Abstract
Aims
This study compared rates of self harm among victims of domestic assault presenting to an emergency department (ED) with those rates among other ED patients. It also explored the temporal and numeric relation between domestic assaults and self harm.
Methods
A retrospective matched cohort study was conducted using the medical records of a single ED. The cases were patients who had presented to the ED as a consequence of domestic assault. Two control groups matched for age, sex, and Cambridge postcode were randomly generated from the ED patient list. The second control group cases were also matched for postcode sector as a surrogate approximate for socioeconomic status in addition to age and sex. Cases and controls were followed up between November 1996 and 1 October 2004 documenting the number and timing of episodes of self harm reported in the study period.
Results
Altogether, 294 cases and 558 controls were followed up. Patients suffering domestic assault were more likely to present with self harm than controls (RR 3.6 95% CI 2.1–6.5). This effect appeared to be independent of deprivation. Patients suffering domestic assault had more ED contacts than controls. There was a moderate correlation between the number of episodes of self harm and number of assaults (Spearman's rho 0.3 p<0.001). Socioeconomic status was a poor predictor of self harm. Emergency physicians should consider asking about suicidal ideation in victims of domestic assault.
Keywords: domestic violence, overdose, self harm, suicidality
Previous work has demonstrated an extremely strong association between domestic violence and harm.1 Women who report domestic violence are more likely to report depression than non abused women. The majority of these studies are compromised by recall bias. It is not known, however, whether domestic violence is a causative factor in self harm. Although this is plausible, and the association persists in different study designs, the factors that would strengthen the basis for a causal relationship—namely temporality, dose response, specificity, and interventional effects—have not been demonstrated.2 Self harm is a leading cause of emergency department (ED) attendance and hospital admission, and identifying its precipitating factors may lead to interventions and strategies to reduce this burden.
The study was designed to estimate whether an association between domestic assault and self harm was present in our ED population, whether increasing numbers of violence episodes were associated with higher numbers of self harm episodes, whether there was a temporal relation between domestic violence and self harm, and whether domestic violence was associated with increased ED attendances. This information would have practical utility as well as helping to establish causal pathways.
Methods
A retrospective matched cohort study was conducted using medical records at an ED. Cases were identified using those from a previous study conducted in 20003 and from a routine computer code introduced in 2001. These were cases presenting to the ED as a direct consequence of domestic violence. The study definition of a case was illness or injury as a direct consequence of the intentional actions of partner or family member. Two senior emergency physicians reviewed all the cases and intra‐observer reliability was good (κ = 0.8). For each case, two controls were obtained, using computer generated random matching. The first control group was matched for age, and month and year of presentation. The second control group was additionally matched for postcode sector. This attempted to exclude socioeconomic deprivation as a variable between the groups. Increasing socioeconomic deprivation is an important confounder for the association between self harm and domestic violence. The ED records for both cases and controls were then followed up for the period between November 1996 and October 2004.
The primary outcome measure was presentation to the ED with self harm—either poisoning or mutilation. Two senior emergency physicians reviewed a random sample of these cases and intra‐observer reliability was perfect (κ = 1.0). The Index of Multiple deprivation was assessed ecologically using the subject's postcode. A high score indicates increased deprivation. Person years of follow up were identified using the hospital computer to identify the first and last recorded contact with the hospital for all reasons, not just ED attendances. Subjects who had attended only once were awarded one day of follow up. Cases were excluded before matching if they were under 16 years of age at initial presentation4 or had an address that indicated that they lived out of the hospital catchment area (51 cases).
There was no pilot data on which to base a sample size calculation on. A retrospective sample size calculation demonstrated the study to have a 77% power for detecting a doubling of relative risk. χ2, McNemar's, and Fisher's exact tests were used for bivariate tests where appropriate, relative risks were calculated using a Poisson model, and conditional logistic regression was used for multivariate analysis. Conditional logistic regression does not allow for differing person years between groups and the consequent odds ratio is larger than the estimate from the Poisson model. The local ethics and research committee approved this project.
Results
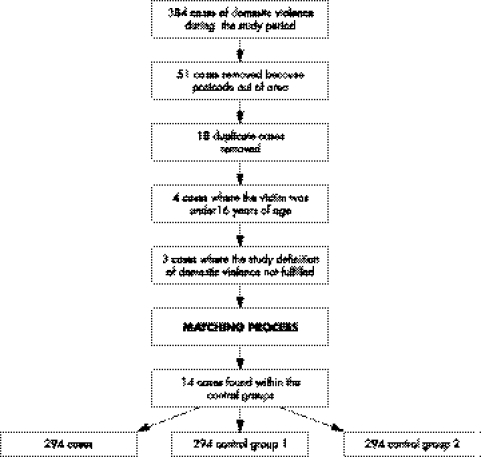
The matching process is shown in fig 1.
