Abstract
Introduction
In 1999, the UK adopted a policy of using TOXBASE, an internet service available free to registered National Health Service (NHS) departments and professionals, as the first point of information on poisoning. This was the first use worldwide of the internet for provision of clinical advice at a national level. We report the impact on database usage and NPIS telephone call loads.
Methods
Trends in the pattern of TOXBASE usage from 2000–2004 are reported by user category. Information on the monographs accessed most frequently was also extracted from the webserver and sorted by user category. The numbers of telephone calls to the National Poisons Information Service (NPIS) were extracted from NPIS annual reports.
Results
Numbers of database logons increased 3.5 fold from 102 352 in 2000 to 368 079 in 2004, with a total of 789 295 accesses to product monographs in 2004. Registered users increased almost tenfold, with approximately half accessing the database at least once a year. Telephone calls to the NPIS dropped by over half. Total contacts with NPIS (web and telephone) increased 50%. Major users in 2004 were hospital emergency departments (60.5% of logons) and NHS public access helplines (NHS Direct and NHS24) (29.4%). Different user groups access different parts of the database. Emergency departments access printable fact sheets for about 10% of monographs they access.
Conclusion
Provision of poisons information by the internet has been successful in reducing NPIS call loads. Provision of basic poisons information by this method appears to be acceptable to different professional groups, and to be effective in reducing telephone call loads and increasing service cost effectiveness.
Keywords: Internet, database, poisons
In 1999, the UK adopted a policy that the first point of contact for poisons information for health professionals in the UK should be TOXBASE, the computer database of the UK National Poisons Information Service (NPIS).1 This followed a Department of Health review of the NPIS in 1997–98. This move to change the way in which poisons information for a whole country is produced and reviewed was, in 1998, unique to the UK. The NPIS has provided poisons information to medical professionals since 1963 by telephone, and since 1983 directly from TOXBASE, which was transferred to the internet in 1999 following the decision to adopt the new policy.
The TOXBASE database contains information on approximately 12 000 products, together with generic advice on the management of poisoning and other toxicity related monographs. It is available free of charge to registered UK National Health Service users. NPIS centres in the UK also promoted the site to telephone enquirers. Use of TOXBASE is endorsed by the National Institute for Clinical Excellence (NICE) guidance on self harm.2 There is also a contract with Ireland, which allows access to TOXBASE by Irish emergency departments and facilitates the inclusion of Irish products to the database. Other suitable applicants (such as pharmaceutical companies) may be granted access for an annual fee.
In addition, the NPIS continues to have a single 24 hour telephone advice line (0870 600 6266) staffed by trained poisons information specialists with 24 hour consultant clinical toxicologist availability. The latter service provides for direct discussion of complicated cases by senior clinicians managing poisoned patients.
All new entries on the database since 1999 are both authored by NPIS centres, and reviewed and agreed by the directors of those centres. Entries are structured in an agreed format and designed to provide front line National Health Service (NHS) staff with up to date advice on managing cases of poisoning.
We have previously reported on the first few months of operation of TOXBASE on the internet.3,4 We now report the impact of the 1998 NHS policy change on database usage and the impact on NPIS telephone call loads over the first 5 years. We also illustrate how different types of registered users access topics in the database.
METHODS
The server that hosts the database allows all logons to the site to be identified with respect to registered user identity (coded by user category), time of access, and monographs accessed during any session of database usage.
For simplicity, we grouped users into five categories: emergency departments, other hospital departments, primary care, public health telephone services (NHS Direct and NHS24) and others. We excluded NPIS own use from this analysis.
Using the data collected, we examined registrations for access to the system, database accesses overall, and by user type. Data are presented in an aggregate descriptive format, and formal statistical analyses have not been performed. To access the database. users require login access codes. When provided, details of user profile are created and user activity monitored. Database users are regarded as “active” if they access the database in a given period. Data for TOXBASE accesses have been analysed by time period, either quarterly or annually by calendar year.
