pathology can be found. MUPS are very common, comprising up to half of all consultations in primary care and up to one third of those in hospital outpatient clinics.1 Some studies indicate higher prevalence; a landmark study of medical outpatients in North America with new complaints of common symptoms such as chest pain, dyspnoea, dizziness, and headache, found that an organic cause was demonstrated in only 16% of cases.2 Prevalence data for undifferentiated emergency department (ED) populations are very limited. A study of adult patients attending a UK inner city ED found the rate of somatisation and somatoform disorders to be a surprisingly low 3.8%.3 However, this may have arisen due to the application of overly strict diagnostic criteria, allied with a lack of verification of the presence of an organic cause for self‐reported illness. The true ED prevalence probably lies somewhere between this figure and the rates seen in primary care and outpatient clinics.
Although MUPS are a major clinical problem and widely regarded as being difficult to manage,4 sophisticated approaches to management or even recognition of the problem are unusual, especially in hospital medicine. The standard approach is often to rule out all possible physical causes with extensive investigation, and then to either tell the patient that there is nothing wrong or refer them to a psychiatrist. As this approach may take weeks or months, it is not usually possible in a brief ED consultation, even if it were desirable. Moreover, early recognition and communication of the fact that symptoms may not result from organic disease, and early appreciation of the role of psychosocial factors, may improve outcomes.5,6 Emergency physicians are well placed to employ this approach, with the potential to avoid unnecessary investigation, reduce hospital admissions, and avoid reinforcing the patient's belief that there is something physically wrong.7
Despite their impact, and the importance of effective management, MUPS are rarely considered in ED teaching or literature. This article is a narrative review that aims to raise awareness and understanding of this common problem and make suggestions for improved management. Cited literature is selected from that obtained by Medline searches, hand searches, the authors' own knowledge, and expert opinion. By necessity, the evidence is partly drawn from work undertaken outside the ED, and at times is qualitative or of limited quality. Learning objectives are listed in box 1.
Box 1 Objectives for the emergency physician in the management of medically unexplained symptoms (MUPS)
To be aware that patients commonly present with MUPS
To understand the terminology and scope of MUPS
To be able to explore relevant psychosocial issues with the patient
To avoid unnecessary investigation and referral where possible
Terminology
Several groups of patients with MUPS can be identified. The clinical distinction between these groups can be difficult, and the terminology continues to develop. Formal classification systems such as DSM‐IV and ICD‐10 provide precise case definitions relating to MUPS.8,9 However, these terms are not useful to the emergency physician in everyday practice, and the aim here is to provide basic terminology that will be useful and easily understood in normal practice.
Somatisation is the presentation to medical care of physical symptoms for which no organic explanation can be found, as a manifestation of psychological distress. The symptoms are not intentionally produced and are experienced as real. If any physical disorders are present, they do not explain the nature or extent of the symptoms, or the distress of the patient. When many symptoms are presented over a long period of time, this is termed somatisation disorder. When a single symptom is presented, this is termed a functional somatic syndrome. Most medical specialties have one or more such syndromes associated with them (box 2), and patients with these syndromes commonly present to the ED. While there is a tendency for each speciality to see a discrete condition within its own domain, patients being treated for one somatic syndrome frequently have several symptoms from other syndromes, and there is considerable overlap of symptoms between different syndromes.10
Box 2 Functional somatic syndromes by medical speciality
Cardiology – non‐cardiac chest pain, benign palpitation
Gastroenterology – irritable bowel syndrome, non‐ulcer dyspepsia
Rheumatology – fibromyalgia, repetitive strain injury
Immunology – multiple chemical sensitivity
General medicine – chronic fatigue syndrome
ENT – globus syndrome
Neurology – conversion disorders, non‐epileptic attacks, chronic benign headache
Gynaecology – chronic pelvic pain
Paediatrics – non‐specific abdominal pain
Hypochondriasis is preoccupation with the presence of one or more serious diseases, in the absence of relevant organic disease, that persists despite medical reassurance. It contrasts with somatisation in that the preoccupation is with a specific disease rather than specific symptoms.
