Abstract
Background
The purpose of this study was to evaluate the usefulness of a particular magnetic resonance imaging technique known as primary diffusion weighted imaging (DWI) for patients with lacunar syndrome in the emergency department (ED).
Methods
Patients with one of five classic lacunar syndromes underwent DWI as primary imaging modality. The DWI findings were classified into groups: (a) having a lesion with high signal intensity, (b) having a lesion with mixed signal intensity, and (c) unremarkable. The final clinical diagnoses were extracted from the patients' medical records, and used as a reference standard.
Results
Of 151 DWI images, 120 (79%) were interpreted as high signal lesions, 21 (14%) as mixed signal lesions, and 10 (7%) as unremarkable. All patients with high signal lesions or unremarkable findings were diagnosed with ischaemic stroke. The patients with mixed signal lesions were diagnosed with haemorrhagic stroke with an exception of one ischaemic stroke.
Conclusion
Primary DWI is a feasible and useful neuroimaging tool for patients with lacunar syndrome in the ED.
Keywords: Diffusion magnetic resonance imaging, cerebrovascular accident
A non‐contrast computed tomography (CT) scan is the standard method to diagnose stroke, with door to CT scan time usually being <25 minutes for potential fibrinolytic cases.1 CT scans can show negative results in acute ischaemic stroke patients, however, more advanced diagnostic studies are frequently performed after the CT scan.
About 20% of first time stroke patients have a lacunar stroke, with a relatively good prognosis.2 The five classic lacunar syndromes, established by Fisher, are pure motor stroke (PMS), ataxic hemiparesis (AH), dysarthria clumsy hand syndrome (DCH), sensorimotor stroke (SMS), and pure sensory stroke (PSS).3 Clinical lacunar syndromes are highly predictive for a small infarct.4 About 7% of intracerebral haemorrhages also present with lacunar syndrome, while haemorrhagic lacunar stroke accounts for 3.8% of lacunar syndromes.5 It is difficult to clinically differentiate infarction from haemorrhage in patients with lacunar syndrome. Moreover, it is difficult to clinically estimate the location of a stroke lesion.
Although the CT scan is more sensitive in excluding a haemorrhage, a newer magnetic resonance imaging technique, diffusion weighted imaging (DWI), is very sensitive to hyperacute ischaemic stroke and intracerebral haemorrhages.6,7,8 CT angiography source images have been found to be comparable with magnetic resonance imaging (MRI) for acute ischaemic stroke, while small lacunar infarctions were only visible by initial DWI.9 Therefore, it is reasonable to use DWI as a primary imaging method for patients with lacunar syndrome.
We performed primary DWI in the emergency department (ED) on patients with lacunar syndrome. The purpose of this study was to evaluate the usefulness of primary DWI in diagnosing lacunar syndrome.
METHODS
Study design
This was a prospective observational study of patients receiving DWI after presenting to the ED with lacunar syndrome. The study was reviewed and approved by the institutional review board.
Study setting and population
The study was conducted in an urban teaching hospital ED with an emergency medicine residency programme. The ED has approximately 35 000 visits per year, most of whom are East Asian patients. Patients diagnosed by the attending emergency physicians as having one of the five classic lacunar syndromes were enrolled in the study. PMS was defined as a unilateral motor deficit involving at least two of three possible areas (face, arm, and leg); PSS as any unilateral pure sensory deficit; SMS as any unilateral motor and sensory deficit; DCH as dysarthria combined with clumsiness and slowed fine movement in one hand; and AH as unilateral ataxia accompanied by motor deficit. We classified PMS and AH into the same category because hemiparesis often results in uncoordinated movement. As such, they are sometimes difficult to differentiate clinically.10
Patients were excluded based on several criteria. The first criterion was having a symptom duration <3 hours or >48 hours. Patients with a symptom duration <3 hours received a CT scan first, following standard evaluation protocol. Patients with a duration >48 hours also received the primary CT protocol, owing to a high probability of detecting lesions with a CT scan. The second exclusion criteria was presenting with additional cortical symptoms such as aphasia or neglect. Patients with suspected transient ischaemic attack also presented with lacunar syndrome, but their symptoms were improving prior to imaging and thus were excluded. Finally, patients who were unwilling to participate or had a contraindication for MRI such as pacemaker, intracranial metallic fragment, or claustrophobia were excluded. This study took place between July 2002 and June 2004.
