Abstract
The majority of mandibular fractures occur in young males aged 16–30 years. As with all traumas, the history and examination cannot be over emphasised as diagnoses can be made with these tools. It is important when taking an accurate history to ascertain the mode and mechanism of injury (fall, punch, road traffic accident), and the magnitude and direction of the force involved (high or low velocity impact).
Keywords: maxillofacial injuries, emergency department, mandibular fracture
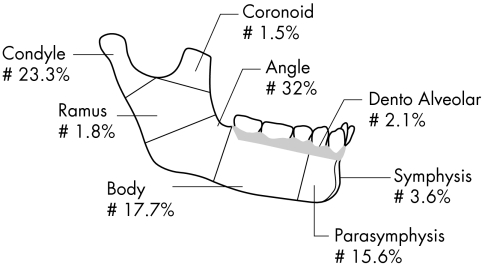
Multiple injuries are common in severe trauma or high velocity impact and the more severe the forces the greater the likelihood of fractures (fig 1).
Figure 1 Anatomical regions of the mandible and the relative percentages of areas involved in mandibular fracture.1
Diagnosis is obvious with a gross deformity or displacement, but in other cases a fracture may be suggested in the history and examination. Radiographs will then confirm the fracture.
History
Enquire about mechanism of injury. It is important to ask about previous facial fractures.
In mandibular fractures the occlusion is the key. Occlusion is the way the teeth bite together. Get the patient to gently close their teeth together and then ask them if the teeth feel in the correct position.
Note, in a displaced fractured mandible the patient may sometimes believe they have lost a tooth when in fact they have not; it is because of mobility at the fracture site.
Is there loss of function (can not bite or chew); is this because of pain, swelling or mobility? It is important to document any altered sensation along the distribution of the mental nerve.
Clinical examination
Examine for any obvious fracture: a gingival tear, displacement or step in the teeth, or mobility in the mandible.
A sublingual haematoma is not always a consistent finding, but when present is strongly suggestive of a mandibular fracture.
Probably the most important feature is evidence of altered occlusion. Are the teeth biting together in a normal or abnormal position? The patient is the best judge of this. If occlusion is altered a fracture is very likely.
Palpate both extra‐orally and intra‐orally, feeling for crepitus, assessing for pain or tenderness on palpation of the mandible.
Evaluate the dentition; check for any loose or avulsed teeth. If teeth are missing are they accounted for? If not, a chest x ray is mandatory. If the patient wears a denture ensure all pieces are present; remember that inhaled pieces of broken denture may not show on x ray.
Assess for tenderness in the region of the tempromandibular joints, as well as examining the ear canal bilaterally for bleeding or haematoma, as these symptoms and signs can be suggestive of a condylar neck fracture. Beware of the patient with a graze on the chin with trismus as it is suggestive of condyle fracture. Bleeding from the ear is often diagnosed as a skull base fracture; remember it is common in condylar fractures because of a tear in the anterior wall of the meatus.
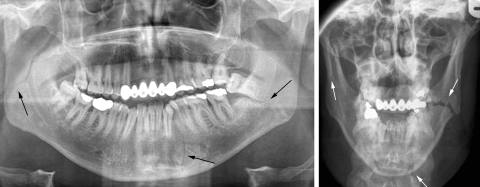
Figure 2 Symphysis and bilateral condyle fracture. Note that the left condyle is displaced and the right condyle is minimally displaced. Note the soft tissue shadow of oropharynx highlighted (white broken line) on left, which is often mistaken as a fracture.
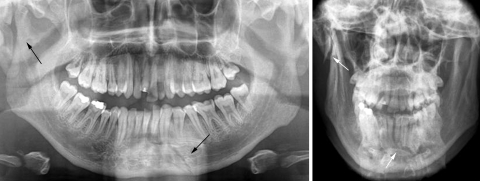
Figure 3 Right condyle/ramus, undisplaced left parasymphysis, and left angle fractures. Note widening of tooth socket of last standing lower left molar on oral pan tomogram, which suggests a fracture.
Figure 4 Right condyle left parasymphysis fracture. The condyle fracture is difficult to see on the oral pan tomogram and confirms the need of a second view, where it is easily seen.
Radiological assessment
Radiographs help confirm any clinical findings ( figs 2–4). Two views are advised in maxillofacial trauma. In suspected mandibular trauma standard views required are the oral pan tomogram and posterior anterior mandible. If an oral pan tomogram is not available perform a lateral oblique view.
Check the radiograph for obvious fractures. In displaced fractures a step is obvious in the cortex. An undisplaced fracture may not show on plain film for 7–10 days. Pay close attention to the condylar head area as fractures here are easily missed.
Initial management
Airway compromise is uncommon in the conscious patient; however, it may occur in an unconscious patient, particularly those who have sustained bilateral parasymphyseal fracture. These patients may require forward repositioning of the mandible and tongue to prevent airway obstruction.
A conscious patient with maxillofacial injuries is usually more comfortable sitting upright as this allows blood and secretions to drain out of the mouth.
Mandibular fractures are usually open in nature, and patients should be given appropriate antibiotics and analgesia prior to referral to the maxillofacial service. They should be advised to remain nil by mouth. Ensure the lips are kept moist with Vaseline ointment.
There is no need for antibiotics in a closed condylar fracture.
Suggested further reading
Fonseca RJ. Oral and maxillofacial surgery. Volume 3: trauma. London: Saunders, 2000:85–148.
Ward Booth P, Eppley B, Schmelzeisen R. Maxillofacial trauma and esthetic facial reconstruction. London: Churchill Livingstone, 2003:261–298.
Acknowledgements
The authors would like to thank Simon Edwards, Medical Illustrator, Morriston Hospital, and Michelle and Ronan for their cooperation in the production of this article.
Footnotes
Competing interests: None declared.
References
- 1.Dongas P, Hall G M. Mandibular fracture patterns in Tasmania, Australia. Aust Dent J 200247(2)131–213. [DOI] [PubMed] [Google Scholar]