Dissociative disorder (formerly hysteria or conversion) is the presentation of neurological symptoms that cannot be explained by physical disorder. It includes paralysis, sensory loss, amnesia, stupor, and non‐epileptic attacks (pseudoseizures). It differs from somatisation in that there must also be physical signs of altered or lost function. Patients may exhibit “la belle indifference”, in that they appear inappropriately unconcerned about their often florid symptoms, but this feature is neither sensitive nor specific. The pattern of symptoms and signs tends to reflect lay views of the human body's functioning rather than medical understanding. For example, the pattern of sensory loss will often not correspond with that caused by any genuine neurological lesion.
Psychogenic (or somatoform) pain disorder involves persistent pain in a single organ system, the duration or intensity of which cannot be explained in physical terms. Many cases are precipitated by trauma such as a road traffic accident. Common examples are neck and back pain. Pain, rather than any diagnostic implications, is the focus of attention, in contrast to hypochondriasis.
Factitious disorder, an extreme form of which is Munchausen's syndrome, is the deliberate feigning of symptoms in order to gain medical attention. Physical symptoms include abdominal pain, chest pain, or haematuria, for example. Psychiatric symptoms can also be presented, such as delusions or hallucinations.
Malingering is the deliberate feigning or exaggeration of symptoms for obvious material gain, such as insurance payment, or to avoid sleeping rough or imprisonment.
These terms may be unacceptable to patients. The challenge for doctors is to use terminology that is meaningful to both colleagues and patients. This is probably best achieved by describing the problem rather than communicating a diagnosis. The term “functional symptoms” may be more acceptable and has been evaluated elsewhere.11
Aetiology
Explanations for MUPS range from the purely physical to the purely psychological (box 3). At the physical end of the spectrum, it is possible that a symptom is medically unexplained only because we do not yet understand its pathophysiology. As our understanding advances, the unexplained may cease to be so. For example, there is evidence supporting the role of abnormal sensitivity to visceral pain as a possible mechanism in several functional somatic syndromes, such as non‐cardiac chest pain and irritable bowel syndrome.12 It would therefore be more correct, but rather clumsy, to use the term “symptoms unexplained by known organic disease”.
Box 3 The scope of medically unexplained physical symptoms
Physical symptoms of anxiety and depression
Anxiety or depression secondary to physical illness
Acute somatisation
Chronic somatisation (usually multiple symptoms and systems)
Functional somatic syndromes
Fabricated symptoms – factitious disorder and malingering
Symptoms with organic pathophysiology which has yet to be discovered/understood
At the psychological end of the spectrum, sometimes the physical symptoms are clearly recognised symptoms of anxiety and depression. Depression often presents with poor appetite, weight loss, fatigue, sleep disturbance, and, in the elderly, apparent cognitive impairment. Anxiety may present acutely with symptoms such as dizziness, shortness of breath, palpitation, and chest pain. Indeed, in cultures where the stigma of mental illness is great, the majority of psychiatric presentations consist of purely physical symptoms.13 Furthermore, depression increases sensitivity to pain, and anxiety may increase health concern. These changes increase the likelihood that patients with physical symptoms will present to the ED.
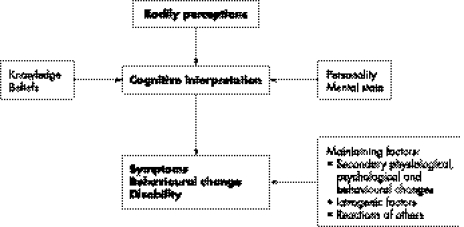
However, most MUPS are neither entirely physical nor entirely psychological. It is therefore rarely helpful to think of a single explanatory cause.14 Rather, as indicated in fig 1, there is usually a complex interaction between physical, psychological, and social mechanisms. The biomedical model clearly fails in achieving an understanding of MUPS and the biopsychosocial model is more useful.15
Figure 1 Interactive aetiology of unexplained symptoms (reproduced from Mayou R, Sharpe M, Carson A, eds. The ABC of psychological medicine. London: BMJ Books, 2003, with the permission of Blackwell Publishing).
The influence of cultural background has already been mentioned. A cultural tendency to somatise will be compounded if there is a language barrier, as the concept of physical pain is easier to convey with limited communication than that of psychological pain. Individual health beliefs are also influenced by many other factors. Childhood experience, the media, patient groups, and the internet may all play a part. Life events such as bereavement and chronic psychosocial stressors may trigger somatic presentations. Illness behaviour refers to the variety of possible responses to a given symptom, which can in some cases be out of all proportion to the underlying disorder. Abnormal illness behaviour may increase medical help‐seeking and disability in patients with symptoms due to both organic pathology and somatisation. A variety of iatrogenic factors may maintain MUPS. These include expressions of clinical uncertainty, unnecessary investigation, ambiguous or contradictory advice, reassurance that nothing is wrong without an adequate causal explanation, and appearing to reject the reality of the patient's symptoms.
