Abstract
Following the accession of Poland to the European Union in 2004, large numbers of Polish migrant workers have come to the UK. We describe how this migration has impacted on an emergency department in the West Midlands, and suggest advice that should be given to such visitors about how to use the NHS.
On 1 May 2004 10 new countries, including the Republic of Poland, joined the European Union (EU). This allowed the free movement to the UK of workers from these countries. Soon after this date it was noticed that increasing numbers of patients of Polish origin were attending the emergency department at the Princess Royal Hospital, Telford. It was further noted that many of these attendances related to general practice conditions, and that these episodes were often complicated by language difficulties. We performed a retrospective study in order to analyse this phenomenon.
Methods
Patients of Polish origin who had attended the emergency department at the Princess Royal Hospital, Telford, were identified using a novel computer program that assigns a country of origin according to a patient's given and family names.1 Using this software the emergency department's records of the past 6 years were screened, up to and including 2005. Patients of Polish origin were further subdivided into those who were registered with a general practitioner (GP) and those who were not.
Of the unregistered Polish patients who attended in 2005, a convenience sample of 90 were further analysed. In particular, the appropriateness of the attendance was assessed by experienced practitioners in emergency medicine and in general practice, using agreed criteria (see appendix) and the notes were reviewed for any comments relating to communication difficulties.
Results
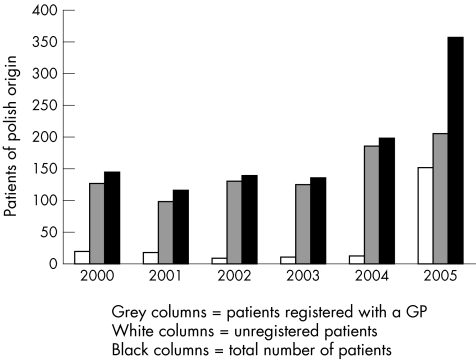
The results show that in the first 18 months following the expansion of the EU there was a significant increase in patients of Polish origin attending the emergency department at the Princess Royal Hospital, Telford (fig 1).
Figure 1 Annual attendances at the emergency department by patients of Polish origin.
Such attendances rose by over 150% from an average of 134 (2000–2003) to 357 in 2005. Of these 357 patients, 152 (43%) were not registered with a GP. The departmental average for unregistered patients was 7.4%.
Analysis of a convenience sample of 90 of the unregistered Polish patients who attended in 2005 showed that there were communication difficulties in at least 47 cases (52%) and that 35 (39%) presented with conditions that could have been treated by a GP.
Discussion
These statistics show a significant increase in the number of attendances of patients of Polish origin to the emergency department at the Princess Royal Hospital, Telford, since Poland acceded to the EU in May 2004. The data further indicate that many of these attendances were complicated by communication difficulties, and could have been dealt with by a GP.
Emergency departments have a duty to provide a timely and accurate service to all patients, regardless of their ability to speak English. Communication difficulties, however, can jeopardise good care and can be associated with considerable delays while interpretation facilities are arranged. It is, therefore, generally best if patients who do not speak English present to the emergency department with someone who can interpret on their behalf.
The issue of what constitutes an appropriate emergency department attendance is contentious, and in the past attempts have been made to define what conditions are appropriate and inappropriate.2,3 More recently, the British Association for Emergency Medicine has stated that any “acute illness” should be dealt with by emergency departments.4 The medical authors of this study disagree with this “open‐house” policy, and believe that general practice conditions are most expertly and economically managed in general practice.
With these thoughts in mind we suggest that when migrant workers apply to work in the UK they should be given information in their own language about how to use the National Health Service. In particular, that general practice conditions should be dealt with in general practice; that they can be seen by a GP as a temporary resident, and that GP cooperatives provide a 24‐h emergency service. Also, that if they require medical attention and do not speak English, they should be accompanied by someone who can translate for them.
Acknowledgements
The authors would like to thank Dr Peter Coventry MRCP MRCGP, and Rajvir Uppal, Information Department, Princess Royal Hospital for their kind assistance.
Abbreviations
Eu - European Union
GP - General Practitioner
Appendix
AGREED CRITERIA FOR APPROPRIATENESS OF ATTENDANCE AT EMERGENCY DEPARTMENT OR GENERAL PRACTICE SURGERY
Emergency department
Acute and serious illness *
Major trauma†
-
Minor trauma + x ray
-
-
and/or damage to deep structures
-
-
and/or administration of advanced anaesthetic techniques
-
-
and/or the application of a plaster cast
-
-
General practice
Acute minor illness
Chronic illness
Minor trauma not including emergency department categories above
*Characterised by admission to hospital and/or x rays and other investigations.
†Characterised by admission to hospital.
Footnotes
Competing interests: RW created the OriginsInfo software and receives royalties for its use.
References
- 1. OriginsInfo software—details of methodology and access terms available from richardwebber@blueyonder.co.uk
- 2.Lowy A, Kohler B, Nicholl J. Attendance at accident and emergency departments: unnecessary or inappropriate? J Pub Health Med 199416134–140. [DOI] [PubMed] [Google Scholar]
- 3.Dale J, Green J, Reid F, et all Primary care in the accident and emergency department: I. Prospective identification of patients. BMJ 1995311423–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.British Association for Emergency Medicine: The Way Ahead http://www.emergencymed.org.uk/