Details of telephone calls to the NPIS are collected by individual NPIS centres, and amalgamated for publication in the NPIS annual report. In 2004, the Health Protection Agency requested the annual report be produced by financial rather than calendar year; telephone data for the period April 2004 to March 2005 are therefore presented for illustrative purposes.
RESULTS
Users and usage
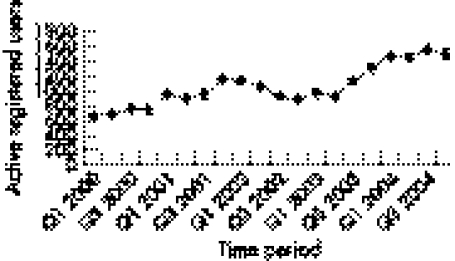
When TOXBASE was transferred to the internet in September 1999, there were 568 registered users after 15 years of operation of the previous Viewdata system. The majority of users were hospital emergency departments. The UK public health advice telephone lines (NHS Direct in England and Wales, and NHS24 in Scotland) were in their infancy, and a significant part of the increase in activity has been due to this development. By the end of 2004, there were 5229 registered users of TOXBASE. The majority are now hospital departments or public access call centres, rather than individual medical professionals. However, not all regularly access the database, thus 2547 different users had accessed the system in 2004. Quarterly “active” users increased from 690 in the first quarter of 2000 to 1519 at the end of 2004 (fig 1). Normal policy is that user accesses are reviewed, and those inactive for 2 years are removed.
Figure 1 Registered users of TOXBASE accessing the database by quarter, 2000–2004.
When TOXBASE moved online in late 1999, major users (as measured by number of logons) were emergency departments, who were responsible for than 80% of logons. During 2000 and 2001 there was an increase in use by the public access, nurse led, telephone health enquiry services in England and Wales (NHS Direct) and from 2002 in Scotland (NHS 24). Since 2002, the proportion of types of user has remained stable, with emergency departments accounting for approximately 60% and public access around 29% (table 1). Other hospital departments account for approximately 7% of use. The remainder is principally by GPs and for educational purposes.
Table 1 Percentage usage (logons) to TOXBASE by user category, 2000–2004.
| Category | 2000 | 2001 | 2002 | 2003 | 2004 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Emergency departments | 82.4 | 65.1 | 59.6 | 61.4 | 60.5 | |||||
| Other hospital departments | 7.8 | 8.4 | 7.3 | 7.4 | 7.9 | |||||
| GPs | 1.5 | 1.1 | 0.7 | 0.6 | 0.7 | |||||
| Public access services | 7.2 | 24.6 | 31.4 | 29.6 | 29.4 | |||||
| Other | 1.0 | 0.9 | 0.9 | 1.0 | 1.5 |
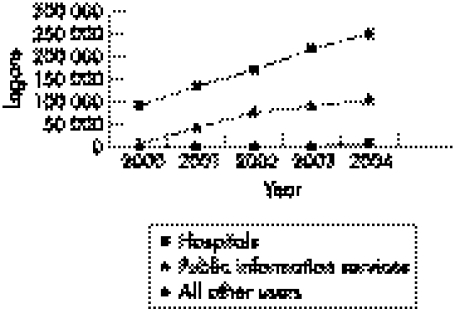
The total number of logons by user type is shown in fig 2, with a steady rise from a total of 102 352 in 2000 to 368 079 in 2004. The average number of products accessed in each usage session rose from 1.5 in 2000 to 2.1 in 2004.
Figure 2 Database activity: logons (usage session) by user type 2000–2004.
Impact on NPIS activity
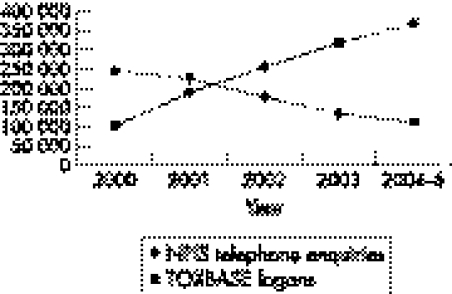
The expansion in use of TOXBASE has led to a drop in the number of telephone enquiries requiring input from the NPIS telephone service. In 2000, there were 248 575 calls, and by the financial year 2004–5 this had declined to a more manageable 113 125, in line with Department of Health policy to make TOXBASE the first line for information for managing poisoned patients (fig 3).