Study protocol
The department of emergency medicine, neurology, and neuroradiology formally agreed that DWI be instituted as the first line neuroimaging for patients with suspected acute lacunar syndrome prior to the start of the study. All patients underwent limited MRI confined to a diffusion weighted sequence on a 1.5 Tesla whole body scanner (GE Signa, General Electric) with echo planar imaging data acquisition capability (Advanced NMR Systems) designed to obtain rapid images. DWI was obtained as soon as possible after informed consent was given. The pulse sequence for DWI was a single shot, spin echo sequence with an echo time of 71.8 ms, a 128×128 matrix, a 200–240 mm field of view, and 5 mm slice thickness with no gap between the 20 sections covering the whole brain. The two b values were 0 and 1000 s/mm2. Apparent diffusion coefficient maps were not routinely acquired.
A neuroradiologist blinded to the clinical information interpreted the DWI films. If necessary, the patient underwent further diagnostic studies following neurology department protocol. The final clinical diagnoses were extracted from the patient's medical records, and used as a reference standard. These diagnoses were based on clinical assessment and neuroimaging without an attempt to blind the neurologist to the DWI results.
Data analysis
The DWI findings were classified into groups: (a) having a lesion with high signal intensity, (b) having a lesion with mixed signal intensity, and (c) unremarkable. Anything without a high or mixed signal intensity, such as inconclusive faint signals, was considered unremarkable. The lesions with high and mixed signals were considered to be acute ischaemic and haemorrhagic stroke, respectively.
Demographic data and time intervals of examinations were given as mean values with SD. For statistical analysis we used the Mann‐Whitney U test and χ2 test to determine whether there were significant differences in time interval and demographic data between unremarkable and DWI positive groups, using SPSS software (SPSS Inc, Chicago, IL, USA).
RESULTS
Patients
Data were collected from 212 patients with lacunar syndrome over the 2 year period. Of these, 61 patients were excluded. The reasons for exclusion were: symptom duration <3 hours (5 patients) or >48 hours (25), additional cortical symptoms (9), improving symptoms (5), refusal to consent to MRI (13), and equipment failure (4). One patient visited twice during the period. Therefore, 151 lacunar syndromes from 150 patients were analysed.
The mean (SD) age was 64.9 (10.7) years (range 27 to 91), comprising 96 men and 54 women (sex ratio 1.8:1). Of the 151 lacunar syndromes classified, 94 (62%) were PMS/AH, 35 (23%) SMS, 17 (11%) DCH, and 5 (3%) PSS. Final diagnosis was ischaemic stroke for 131 patients and haemorrhagic stroke for 20 (table 1).
Table 1 Final diagnoses and DWI findings according to type of lacunar syndrome.
| Lacunar syndrome | Total (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| PMS/AH | SMS | DCH | PSS | ||||||||
| Diagnosis | |||||||||||
| Ischaemic stroke | 81 | 28 | 17 | 5 | 131 (87) | ||||||
| Haemorrhagic stroke | 13 | 7 | 0 | 0 | 20 (13) | ||||||
| DWI finding | |||||||||||
| High signal intensity | 76 | 22 | 17 | 5 | 120 (79) | ||||||
| Mixed signal intensity | 13 | 8 | 0 | 0 | 21 (14) | ||||||
| Unremarkable | 5 | 5 | 0 | 0 | 10 (7) | ||||||
| Total (%) | 94 (62) | 35 (24) | 17 (11) | 5 (3) | 151 | ||||||
DWI, diffusion weighted imaging; PMS, pure motor stroke; AH, ataxic hemiparesis; SMS, sensorimotor stroke; DCH, dysarthria clumsy hand syndrome; PSS, pure sensory stroke.
DWI diagnoses
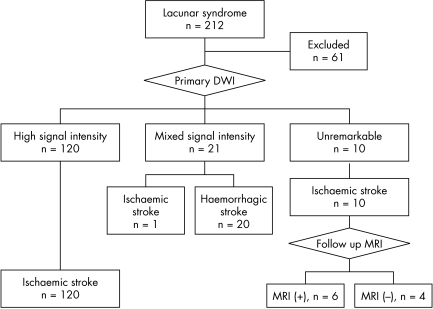
From 151 DWI images, 120 were interpreted as high signal lesions, 21 mixed signal lesions, and 10 unremarkable. All patients with high signal lesions or unremarkable findings were diagnosed with ischaemic stroke. The patients with mixed signal lesions were diagnosed with haemorrhagic stroke with an exception of one ischaemic stroke. The results of DWI and final diagnoses were displayed using an algorithm (fig 1).
Figure 1 The final diagnoses of the patients are shown according to DWI findings.