Effective management of patients presenting with MUPS
There is a risk of missing important cues in patients with MUPS and assessing them as if they definitely have purely physical pathology that must be investigated and treated. Most doctors are understandably somatically focused, in that they focus on the more familiar territory of physical symptoms stemming from organic pathology16 and may ignore psychological aspects of an illness or the possibility that its cause may be mainly or entirely psychological. The high prevalence of somatic focus amongst doctors (and other healthcare professionals) may be part of the reason why some patients use somatic symptoms to communicate their psychological distress. Using the term “medicalisation” in a similar sense to somatic focus, Tate17 summarised the problem well, by stating that “a medicalising doctor and a somatising patient are a bad combination”. Stigma relating to psychological disorder may also play a role.
Communication with patients with MUPS needs to be flexible as they are a heterogeneous group. Patients will vary greatly in how willing they are to discuss psychosocial factors and accept the suggestion that such factors play a causal role in their physical symptoms. There are, broadly, three groups of patients. The first group may be relieved to talk about psychosocial issues and may already be aware that stress may cause or exacerbate their condition. The key is early recognition of the psychological origin of the complaint, so that the true problem can be addressed and reinforcement encouraging further somatic presentations avoided. Advice about stress management and other simple psychological approaches may benefit these patients. The second group may be angered and offended by any suggestion that their condition is not entirely physical in nature, and see it as tantamount to suggesting that they are “making it up”. Unless these patients can be encouraged to accept the role of psychological factors, their prognosis is likely to be poor. The third group are uncertain of the role of psychological factors. These patients are often at an early stage in their illness and unsure as yet as to whether their condition is physical or psychological in nature. Their early contacts with the medical profession, often in the ED, may therefore have a major influence on the future course of their illness.
Rule‐out medicine
There is a growing trend in emergency medicine for rapid rule out of certain medical conditions. The greatest focus has been on rapid rule out of ischaemic heart disease, often in chest pain units (CPUs), but other conditions such as pulmonary embolism, deep vein thrombosis (DVT), and subarachnoid haemorrhage have also been addressed. This new approach greatly compresses the timescale in which these conditions are ruled out. For example, patients who might previously have waited several weeks for outpatient exercise tolerance tests can now complete the assessment within a few hours in the ED. This has clear advantages to the patients with disease ruled in, in that further care can be planned and implemented much more quickly. In addition, patients in whom disease is ruled out may also benefit. It is known that there are high rates of psychological morbidity amongst patients with non‐cardiac chest pain,18 and there is now some evidence that this can be reduced by CPU assessment.19 The explanation for this is not clear, but it seems likely that addressing the problem early on reduces the potential for the patient to establish unhelpful ideas and behaviours linked to the sick role.
Within rapid rule‐out paradigms, the number of patients ruled out considerably exceeds the number ruled in. ED staff, both doctors and specialist nurses, are therefore frequently required to feed back the normal results of examination and investigation, in the presence of often severe physical symptomatology. The main interest is in detecting cases of significant, treatable disease. The experience in cardiology outpatient clinics suggests the opportunity to provide explanation and lifestyle advice regarding primary prevention to those patients with disease ruled out is often missed.6,20 Patients are usually urged to return to their GP for follow up, but the nature of this communication is probably very variable. The patient may be left with the rather unsatisfactory explanation that “we don't know what is wrong with you, but we do know what it isn't”, or given pseudo‐diagnoses such as “non‐cardiac chest pain” or “swollen calf, Doppler negative”. Clearly it is good practice to look for evidence supporting alternative diagnoses to that ruled out, such as gastroesophageal reflux disease in the case of chest pain, and ruptured Baker's cyst or gastrocnemius tear in the case of DVT. Unfortunately, this is not always done well or even at all. The logic of protocol‐based rule‐out medicine can be unthinkingly applied and explained to patients as “there is nothing (seriously) wrong with you, you can go home”. Careful consideration needs to be given to the explanation of negative results in order to avoid creating iatrogenic anxiety and to provide appropriate reassurance.