Figure 3 NPIS telephone enquiries and TOXBASE logons. Data are presented by calendar year, apart from 2004–5, which are presented by financial year (see text).
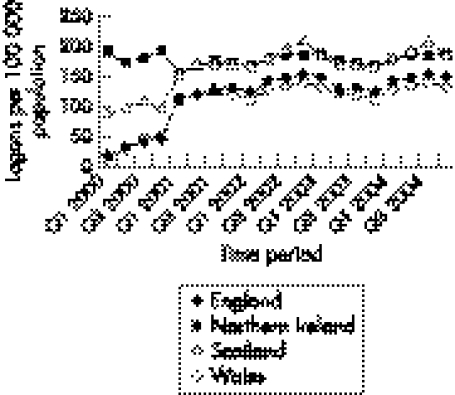
In 1999 when TOXBASE was placed on the internet, most of the usage came from Northern Ireland and Scotland, where the former Viewdata system had been promoted. There has been increasing use in England and Wales, so that population based figures are now much closer for all four countries (fig 4). The majority of accesses are made from the UK and Channel Islands, with 2% coming from Ireland and <1% from overseas (mainly British armed forces and fee paying overseas users).
Figure 4 Logons to TOXBASE by quarter expressed per 100 000 population by country, 2000–2004.
Products and items
The most common products accessed in 2000 and 2004 by emergency departments are shown in table 2. Five of the top 10 monographs are identical in the two lists (paracetamol, diazepam, ibuprofen, aspirin, and zopiclone), and all the top items were pharmaceuticals.
Table 2 Most frequent product monograph accesses and numbers in 2000 and 2004 by EDs .
| Product and year | No. of accesses | |
|---|---|---|
| 2000 | ||
| Paracetamol | 9058 | |
| Co‐proxamol | 3062 | |
| Diazepam | 2879 | |
| Aspirin | 2410 | |
| Ibuprofen | 2363 | |
| Zopiclone | 2237 | |
| Co‐codamol | 2136 | |
| Anadin extra | 2094 | |
| Karvol decongestant capsules | 2058 | |
| Olbas oil | 1904 | |
| 2004 | ||
| Paracetamol | 21445 | |
| Diazepam | 11324 | |
| Ibuprofen | 10786 | |
| Zopiclone | 10159 | |
| Aspirin | 7893 | |
| Fluoxetine | 7031 | |
| Venlafaxine | 7004 | |
| Amitriptyline | 6731 | |
| Citalopram | 6718 | |
| Ecstasy | 5754 |
Table 3 lists the most frequently accessed products for public access services. Four of the five monographs most frequently accessed by emergency departments were also accessed most frequently by these public health telephone services. TOXBASE enables users to print “fact sheets” in which all relevant advice is linked onto a single printout, which can be used throughout a patient's journey. Emergency departments generate a fact sheet in approximately 10% of product accesses, in contrast to 1.5% of accesses by other users.
Table 3 Most frequent product monograph accesses in 2000 and 2004 by public access telephone health services (NHS Direct and NHS24).