There were no differences in time interval from symptom onset to MRI between unremarkable (19.4 (13.6) hours) and positive (16.2 (14.6) hours) MRI groups. There were also no differences in age (65.6 (13.9) years), sex (six men, four women). or lesion subtype (five PMH, five SMS).
DISCUSSION
Lacunar syndrome usually suggests a lacunar infarct, defined as a small deep infarct with a maximum diameter of 15 mm. In this study, 87% of the patients with lacunar syndrome had lacunar infarcts, and all others had a small haemorrhagic stroke. PMS/AH was the most abundant lacunar syndrome, followed by SMS, DCH, and PSS, in that order. These frequencies are consistent with other reports.11
In patients with lacunar syndrome, routine CT scans were only positive in 30–50% of cases.2,12 MRI has been considered a redundant test for lacunar syndrome when a CT scan excludes non‐ischaemic causes of stroke.4 Using a rapid echoplanar technique allows examination times comparable to CT, thus making MRI a feasible alternative in routine practice when the study is confined to a diffusion weighted sequence. In this study, primary DWI showed a relevant lesion in 120 of 131 confirmed lacunar infarcts (91.6%). Lai et al showed the sensitivity of DWI for acute lacunar infarcts to be as high as 95%, with specificity 94%, positive predictive value 97%, and negative predictive value 90%.13 Lindgren et al. found that 22 of 23 patients (96%) with clinical lacunar syndromes showed lesions on DWI, consistent with a lacunar infarct.14
Although DWI is known to have a higher sensitivity and specificity for lacunar infarction than a CT scan, false negatives are also reported.15 Our study revealed 10 cases in which the final diagnosis was infarction, but no high signal lesions appeared on DWI. Six of these cases had relevant lesions discovered on a follow up MRI. The remaining four patients also obtained unremarkable findings on the follow up MRI. Their final diagnoses were made according to persistent clinical findings. One possible explanation for false negatives is that the lacune size is too small to cut with a DWI slice.
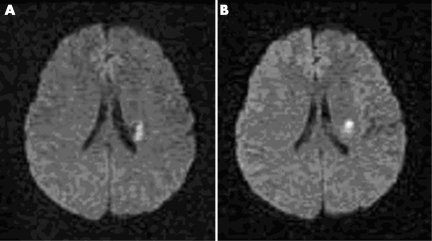
One case showed a false positive mixed signal lesion that confirmed a recurrent infarction in an adjacent area (fig 2). False positive DWIs for ischaemic stroke are very rare. Mullins et al reported that only one false positive was discovered from 411 images, possibly due to the “T2 shine through effect”.16 We used an algorithm to describe test results instead of using sensitivity and specificity because the results could not simply be divided into positive or negative. Both lesions with high and mixed signals were considered positive for stroke.
Figure 2 False positive for haemorrhage on DWI. (A) The DWI of a 60 year old man with pure motor stroke shows a lesion with mixed signal intensity, which indicates haemorrhage in the left basal ganglia. (B) The DWI of the same patient presented signs of pure motor stroke 3 months previously, showing a lesion with high signal intensity compatible with infarct in the adjacent area.
In this study, the lacunar infarcts mainly occurred in the basal ganglia, pons, corona radiata, thalamus and internal capsule. It is well known that lacunar syndrome type does not correlate with anatomical location.11 The same type of lacunar syndrome can be caused by lesions in a variety of locations. Furthermore, lesions that appear to be in the same location can give rise to different lacunar syndromes. Nine patients showed multiple lacunes on DWI. Multiple lacunes are seen in about 16% of lacunar infarctions, and suggest an embolic stroke mechanism.17
We have restricted our primary DWI study to classic lacunar syndrome. There are other atypical lacunar syndromes such as hemiballism and internuclear ophthalmoplegia.3 We believe that such patients may also be primary DWI candidates. Making use of MRI equipment more feasible in the ED would allow primary DWI to be used on many suspected stroke patients in the near future.
Limitation and future questions
There are several limitations to our study. Firstly, the study has no pathological heterogeneity other than stroke. All small lesions (brain tumour, infections, and neurosurgical procedure) regardless of the aetiology can produce lacunar syndrome. Moreover, the 13% haemorrhagic stroke rate in this study is much higher than in other reports.5 This discrepancy may be due to the differences in the patient populations. Secondly, being observational, this study was not able to compare DWI with a standard imaging modality, such as CT. Future studies should be larger, randomised, and compared with the current stroke evaluation algorithms on the basis of improving patient important outcome, cost effectiveness and diagnostic performances.