Explaining negative results
Doctors' explanations of MUPS have been analysed and three types of explanation identified.21 The commonest is rejection, in which the reality of the symptoms is denied, negative results equated with absence of cause, and an imaginary disorder or stigmatising psychological problem implied. In collusion, the doctor simply agrees with the patient's explanatory beliefs. Positive explanations involving empowerment are uncommon. In these, the doctor provides a tangible psychophysiological mechanism, removes blame, and provides opportunities for self help. Empowering explanations are clearly the ideal as they legitimise the patient's suffering and ally rather than alienate the patient and doctor. In contrast, explanations involving rejection, by offering no acceptable alternative explanation of symptoms, are likely to leave the patient clinging to the idea that their symptoms must in some way be related to physical illness.22
Taking a little extra time to provide a robust explanation to patients with negative results may be worthwhile in the longer term, by reducing the likelihood of such patients re‐presenting with the same problem. Better explanation may be facilitated by the provision of simple written materials for the different diagnostic categories. A CPU, for example, might provide three patient leaflets – two for “rule ins” such as myocardial infarction and angina, and one for “rule outs” such as non‐cardiac chest pain.20
Iatrogenic anxiety and reassurance
By raising the possibility, however remote, of organic disease, a Pandora's box can be opened that is not necessarily closed merely by carrying out negative investigations.23 In a study of 40 outpatients referred for echocardiography, anxiety persisted in the symptomatic group after negative investigation in all cases, and anxiety in the group referred due to the incidental finding of a heart murmur also persisted in 55% of cases following negative investigation.23 One common cause for failure of reassurance was referred to by the authors as “wild card effects”. This is when a particular aspect of the patient's personal beliefs or social experiences acts as an impediment to reassurance, such as when a patient presenting with headaches knows of someone who recently died of a brain tumour. This emphasises that to effectively reassure a patient it is first necessary to find out what they fear.
Reassurance in patients with unexplained symptoms has been studied in primary care.24 The term “normalisation” was favoured over “reassurance” as it makes no assumption as to the effect of the statement. Normalising statements without explanation, for example on the authority of a negative test result, or with explanation unrelated to the patient's concerns, were ineffective. In these cases, patients responded either with further requests for explanation, or by elaborating their symptoms, making further somatically focussed management more likely. The authors suggested that effective normalisation includes elements that acknowledge and validate patients' sense of suffering, provide tangible mechanisms to explain symptoms arising from patients' expressed concerns, and offer opportunity for linkage between psychological factors and physical mechanisms. Explanations that linked physical and psychological factors contributed to psychological management outcomes.
It is clear that explanation and reassurance regarding MUPS are central to effective management. Providing negative investigation results without appropriate explanation is of limited value, and can be counterproductive.
Talking about the contribution of psychosocial factors
The reattribution approach aims to develop the patient's understanding of the link between physical symptoms and psychosocial factors. It was first described by Goldberg et al25 following the observation of over 1000 primary care consultations. There have been later modifications26 and the approach has a sound evidence base in primary care.27 There are three basic stages (box 4), which have been amended slightly for the ED environment.
Box 4 The reattribution approach
1) Feeling understood – engage the patient and gather information
2) Broadening the agenda – to include social and psychological factors
3) Making the link – between physical symptoms, psychological distress, and social problems
Stage one: feeling understood
This stage aims to engage the patient and demonstrate that their problem is being taken seriously. A history is taken, during which emotional cues are responded to appropriately. Enquiry is made regarding primary care and hospital attendances regarding the current problem and other physical symptoms. A physical examination is then performed. Techniques such as making empathic statements, acknowledging the reality of the symptoms, and normalisation (explaining that such problems are commonly seen), may be used to facilitate engagement. Enquiring about disability and self care activities, and encouraging the patient to discuss their presenting problems without interruption or premature closure by the doctor, are also helpful.
Stage two: broadening the agenda
Once basic information has been gathered and a rapport has been established, the assessment can be broadened to include emotional and psychological aspects. Relevant social and family factors and the patient's health and illness beliefs are explored. At the end of this stage, a summary is presented to the patient, which includes relevant physical, psychological, and social factors, and points out temporal links between them, where possible.