| Product and year | No. of accesses | |
|---|---|---|
| 2000 | ||
| Karvol decongestant capsules | 768 | |
| Paracetamol | 535 | |
| Sudocrem antiseptic healing cream | 405 | |
| Olbas oil | 399 | |
| Paint | 240 | |
| Ibuprofen | 192 | |
| Karvol decongestant drops | 168 | |
| Perfume | 158 | |
| Bleach: liquid | 156 | |
| Deodorant: aerosol spray | 144 | |
| 2004 | ||
| Paracetamol | 11742 | |
| Ibuprofen | 7583 | |
| Sodium hypochlorite solution | 3130 | |
| Bleach: liquid | 3118 | |
| Sudocrem antiseptic healing cream | 2314 | |
| Calpol infant suspension | 2267 | |
| Aspirin | 2209 | |
| Ethanol | 1822 | |
| Co‐codamol | 1813 | |
| Diazepam | 1805 |
Users from public access telephone services require poisons information to decide on the disposition of their patients. Those in emergency departments require it to triage and manage poisoned patients. Some of the other users, such as pharmacists and those involved in planning for or managing chemical incidents, have different requirements and are primarily interested in different parts of the database. TOXBASE includes a variety of other monographs and pieces of information and the most commonly accessed are the toxic dosage calculator, teratology monographs provided by the National Teratology Information Service, information on eye decontamination, antidotes (doses and sources), general information on paediatric poisoning, oral activated charcoal, and snakes. For example, pharmacists were more interested in antidotes and teratology (table 4). They accessed none of the product monographs as frequently as these items, which is not surprising as they do not, in general, give poisons information. Those involved in emergency planning or managing chemical incidents used the database infrequently but their most common accesses were biological and chemical release, antidotes, and decontamination and the most common products accessed were chlorine, arsenic, ammonia, and lead.
Table 4 Monographs most frequently accessed by pharmacists in 2004.
| Item | No. of accesses | |
|---|---|---|
| Antibiotics: use in pregnancy | 1626 | |
| Antidotes: doses and sources | 1472 | |
| Antiemetics: use in pregnancy | 909 | |
| Useful things* | 903 | |
| Fluoxetine in pregnancy | 781 | |
| Paediatric poisoning | 749 | |
| Antidepressants: neonatal withdrawal syndrome | 648 | |
| Household chemicals | 640 | |
| Amitriptyline: use in pregnancy | 541 | |
| Gastrointestinals: use in pregnancy | 541 |
*Units, conversions, calculations and links.
Education
Originally, access to TOXBASE was only granted to medical professionals and not to students, but several requests were received from UK medical schools for access as part of senior medical student courses, and access is now permitted via secure links on university websites. Additionally, an interactive module on how to use TOXBASE has now gone live on a stand alone site with multiple choice questions for two levels of staff: nurse advisors (NHS 24) and triage nurses/junior doctors/medical students in Scotland. This has led to an increase in educational use, and further modules are planned.
DISCUSSION
Poisons information services originated in small hospital departments in the 1950s. The first was in Chicago, and subsequently centres have developed across the world.5 In the UK, the first centres were in major teaching hospitals in the early 1960s, and a national network evolved. A policy decision was made that these centres should only serve health professionals, and between the 1960s and the 1990s the demand for telephone information to aid management of poisoning increased. Despite this demand, funding for the NPIS was based on non‐clinical budgets, and hence ability to recruit more staff to support telephone lines was severely limited. From a cost effectiveness perspective, there was therefore a need to review the way in which poisons information was delivered in the UK. In the early 1980s, a system based on a Viewdata platform was introduced into Scotland and we have previously described how this was converted into an internet based service, which was launched in 1999.3 At the time, this was the first such system in the world, and there was uncertainty as to how readily health professionals would adopt this new technology, and how this would affect the demand for telephone enquiries. Placement of TOXBASE on the internet has allowed us to document the effects of this major public health policy decision.
The situation was further complicated by the launch in England and Wales of the public access telephone health information service, NHS Direct, and later in Scotland, NHS 24. The NPIS recognised that these services would require expert advice on poisoning and its triage in the home. As the services rely on nurse advisers who base their recommendations on computer based algorithms, it seemed logical to add TOXBASE to the suite of information they used. It was also reasoned that this would permit a standard advice structure on poisoning management for the NHS, and hence commonality of treatment approach. In view of the high use of TOXBASE by these services, there seems little doubt that the NPIS would have been overwhelmed without a system such as TOXBASE to support these new services.