CONCLUSION
Primary DWI is a useful neuroimaging tool for patients with lacunar syndrome in the ED. Although more studies are required, primary DWI may be another diagnostic option for lacunar syndrome.
Abbreviations
AH - ataxic hemiparesis
CT - computed tomography
DCH - dysarthria clumsy hand syndrome
DWI - diffusion weighted imaging
ED - emergency department
MRI - magnetic resonance imaging
PMS - pure motor stroke
PSS - pure sensory stroke
SMS - sensorimotor stroke
Footnotes
Competing interests: there are no competing interests
References
- 1.ECC Committee, Subcommittees and Task Forces of the American Heart Association 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2005112IV1–203. [DOI] [PubMed] [Google Scholar]
- 2.Bamford J, Sandercock P, Jones L.et al The natural history of lacunar infarction: the Oxfordshire Community Stroke Project. Stroke 198718545–551. [DOI] [PubMed] [Google Scholar]
- 3.Fisher C M. Lacunar strokes and infarcts: a review. Neurology 198232871–876. [DOI] [PubMed] [Google Scholar]
- 4.Stapf C, Hofmeister C, Hartmann A.et al Predictive value of clinical lacunar syndrome for lacunar infarcts on magnetic resonance brain imaging. Acta Neurol Scand 200010113–18. [DOI] [PubMed] [Google Scholar]
- 5.Arboix A, Garcia‐Eroles L, Massons J.et al Hemorrhagic lacunar stroke. Cerebrovasc Dis 200010229–234. [DOI] [PubMed] [Google Scholar]
- 6.Schaefer P W, Grant P E, Gonzalez R G. Diffusion‐weighted MR imaging of the brain. Radiology 2000217331–345. [DOI] [PubMed] [Google Scholar]
- 7.Chung S P, Ha Y R, Kim S W.et al Diffusion weighted MRI as a screening tool of stroke in the ED. Am J Emerg Med 200220327–331. [DOI] [PubMed] [Google Scholar]
- 8.Chung S P, Ha Y R, Kim S W.et al Diffusion‐weighted MRI of intracerebral hemorrhage clinically undifferentiated from ischemic stroke. Am J Emerg Med 200321236–240. [DOI] [PubMed] [Google Scholar]
- 9.Schramm P, Schellinger P D, Fiebach J B.et al Comparison of CT and CT angiography source images with diffusion‐weighted imaging in patients with acute stroke within 6 hours after onset. Stroke 2002332426–2432. [DOI] [PubMed] [Google Scholar]
- 10.Landau W M. Clinical neuromythology III: ataxic hemiparesis: special deluxe stroke or standard brand? Neurology 1988381799–1801. [DOI] [PubMed] [Google Scholar]
- 11.Schonewille W J, Tuhrim S, Singer M B.et al Diffusion‐weighted MRI in acute lacunar syndromes. A clinical‐radiological correlation study. Stroke 1999302066–2069. [DOI] [PubMed] [Google Scholar]
- 12.Kase C S, Wolf P A, Hier D B.et al Lacunae infarcts: clinical and CT aspects. The Stroke Data Bank experience. Neurology 198636178–179.3945388 [Google Scholar]
- 13.Lai P H, Li J Y, Chang C Y.et al Sentitivity of diffusion‐weighted magnetic resonance imaging in the diagnosis of acute lacunar infarcts. J Formos Med Assoc 2001100370–376. [PubMed] [Google Scholar]
- 14.Lindgren A, Staaf G, Geijer B.et al Clinical lacunar syndromes as predictors of lacunar infarcts. A comparison of acute clinical lacunar syndromes and findings on diffusion‐weighted MRI. Acta Neurol Scand 2000101128–134. [DOI] [PubMed] [Google Scholar]
- 15.Ay H, Buonanno F S, Rordorf G.et al Normal diffusion‐weighted MRI during stroke‐like deficits. Neurology 1999521784–1792. [DOI] [PubMed] [Google Scholar]
- 16.Mullins M E, Schaefer P W, Sorensen A G.et al CT and conventional and diffusion‐weighted imaging in acute stroke: study in 691 patients at presentation to the emergency department. Radiology 2002224353–360. [DOI] [PubMed] [Google Scholar]
- 17.Ay H, Oliveira‐Filho J, Buonanno F S.et al Diffusion‐weighted imaging identifies a subset of lacunar infarction associated with embolic source. Stroke 1999302644–2650. [DOI] [PubMed] [Google Scholar]