Figure 1 Generating the lists of cases and controls.
The proportions of missing data were the same in all three groups—8.5%. The characteristics of the study sample are shown in Table 1. As expected, the majority of domestic assault victims were young women.
Table 1 Characteristics of the two control groups and the cases.
| Cases/294 | Control group 1/294 | Control group 2/294 | |
|---|---|---|---|
| Mean age (SD) | 34.2 (13.3) | 34.2 (13.3) | 34.2 (13.3) |
| Men/women | 78/216 | 78/216 | 78/216 |
| Quintile 1 (least deprived) n (%) | 74 (25.2) | 113 (38.4) | 94 (32.0) |
| Quintile 2 n (%) | 136 (46.2) | 152 (51.7) | 145 (49.3) |
| Quintile 3 n (%) | 8 (2.7) | 5 (1.7) | 8 (2.7) |
| Quintile 4 n (%) | 55 (18.7) | 21 (7.1) | 32 (10.9) |
| Quintile 5 (most deprived) n (%) | 21 (7.1) | 3 (1.0) | 15 (5.1) |
| Mean index of deprivation score (SD) | 15.2 (9.9) | 10.7 (6.6) | 12.9 (8.7) |
Controls in group 1 scored less highly on the index of multiple deprivation—this difference was statistically significant (Fisher's exact test p< 0.01). Controls in group 2 were also less deprived than cases but this difference was not statistically significant (χ2 (4df) = 9.75, p = 0.05). Table 2 shows the relative risks of self harm between the two control groups and the cases. Table 3 shows the multivariate analysis.
Table 2 Relative risks of self harm between the two control groups and the cases.
| Domestic violence victims/294 | Incidence rate/1000 person years | Control Group 1/294 | Incidence rate/1000 person years | Rate ratio (95% CI) | Control group 2/294 | Incidence rate/1000 person years | Rate ratio (95% CI) | |
|---|---|---|---|---|---|---|---|---|
| Self harmed in the study period | 75 | 47 | 17 | 13 | 3.6 (2.1–6.5) | 17 | 13 | 3.5 (2.1–6.4) |
| Episodes of self harm | 160 | 101 | 30 | 39 | ||||
| Patient episodes at ED | 552 | 394 | 356 | 276 | 1.3 (1.1–1.4) | 361 | 285 | 1.2 (1.1–1.4) |
| Number of ED attendances per subject in the study period | 1.87 | 1.21 | 1.23 | |||||
| Number of deaths in the study period | 0 | 0 | 4* | 7.4 | N/A | 1 * | 2 | N/A |
*None of the deaths were because of suicide or domestic violence. ED, emergency department; N/A, not applicable.
Table 3 Multivariate analysis.
| Variable | Control group 1 | Control group 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | Standard error | z | p>z | Odds ratio (95% CI) | Standard error | z | p>z | |
| Previous domestic violence | 5.9 (3.0–11.6) | 2.0 | 5.2 | 0.0 | 6.1 (3.2–11.6) | 2.01 | 5.5 | <0.01 |
| Lower index of multiple deprivation | 0.8 (0.3–1.9) | 0.4 | −0.4 | 0.7 | 2.2 (0.9–5.4) | 1.0 | 1.7 | 0.1 |
The temporal relation between self harm and domestic assault was examined. For this purpose the two control groups were combined. For the control groups, the index group was defined as the presentation that led to matching. For cases, the index presentation was taken as the first time that they presented with domestic assault. We did not demonstrate a temporal association between self harm and domestic assault presentation at the ED (see Table 4).
Table 4 The temporal association between domestic assault and self harm.
| Reporting deliberate self harm before the index presentation | Reporting deliberate self harm after the index presentation | Total | |
|---|---|---|---|
| Domestic assault | 46 | 29 | 74 |
| No domestic assault | 15 | 19 | 34 |
| 61 | 48 | 108 |
χ2 = 2.81 (1df), p = 0.09
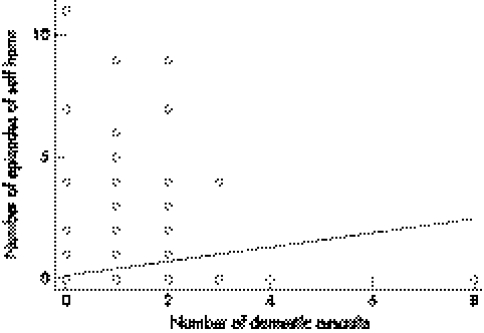
Increasing episodes of domestic assault were positively and significantly correlated with increasing episodes of self harm at the ED (see fig 2) (Spearman's rho 0.3, p<0.01).