Raising psychosocial issues with somatising patients can be difficult, and if done insensitively may suggest that they are not being taken seriously or are thought to be “making it up”. One technique that can be used is the “switch”.28 The doctor suggests that the physical symptoms might be making the patient feel depressed or anxious. For example: “You seem to have a lot of pain at the moment. I wouldn't be surprised if it was getting you down a bit”, or alternatively: “These headaches, are they making you feel on edge and irritable?”. Any positive response is then followed up on with a more detailed enquiry screening for anxiety and depression.29,30 If the response is negative, the patient is less likely to feel undermined than if the doctor had suddenly changed the subject to their mood.
Stage three: making the link
Finally, it is suggested to the patient that psychosocial factors may help to explain their physical symptoms. Goldberg et al25 described several ways in which doctors can make the link between physical symptoms and the patient's emotional state. These should be presented to the patient as suggestions, rather than dogmatically. For example, the doctor may explain that anxiety triggers release of hormones such as adrenaline, causing the heart to speed up and the gut to contract, causing pain. The lowering of the pain threshold by depression, and the link between anxiety, muscular tension and, for example, neck pain and headaches, are other examples. It may be helpful to ask if anyone else in the family experiences similar symptoms, and, if so, what brings them on, as it may be easier for people to see the “link” in other people. Tension headache and period pain are good examples that can be used to demonstrate that pain does not necessarily mean pathology. In these ways, a positive explanation may be provided for physical symptoms in the absence of physical pathology.
Chronic somatisation
A simple brief approach such as reattribution is unlikely to work with chronic somatisers. In primary care, the formulation, recording, and communication of a clear medium to long term management plan is important for such patients. It can involve: (a) providing regular (but not necessarily frequent) visits to the same doctor who is well acquainted with the patient; (b) aiming to avoid unnecessary investigations and referrals to secondary care, and (c) concentrating on coping with the symptoms rather than curing.31
Unfortunately, the objective of a therapeutic relationship with a single physician is not possible in the ED environment. Some patients become frequent attenders at the ED, where they are likely to see an inexperienced junior doctor who is not familiar with the nature of their condition or experienced in management, and therefore much more likely to make referrals and order investigations. Ensuring that old records are available whenever these patients present is essential, and computerised hospital records can aid identification. It can also help to have a management plan agreed by senior staff for patients with stereotyped multiple presentations, placed prominently in their notes (preferably ED as well as inpatient notes). Early involvement of senior staff is advisable. The best place for the management of chronic somatisation is primary care, and consistent attempts should be made to persuade the patient of this. Effective communication between the ED and primary care is crucial, and a jointly devised management plan may help.
Factitious disorder
Background
Munchausen's syndrome was described in 1951 and described the well known stereotype of the psychopathic male wandering between hospitals and feigning signs and symptoms often leading to multiple laparotomies.32 Although such patients do exist, the majority of patients with factitious disorder are now recognised to be relatively young, often female, and often working in healthcare.33,34 Estimates of incidence are difficult, because many cases probably go unrecognised. However, these patients can certainly use a disproportionate amount of healthcare resources35 and are difficult to manage.
The disorder can manifest at several levels. The simplest is fabrication of symptoms and feigning of physical signs. Investigations may be tampered with, such as by using blood from a finger prick to contaminate a urine sample. At the most extreme level, the disorder involves self‐inflicted injury and illness, for example, self injection of pyrogenic material or insulin, or creating or interfering with wounds. Associated psychiatric disorder is not universal, although personality difficulties are common. Motivation for this behaviour is hard to establish but seems to involve a desire to take up the sick role, perhaps as an escape from difficult circumstances or emotions. Unlike malingering there is no obvious material gain such as compensation or avoidance of imprisonment. As with somatisation, the emergency physician plays a crucial role in early recognition and the prevention of unnecessary investigation and intervention. In common with chronic somatisation, the key is prompt recognition of the problem on attendance at the ED, facilitated by the flagging of records where possible.
Management
ED staff may be angry or embarrassed when they realise that they have been deceived. The immediate instinct may be to seek retribution by unmasking the deception and then expelling the patient from the ED. However, this does little to solve anything other than the immediate problem, as the patient is likely to present elsewhere, or subsequently to the same department, and probably to different staff. It is obviously essential that professional standards of behaviour are maintained despite what can be unusually trying circumstances.