Early after launching TOXBASE on the internet questionnaires were used to assess how easily emergency department staff found TOXBASE to use.4 This questionnaire demonstrated that the overall satisfaction rates were high. We were therefore encouraged to continue to promote this system. Further support came from NICE.2
From the data presented in this report it is clear that database usage continues to grow, and has yet to reach a plateau. In 2000, telephone calls exceeded TOXBASE accesses by more than 2.5:1 (fig 3). There has also been a gradual and steady reduction in telephone enquiries with an increase in TOXBASE usage, such that by 2004 TOXBASE usage was almost four times the number of telephone enquiries. Furthermore, total NPIS contacts, of telephone and TOXBASE together, have increased by 50%. We have previously reported that in Scotland such a change was associated with an increase in the complexity of referral by telephone.6 Our conclusion at that time was that clinical staff were using the systems available to them in a logical manner, and using the telephone selectively to discuss more unusual or complex cases. Even with a database of the size available on TOXBASE there will always be occasional enquiries for which a monograph has not been written. NPIS experience suggests that this is a rare occurrence, accounting for less than 5% of telephone enquiries.
It is also possible to calculate from the current database usage the number of monographs necessary to answer any specific proportion of overall monograph access. Thus in the UK, 1000 pharmaceutical monographs would be enough to answer 98% of pharmaceutical enquiries. With this information, editorial activity can be focused on the commonly used monographs. Users of TOXBASE have a facility to respond by e‐mail to comment on individual monographs; however, less than 0.01% of user accesses result in such feedback.
One disadvantage of an internet based system is that detailed clinical data on specific cases can less readily be collected. It is important to remember that such information is of use in surveying the safety of household products, chemicals such as pesticides, and pharmaceuticals taken in overdose. TOXBASE offers the facility for feedback, but this is relatively infrequently provided. As a result, focused surveillance activities were introduced in April 2004 for pesticide exposures.7 Users are also encouraged to report exposures to new drugs, exposures in pregnancy (to the National Teratology Information Service), and adverse effects of veterinary medicines (to the Veterinary Medicine Directorate).
Since TOXBASE was launched, a similar online system has been introduced in New Zealand.8 The very positive response of healthcare professionals in a number of settings to structured online advice for poison management suggests that this method of delivery for peer reviewed clinical management protocols would also work in other settings.
In conclusion, the acceptance and usage of TOXBASE in the UK, particularly by hospital emergency departments, illustrates the potential for the internet to be used to deliver up to date information for use by front line services. The necessity for a telephone response system is not removed, but these data indicate that such services can be used more cost effectively to answer enquiries about rare and more serious poisonings.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the support of the other centres of the NPIS in the support and maintenance of TOXBASE.
Abbreviations
NHS - National Health Service
NICE - National Institute for Clinical Excellence
NPIS - National Poisons Information Service
Footnotes
Competing interests: The authors are responsible for the editing and updating of TOXBASE on behalf of the NPIS. Neither has any financial interest in the database, which is funded by the Health Protection Agency on behalf of the NHS as part of its overall NPIS support.
References
- 1.Donaldson L. Information from the National Poisons Information Service. CMOs Update London: Department of Health, 2000253 [Google Scholar]
- 2.National Institute for Clinical Excellence Guidance on self harm. www.nice.org.uk/pdf/CG016NICEguideline.pdf
- 3.Bateman D N, Good A M, Kelly C A.et al Web based information on clinical toxicology for the United Kingdom: uptake and utilization of TOXBASE in 2000. Br J Clin Pharmacol 2002543–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bateman D N, Good A M, Laing W J.et al TOXBASE: poisons information on the internet. Emerg Med J 20021931–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krenzelok E P. Poison centers at the millennium and beyond. J Toxicol Clin Toxicol 200038693–696. [DOI] [PubMed] [Google Scholar]
- 6.Laing W J, Good A M, Bateman D N. Impact of an internet poisons database on the nature of telephone enquiries to a poisons unit. J Toxicol Clin Toxicol 200442451–452. [Google Scholar]
- 7.Good A M, Adams R A, Bateman D N. Pesticide surveillance using poisons telephone service and TOXBASE, an internet database ‐ first 6 months of a pilot project. Clin Tox 200543455–456. [Google Scholar]
- 8.Fountain J S, Reith D M, Watts M. Comparison of CD‐rom and internet access to clinical information. Int J Med Inform 200574769–777. [DOI] [PubMed] [Google Scholar]