Figure 2 Association between number of assaults and number of episodes of self harm.
Discussion
The results prove that medically recorded domestic violence is significantly associated with an increased risk of self harm, as nearly 25% of domestic assault victims self harmed in the study period. This is the first time that this has been shown in the United Kingdom ED population. Victims of domestic assault have increased rates of ED use compared with controls. A temporal relation between domestic violence and self harm was not confirmed. We demonstrated a moderate correlation between the number of episodes of self harm and the number of domestic assaults. This is the first time that this quantitative relationship has been demonstrated. This relationship provides further evidence towards a causal pathway, although this remains unproven.
The strength of the association is weaker than that identified in similar Swedish studies.4,5 This can be explained by the different nature of the controls, as Bergman and Brismar's study controls were recruited from a population register whereas ours were recruited from the ED patient log. Assault victims of all causes are known to have higher rates of all forms of medical and psychiatric care.6 They differ from domestic assault victims in important ways: they are more likely to be male and many community assault victims may have initiated the assault and are less likely to come into contact with the perpetrator again. Indeed, physical assault is regarded as only a part of a much wider pattern of coercive behaviours in an abusive relationship.
The absence of evidence of a temporal relation between domestic violence and self harm should be viewed in context. Domestic violence is frequently hidden and it is estimated that a woman will suffer, on average, 35 episodes of abuse before seeking help from the police.7 This suggests that most of the sufferers of domestic violence in this sample had almost certainly suffered several episodes of violence before presenting to the ED.
Our results suggest that domestic assault patients should be asked about suicidal ideation and depression. Conversely, our results do not suggest that every self harm patient should be asked about domestic violence. Our department sees around 800 self harm patients a year; we identified 160 episodes of self harm over an 8 year period. It is not clear from this study or other literature how many of these are in abusive relationships. However, at least 5% of self harm patients will have suffered domestic violence in the year before presentation and this rate is probably higher in this group. Routinely inquiring (as opposed to screening) about domestic violence has been advocated for certain high risk groups.8 Self harm patients may be a group that might benefit from inquiry about domestic violence as part of their psychological assessment. Though asking about domestic violence and subsequent referral to agencies has not been proven to reduce violence, this is likely to be because of absence of evidence rather than absence of effect.
Limitations
Our patients were closely matched and this may have lead to overmatching. At least 5% of the controls will have suffered domestic assault in the year preceding their visit.1,9 The effect of this bias would be to decrease the strength of the association. Our study could not adjust for mental illness and this may confound the association between self harm and domestic violence. The gradients that we have demonstrated may be because of a confounding effect of increasingly severe mental illness. Matching prevented us examining the effect of sex. Our ecological method of examining multiple deprivation was too weak to demonstrate an effect.
Conclusions
Domestic assault victims have much greater risks of self harm than other ED patients. Multiple episodes of violence are associated with increasing episodes of self harm. We recommend that patients presenting with domestic assault should be asked about depression and suicidal ideation.
Abbreviations
ED - emergency department
Footnotes
Funding: supported by a NHS Health Services Research Fellowship.
Competing interests: none declared.
References
- 1.Boyle A A, Todd C J. Domestic violence in a UK emergency department: an incidence and prevalence survey. EMJ 200320438–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Golding J M. Intimate partner violence as a risk factor for mental disorders: a meta‐analysis. J Fam Violence 199914(2)99–132. [Google Scholar]
- 3.Boyle A A, Kirkbride J, Jones P B. Capture/recapture techniques applied to domestic violence victims at the police and the emergency department. J Epidemiol Community Health 59909–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bergman B, Brismar B. A 5‐year follow‐up study of 117 battered women. Am J Public Health 199181(11)1486–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bergman B, Brismar B. Suicide attempts by battered wives. Acta Psychiatr Scand 199183380–384. [DOI] [PubMed] [Google Scholar]
- 6.Shepherd J, Peak J D, Haria S.et al Characteristic illness behaviour in assault patients: DATES syndrome. J R Soc Med 19958885–87. [PMC free article] [PubMed] [Google Scholar]
- 7.Yearnshire S.Analysis of cohort data. In: Bewley S, Friend J, Mezey G, eds. Violence against women. London: Royal College of Obstetricians and Gynaecologists, 199745
- 8.Taket A, Nurse J, Smith K, Watson J.et al Routinely asking women about domestic violence in health settings. BMJ 2003327673–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mirrlees‐Black C. Domestic violence: findings from a new British crime survey self completion questionnaire. Home Office Publications 19991–136.