There is controversy as to the benefit of confrontation in factitious disorder. Some authors have suggested a “supportive confrontation”.36 In this, the patient is told that the staff are aware of what the patient is doing, and psychiatric care is offered, although frequently the offer is not taken up. Other authors have suggested that it is not necessary to confront patients but that they will give up their maladaptive behaviour when engaged in an empathic relationship with a doctor or therapist.33 This approach avoids the risk of the patient simply going elsewhere and allows treatment of any co‐existing psychiatric or physical illness. Some suggestions for ED management are given in box 5.
Box 5 Emergency department management of factitious disorder
Maintain professional standards of behaviour at all times
Address security issues where necessary
Provide care for physical illness or injury regardless of whether self induced
Decide need for confrontation on an individual basis. If it is likely to cause harm to the patient or make management more difficult, it is not essential
If confrontation is undertaken, it should be done supportively rather than aggressively
Offer psychiatric care. If there is significant physical illness or injury, this may need to be deferred
Accept that some patients will not engage in any discussion of their behaviour or accept psychiatric care
Communicate with primary care and other local EDs where possible
Conclusion
There is a tendency in emergency medicine, and most of hospital medicine, to practise based on the premise that most physical symptoms result from organic pathology. In the case of a major trauma patient for example, this is clearly the case. However, for many common physical symptoms, it is quite likely that no relevant organic pathology will be found. Awareness of the incidence and spectrum of medically unexplained symptoms, combined with techniques that facilitate communication in this challenging area, should help emergency physicians to improve outcomes by avoiding pursuing an exclusively biomedical approach. Indeed, a biopsychosocial approach may benefit patients regardless of the aetiology of their symptoms. A major challenge in the ED is deciding when full biomedical investigation is necessary, and when it can safely be avoided. There is, unfortunately, no easy answer to this question.
Abbreviations
CPU - chest pain unit
DVT - deep vein thrombosis
ED - emergency department
MUPS - medically unexplained physical symptoms
Footnotes
Competing interests: none
References
- 1.Bass C, Sharpe M. Medically unexplained symptoms in patients attending medical outpatient clinics. In: Weatherall DA, Ledingham JG, Warrell DA, eds. Oxford textbook of medicine. 4th ed. Oxford: Oxford University Press, 20031296–1303.
- 2.Kroenke K, Mangelsdorff D. Common symptoms in ambulatory care: incidence, evaluation, therapy and outcome. Am J Med 198986262–266. [DOI] [PubMed] [Google Scholar]
- 3.Williams E, Guthrie E, Mackway‐Jones K.et al Psychiatric status, somatisation and healthcare utilization of frequent attenders at the emergency department. A comparison with routine attenders. J Psychosom Res 200150161–167. [DOI] [PubMed] [Google Scholar]
- 4.Sharpe M, Mayou R, Seagroatt V.et al Why do doctors find some patients difficult to help? Q J Med 199487(3)187. [PubMed] [Google Scholar]
- 5.Peters A A, van Dorst E, Jellis B.et al A randomised clinical trial to compare two different approaches to women with chronic pelvic pain. Obstet Gynaecol 199177740–744. [PubMed] [Google Scholar]
- 6.Mayou R A, Bass C, Hart G.et al Can clinical assessment of chest pain be made more therapeutic? Q J Med 200093805–811. [DOI] [PubMed] [Google Scholar]
- 7.Purcell T B. The somatic patient. Emerg Med Clin North Am 19919137–159. [PubMed] [Google Scholar]
- 8.World Health Organization The ICD‐10 classification of mental and behavioural disorders. Geneva: World Health Organization, 1993
- 9.American Psychiatric Association Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association, 1994
- 10.Aaron L A, Buchwald D. A review of the evidence for overlap among unexplained clinical conditions. Ann Intern Med 2001134(9)868–881. [DOI] [PubMed] [Google Scholar]
- 11.Stone J, Wojcik W, Durrance D.et al What should we say to patients with symptoms unexplained by disease? “The number needed to offend”. BMJ 20023251449–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manu P.Functional somatic syndromes: etiology, diagnosis and treatment. Cambridge: Cambridge University Press, 2000
- 13.Goldberg D P, Bridges K. Somatic presentations of psychiatric illness in primary care setting. J Psychosom Res 198832(2)137–144. [DOI] [PubMed] [Google Scholar]
- 14.Mayou R, Farmer A. Functional somatic symptoms and syndromes. In: Mayou R, Sharpe M, Carson A, eds. The ABC of psychological medicine. London: BMJ Books, 200317–21. [DOI] [PMC free article] [PubMed]
- 15.Engel G L. The need for a new model: a challenge for biomedicine. Science 1977196126–136. [DOI] [PubMed] [Google Scholar]
- 16.Usherwood T.Understanding the consultation. Buckingham: Open University Press, 1999
- 17.Tate P.The doctor's communication handbook. 3rd ed. Abingdon: Radcliffe Medical Press, 2001
- 18.Mason S S, Arnold J, Angelini K. Psychological morbidity and health‐related quality of life of patients assessed on a chest pain observation unit. Ann Emerg Med 200138369–376. [DOI] [PubMed] [Google Scholar]
- 19.Goodacre S, Nicholl J. A randomised controlled trial to measure the effect of chest pain unit care upon anxiety, depression, and health‐related quality of life. Health Qual Life Outcomes 2004239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Price J R, Mayou R A, Bass C M.et al Developing a rapid access chest pain clinic: qualitative studies of patients' needs and experiences. J Psychosom Res 200559237–246. [DOI] [PubMed] [Google Scholar]
- 21.Salmon P, Peters S, Stanley I. Patient's perceptions of medical explanations for somatisation disorders: qualitative analysis. BMJ 1999318372–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balint M.The doctor, his patient and the illness. London: Pitman Medical, 1964
- 23.McDonald I G, Daly J, Jelinek V M.et al Opening Pandora's box: the unpredictability of reassurance by a normal test result. BMJ 1996313329–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dowrick C F, Ring A, Humphris G M.et al Normalisation of unexplained symptoms by general practitioners: a functional typology. Br J Gen Pract 200454165–170. [PMC free article] [PubMed] [Google Scholar]
- 25.Goldberg D P, Gask L, O'Dowd T. The treatment of somatisation: teaching techniques of reattribution. J Psychosom Res 198933689–695. [DOI] [PubMed] [Google Scholar]
- 26.Gask L. Management in primary care. In: Mayou R, Bass C, Sharpe M, eds. Treatment of functional somatic symptoms. Oxford: Oxford University Press, 1995396–399.
- 27.Morriss R K, Gask L, Ronalds C.et al Clinical and patient satisfaction outcomes of a new treatment for somatised mental disorder taught to general practitioners. Br J Gen Pract 199949263–267. [PMC free article] [PubMed] [Google Scholar]
- 28.Drucquer M, Hutchinson S.The consultation toolkit. Sutton: Reed Healthcare Publishing, 2000
- 29.Peveler R, Carson A, Rodin G. Depression in medical patients. In: Mayou R, Sharpe M, Carson A, eds. The ABC of psychological medicine. London: BMJ Books, 200310–13.
- 30.House A, Stark D. Anxiety in medical patients. In: Mayou R, Sharpe M, Carson A, eds. The ABC of psychological medicine. London: BMJ Books, 200314–16.
- 31.Bass C, May S. Chronic multiple functional somatic symptoms. In: Mayou R, Sharpe M, Carson A, eds. The ABC of psychological medicine. London: BMJ Books, 200321–24.
- 32.Asher R. Munchausen's syndrome. Lancet 19511339–341. [DOI] [PubMed] [Google Scholar]
- 33.Krahn L E, Hongzhe L, O'Connor M C. Patients who strive to be ill: factitious disorder with physical symptoms. Am J Psychiatry 2003160(6)1163–1168. [DOI] [PubMed] [Google Scholar]
- 34.Reich P, Gottfried L A. Factitious disorder in a teaching hospital. Ann Intern Med 198399240–247. [DOI] [PubMed] [Google Scholar]
- 35.Powell R, Boast N. The million dollar man. Resource implications for chronic Munchausen's syndrome. Br J Psychiatry 1993162253–256. [DOI] [PubMed] [Google Scholar]
- 36.Bass C, Murphy M. Somatisation, somatoform disorders and factitious illness. In: Guthrie E, Creed F, eds. Seminars in liaison psychiatry. London: Gaskell, 1996150